

 |
 |
|
 |
 |
  |
 |
 |
|
Close Extraction Gaps with Allograft
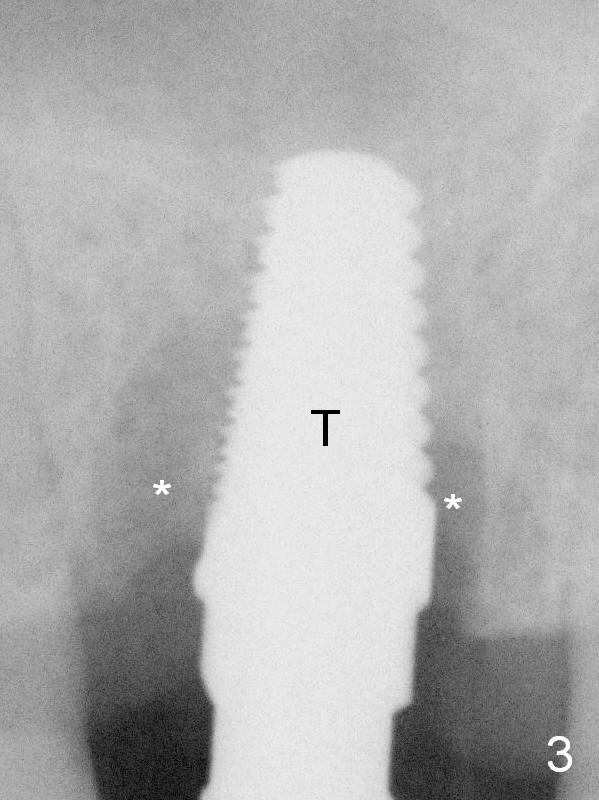
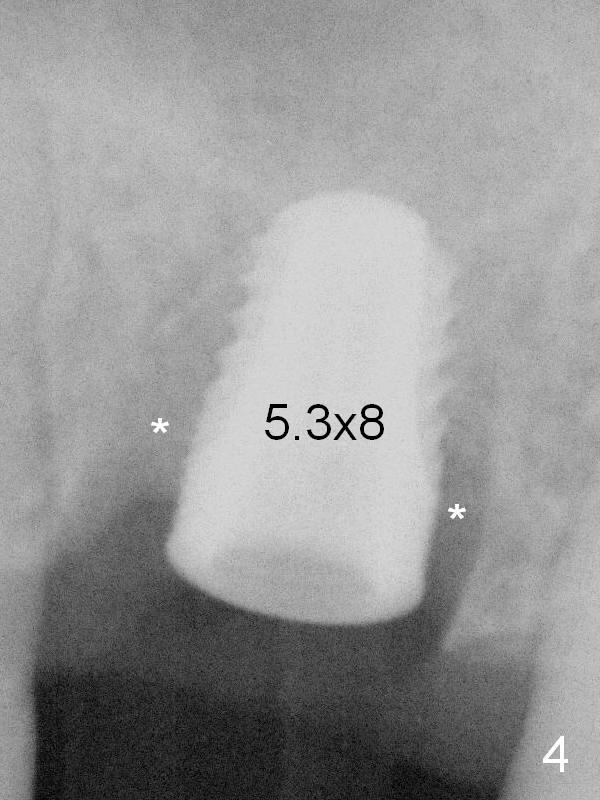
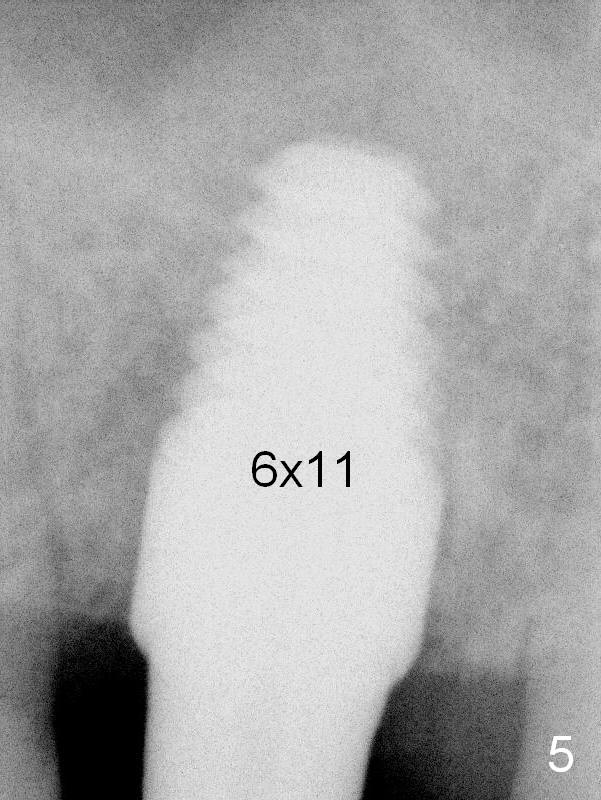
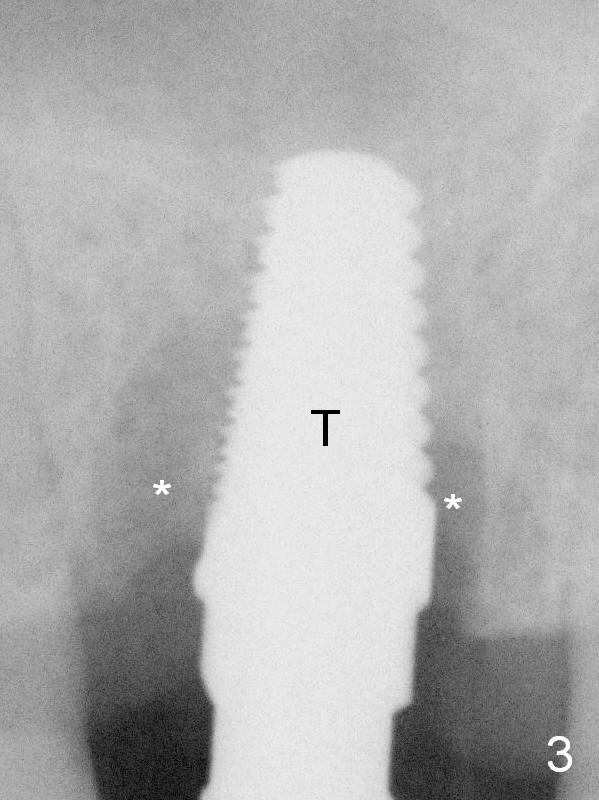
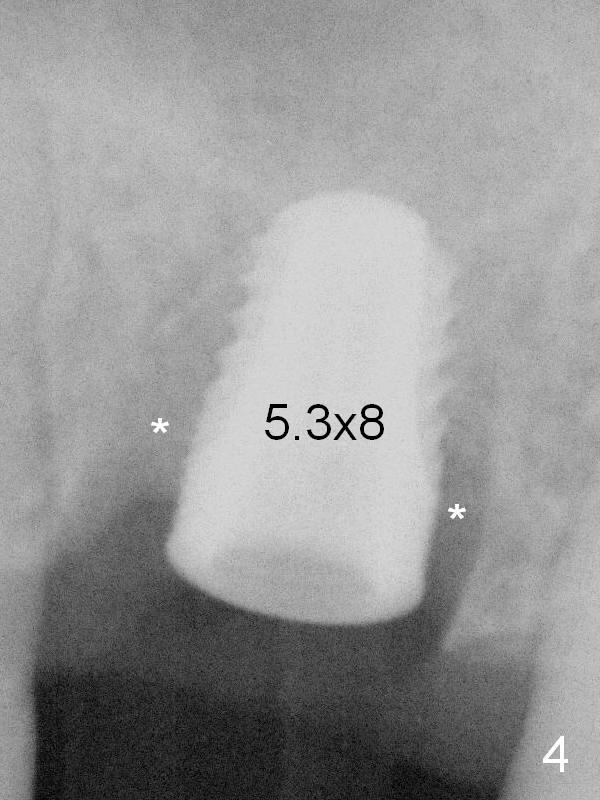
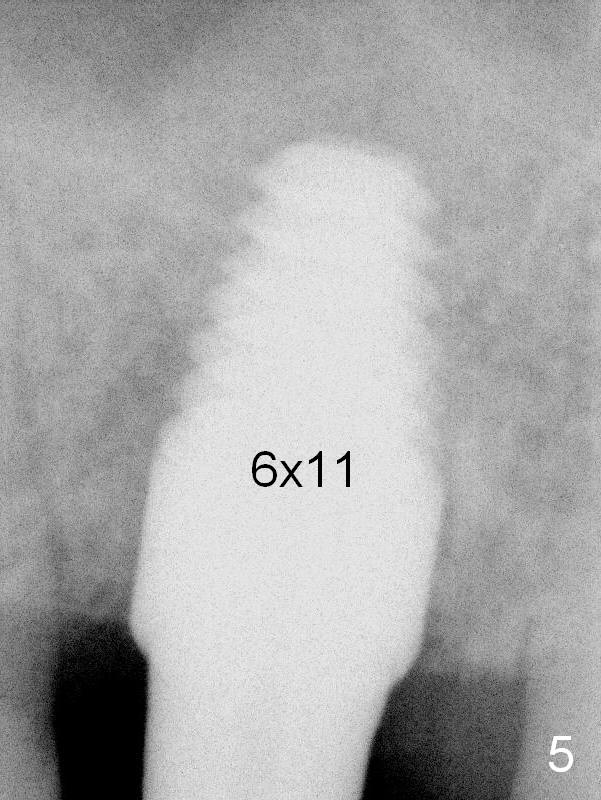
