
.jpg)


  |
 |
.jpg) |
 |
|
 |
 |
 |
||
 |
 |
 |
 |
 |
 |
 |
 |
||
 |
 |
|||
Occlusal and RPD Clearances M
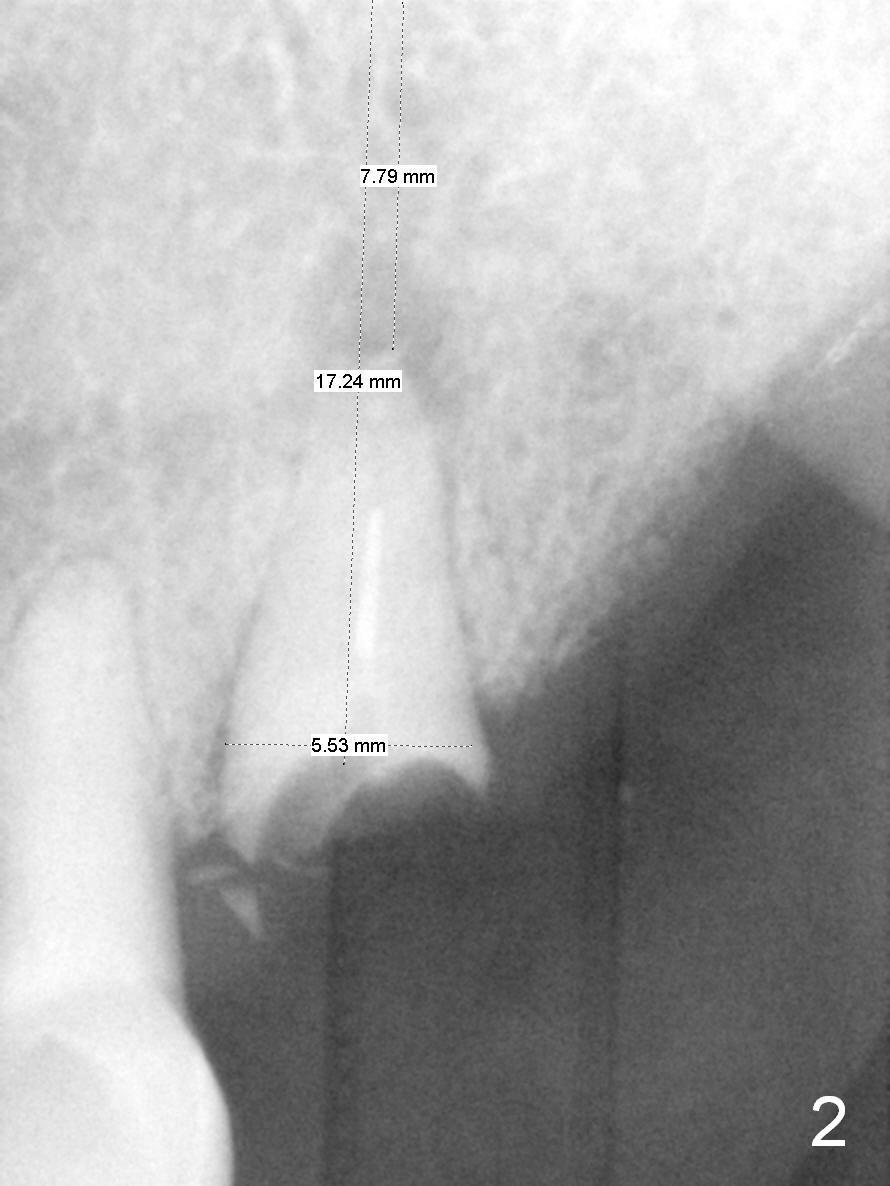
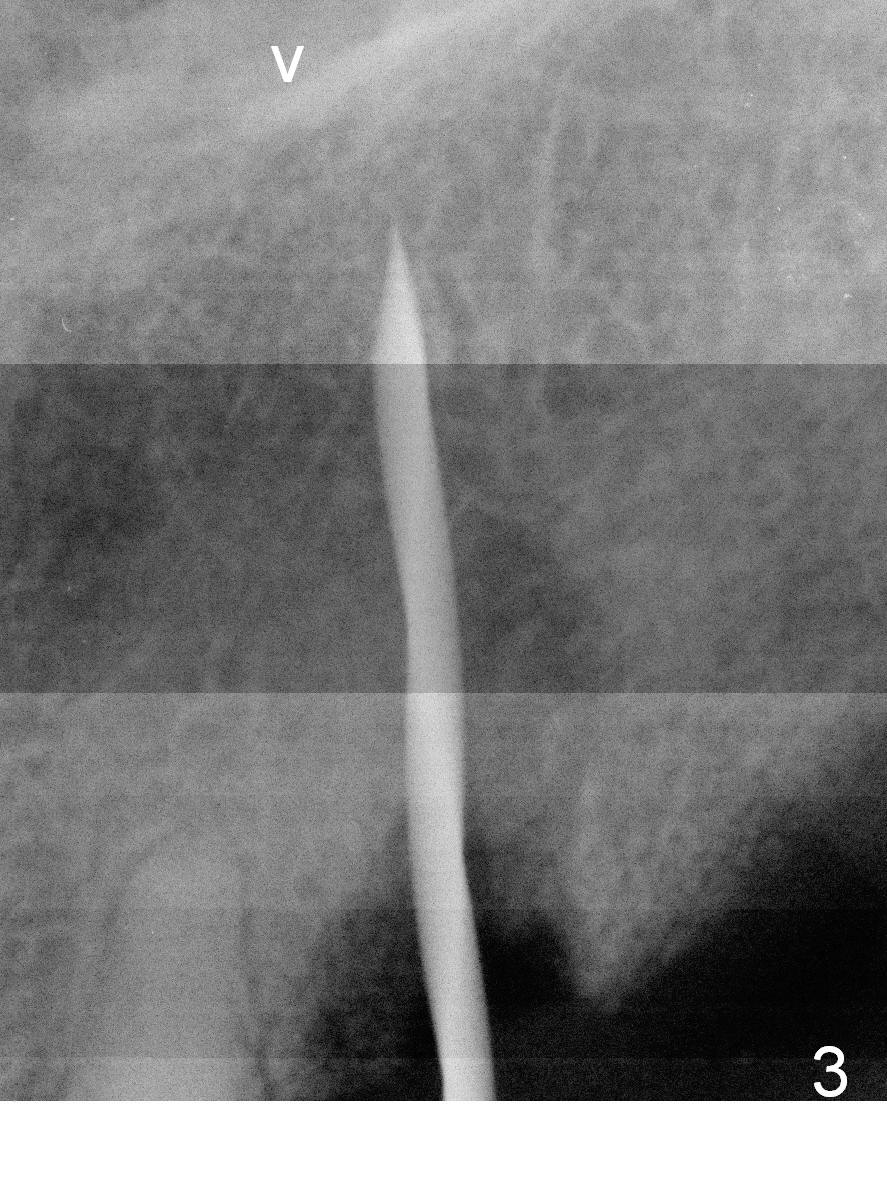
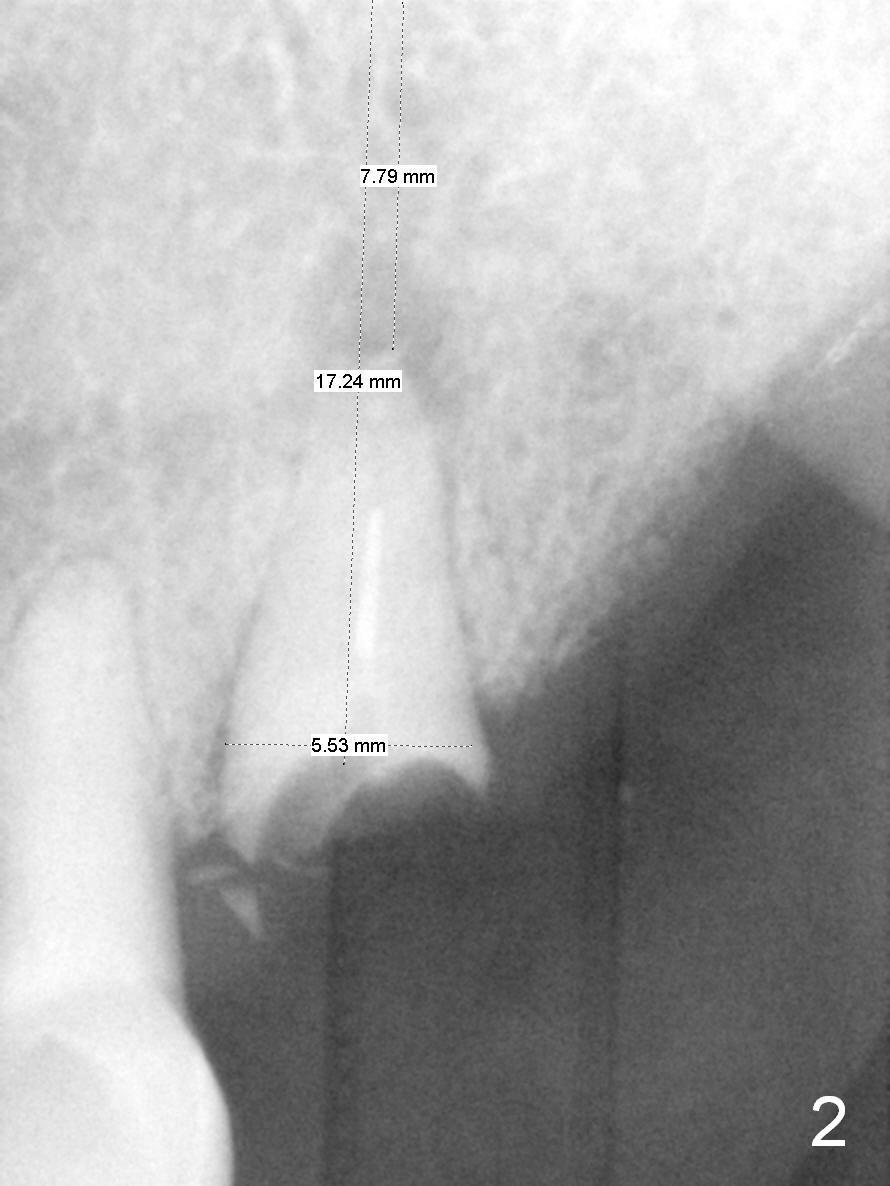
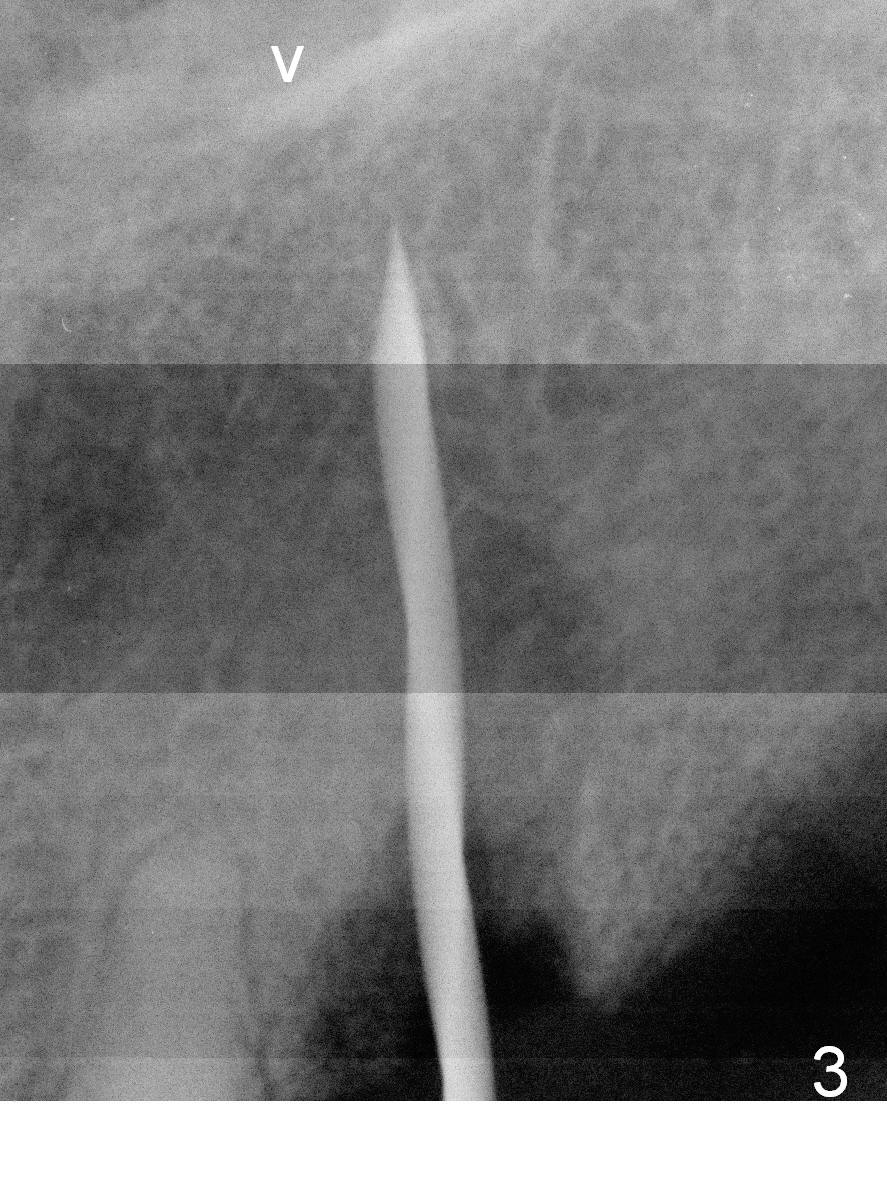
Preop PAs show periapical radiolucency at #11 (Fig.1 *) and bone height for at least 17 mm bone-level implant (Fig.2). The root of the extracted tooth is measured 4 mm mesiodistal and 6.5 mm buccopalatal. The labial plate is thin. A 1.5 mm pilot drill is used to start osteotomy at 17 mm (gingiva level; Fig.3); it appears that a longer implant is possible (arrowhead: presumptive nasal floor). The osteotomy is then moved distal before using 2, 3 and 3.2 mm drills at 18 mm (bone level). A 4x18 mm implant is placed (>50 Ncm) with a 4.5x5(3) mm abutment (Fig.4). The mesial margin of the abutment is too close to the crest. In fact an abutment with longer cuff (4 or 5 mm) should be used instead. The distal margin of the longer cuff may be supragingival, which could be trimmed.
