





 |
 |
 |
|||
 |
 |
 |
|||
 |
 |
 |
 |
 |
 |
 |
 |
 |
 |
||
Type II Bone
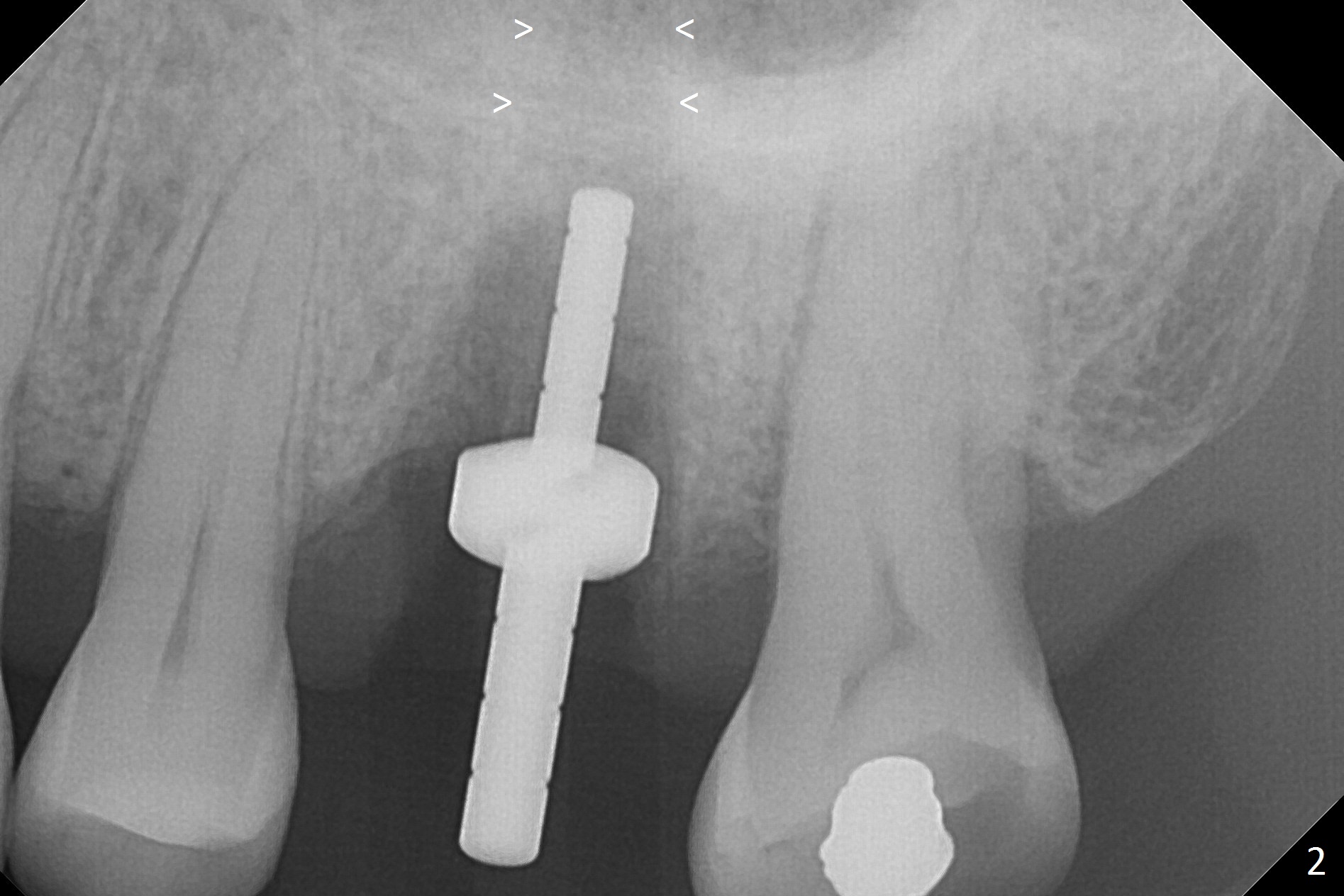
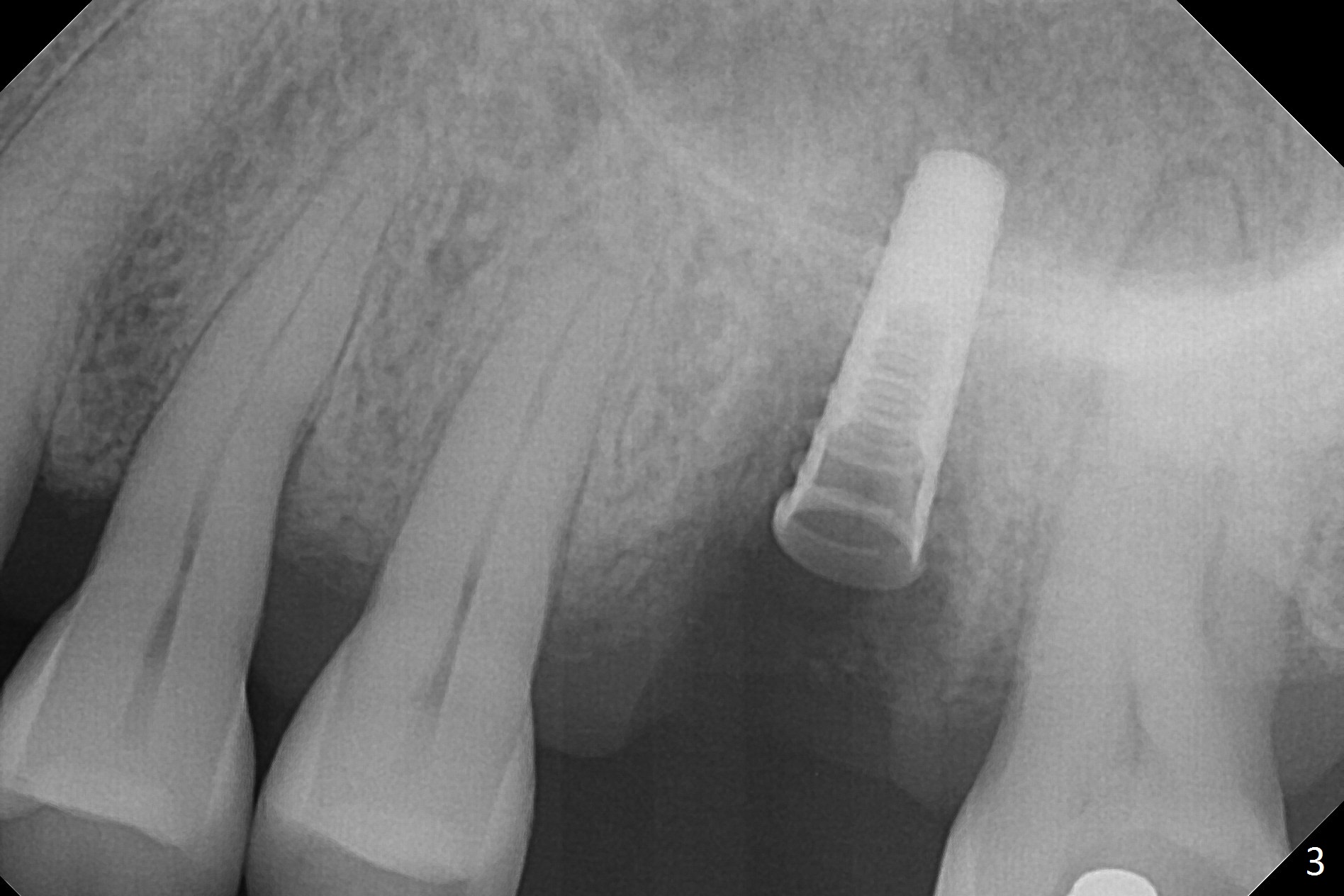
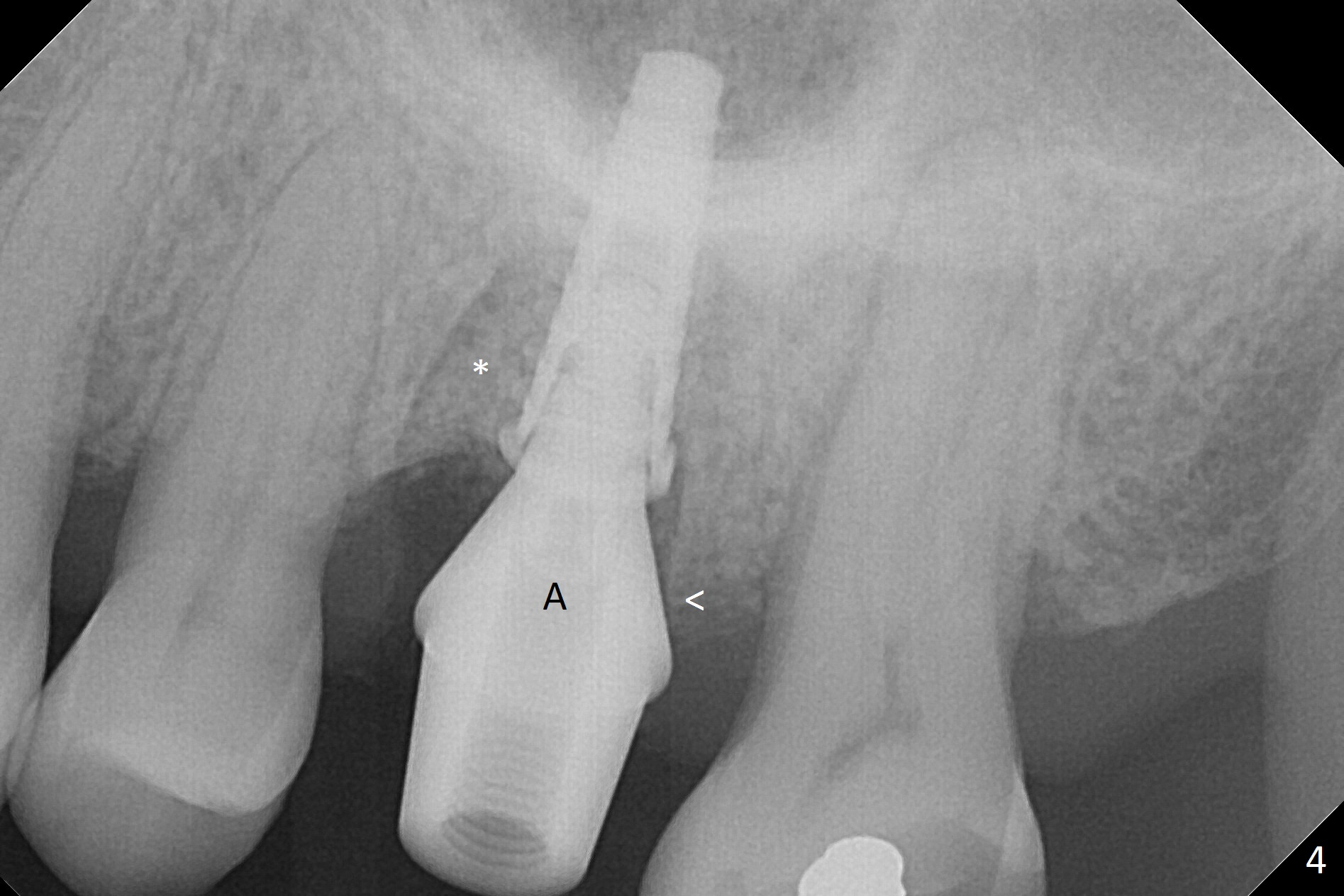
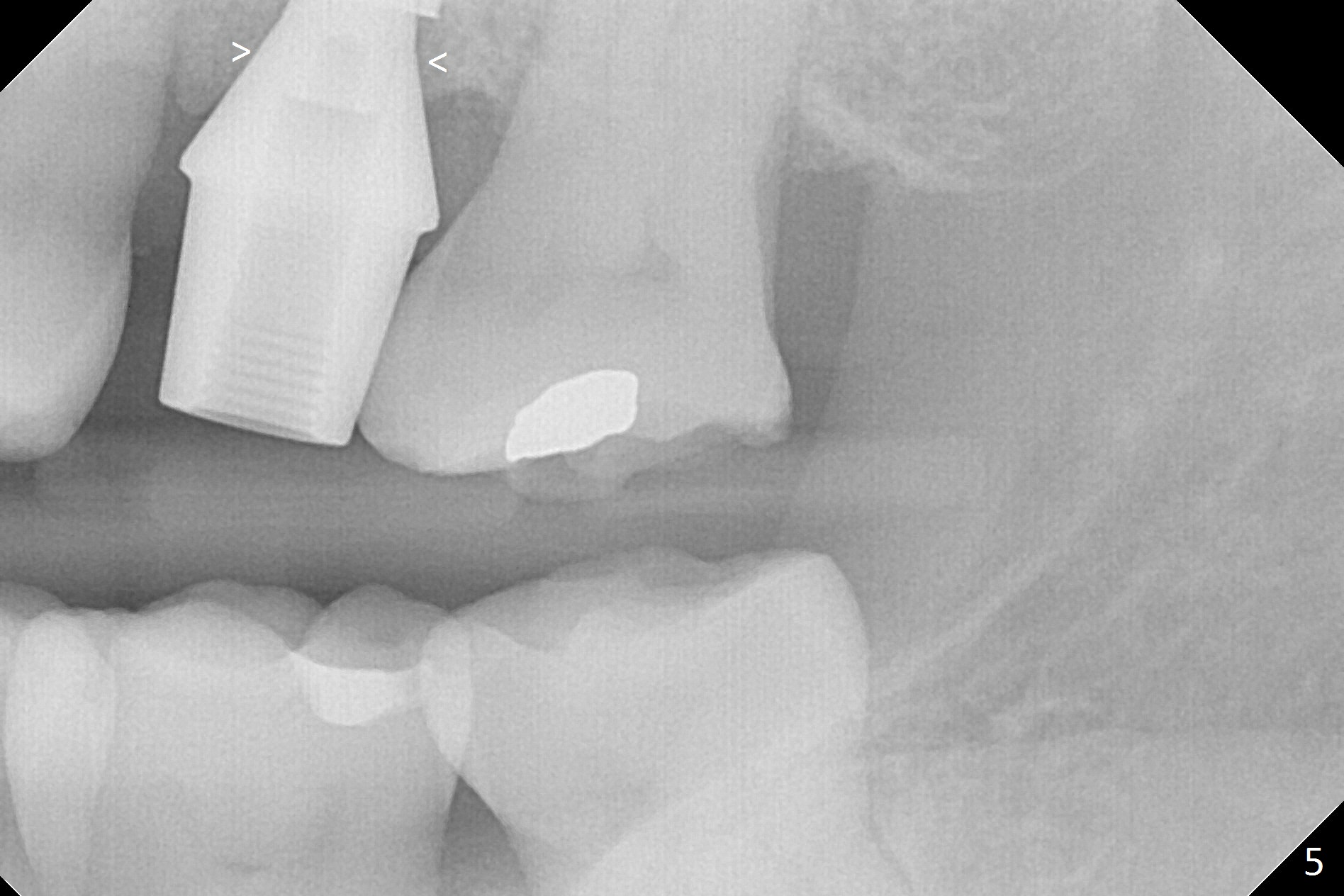
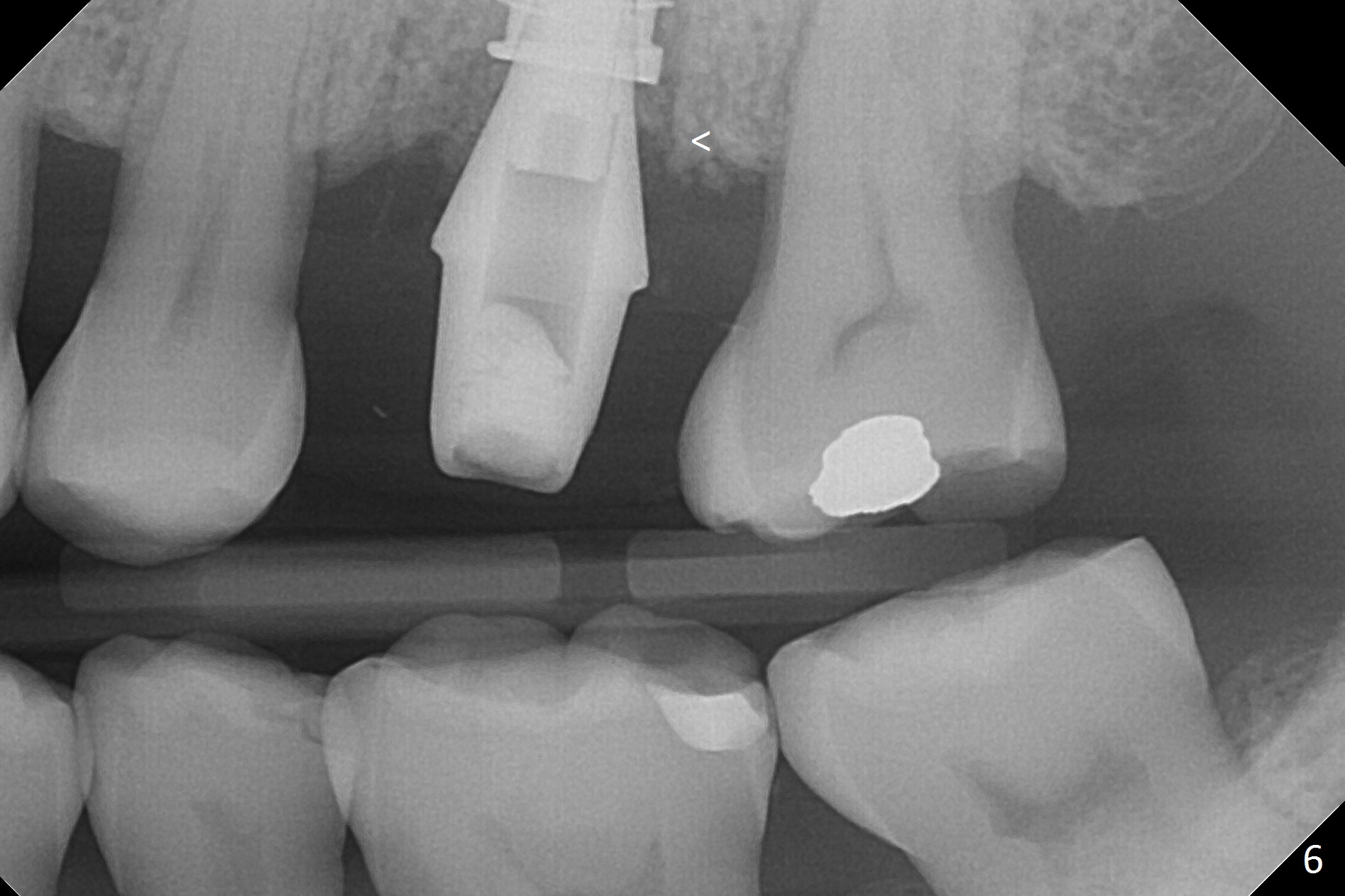
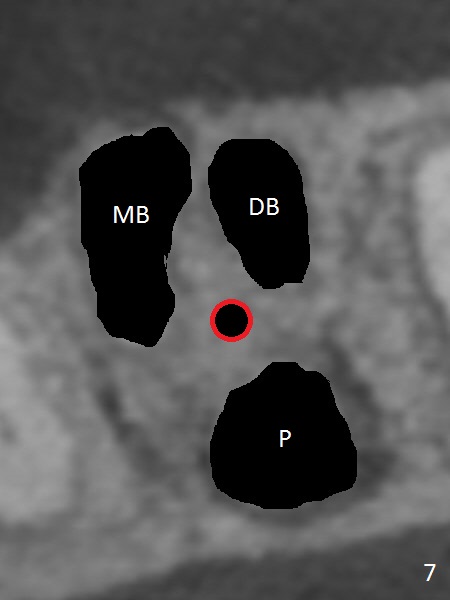
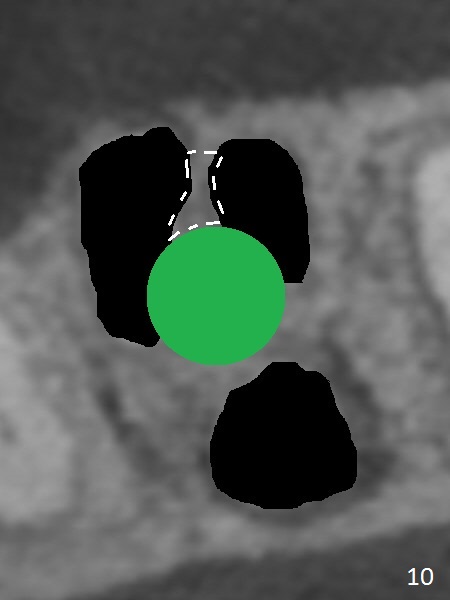
