



 |
 |
 |
 |
 |
 |
 |
 |
Earliest Sign of Root Fracture
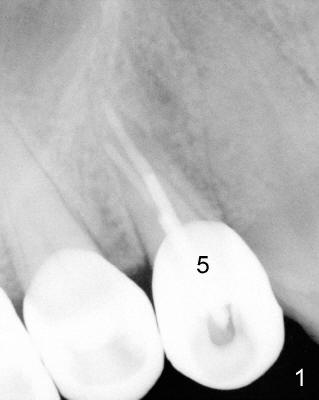
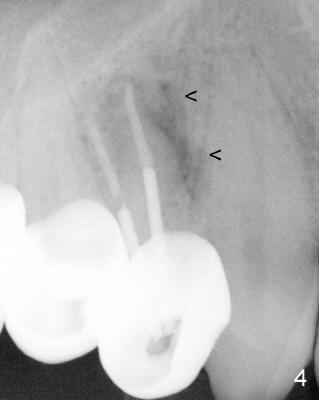
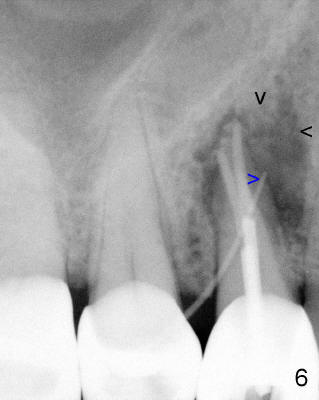
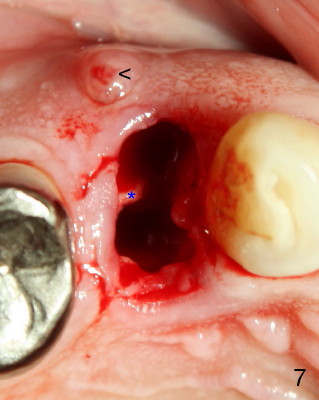
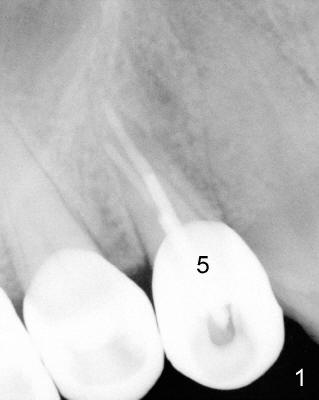
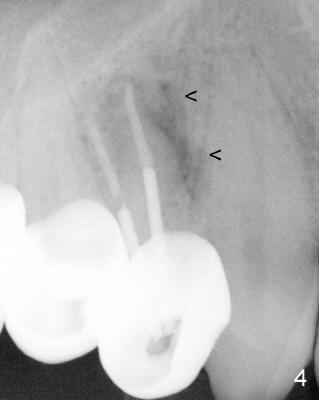
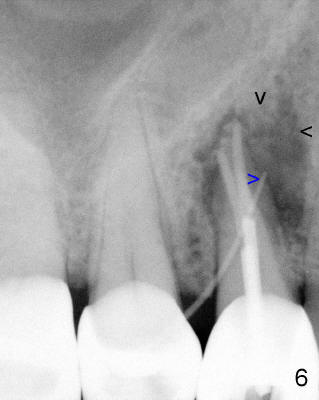
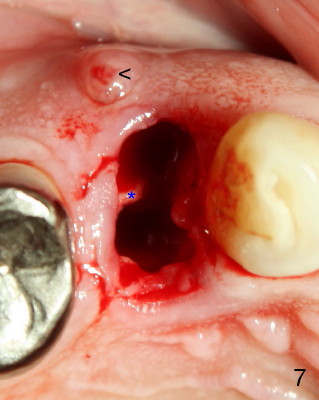
A 68-year-old male patient presented to office in March 2011 with chief complaint "upper right tooth is not comfortable". Clinical exam shows missing teeth: #13,14,30, and 31, replaced by removable partial dentures. The tooth #5 has mild mobility and percussion. Pocket depth is within normal limit. X-ray shows no significant finding (Fig.1,2). Three months later, he returned with chief complaint "The tooth has swelling". It appears that there is exostosis on buccal aspect of upper teeth. There is no erythema or tenderness on buccal mucosa around the tooth #5). But X-ray shows periradicular radiolucency (arrowheads in Fig.3,4). Cone Beam CT was recommended to confirm diagnosis of root fracture. Approximately one month later, abscess developed with fistula formation. Symptoms were controlled by taking Amoxicillin. On August 2, 2011, the patient returned for prophylaxis. The fistula was present (arrowhead in Fig.5). Gutta percha #30 was inserted into the fistula. PA was taken. The point of the gutta percha (blue arrowhead in Fig.6) points to enlarged periradicular radiolucency (black arrowheads). Deep pockets were in distobuccal and lingual. Decision was made to extract the tooth. Fig.7 shows the socket immediately extraction. The buccal plate is perforated. The septum (*) is not intact. Cracking sounds were heard during extraction. In fact the lingual root is obliquely fractured with exposed post (Fig.8: *). There is another cracking line from the buccal root to the lingual one (arrowhead). In brief, the earliest sign of root fracture is nonspecific. It should alert us to its suspicion.
Xin Wei, DDS, PhD, MS 1st edition 08/02/2011, last revision 08/03/2011