


 |
 |
 |
 |
|
 |
 |
 |
 |
|
 |
 |
|||
Immediate Implant in a Four-Walled Defect
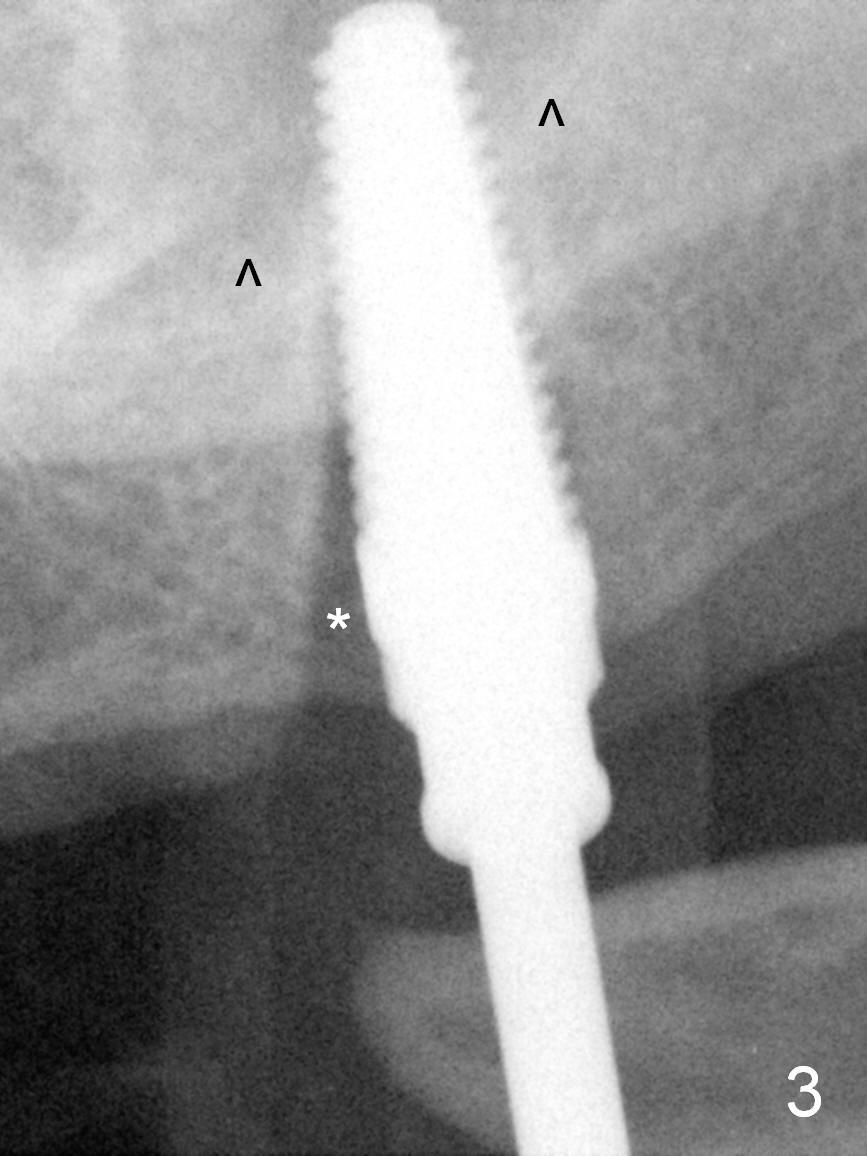
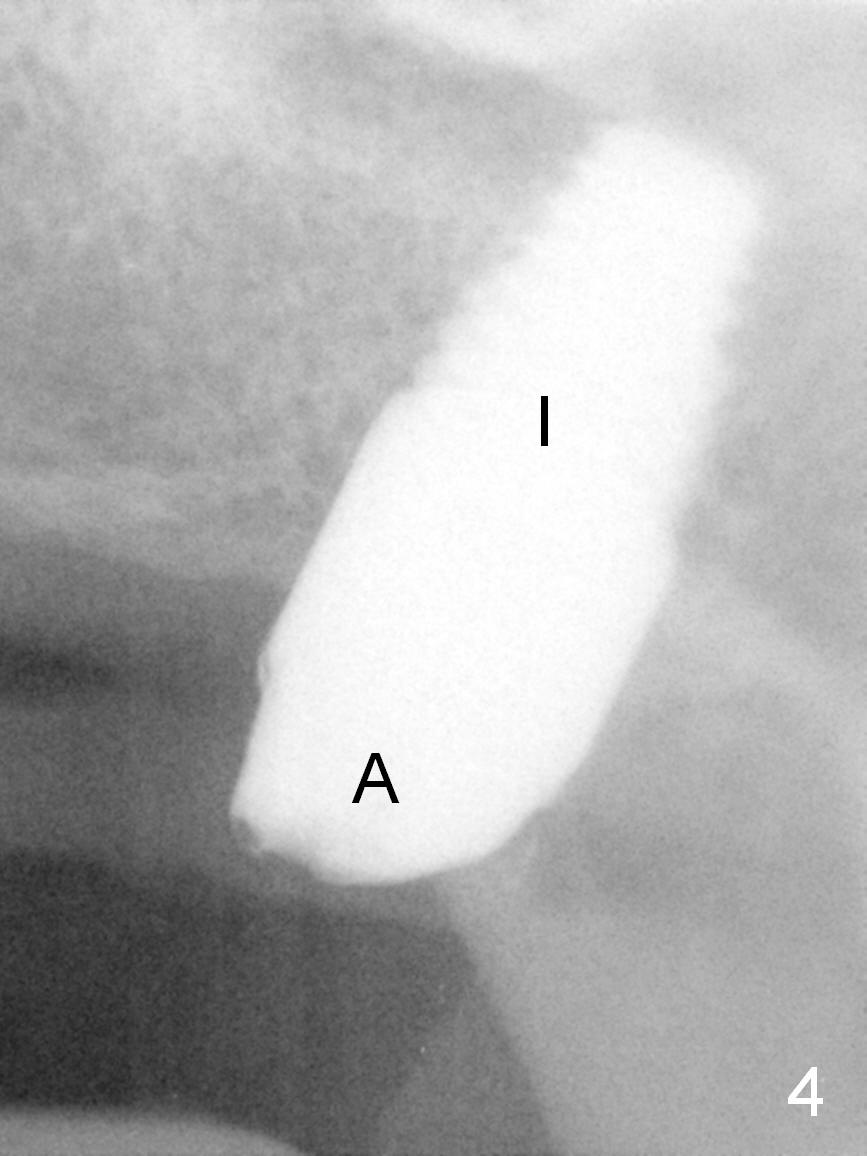
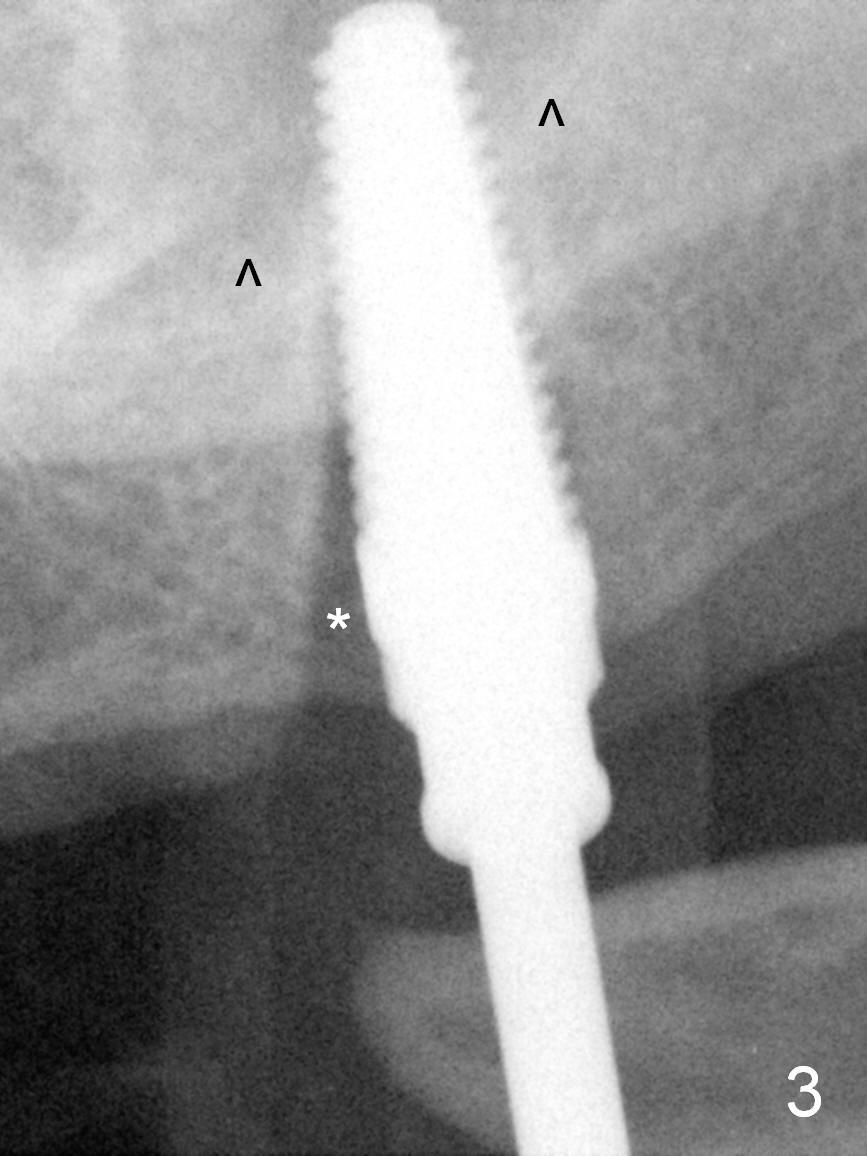
The patient returns for surgery next day. There is severe infection around the tooth #11 (Fig.1). The root stump at #15 is oval in shape: 6x9 mm (Fig2). After extraction of #15 and Metronidazole disinfection, a 5x17 mm tap is used to initiate osteotomy palatally, but it deviates buccally. Drill/reamers have to be used to create osteotomy before re-insertion of the 5x17 mm tap with stability (Fig.3). Note the mesial gap (Fig.3 *); when a 6x17 mm tap is inserted, the mesial gap still exists. It disappears when a 7x17 mm tap is placed. Therefore a 7x14 mm implant is placed with insertion torque > 60 Ncm (Fig.4).