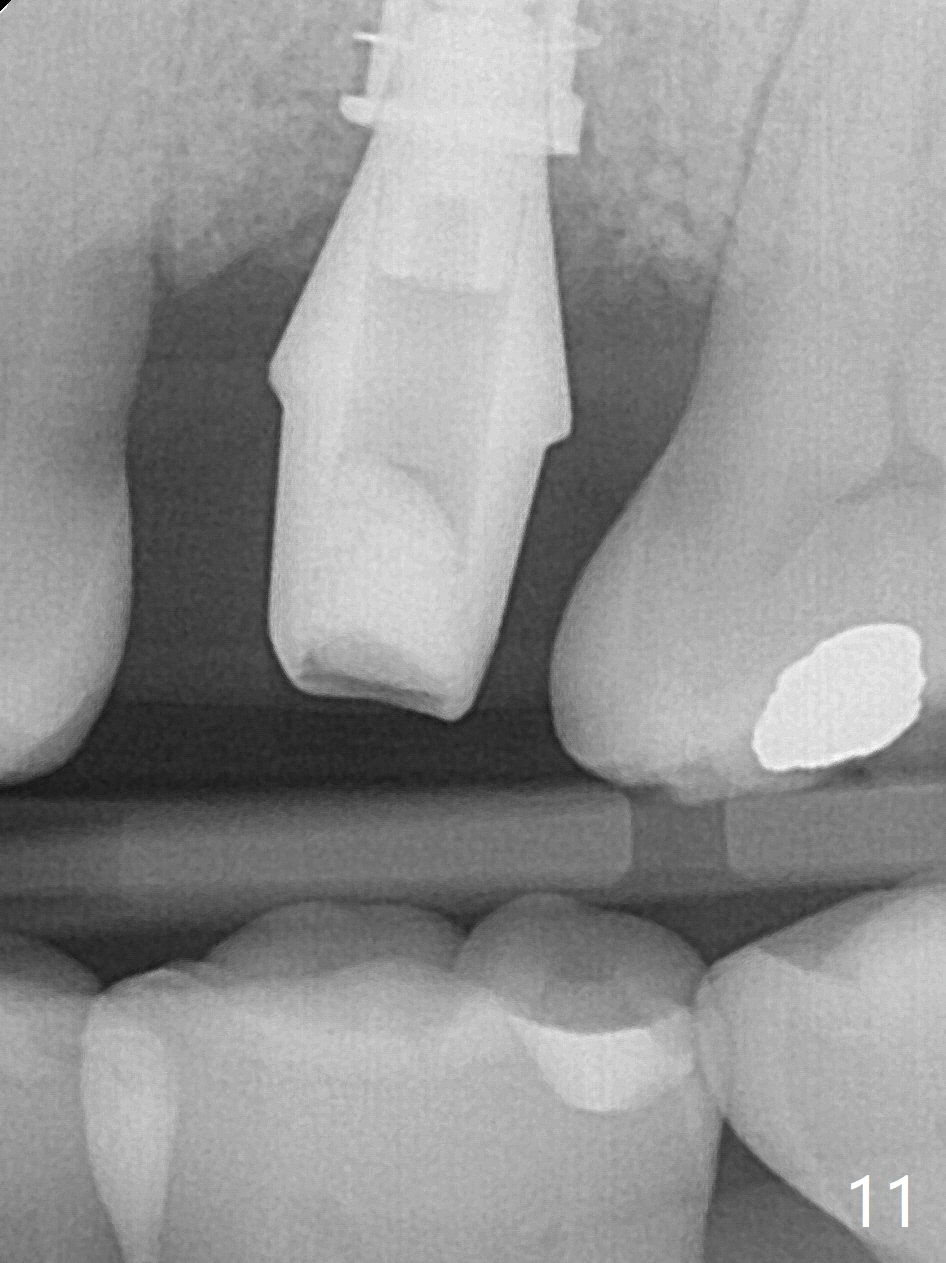
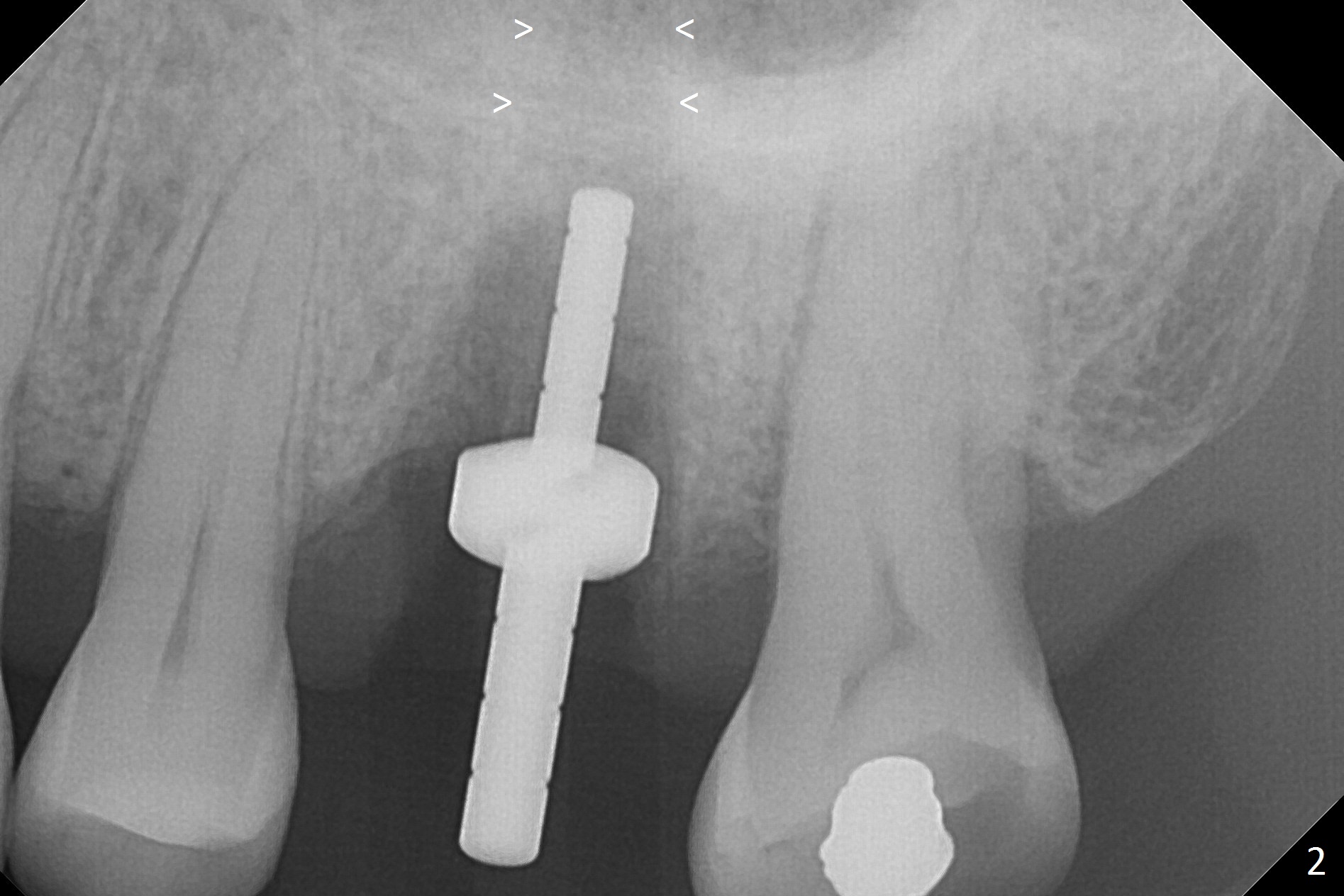
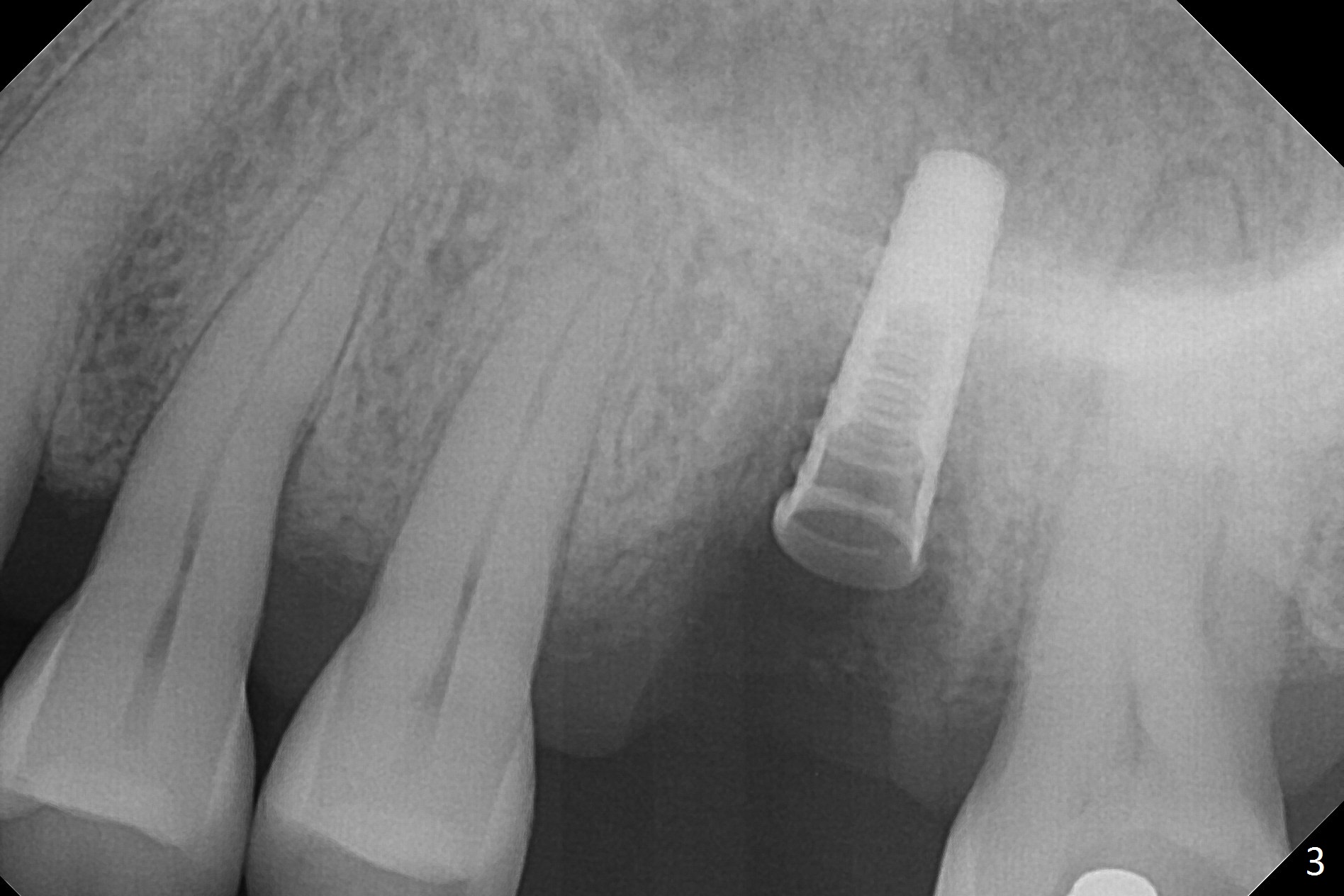
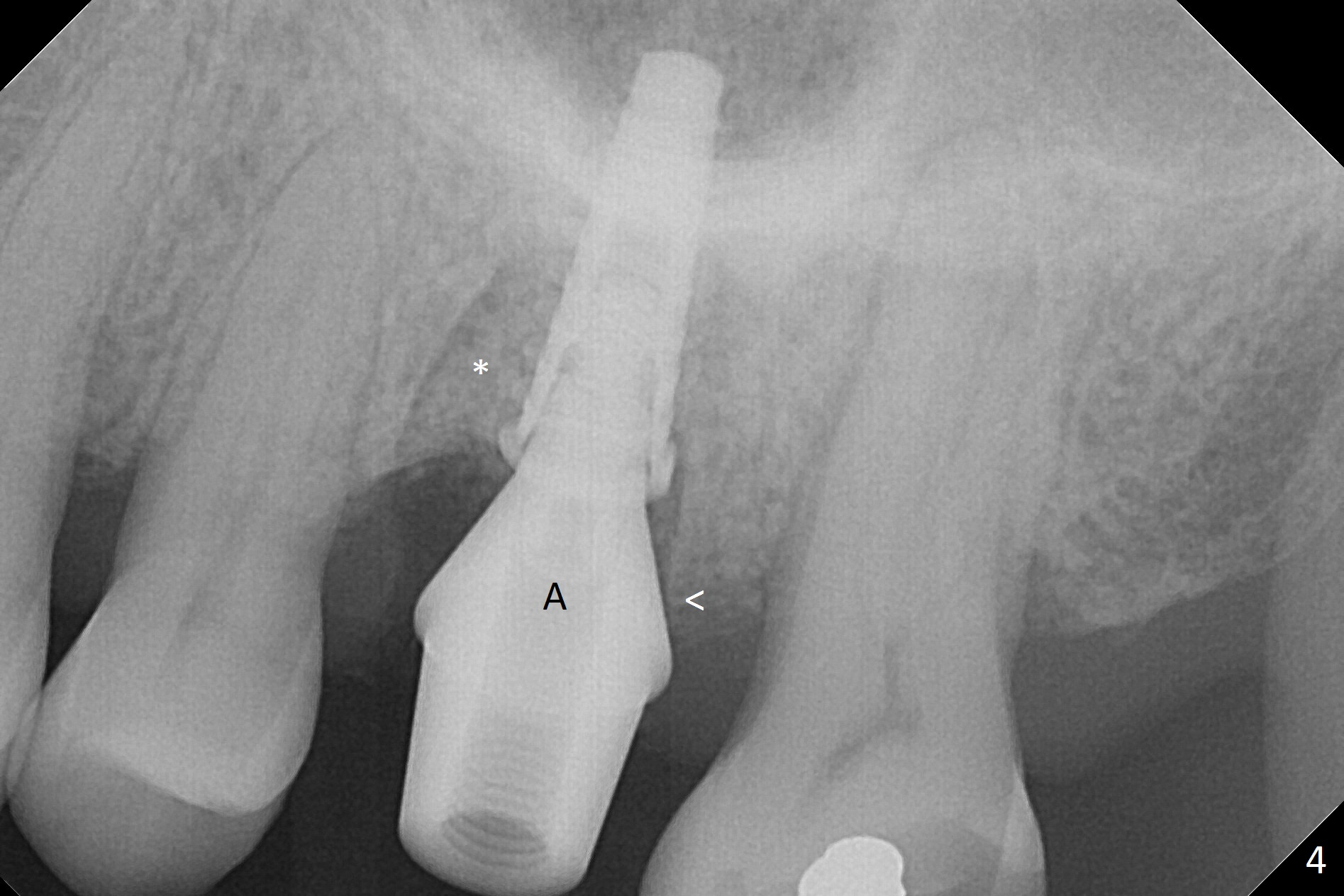
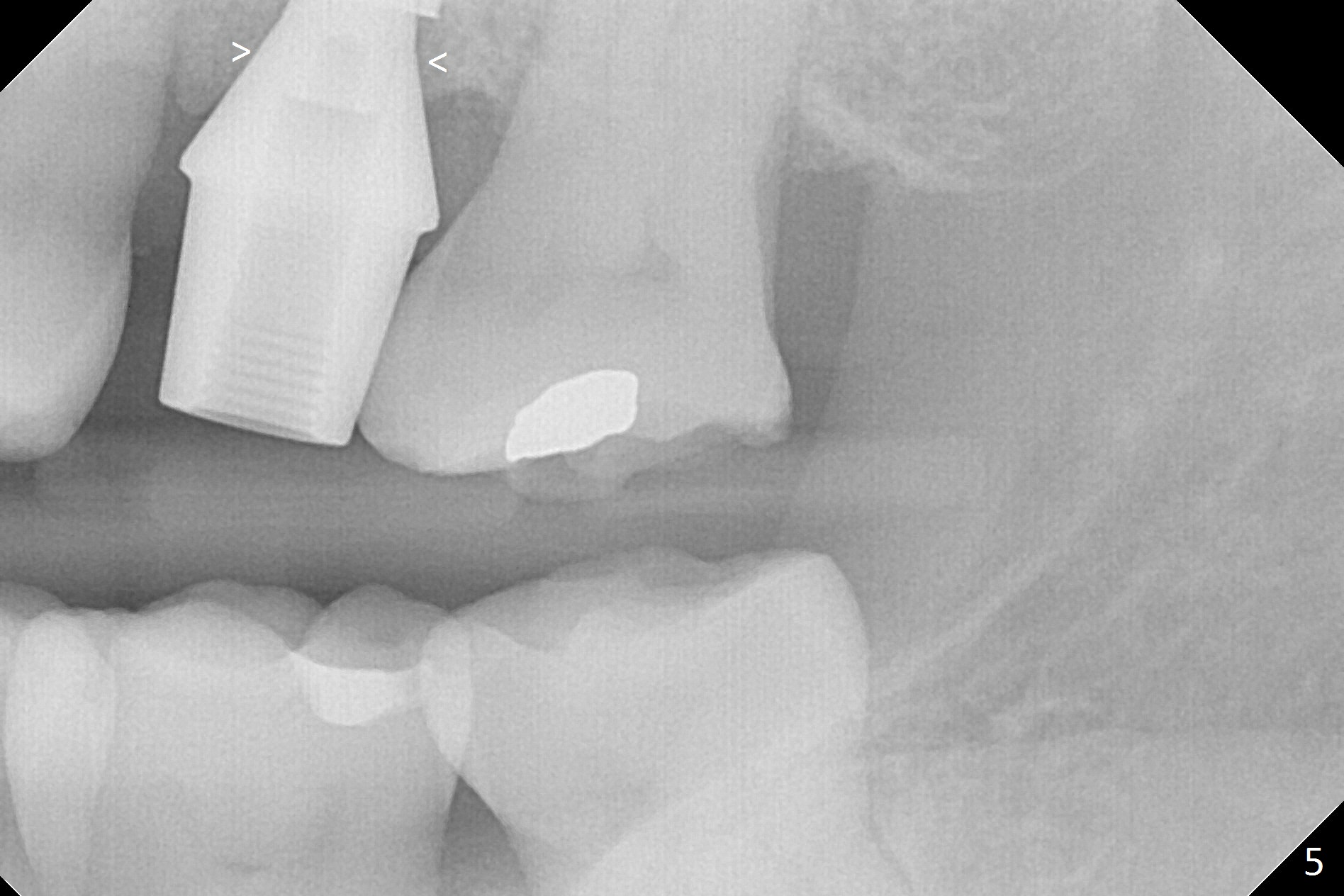
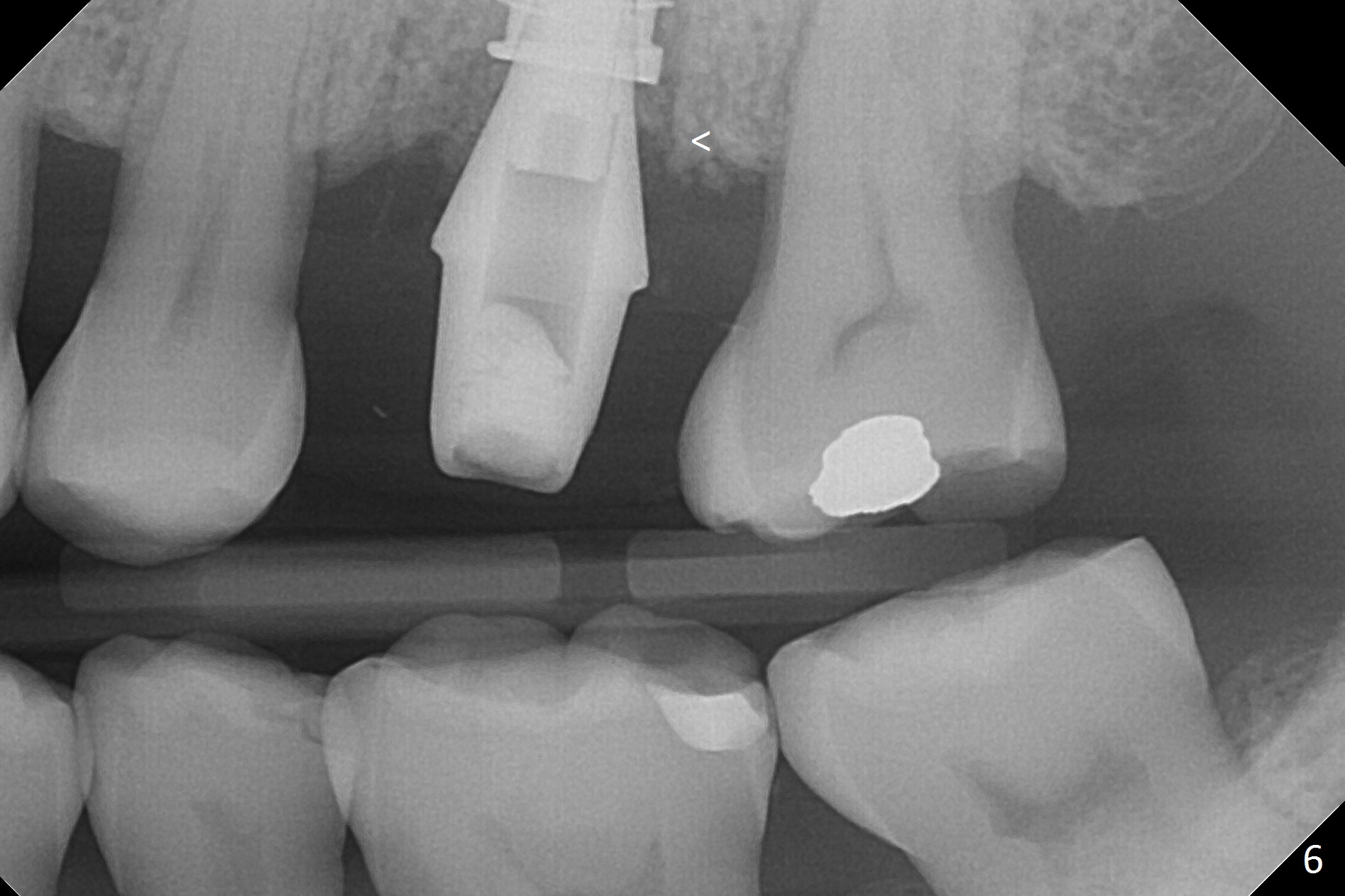
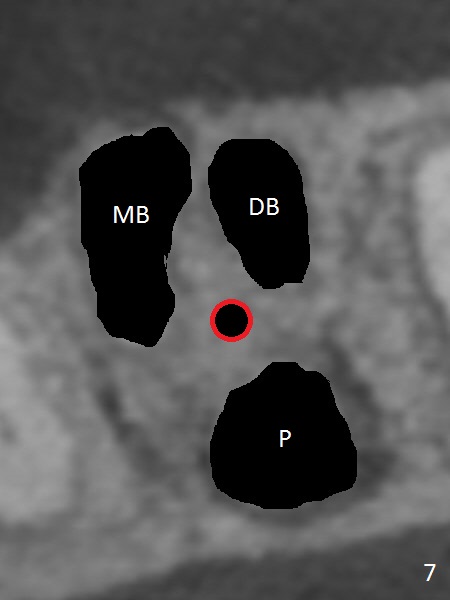
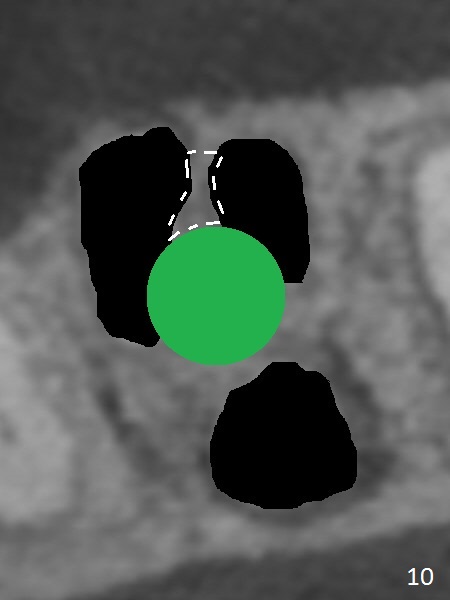