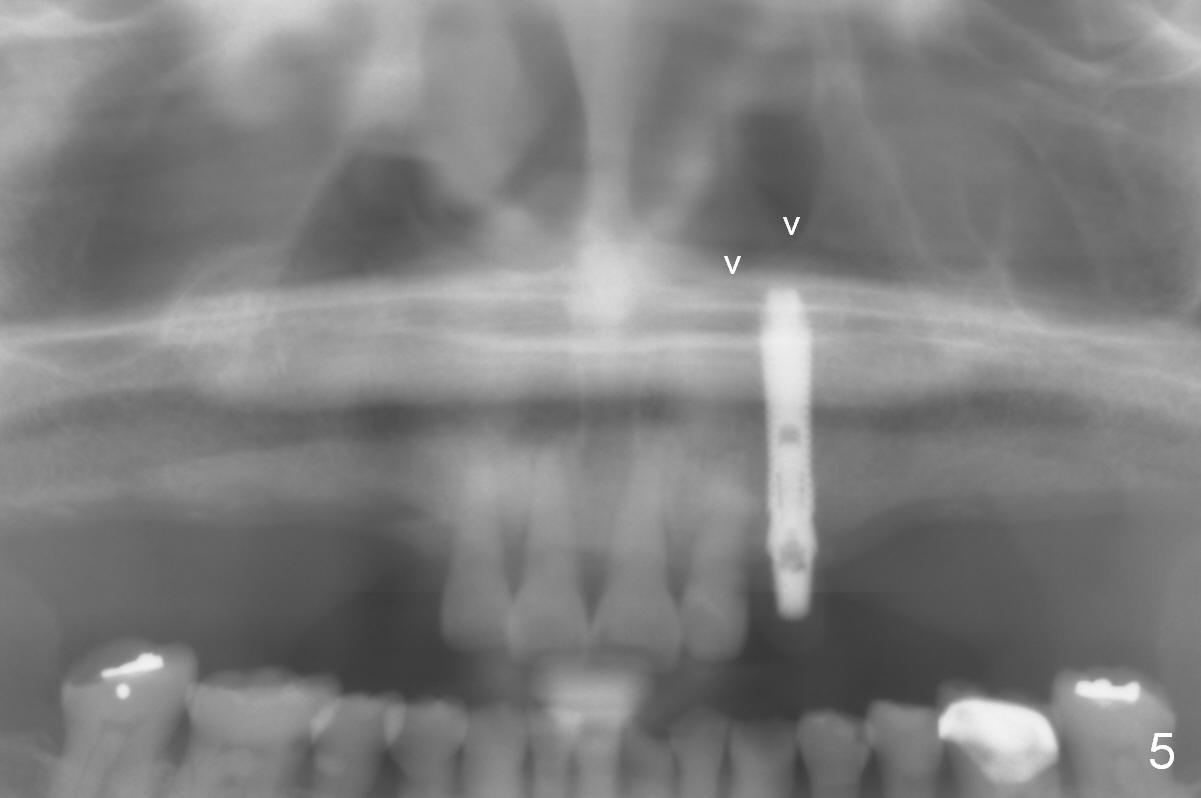
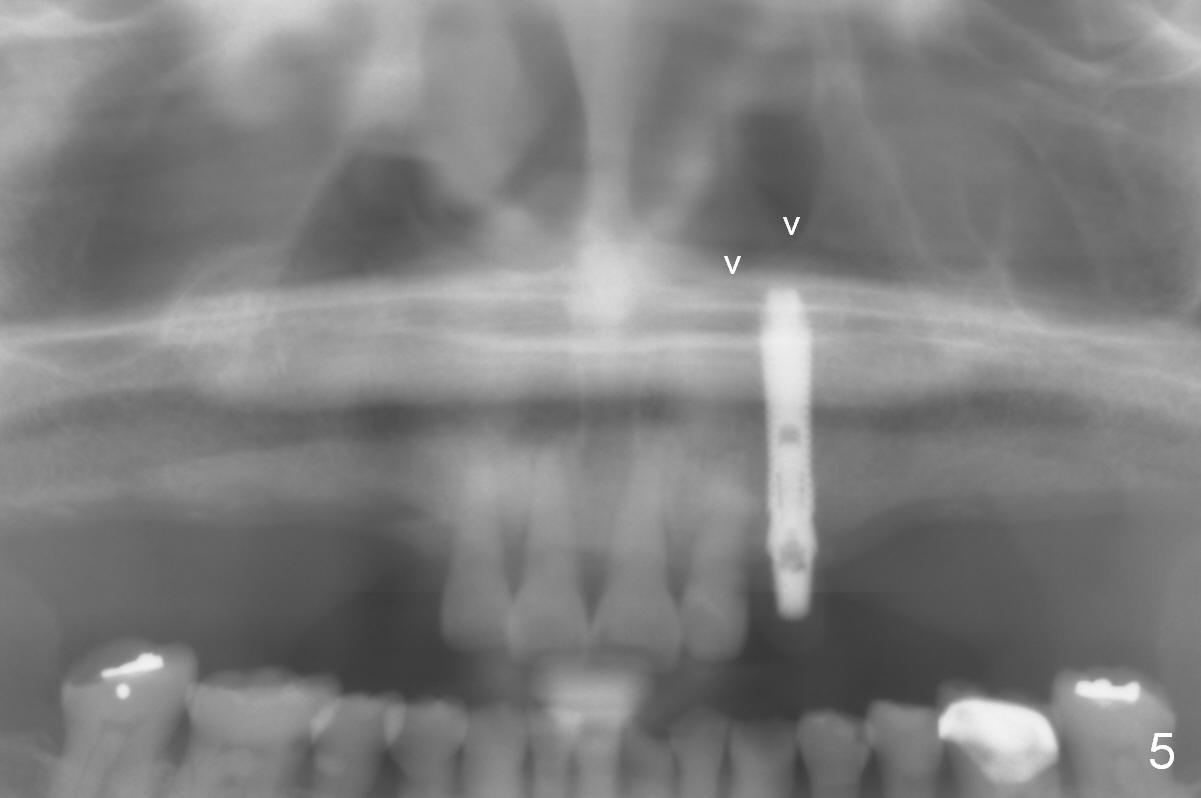
After immediate provisional cementation, panoramic X-ray is taken. The nasal floor (Fig.5 arrowheads) is not invaded; the presumptive nasal floor (Fig.3 arrowhead) is lower.
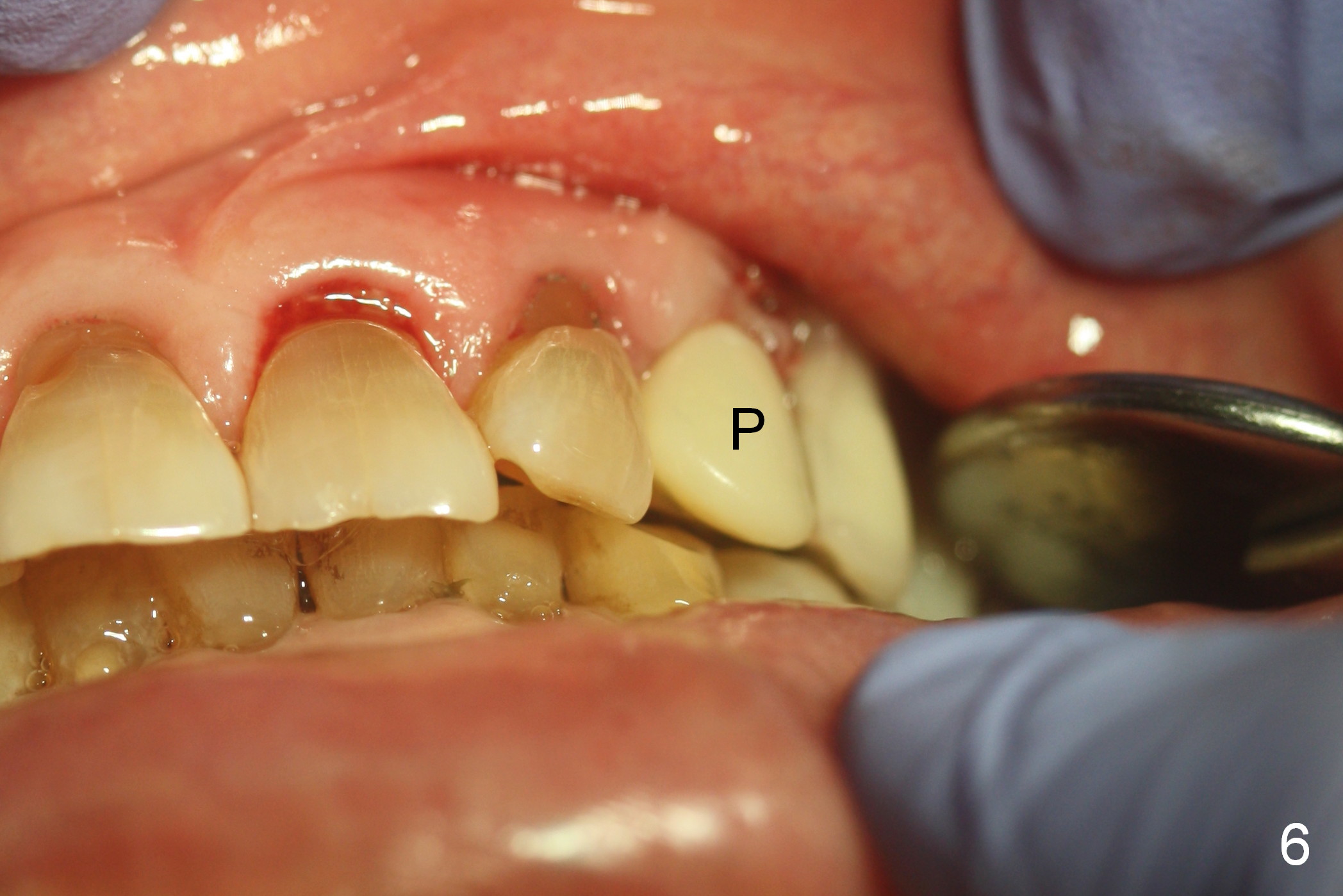
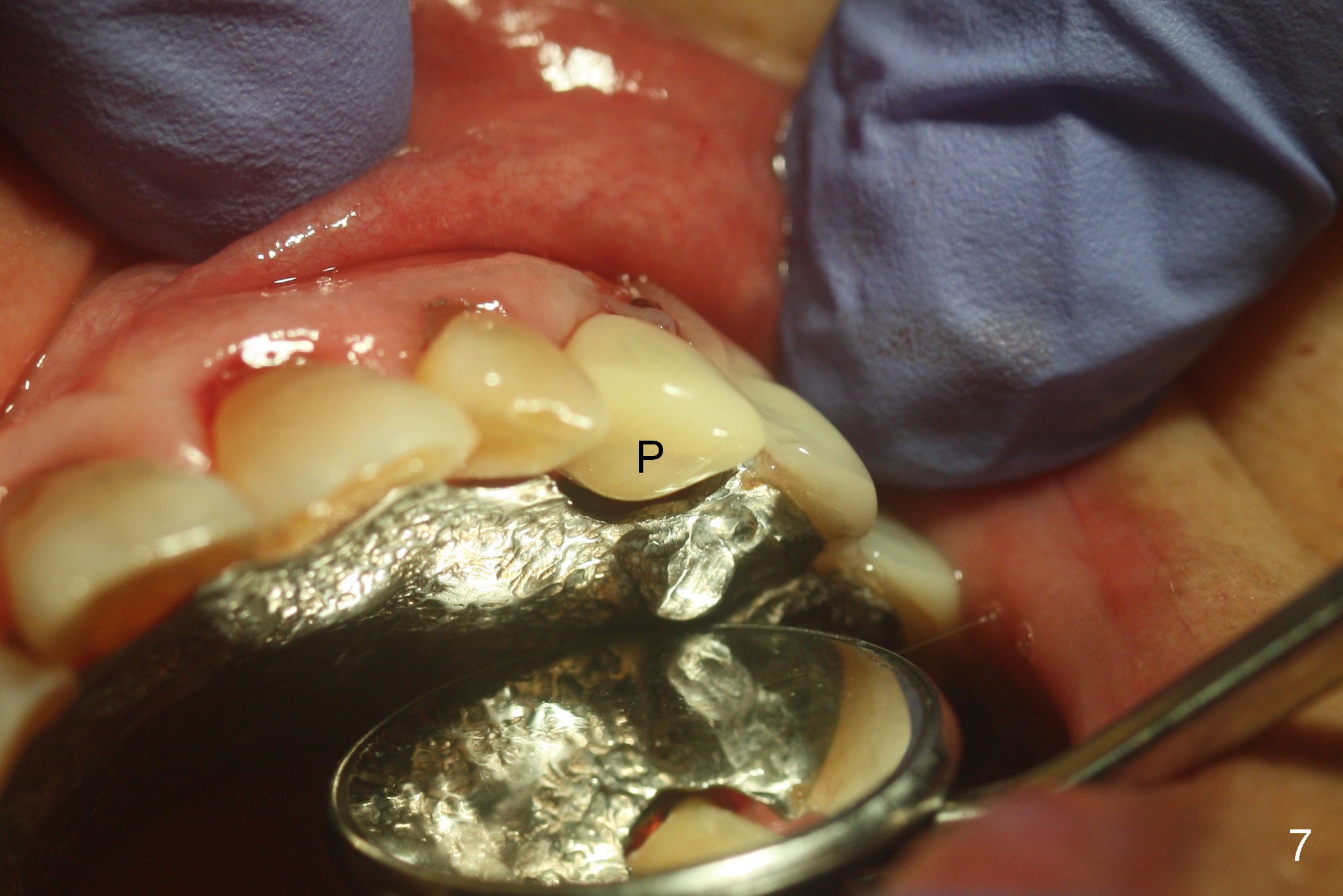
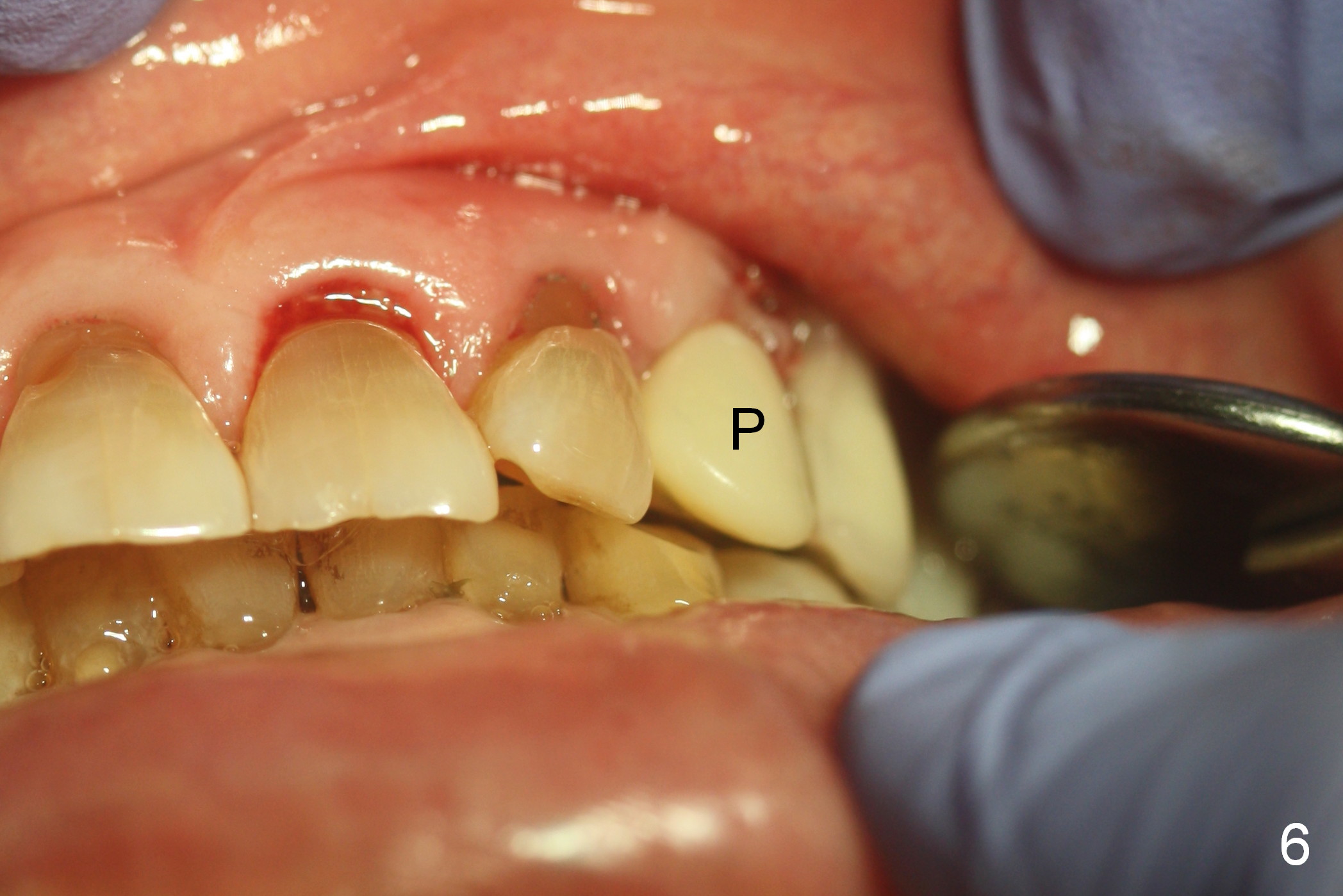
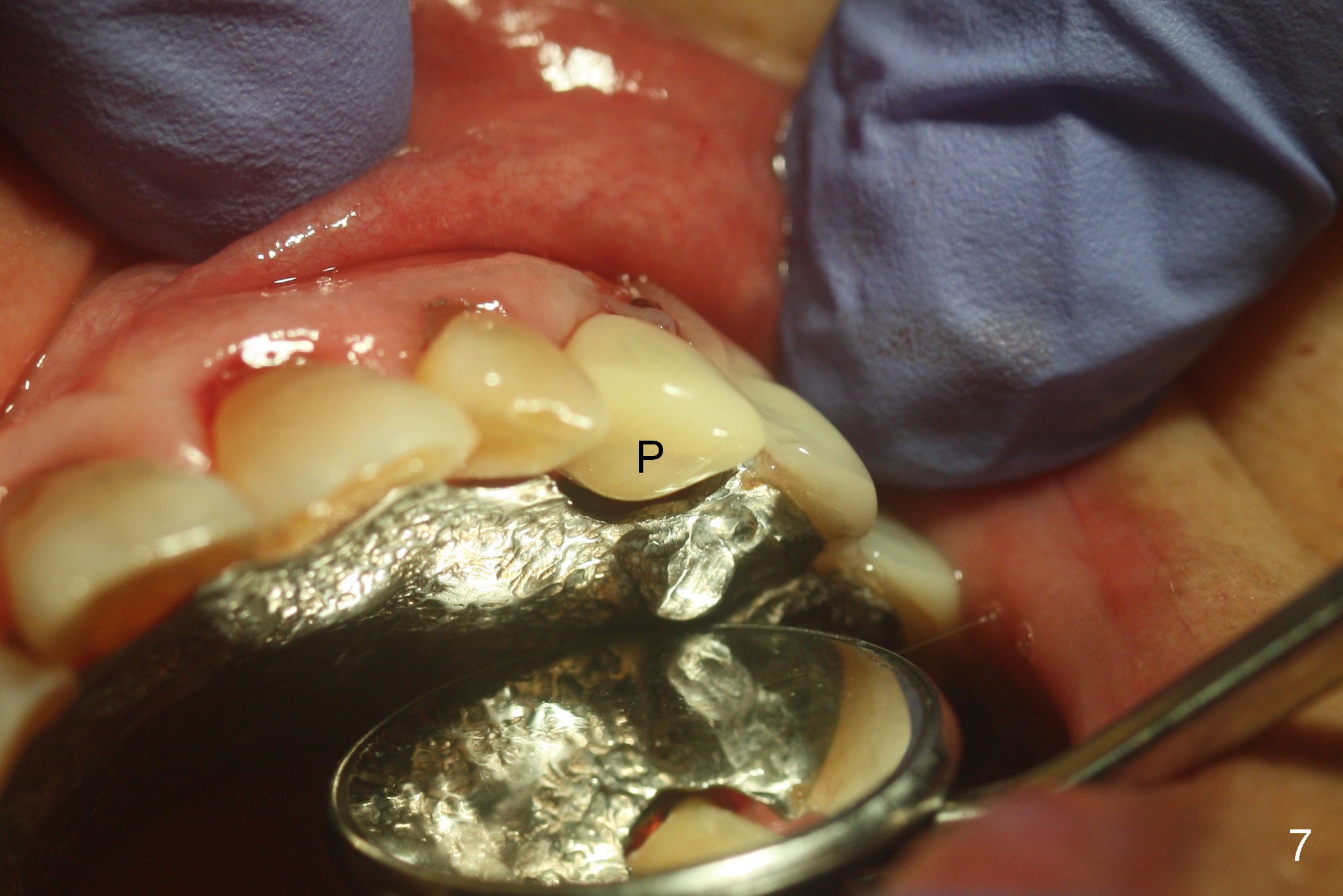
The provisional (Fig.6,7 P) has clearances from the opposing dentition and removable partial denture (RPD).
The implant is dislodged within a month postop. A 4.5 or 5x18 mm 2-piece or 3.5x23 mm 1-piece implant will be placed. No or small provisional will be fabricated. Make sure that there is no any possible contact when the partial denture is worn. In fact, there is more occlusal contact when the RPD is not worn. Advice the patient for soft food.
