

 |
 |
 |
 |
 |
 |
 |
 |
 |
 |
 |
 |
Implant Placement with Sinus Lift for 1 mm Sinus Floor
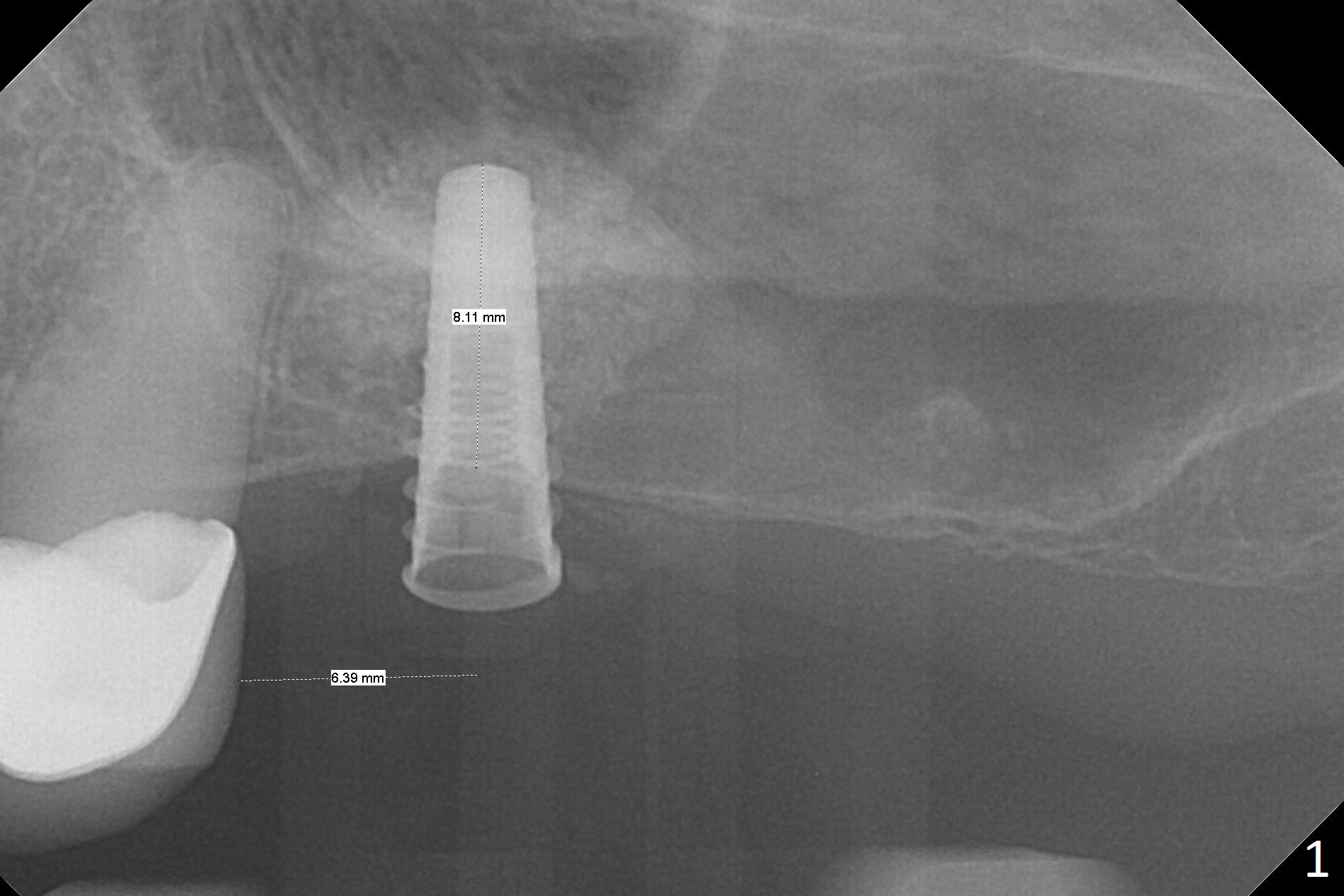