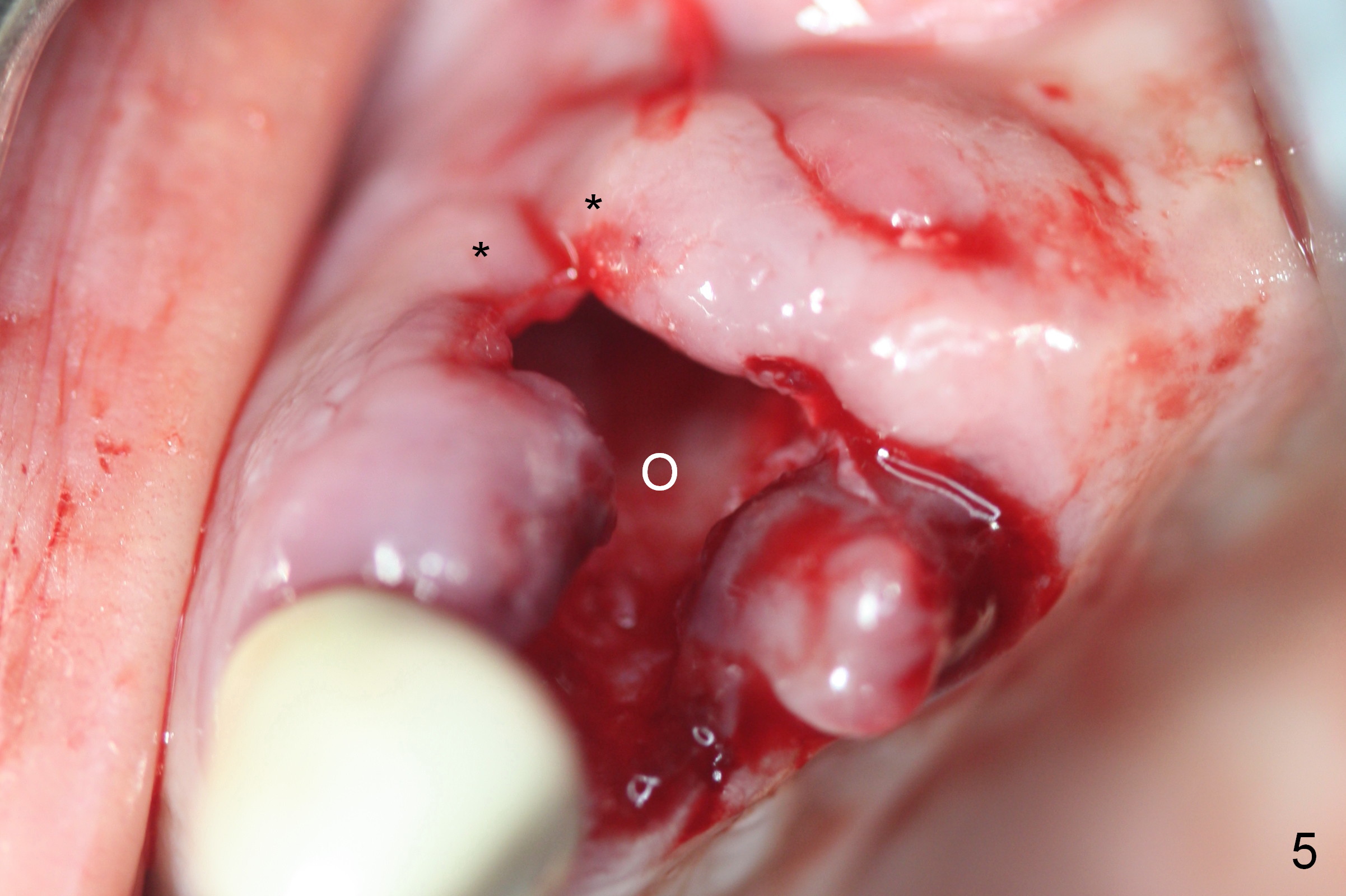
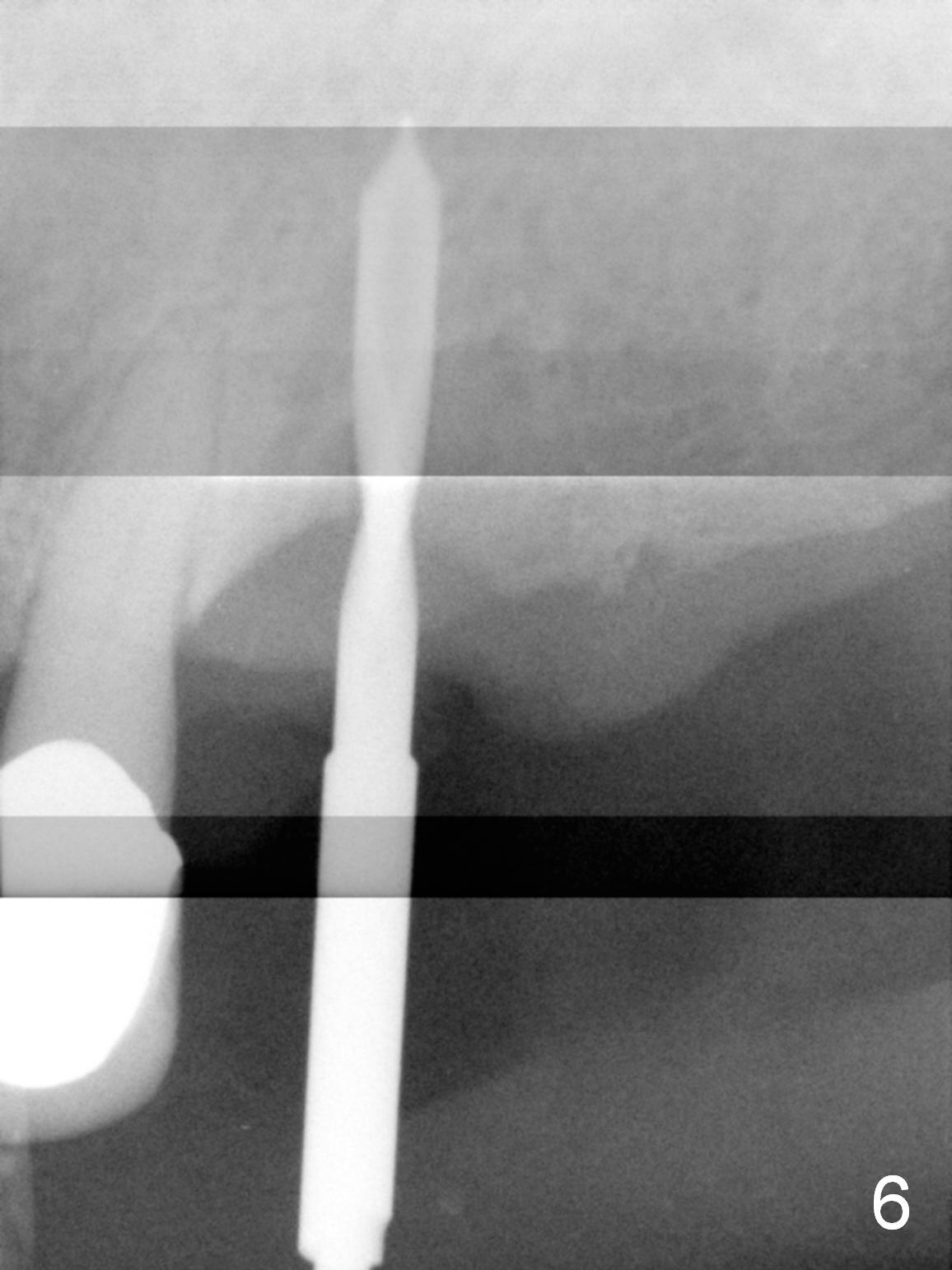
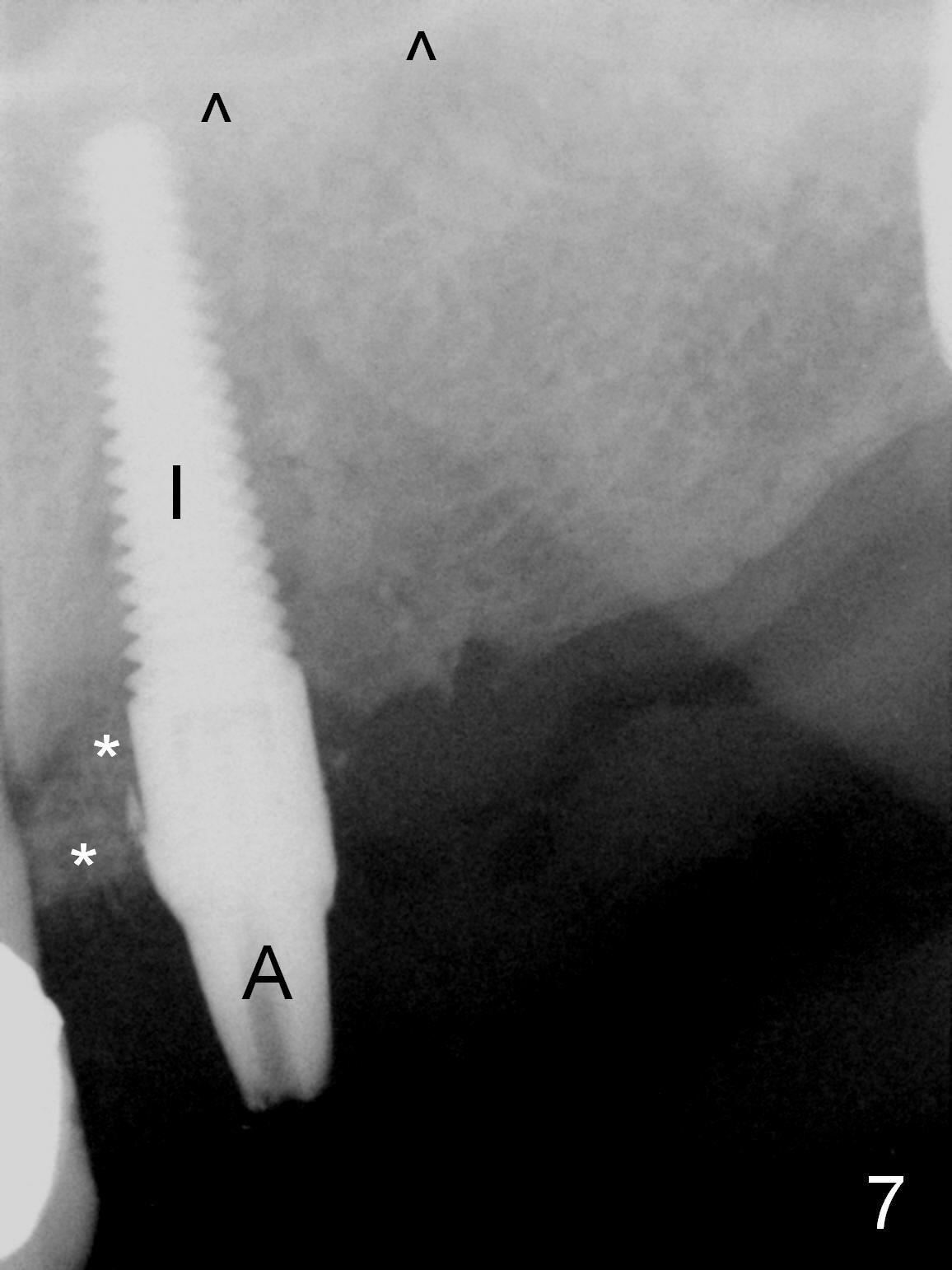
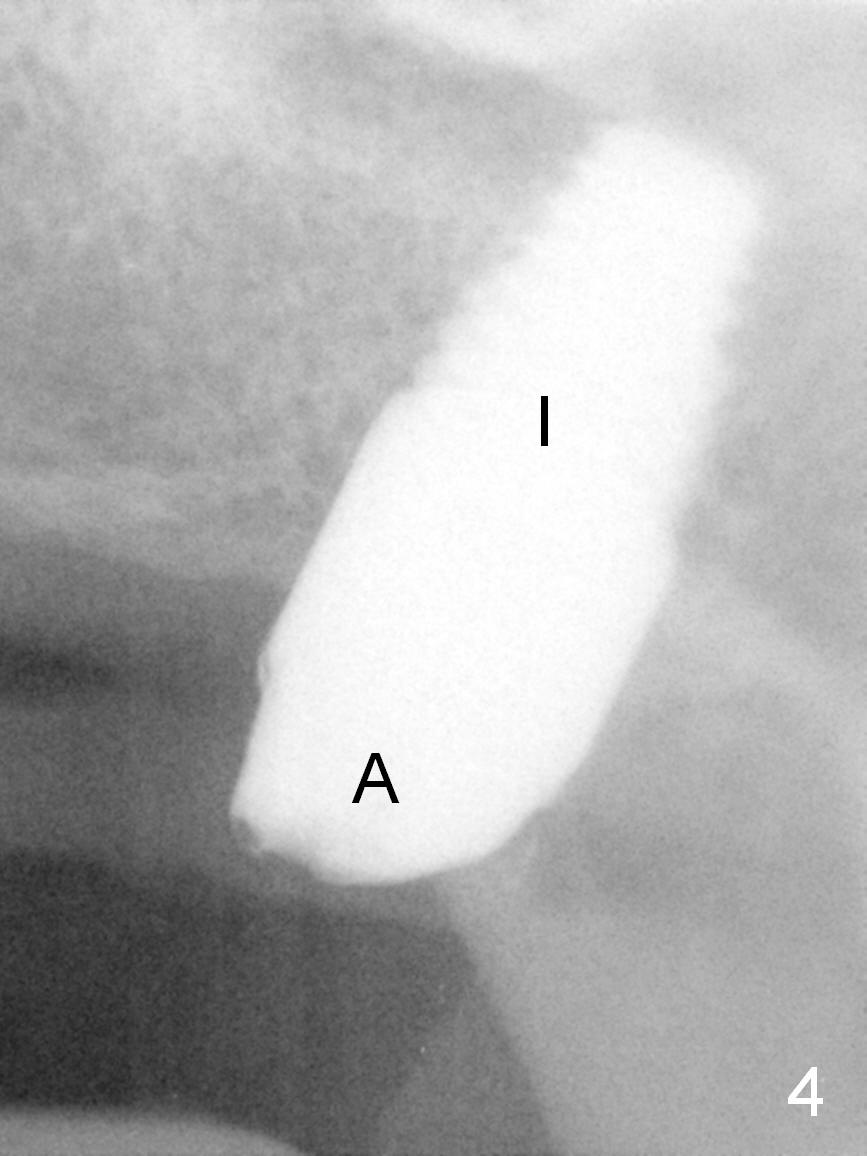
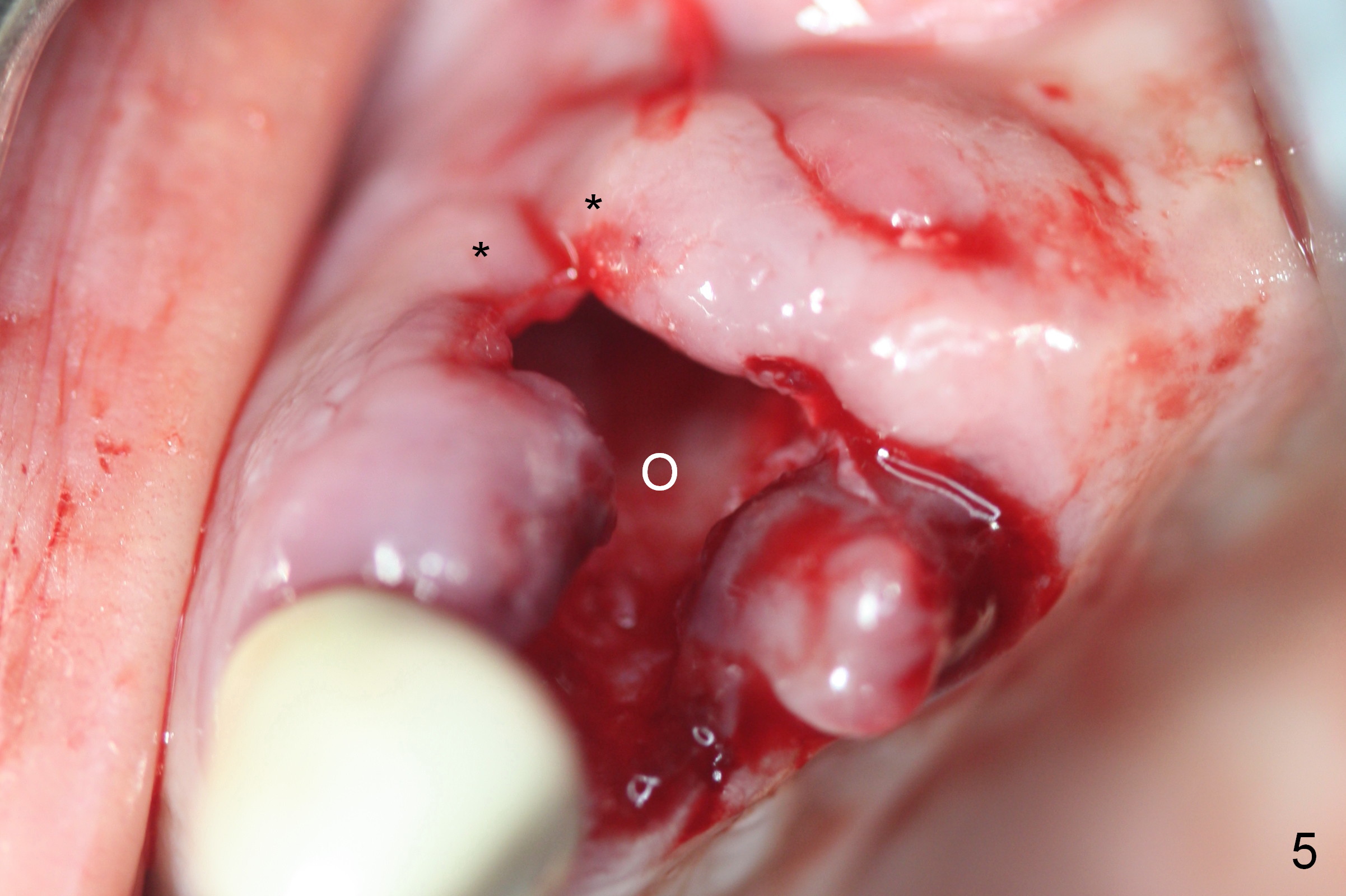
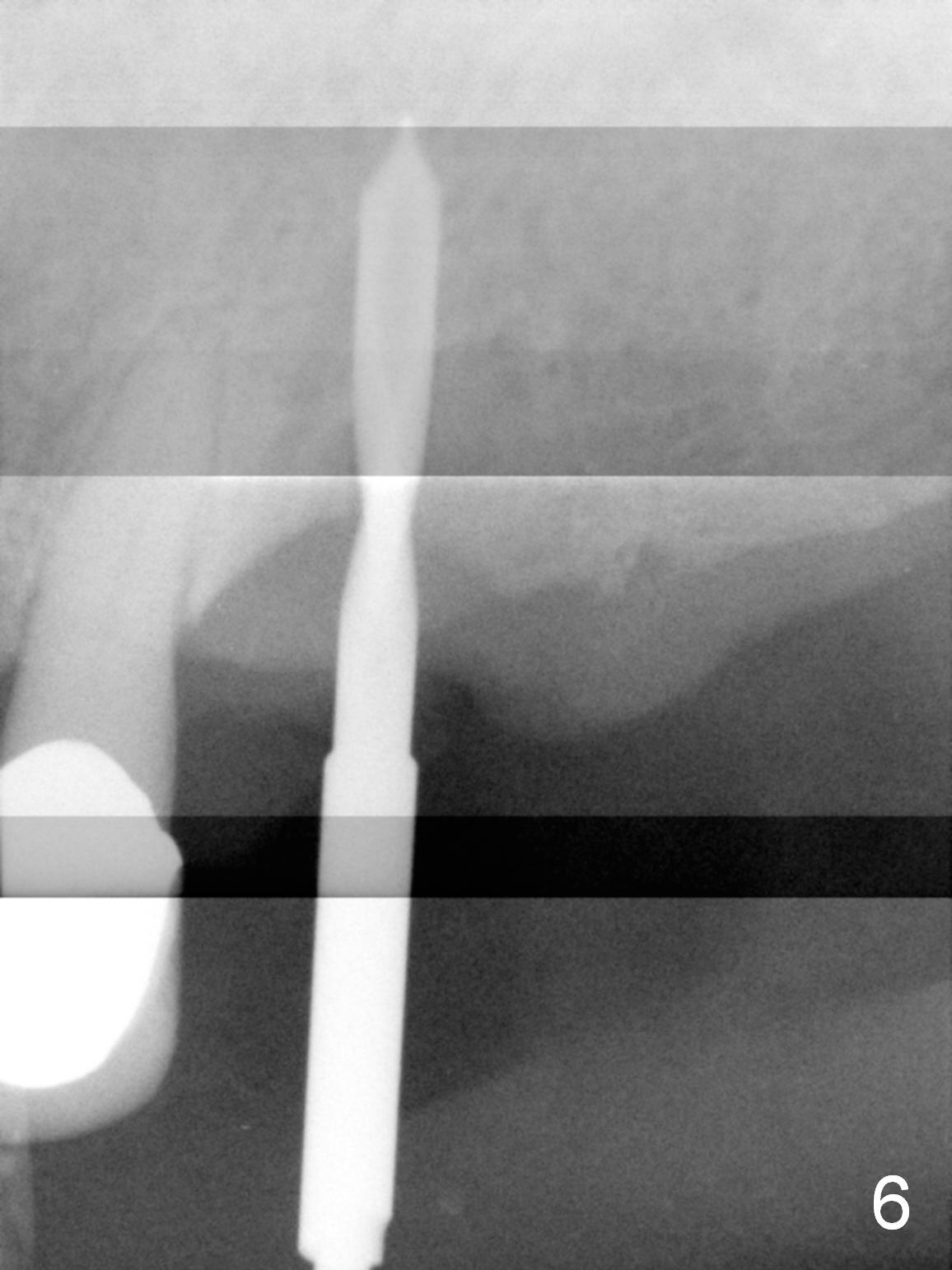
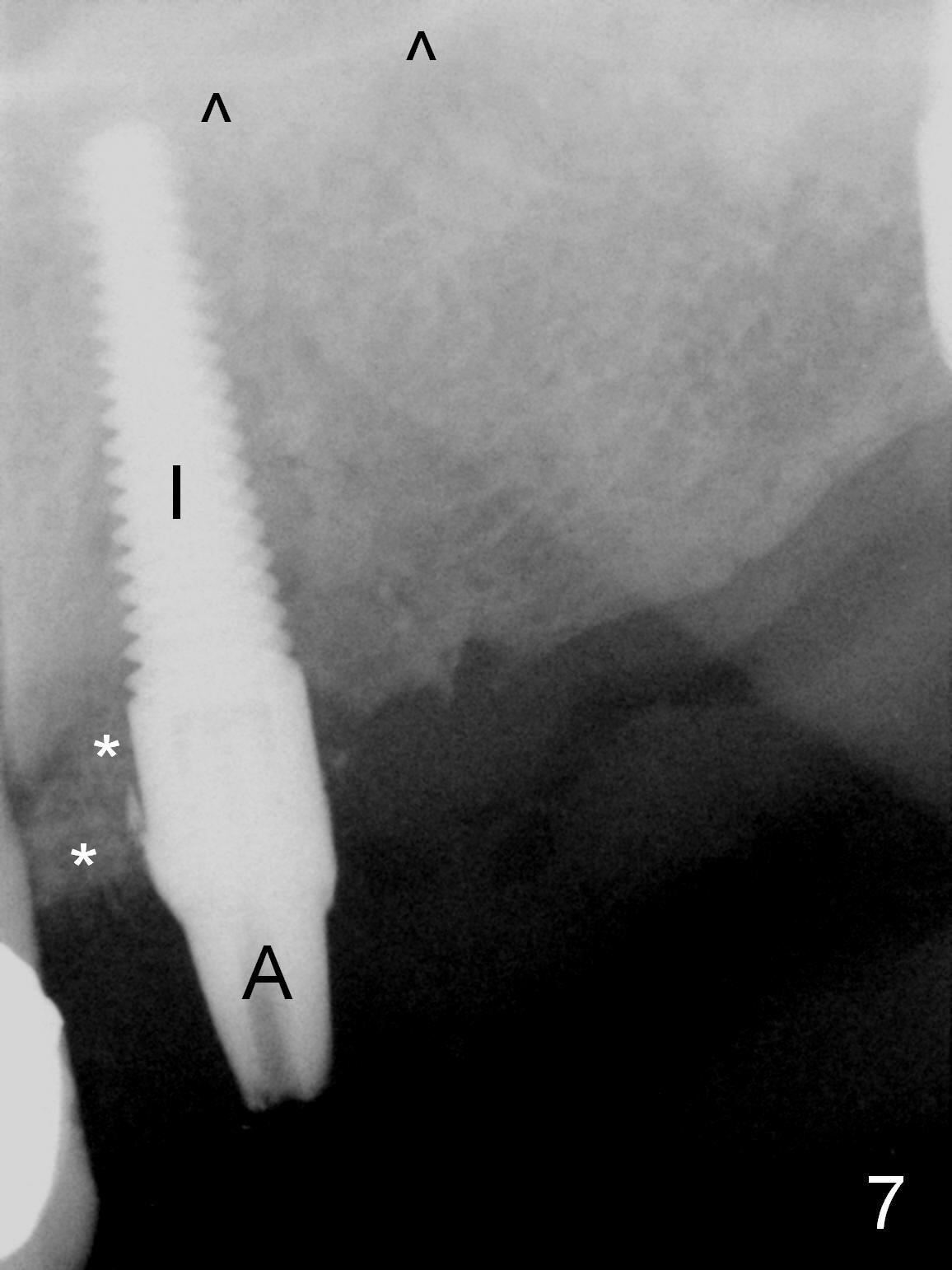
Immediate implant placement at #11 is done second, because the socket needs longer period of time for Metronidazole disinfection than #15. The antibiotic tablet is effectively ground with a bone mill. It appears that Metronidazole does not taste as bad as Clindamycin. The coronal portion of the buccal plate of #11 is lost (Fig.5 *), although the base bone is wide. Osteotomy is initiated as palatally as possible (Fig.5 O; Fig.6); in the end, the buccal coronal threads of a 4.5x20 mm implant are exposed and then covered by bone graft (autogenous, mineralized and demineralized allograft and Osteogen; Fig.7 *). Between the bone graft and the buccal gingiva is Osteotape (collagen membrane and Osteogen). After placement of abutments at #11 and 15 (Fig.4,7 A), a provisional FPD is fabricated with a stent. Perio dressing is placed last for maximum wound protection and graft containment.