The affected tooth, #14, has gingival recession and tenderness at the mesiobuccal (MB) root (Fig.1 *). After extraction, osteotomy is established in the septum with 1.6 mm drill (Fig.2, 7 (red circle)). In fact the MB plate is intact. The osteotomy perforates into the distobuccal (DB) socket when 2.8 mm Magic Drill (MD, Fig.8) is used and into the mesiobuccal socket as well when larger MDs are being used (Fig.9). Before and after a 4x11 mm dummy implant is placed (Fig.3, Fig.10 green circle), the septum between MB and DB is displaced or broken down (Fig.10 white dashed line). Because of loss of the buccal bone of the osteotomy, it is difficult to place implant and push the bone core apically. Sinus lift of the bone core is accomplished using 3.0 mm Magic Expander prior to dummy implant placement, partially due to type II bone. Without any allograft for sinus lift, a 4.5x11 mm IBS implant is placed with insertion torque >40 Ncm (Fig.4) with allograft placed in the remaining socket gap (*). A 6.5x5.7(4) mm abutment (Fig.4 A) seems to contact the crestal bone (Fig.4,5 <). A smaller abutment appears appropriate for the site (Fig.6: 5.5x5.7(4) mm). A non-functional immediate provisional is fabricated.
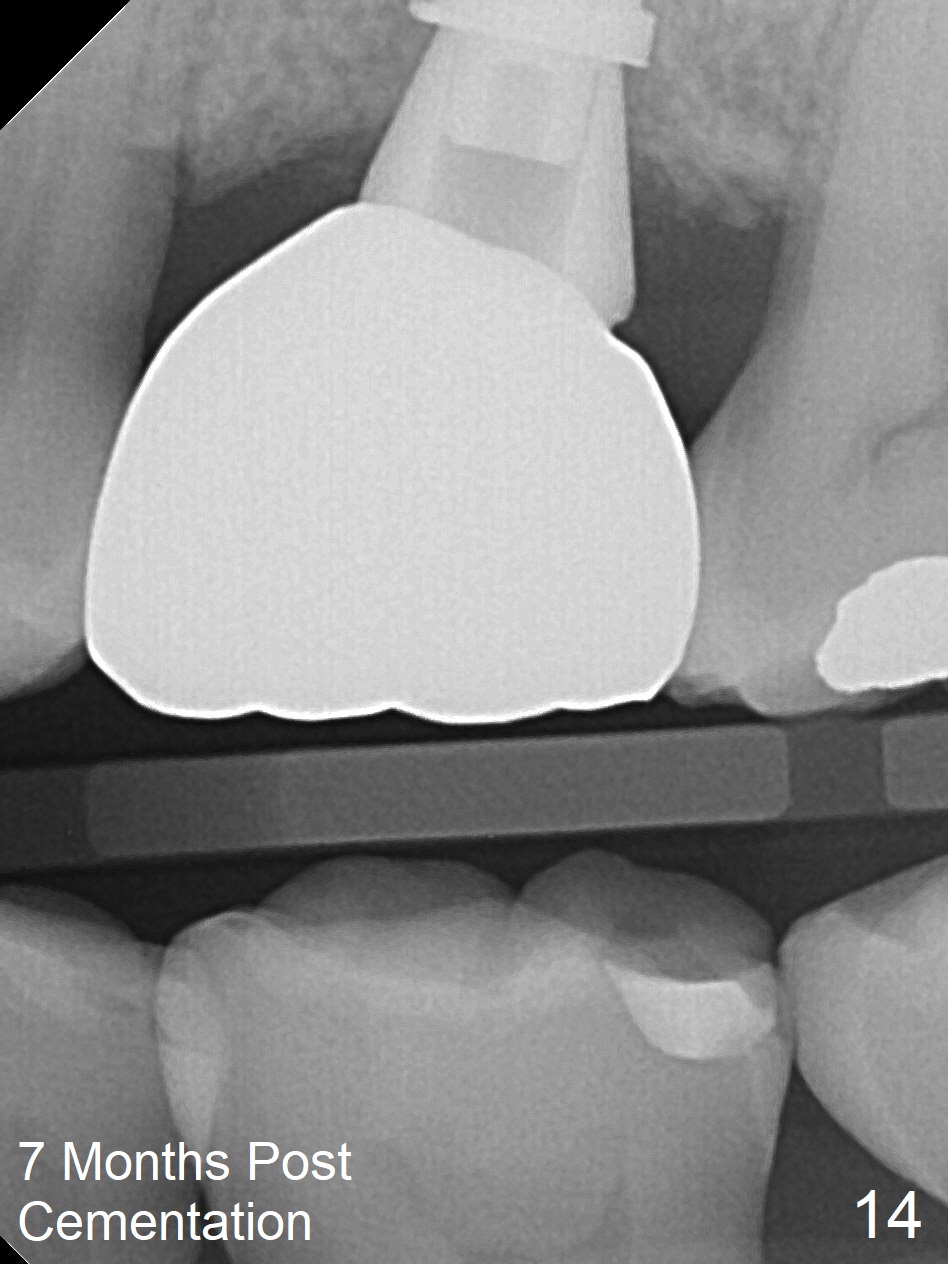
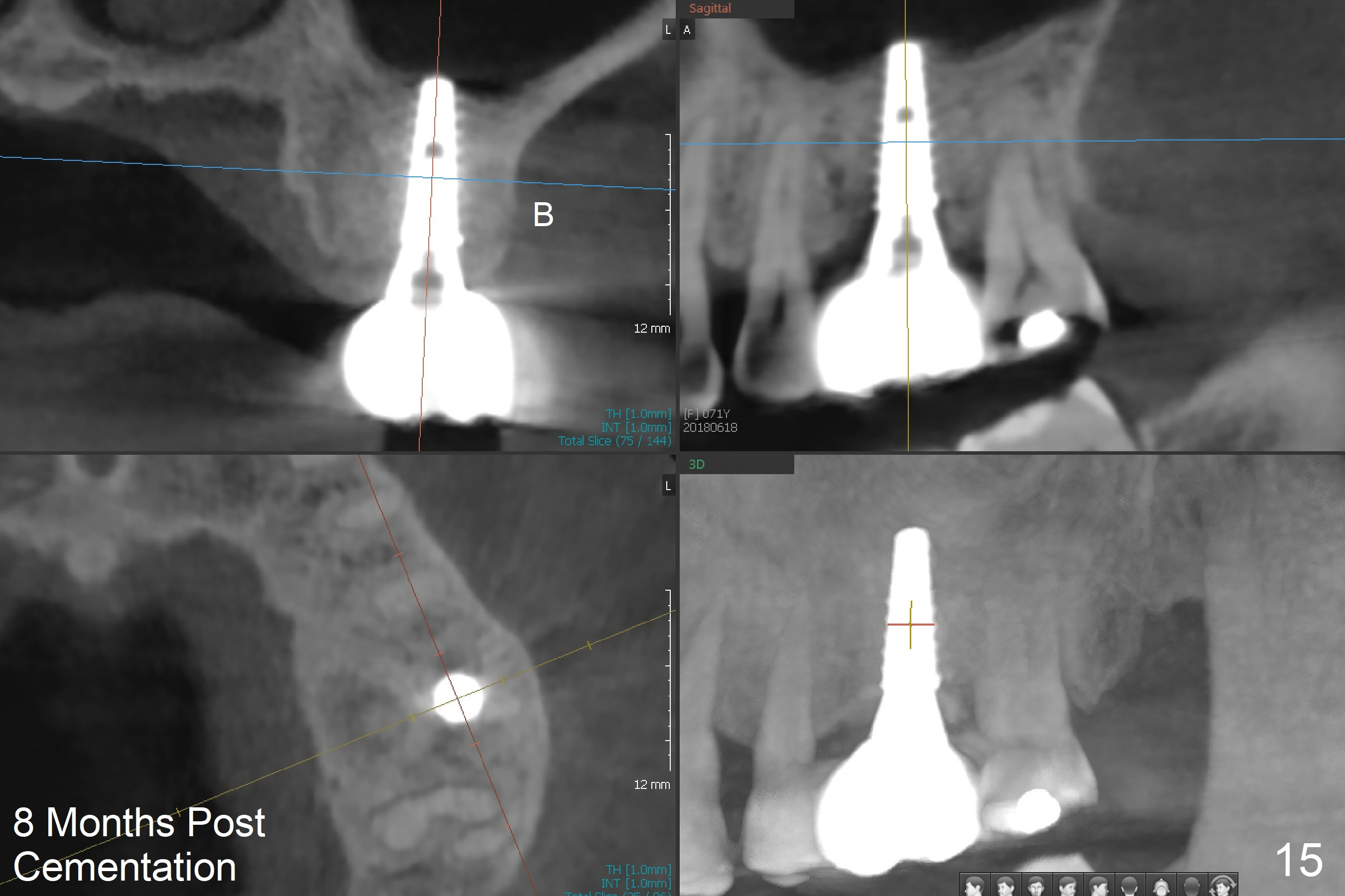
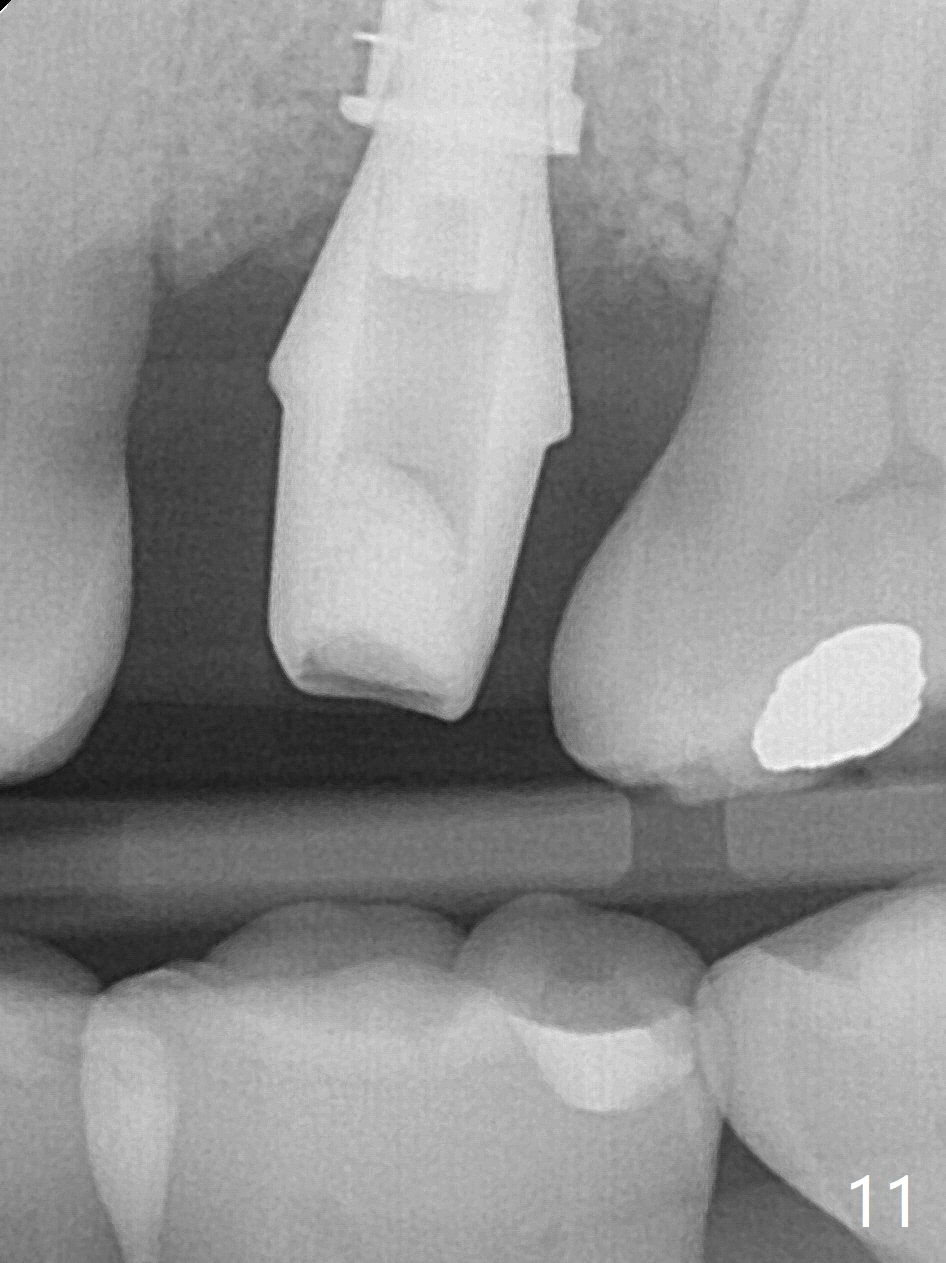
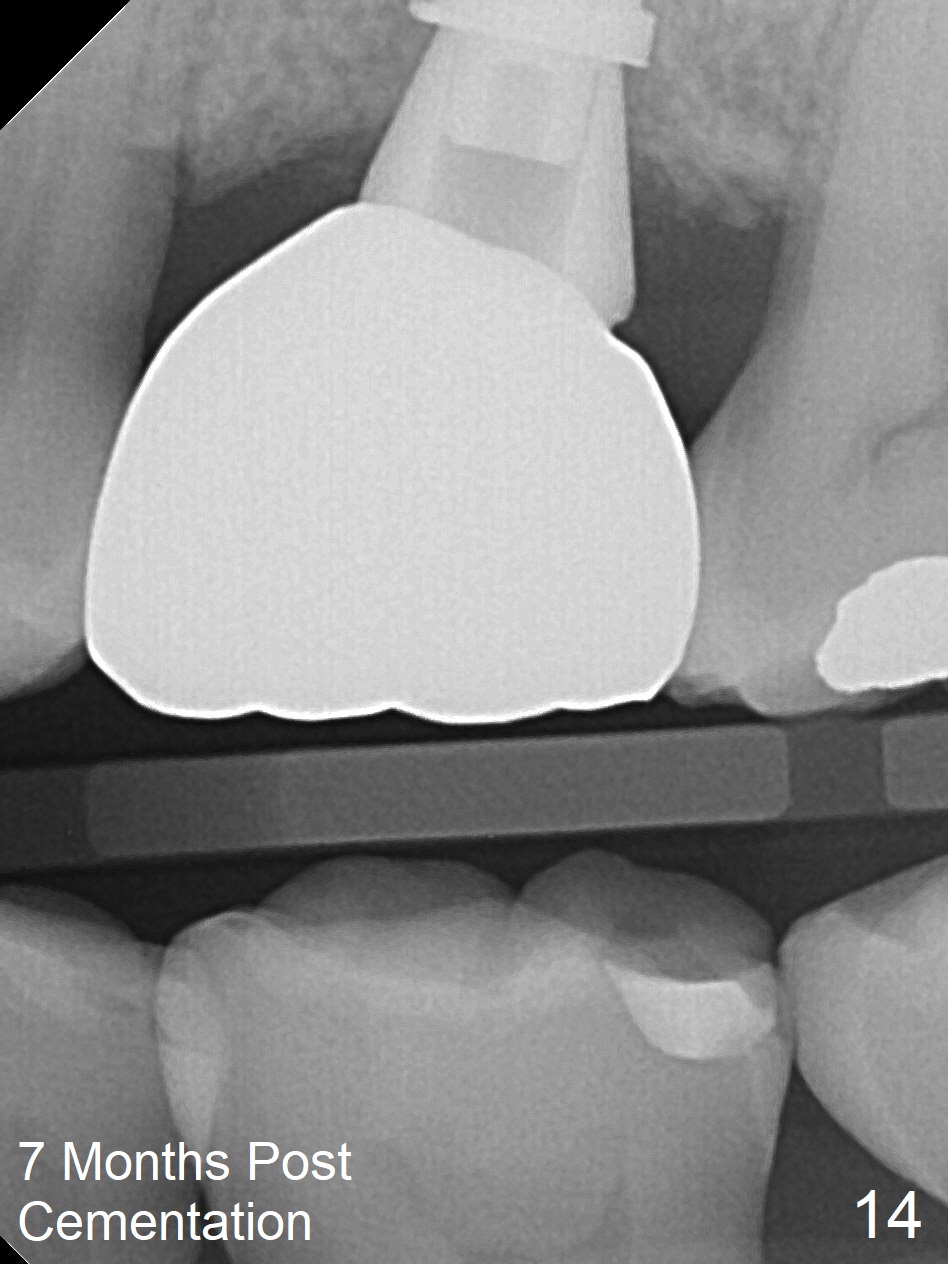