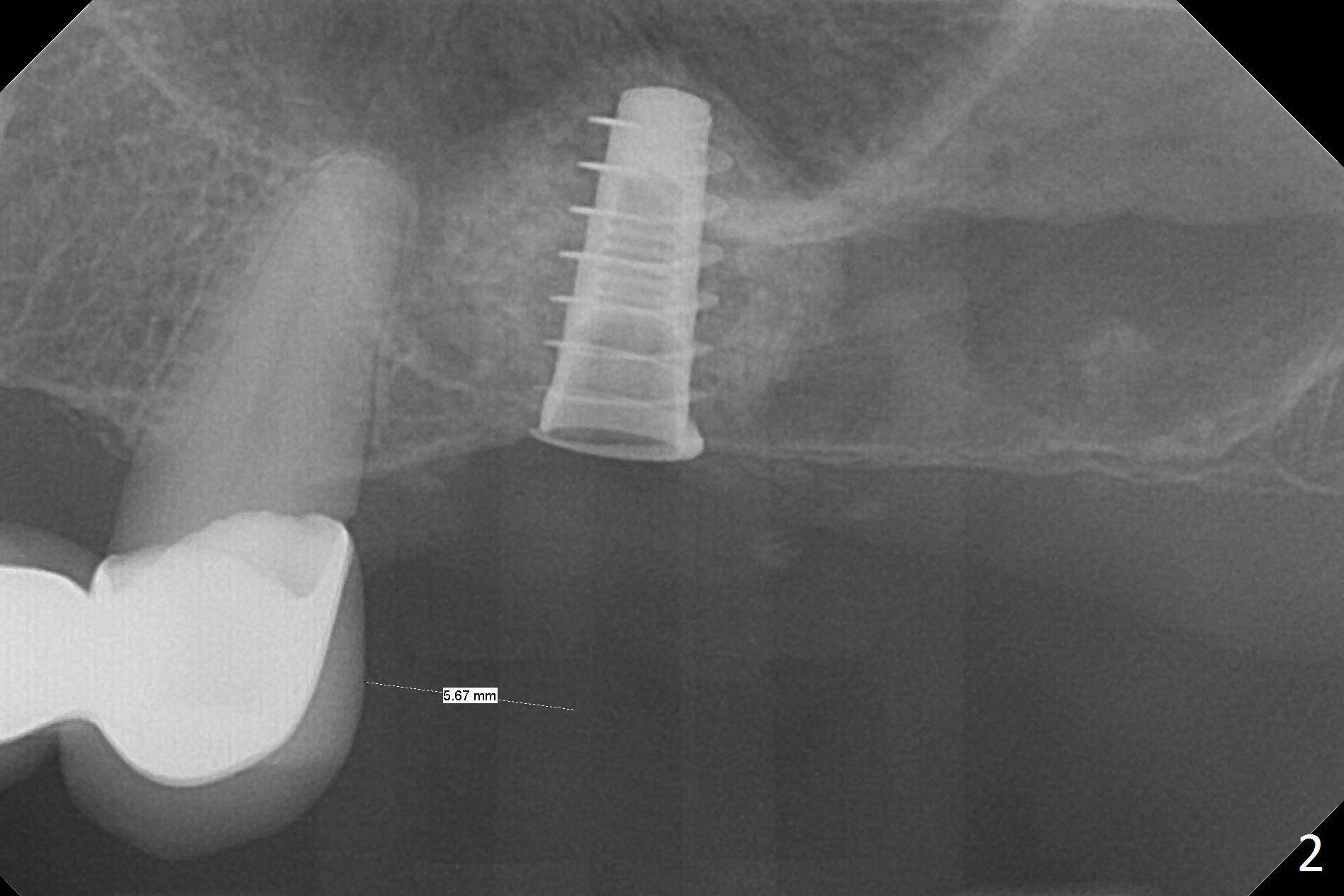
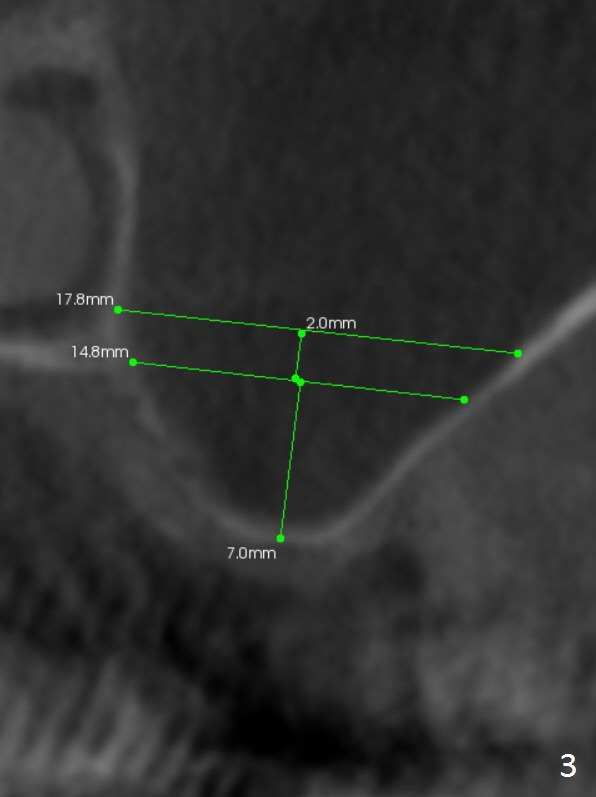