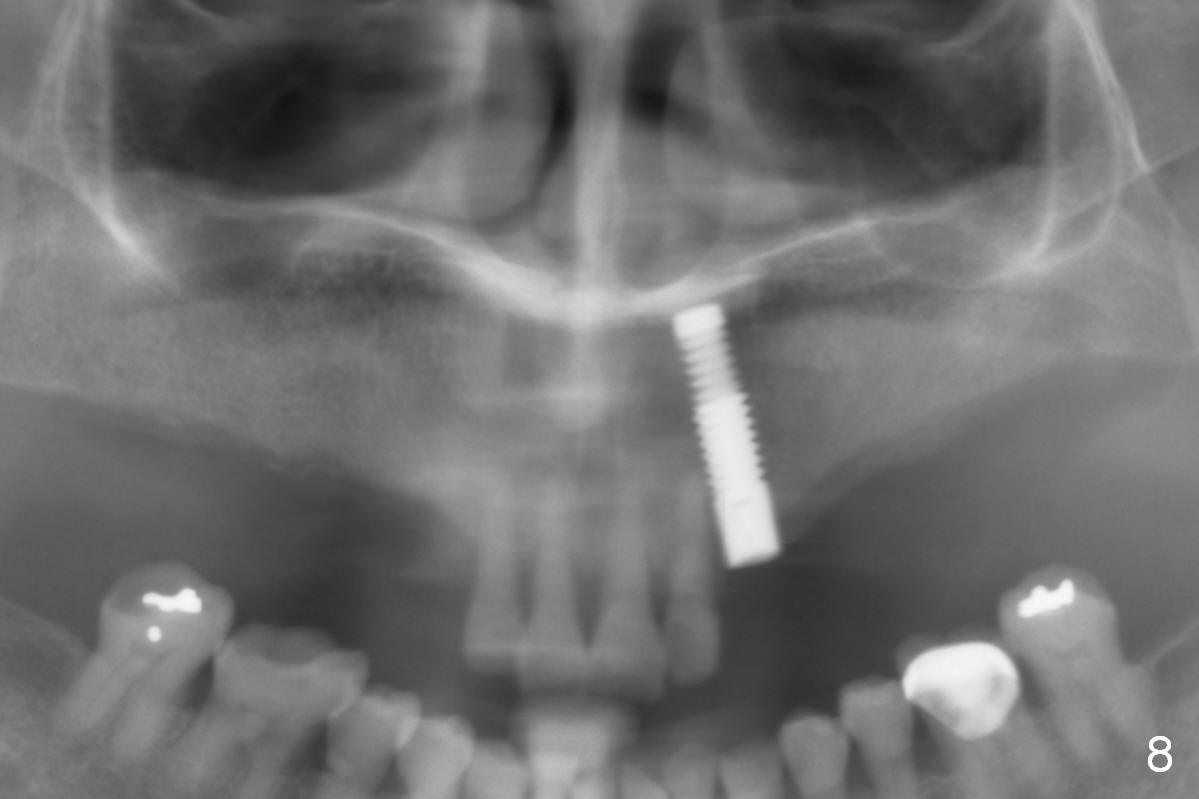
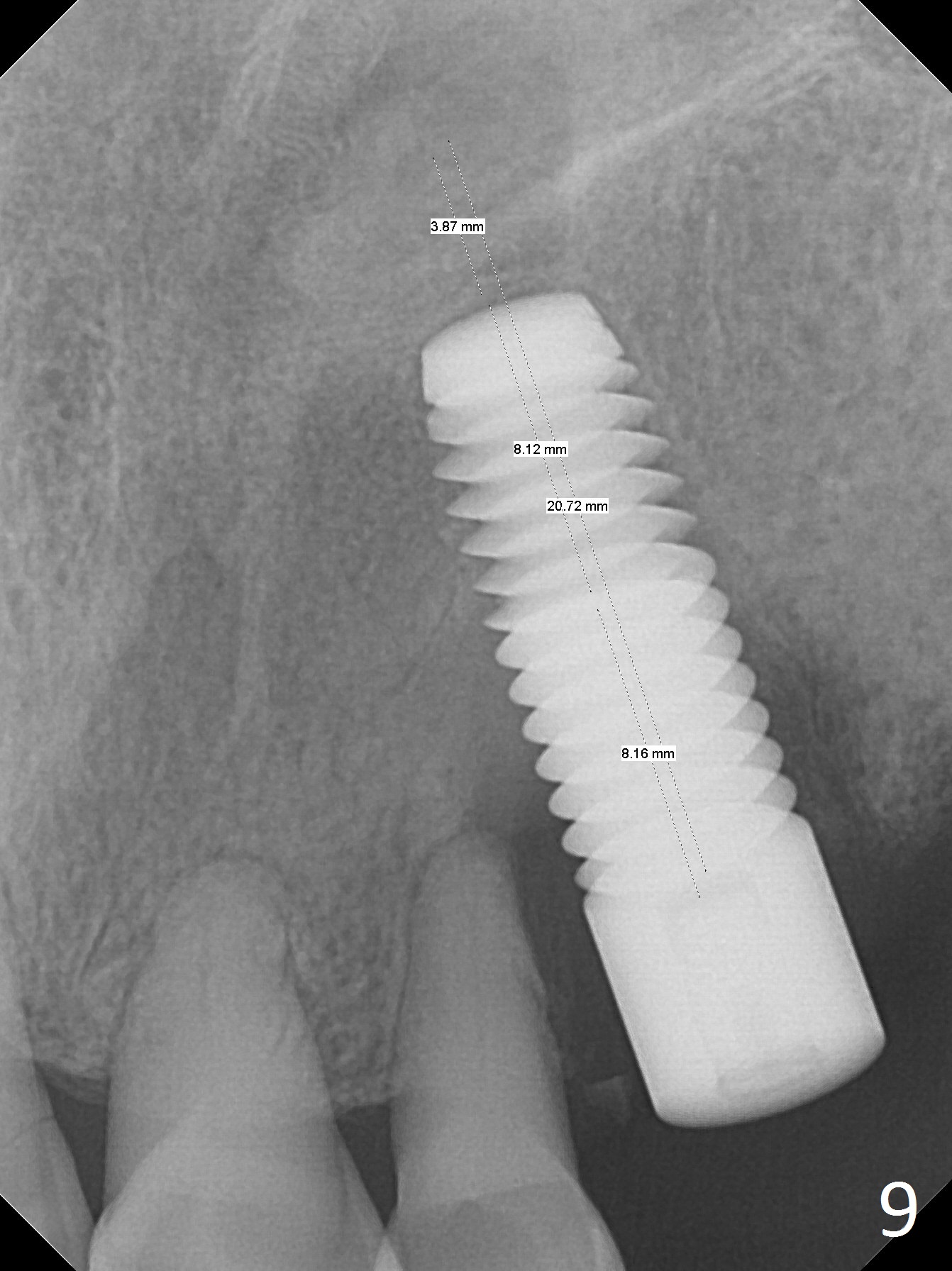
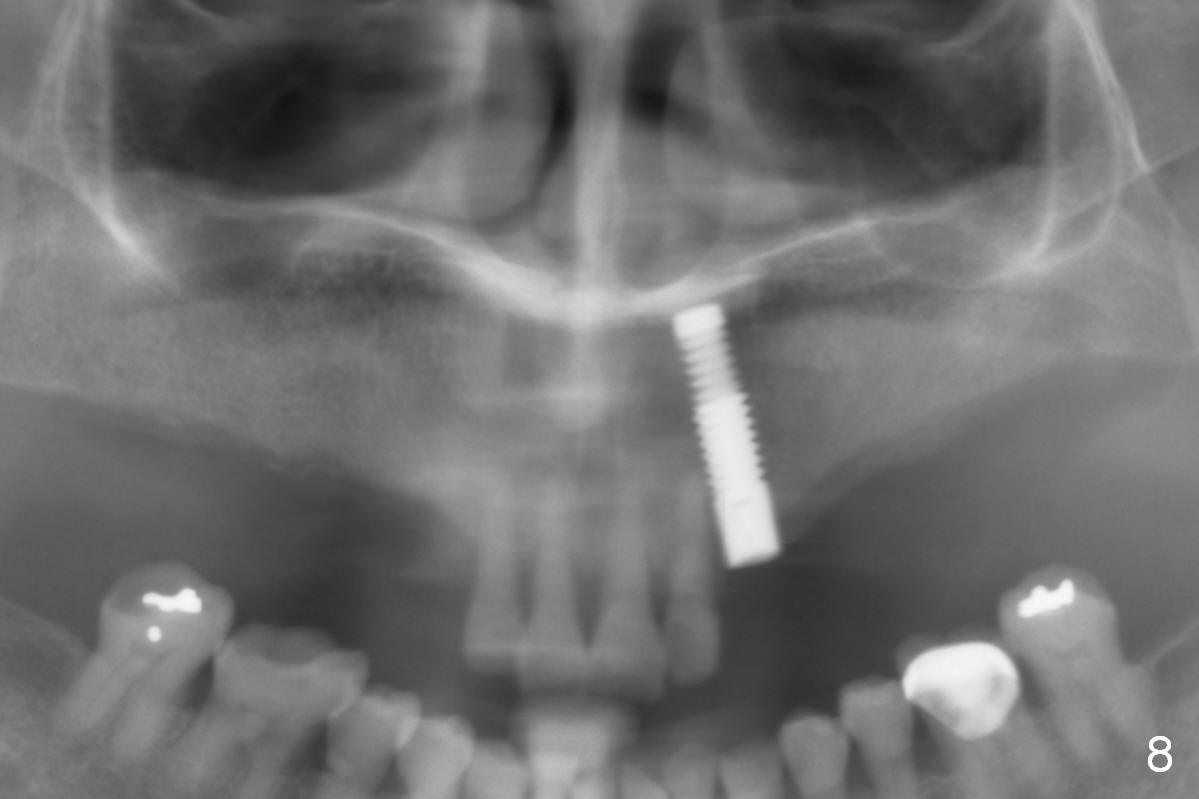
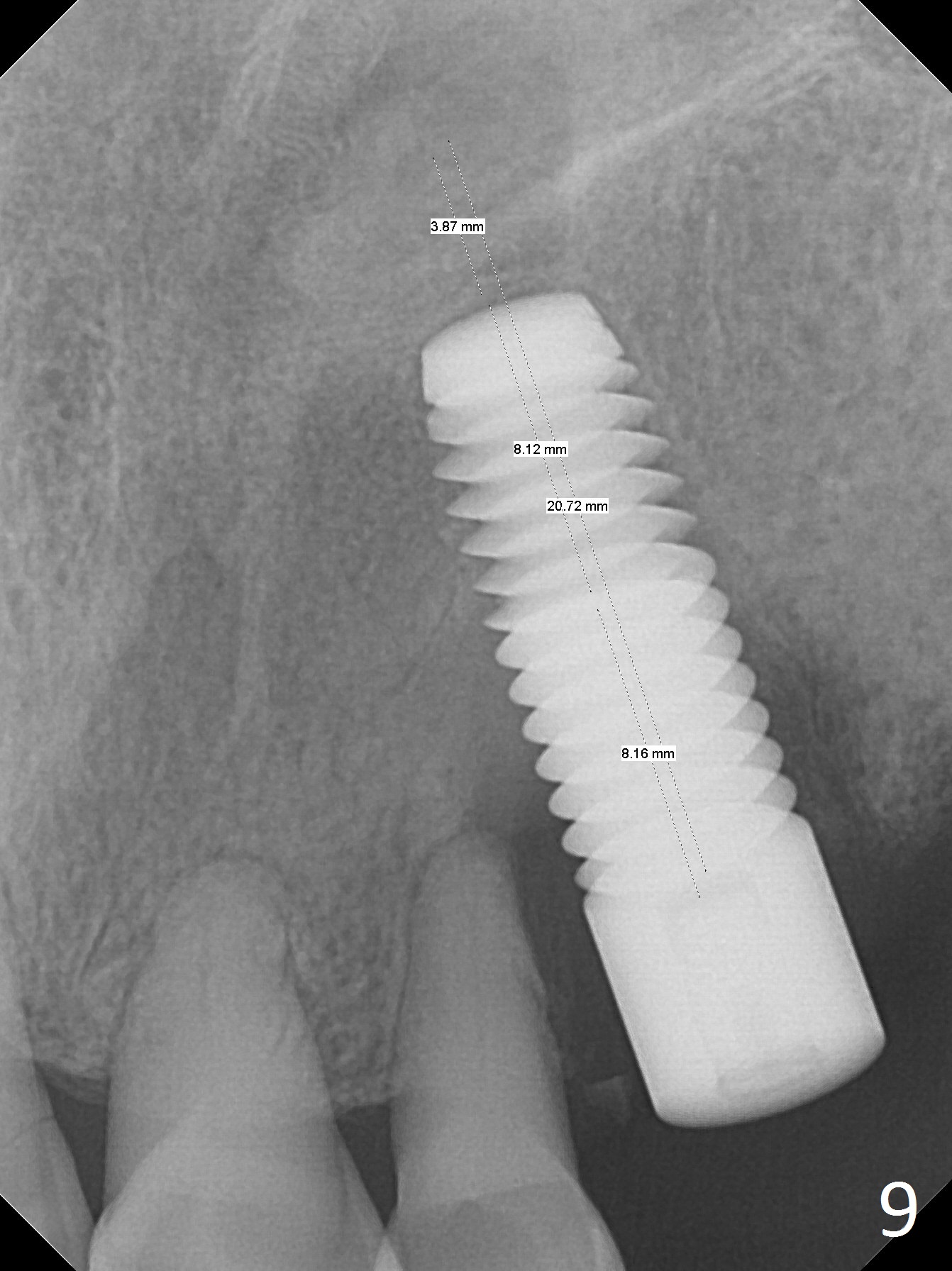
In fact a 6x20 mm tissue-level cylindrical implant is placed with insertion torque <15 Ncm (Fig.8). The palatal margin of the implant has to be trimmed to get ~ 1 mm clearance from the lower canine when the partial is not worn. Overbite increases when the partial is on. The bone is soft due to her age and being a vegetarian. She eats nuts. When the implant is being placed, the labial and palatal plates feel thin and vibrating.