One to three implants will be placed at the sites of #12-14 at a second stage.
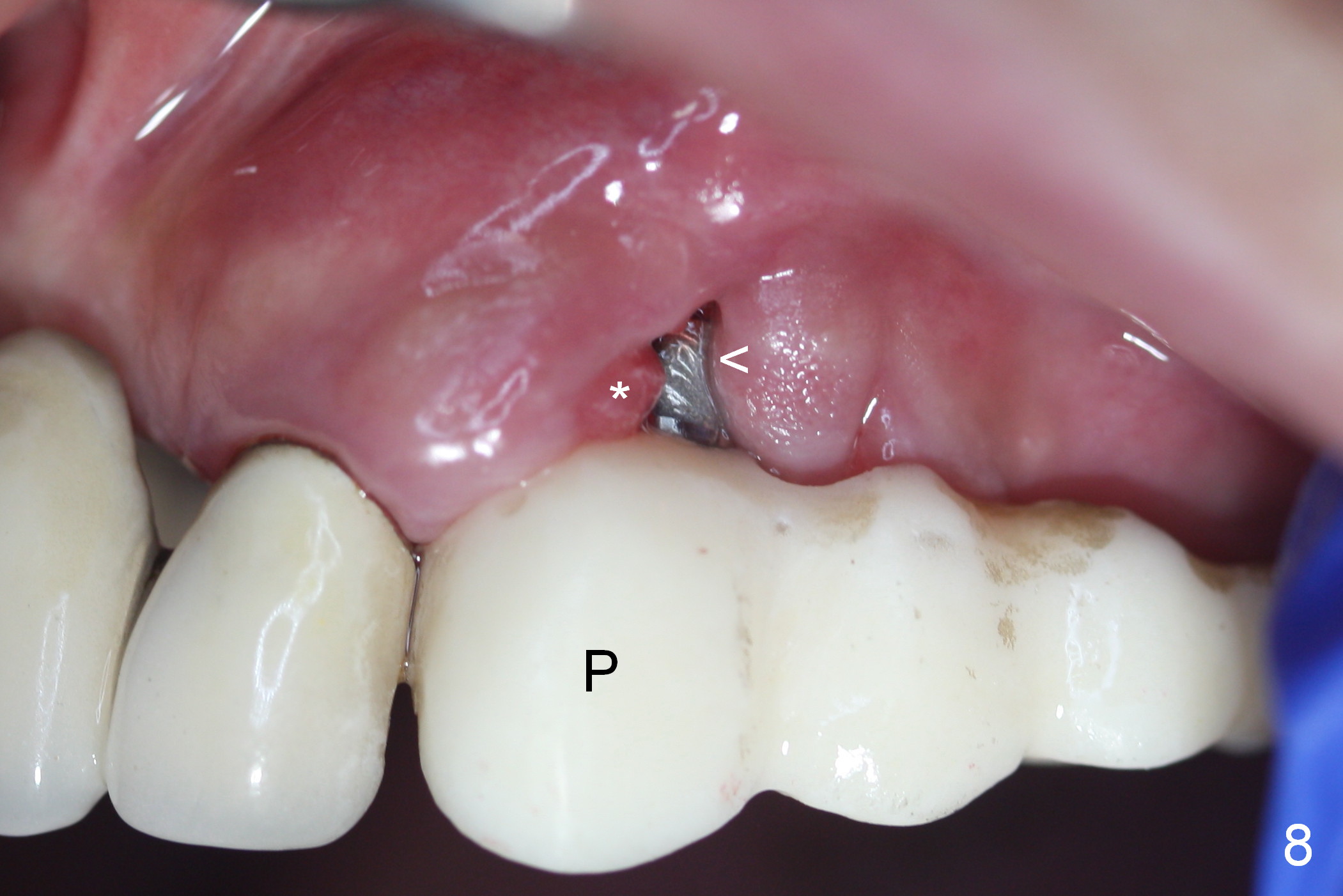
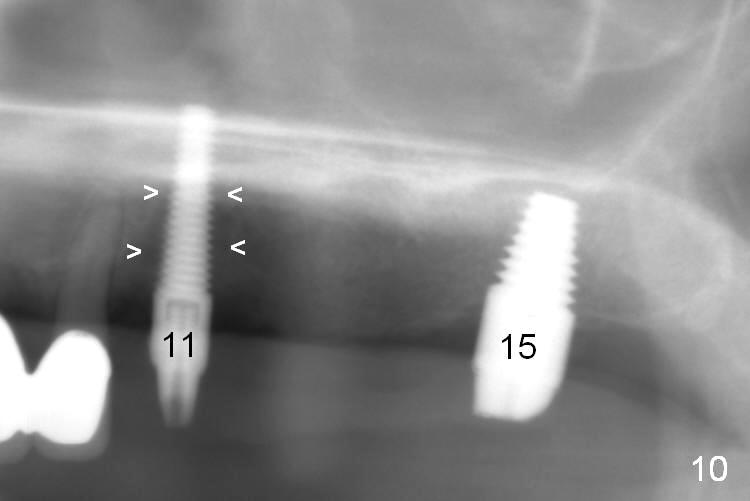
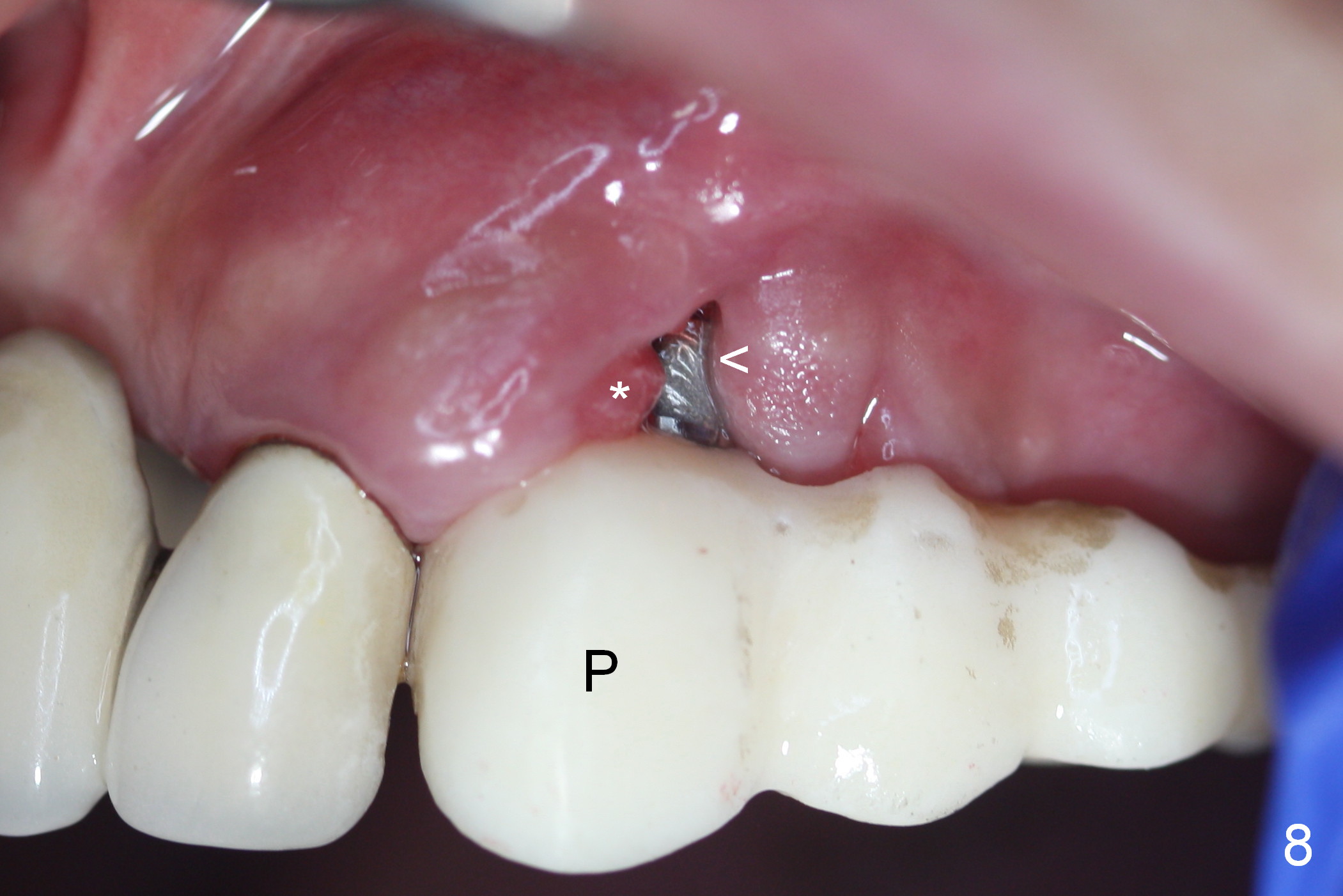
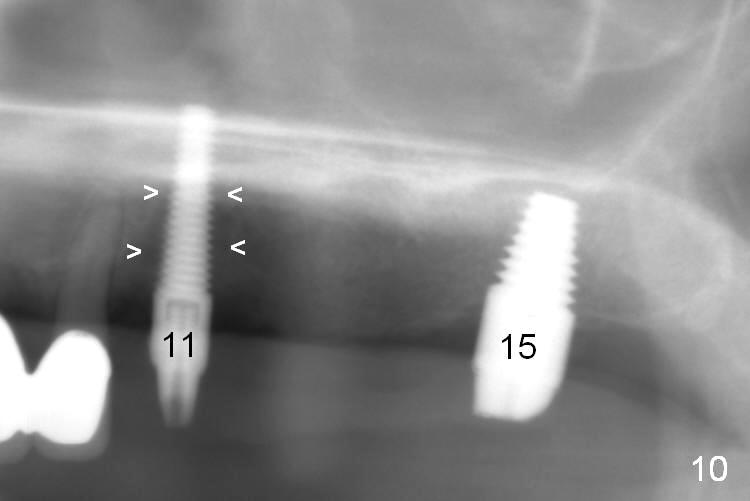
Eight days postop, the perio dressing and buccal bone graft have been lost without closure of the buccal cleft (Fig.8 <, as compared to Fig.5). Ideally, the margin of the immediate provisional (P) should have been extended apically to cover the cleft securely. Closure of the cleft with suture is not practical, since the tissue was and is erythematous and edematous (*). By contrast, the palatal infection subsides more without defect (Fig.9 *). Oral hygiene instruction is re-emphasized. Panaramic X-ray taken 8 days postop shows that there is large radiolucency in the mid-root area (Fig.10 arrowheads). The patient will return for 2nd stage of implant placement between #11 and 15.
Return to Upper Canine, Molar Immediate Implant, Posterior Immediate Provisional, 1-Piece
Xin Wei, DDS, PhD, MS 1st edition 08/04/2015, last revision 02/03/2019