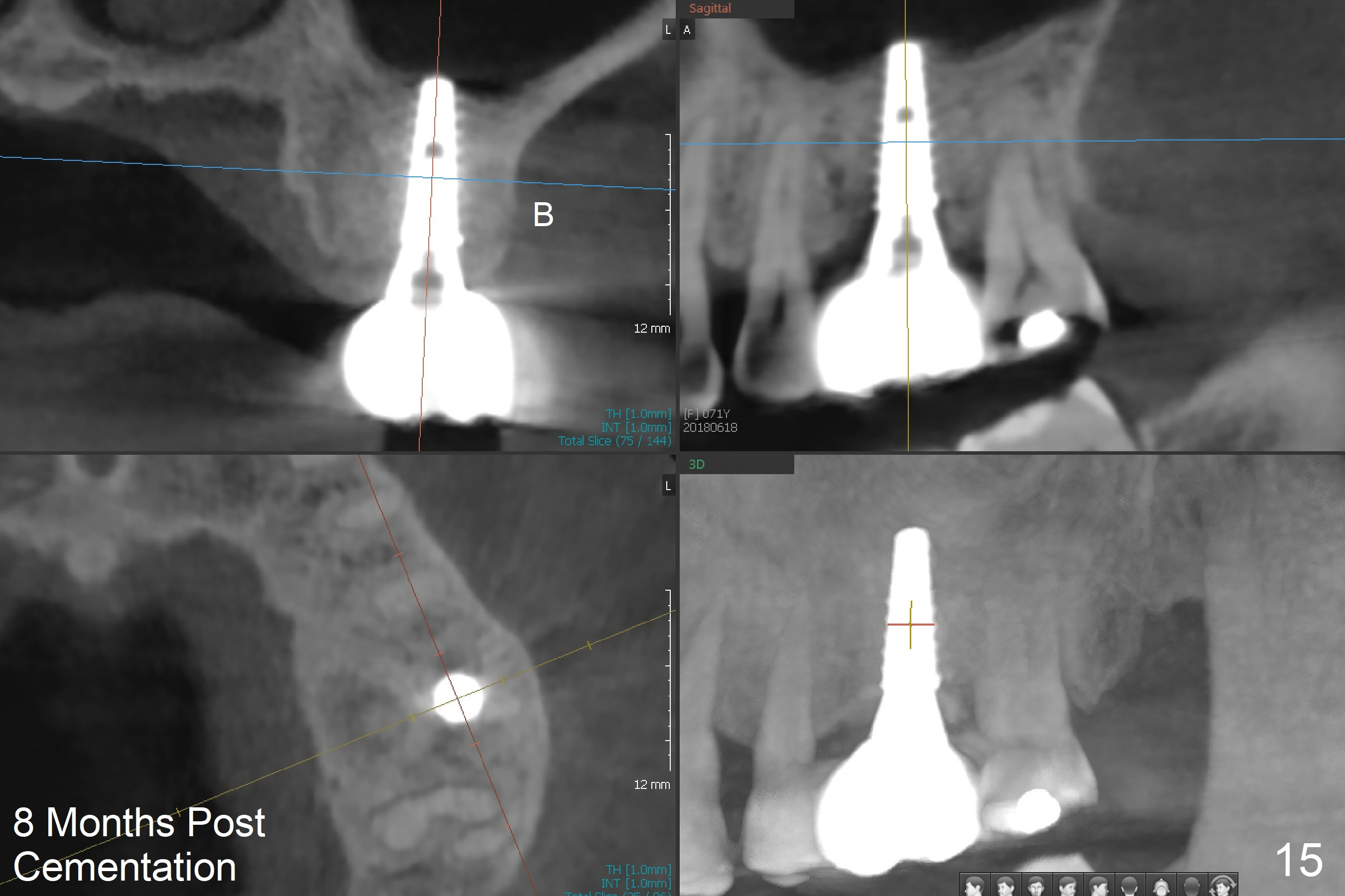
Both the hard (Fig.11,12) and soft (Fig.13) tissues heal 4 months postop. The permanent restoration functions well (Fig.14, 7 months post cementation). She is ready for #30 immediate implant, but she complains that the implant at #14 cannot sustain heavy mastication. CBCT shows that the implant seems small in diameter and buccally placed (Fig.15B). She reports pain after eating steak and pizza crust lasts for a few days, suspecting implant protruding into the sinus (Fig.16 (13 months post cementation)).
Return to
Upper
Molar Immediate Implant, Prevent
Molar Periimplantitis (Protocols,
Table)
Xin Wei, DDS, PhD, MS 1st edition 05/23/2017, last revision 11/26/2018