There are extensive defects involving the tooth #14 buccally (Fig.1) and lingually (Fig.2 subgingival fracture:*). The tooth is extracted by sectioning. There appears no apical infection, although there is minor palatal apical perforation. Osteotomy is initiated in the middle of the septum using Sinus Master Kit. Miscalculation leads to sinus membrane perforation, which is repaired by inserting Osteogen plug. Osteotomy is further enlarged with tissue-level taps (4.5 and 5 mm). The latter achieves stability (Fig.3 T). A 5.3x8 mm implant cannot be seated completely (subcrestal, Fig.4)). Deeper placement of the 5 mm tap results in loosening the implant. After using 6 mm tissue-level tap, the corresponding implant is a little over-seated (Fig.5, insertion torque ~50 Ncm)). With placement of 1-2 mm mineralized cancellous and cortical allograft, the extraction gap (Fig.3,4 *) is obliterated (Fig.5). It may be better to use bone-level tap prior to insertion of the same type of implant. To prevent over seating the tissue-level implant, measure tissue height prior to implantation.
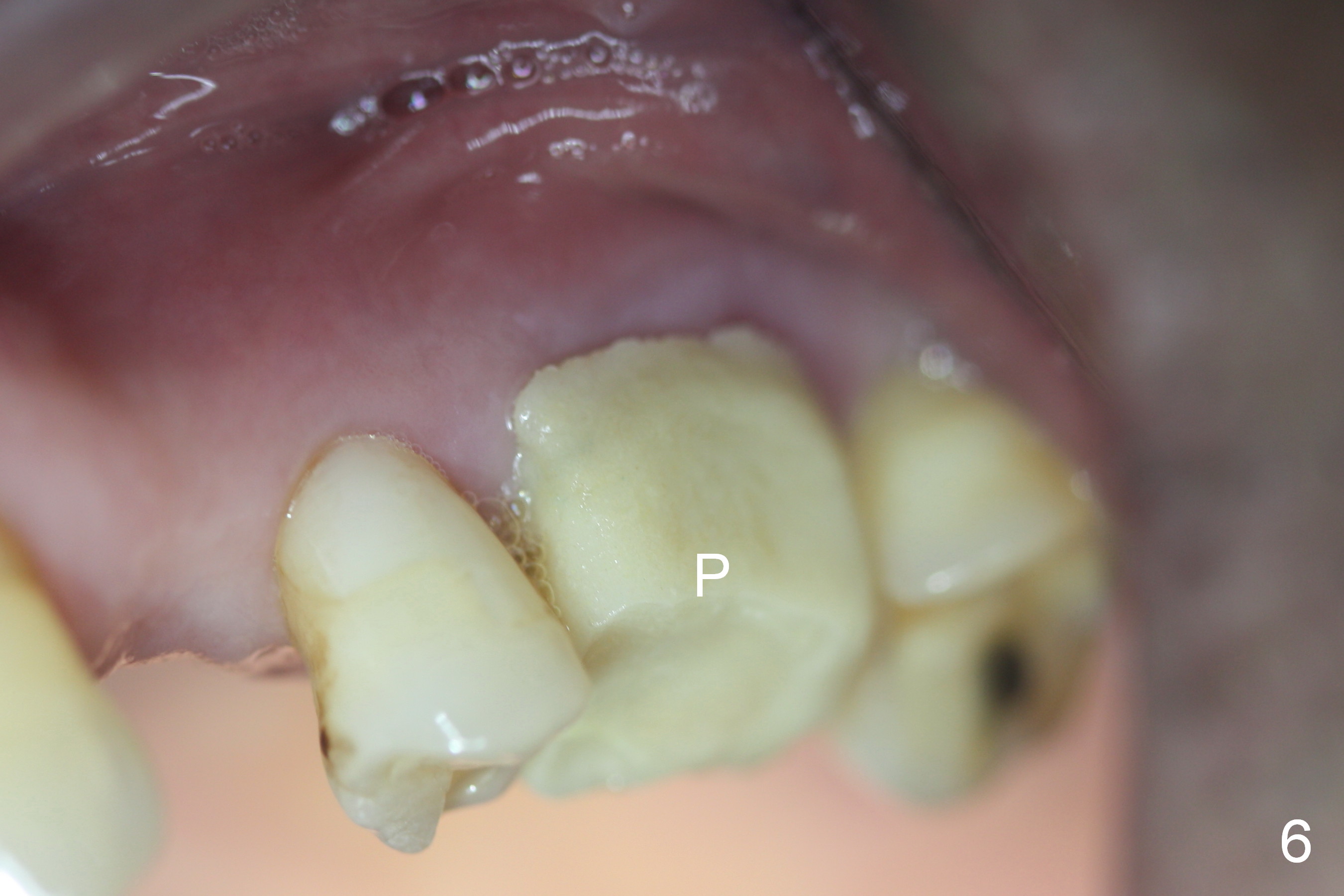
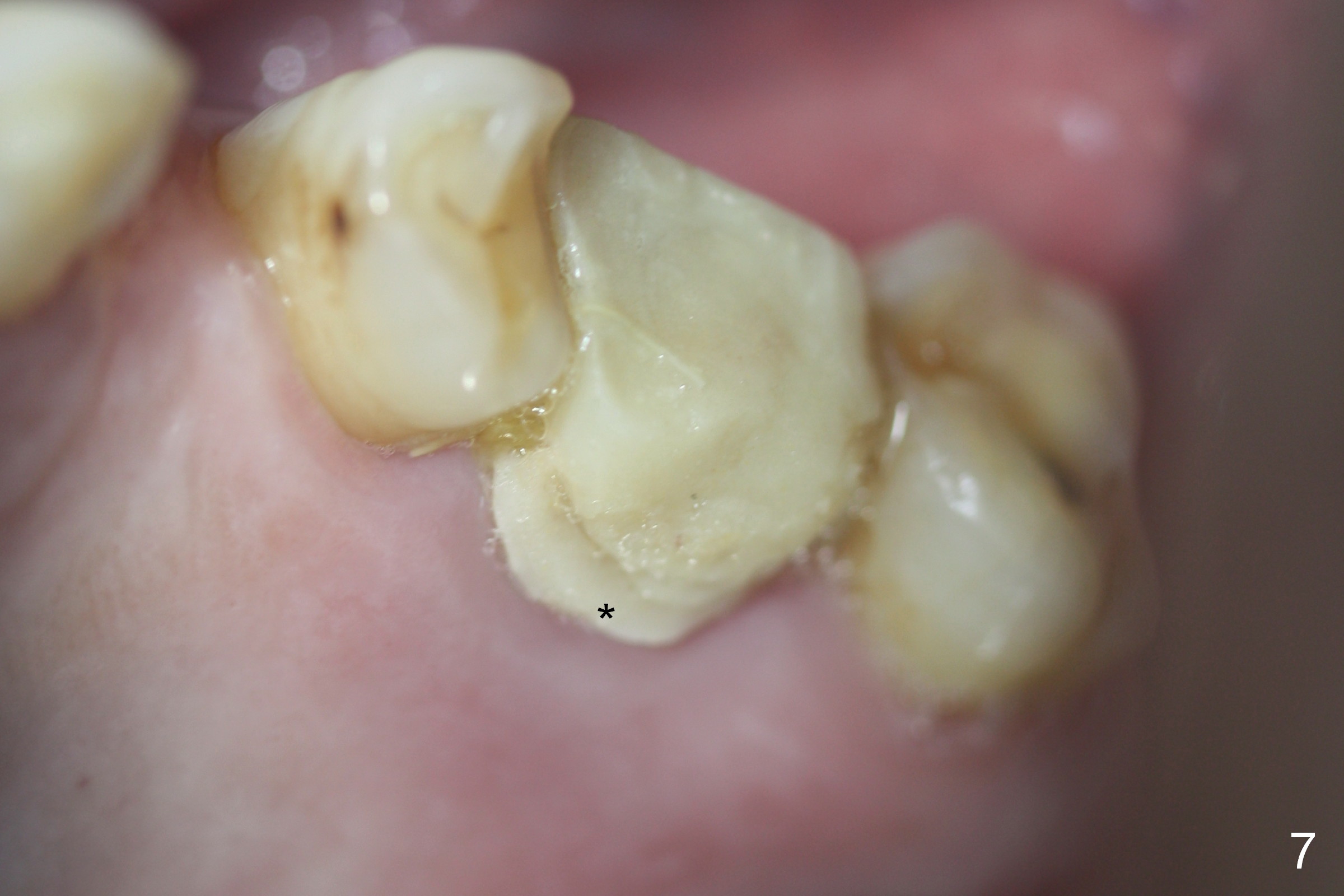
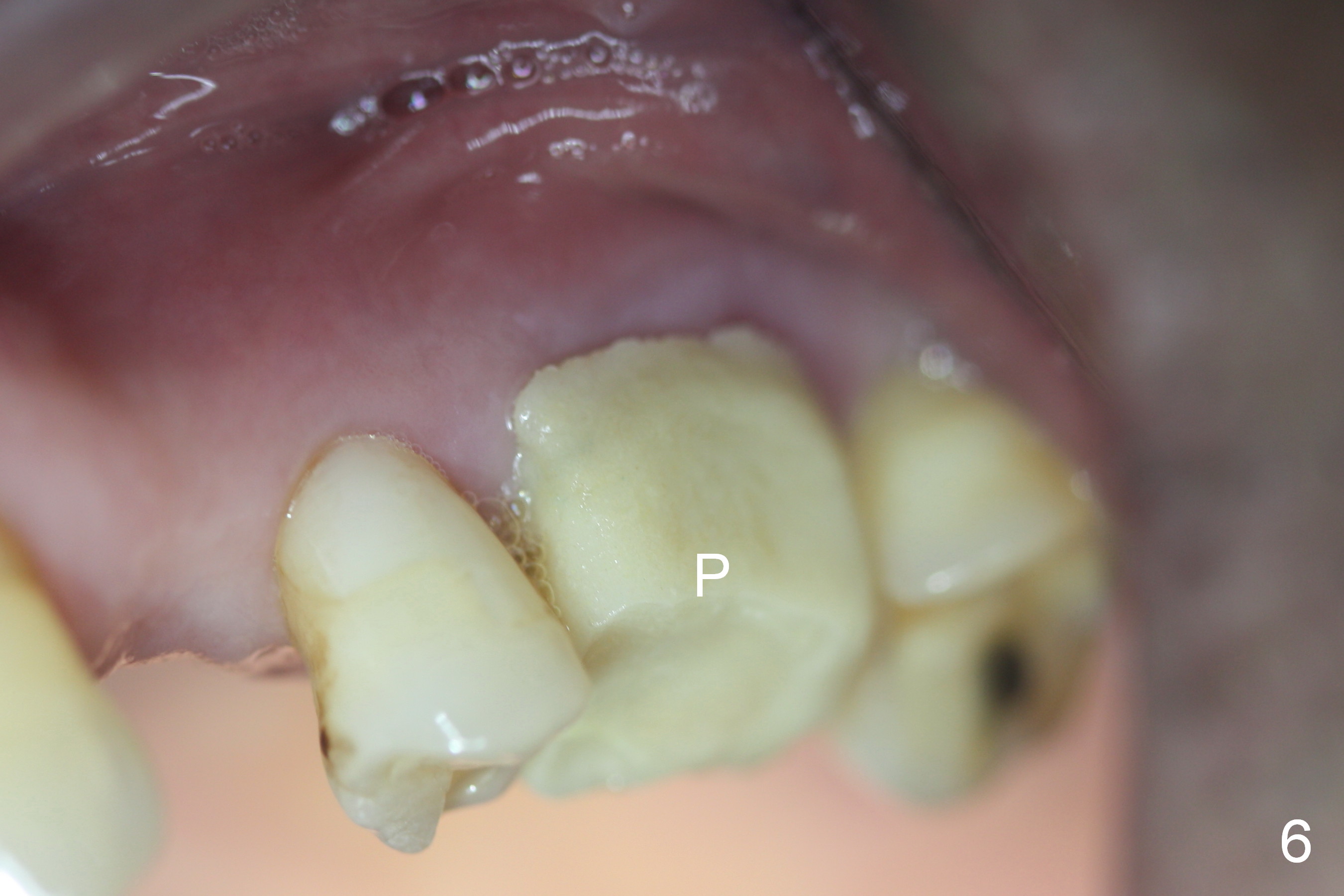
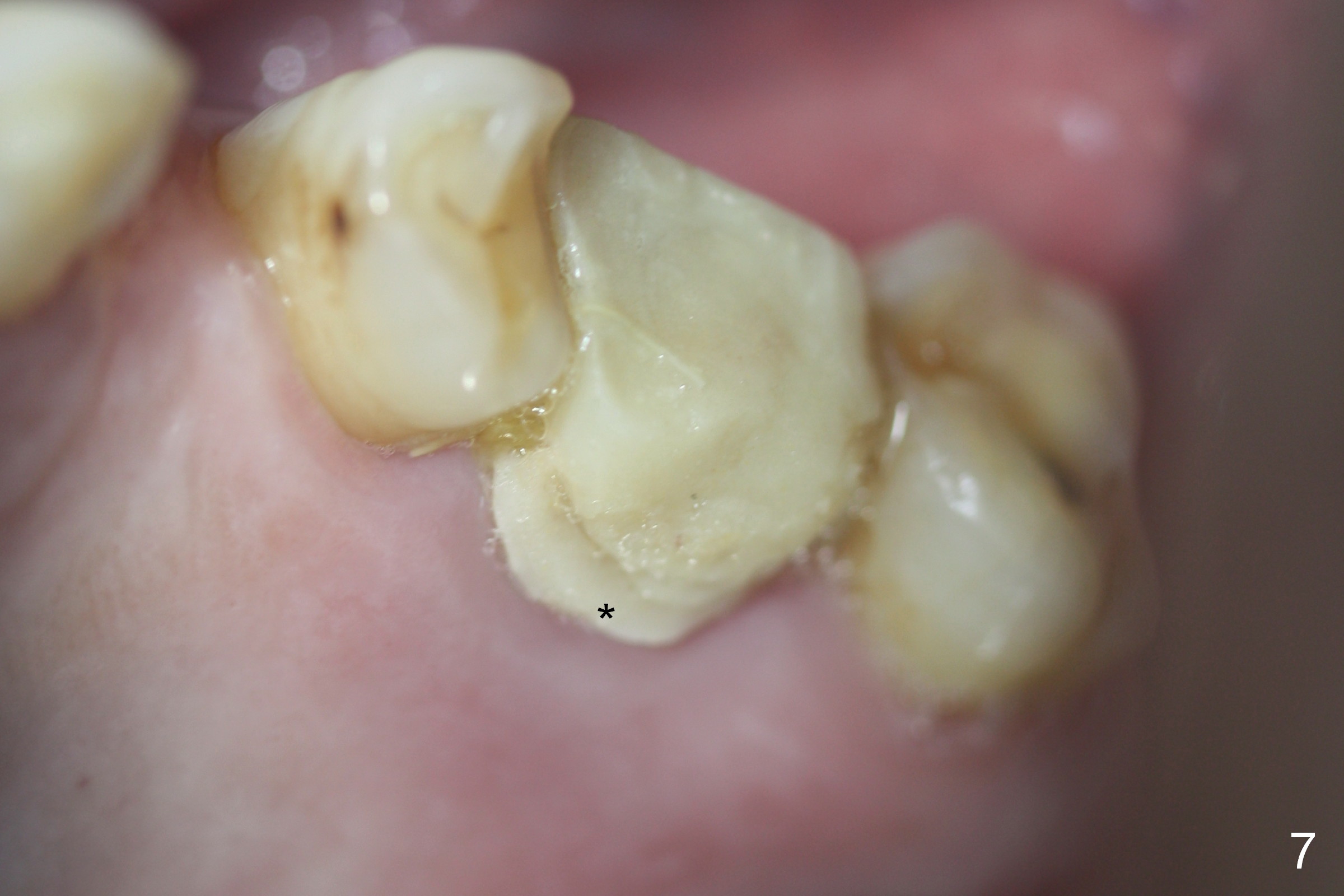
The patient returns 8 days postop (Fig.6,7). The provisional (P) looks rough on surface, especially palatal margin (Fig.7 *). The provisional is trimmed 15 days postop when bone graft is presumably more stable in place than 8 days postop. In fact the socket is healing normally. Seemingly secure provisional may be dislodged in a patient with history of bruxism.