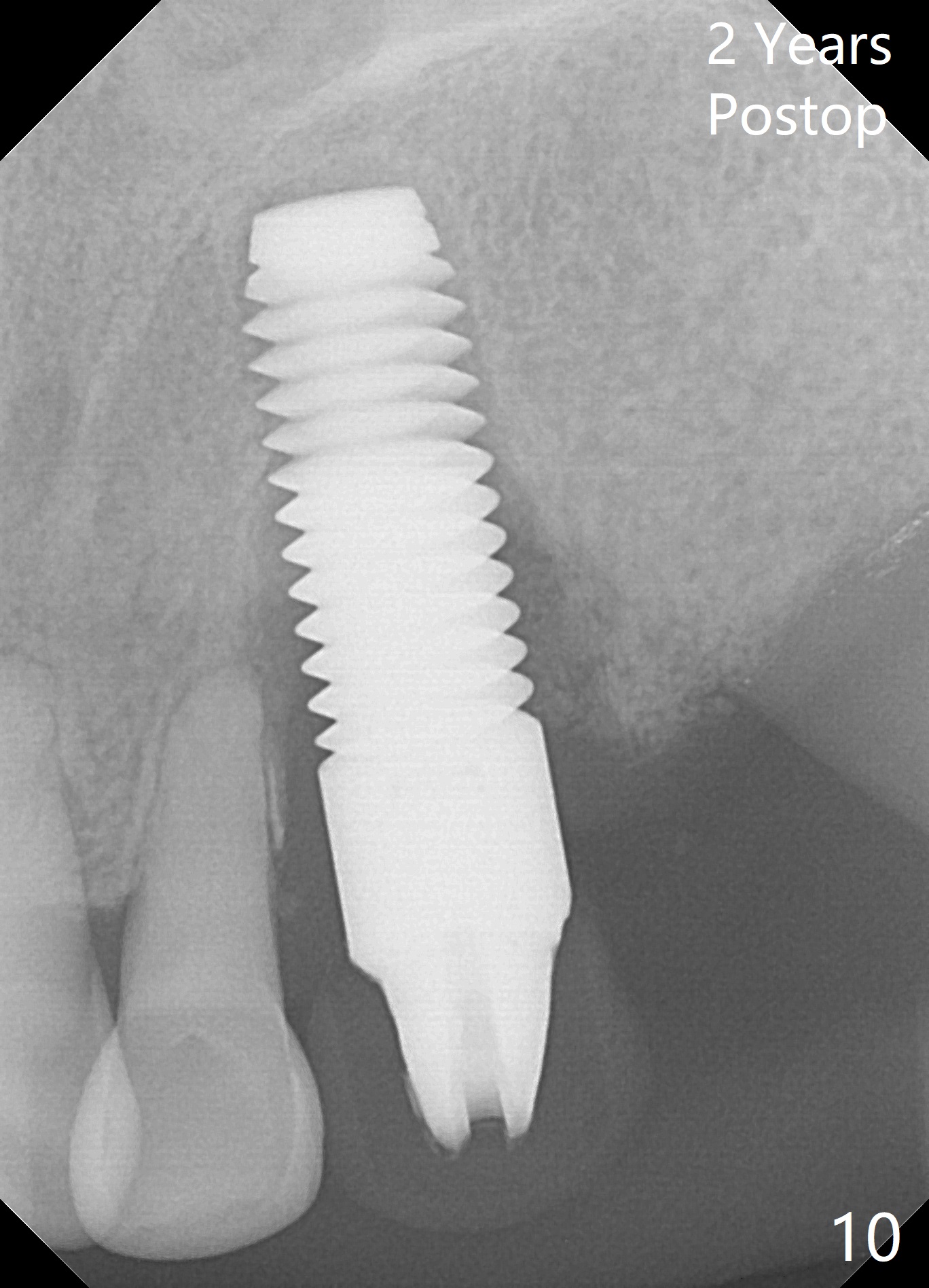
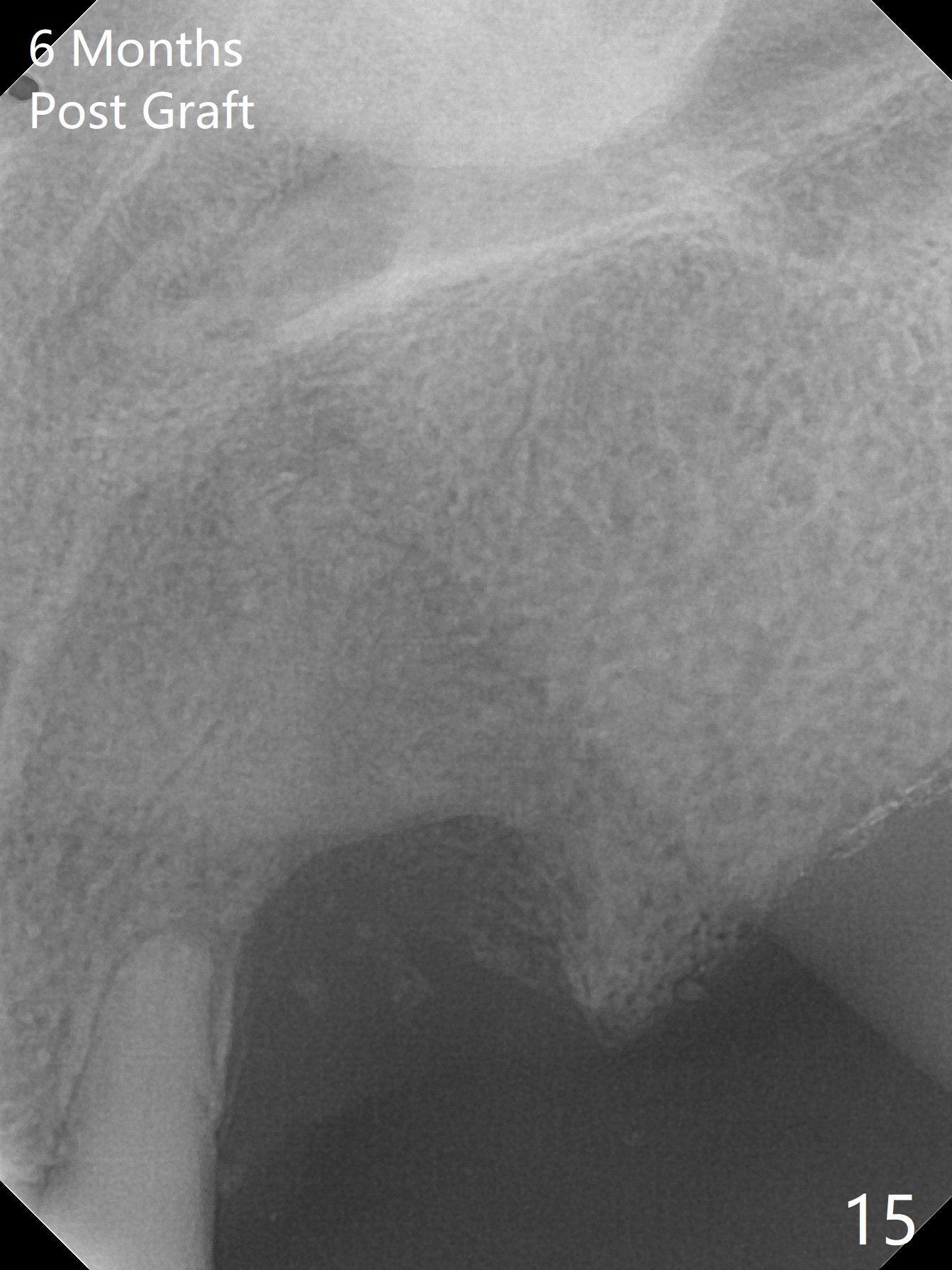
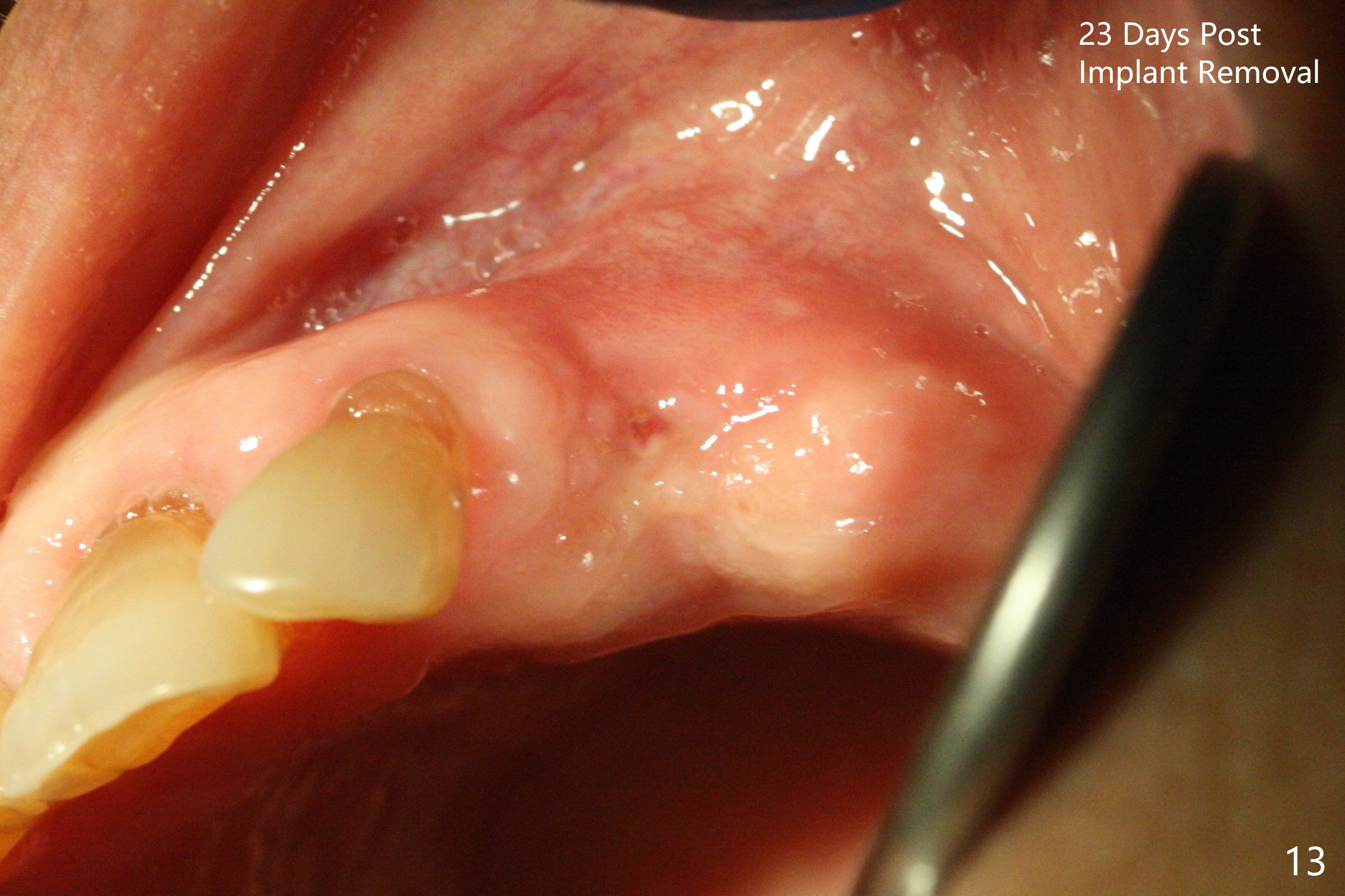
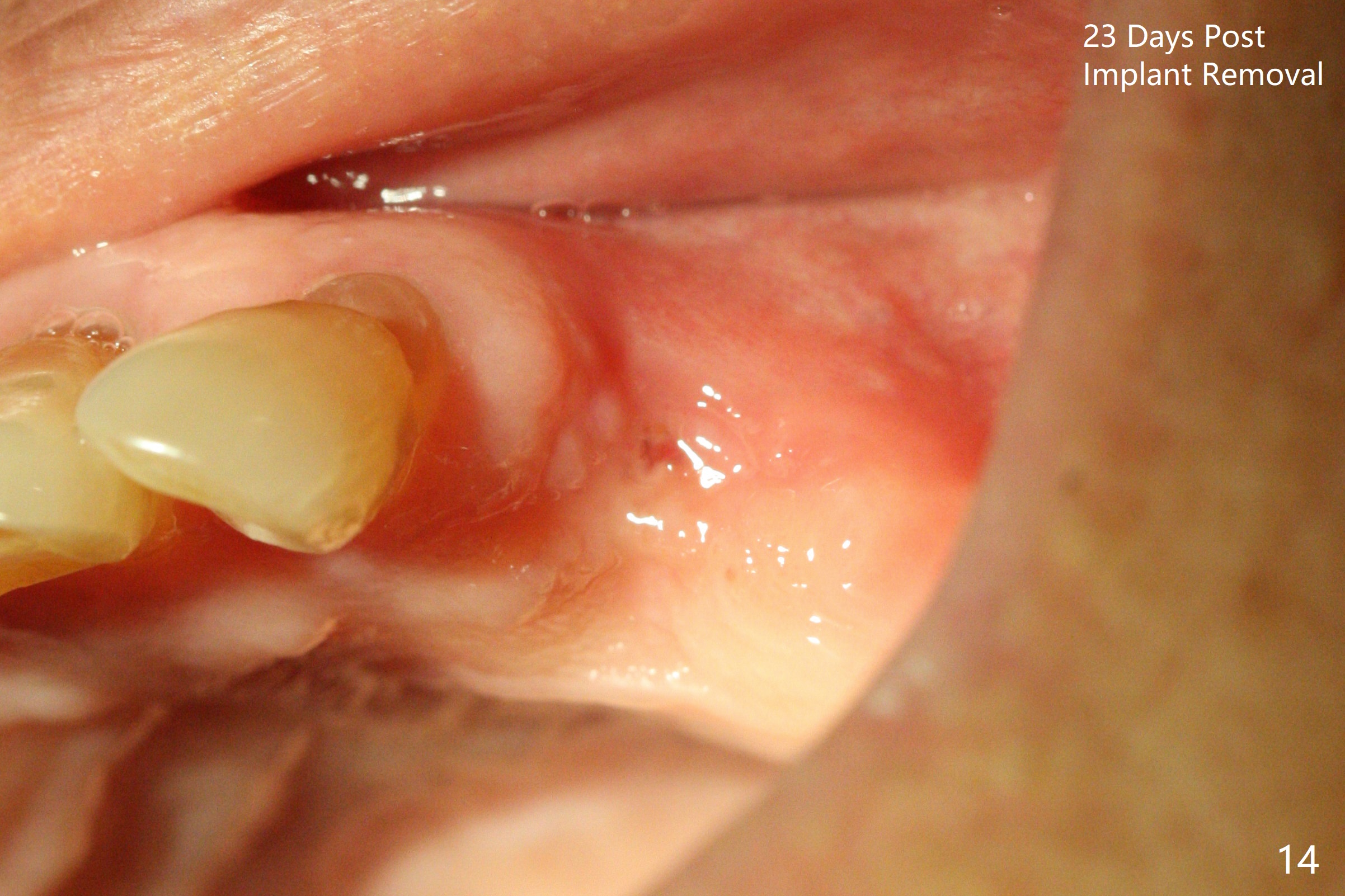
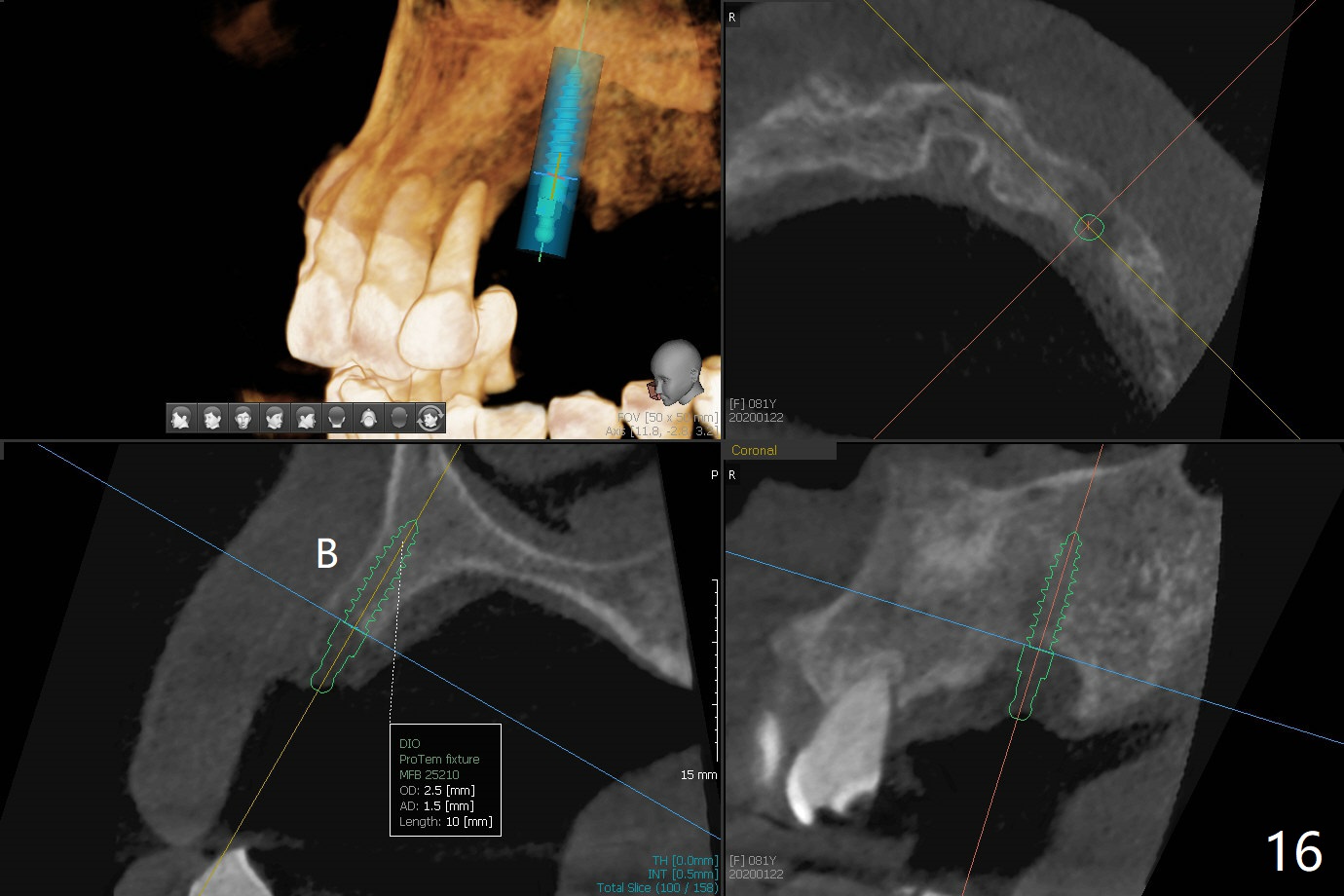
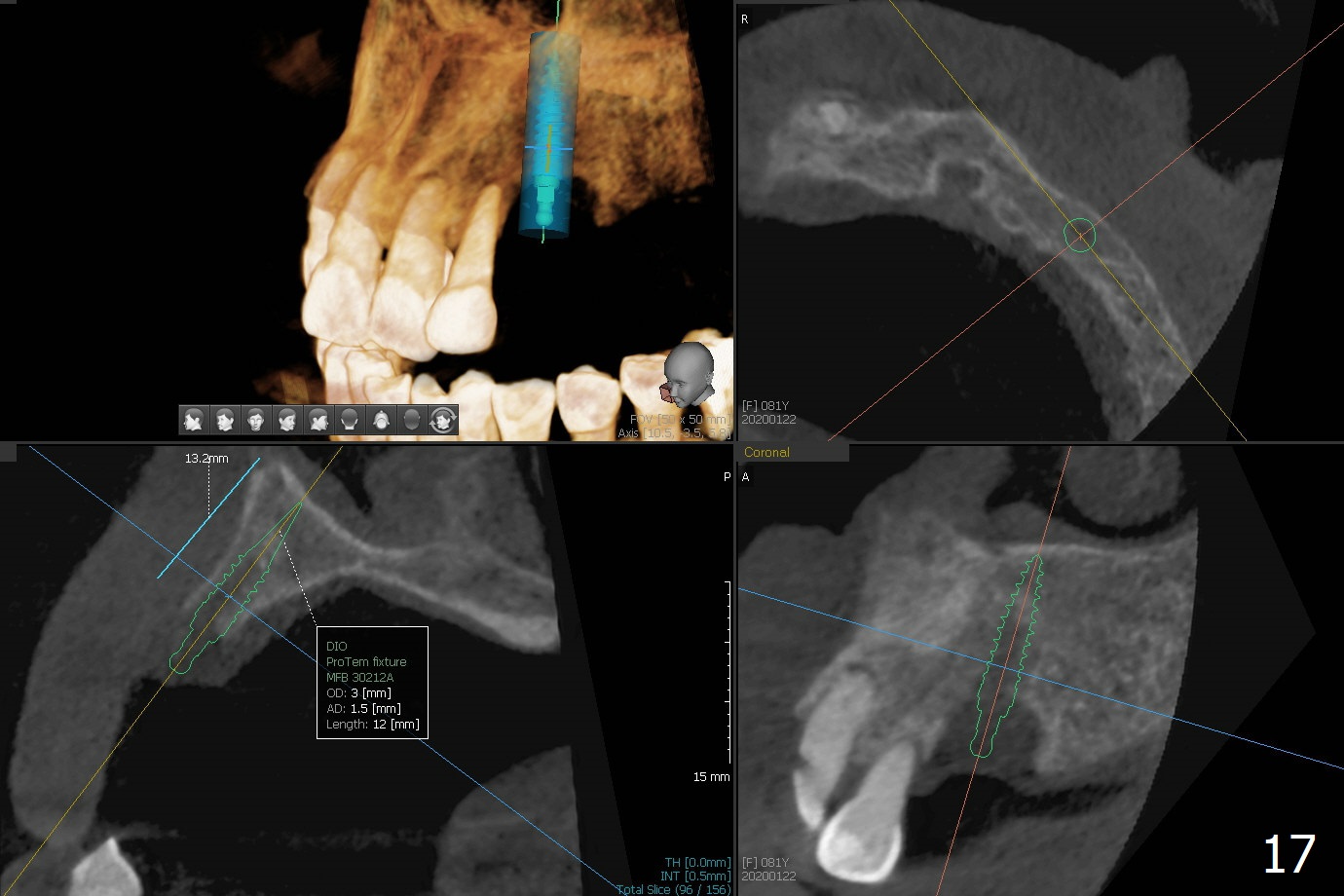
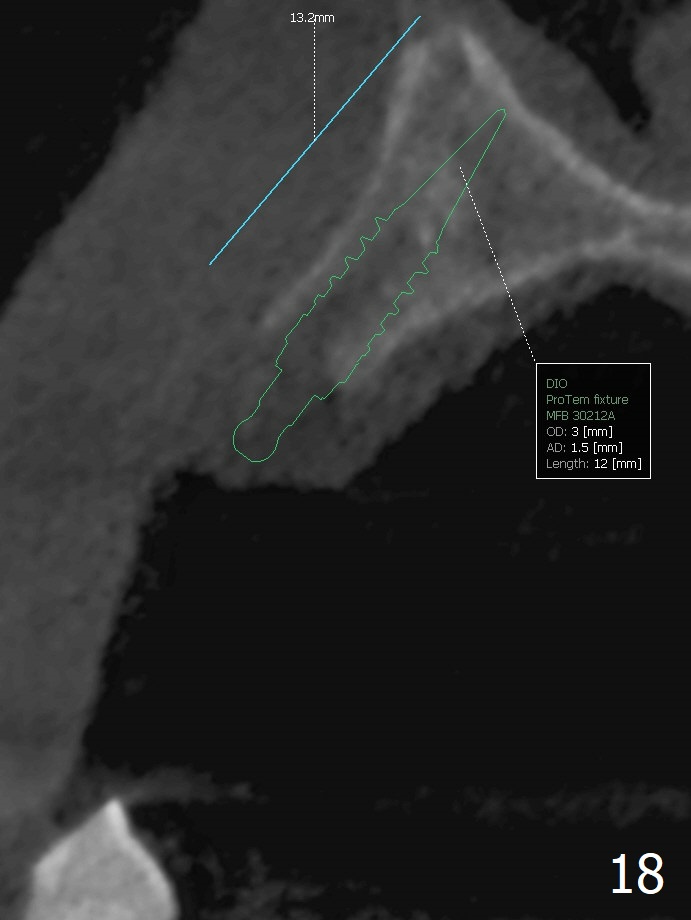
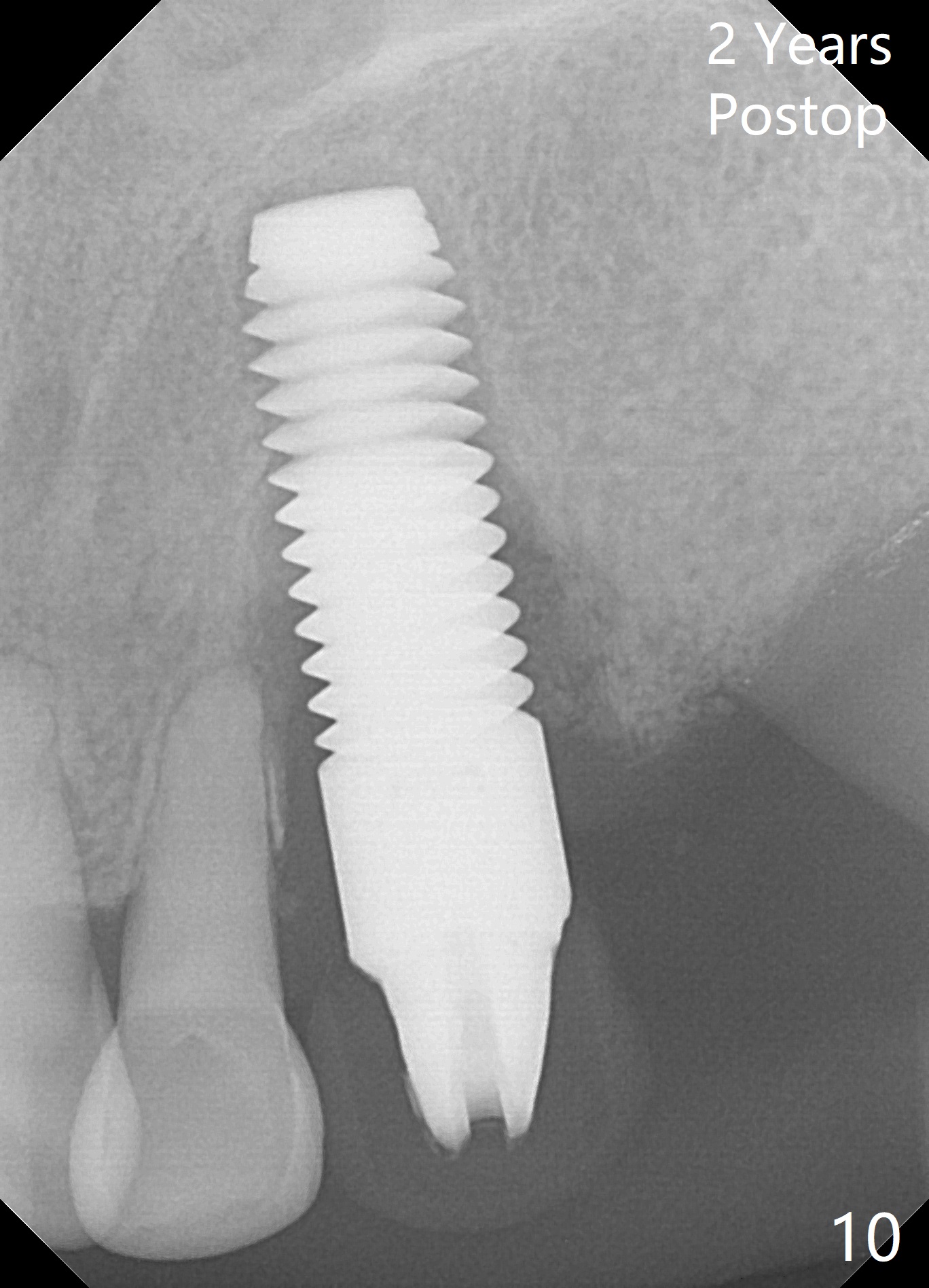
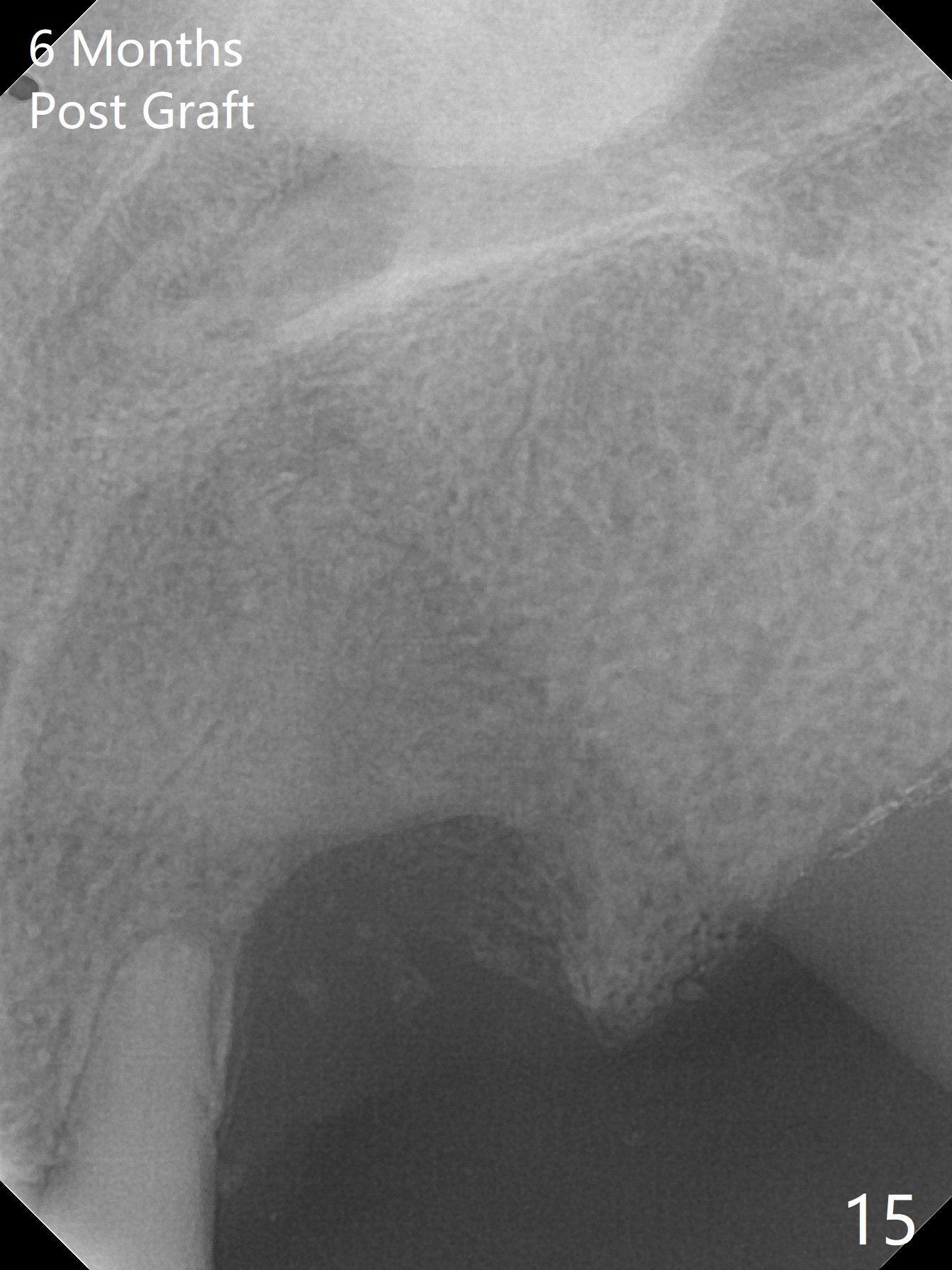
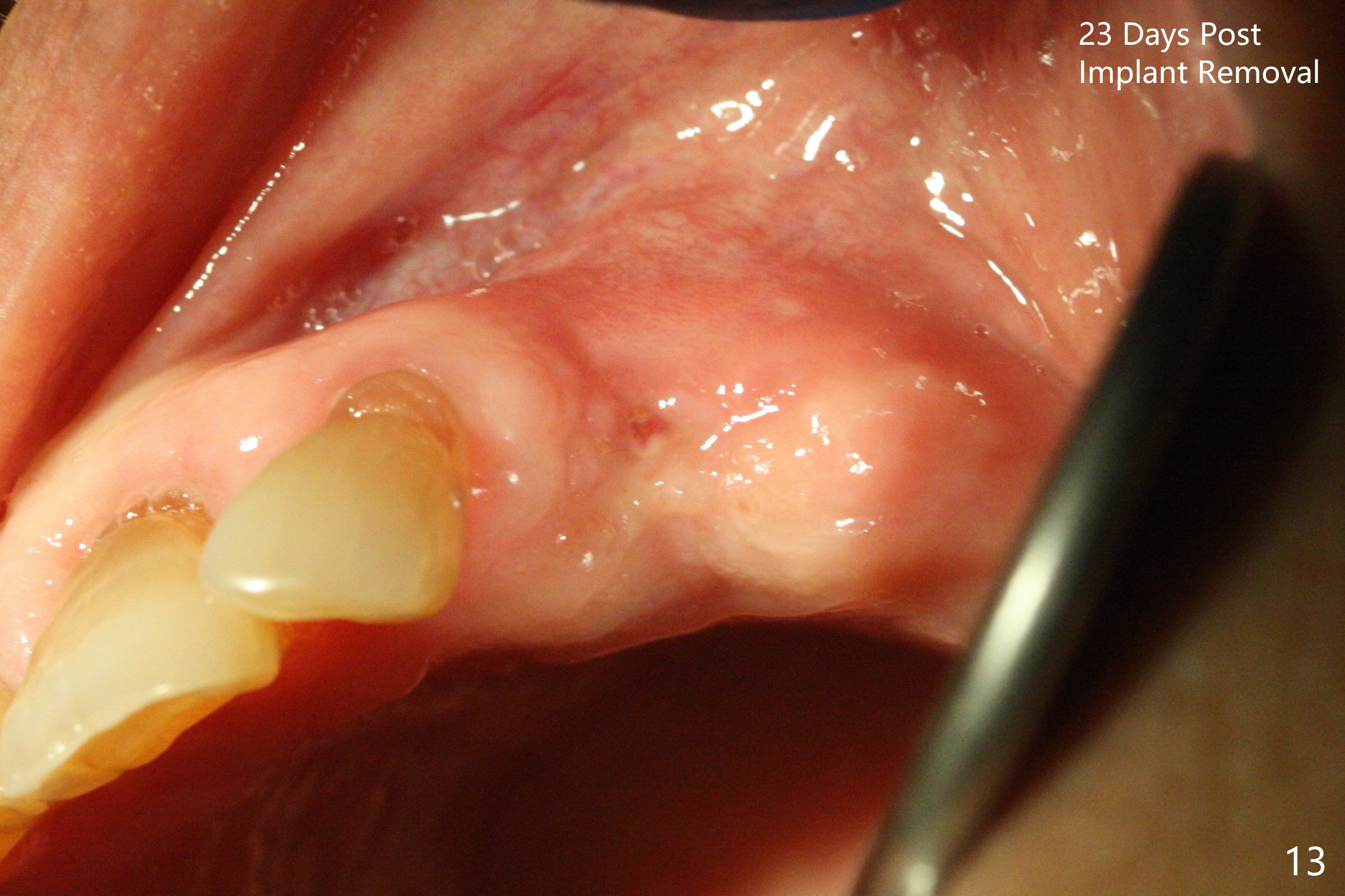
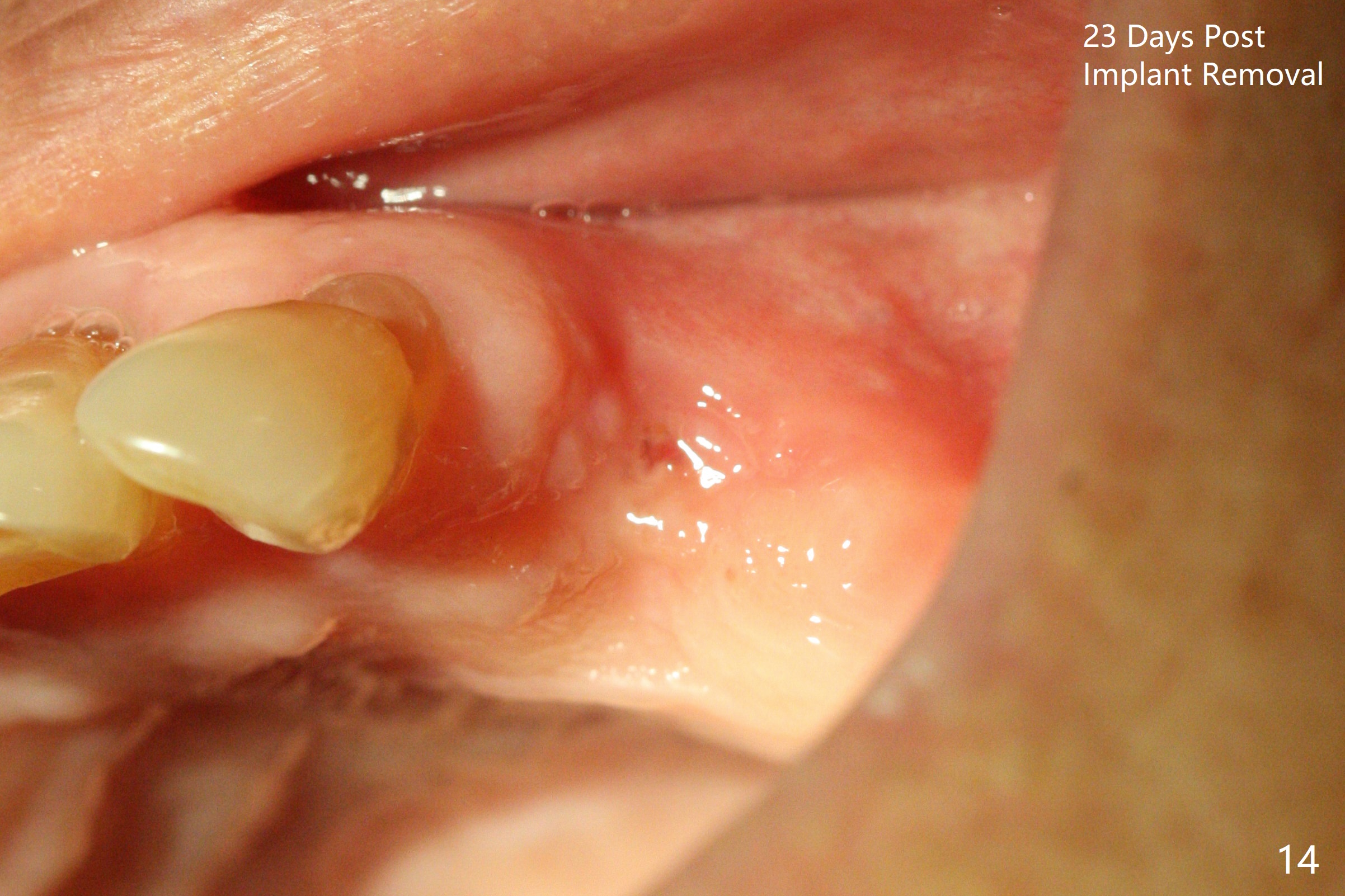
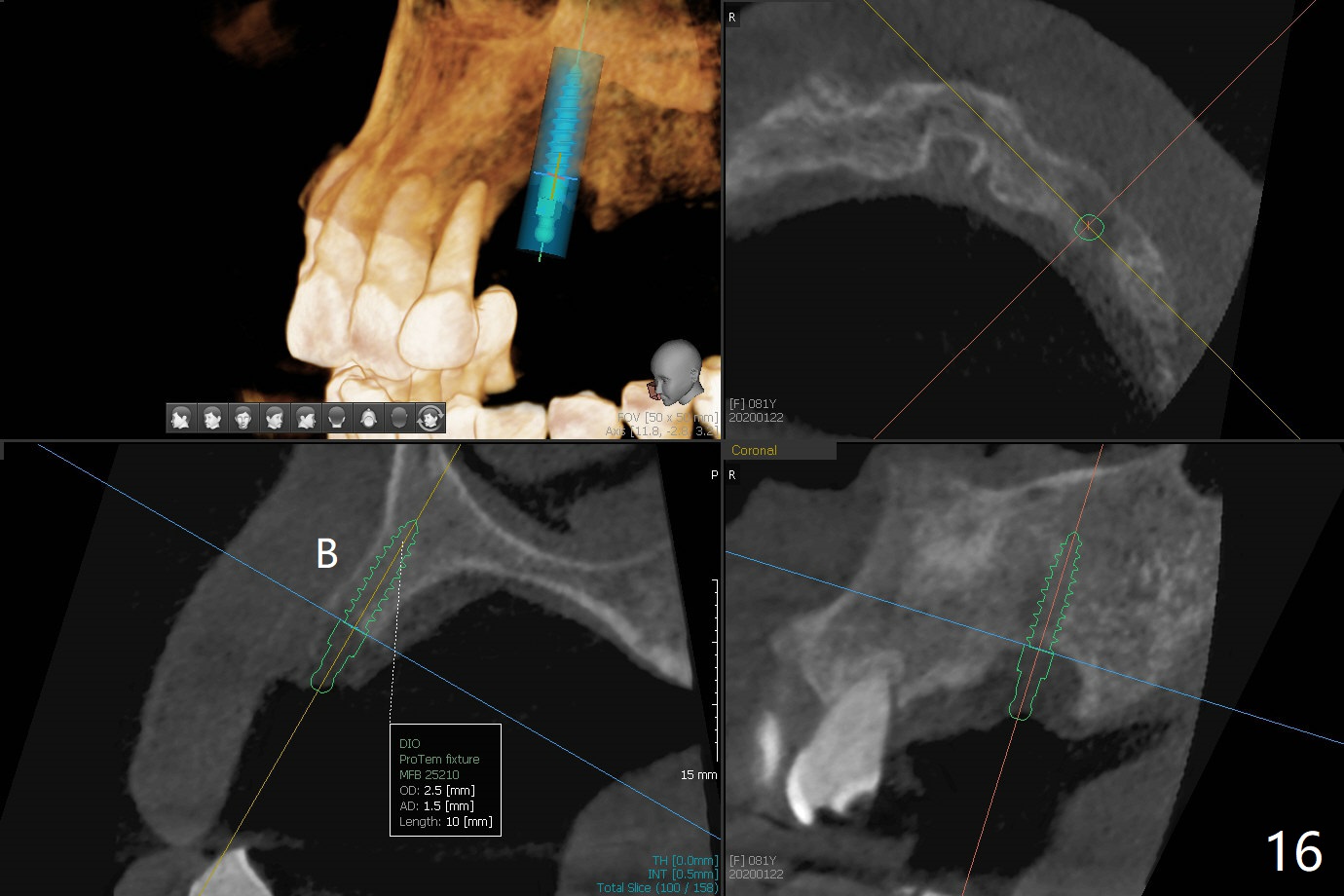
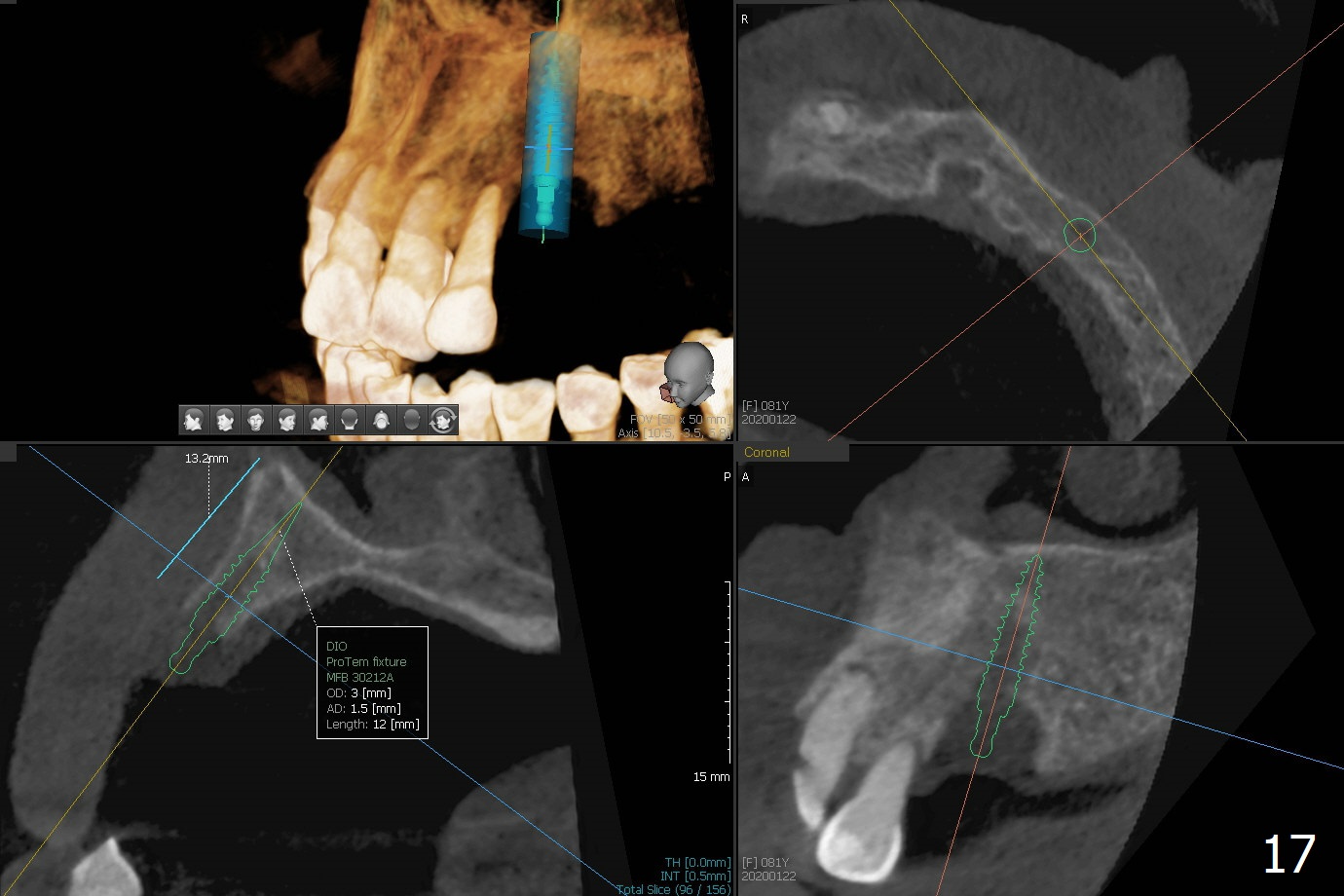
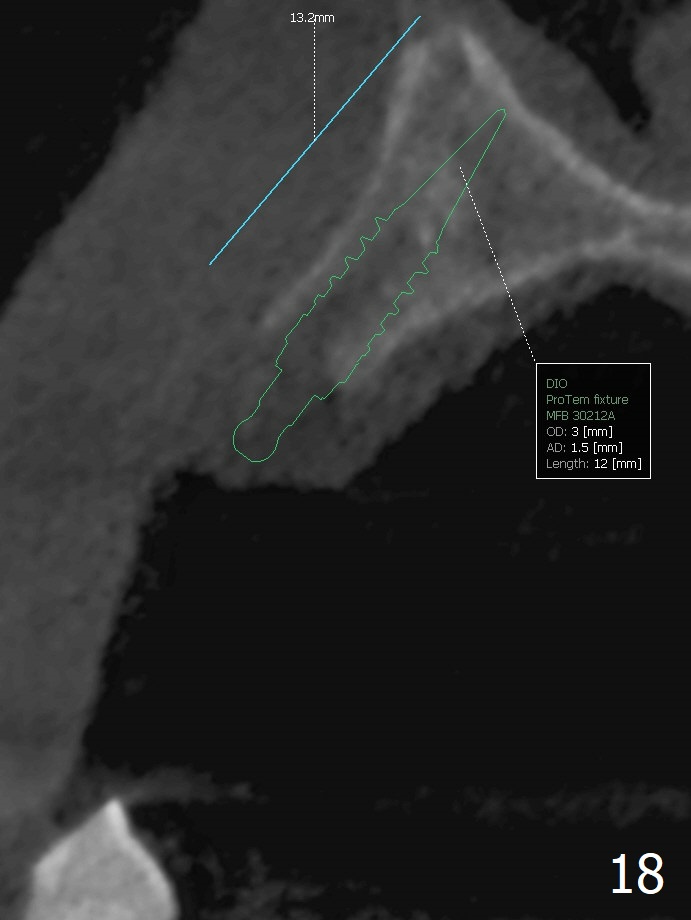
The implant has mobility 4 months postop. Now it is nearly 9 months postop. The patient is eager to return to have the implant restored, since her RPD is loose. The palatal gingiva is erythematous. PA shows severe bone loss. The implant is unstable, but the patient refuses to remove the implant. An abutment is placed for a provisional to stabilize the RPD. If the implant proves to be a failure, place a 3.0 or 3.5x23 mm 1-piece implant. The patient returns 2 years postop (Fig.10); the implant remains unstable, although the provisional is functional. She is receiving venous injection of osteoporosis medicine every month. The provisional is broken 3 years postop; the implant remains mobile. The patient agrees implant removal and bone graft (Fig.11,12). The next implant will be buried. The buccal plate of the healing site seems to have collapsed 23 days post implant removal (Fig.13,14). The future surgery will be guided with incision (palatal for the keratinized gingiva) so that the wound will be closed. The ridge is narrow 6 months postop (Fig.15). A 2.5 mm 1-piece implant with ball abutment will be placed (Fig.16). In fact a 3x13 mm 2-piece IBS implant is better so that it can be buried (Fig.17,18).
Return to
Upper
Canine Immediate Implant,
IBS Improvement
Trajectory
II
No Deviation
Xin Wei, DDS, PhD, MS 1st edition 06/27/2016, last revision 02/19/2020