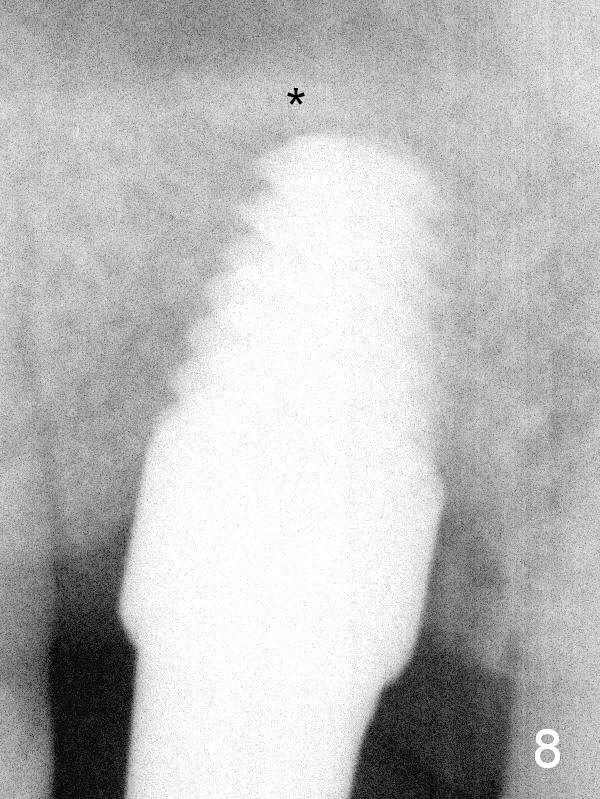
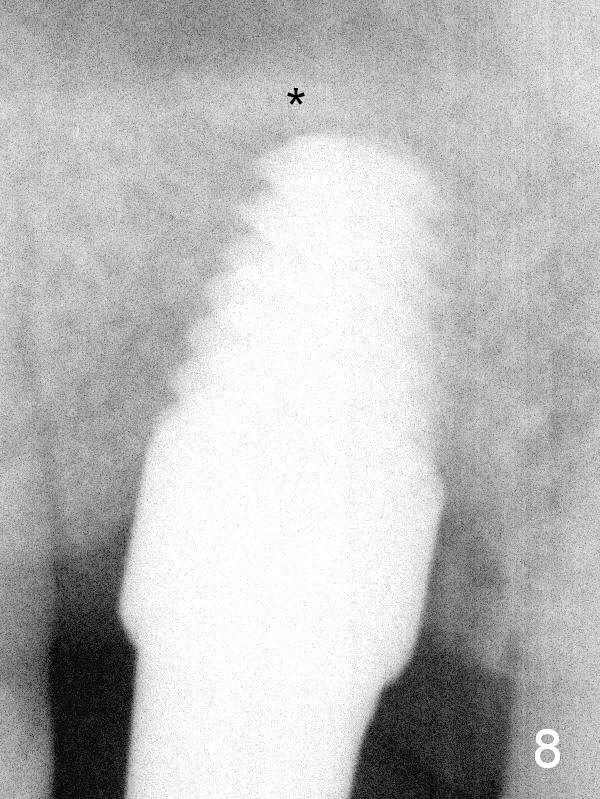
Three months postop, the bone density apical to the implant (within mushroom sinus lift area) increases (Fig.8 *). Socket gaps also appear to have healed.
Return to Upper Molar Immediate Implant,
Berkeley
Xin Wei, DDS, PhD, MS 1st edition 01/25/2016, last revision 05/02/2016