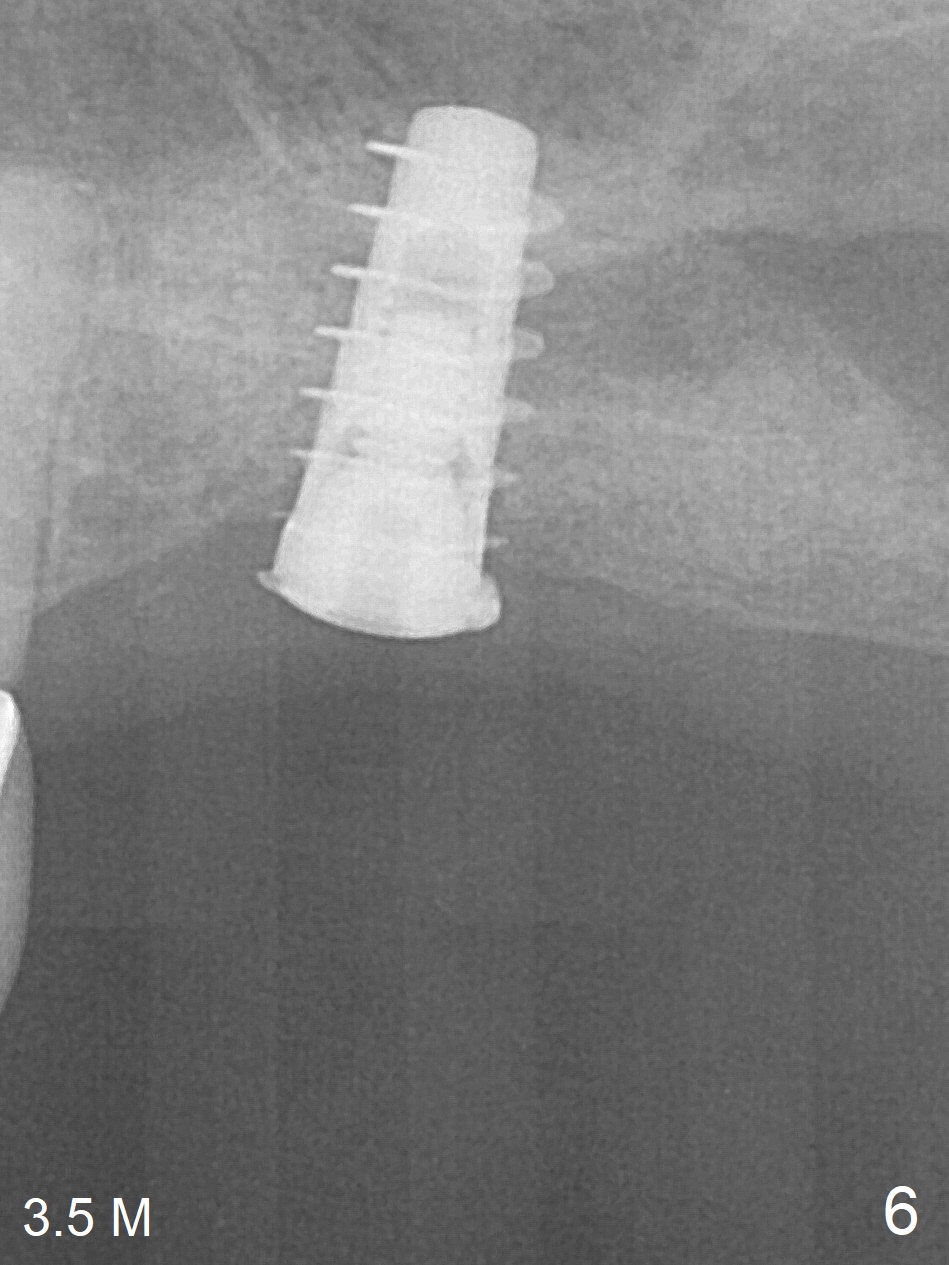
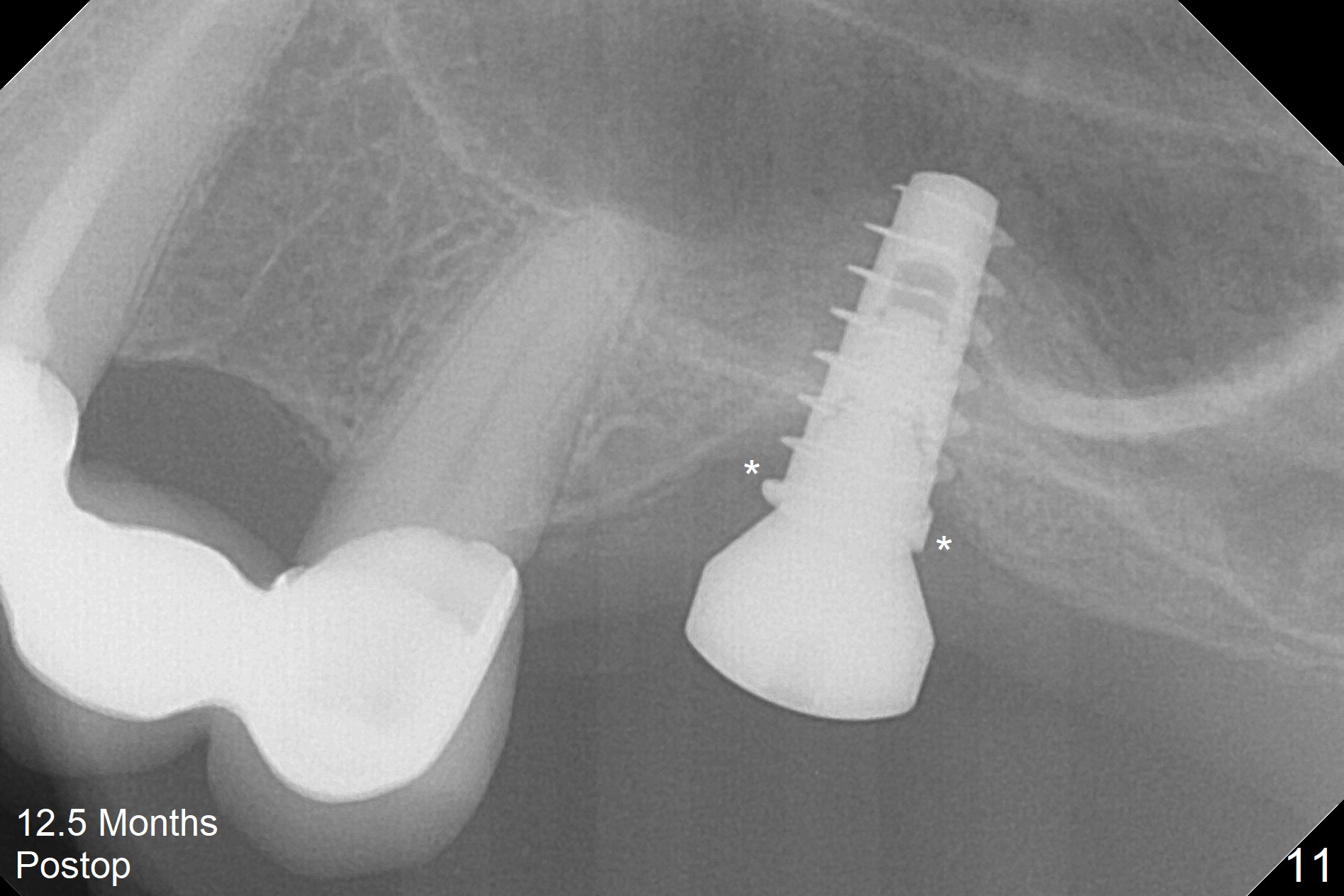
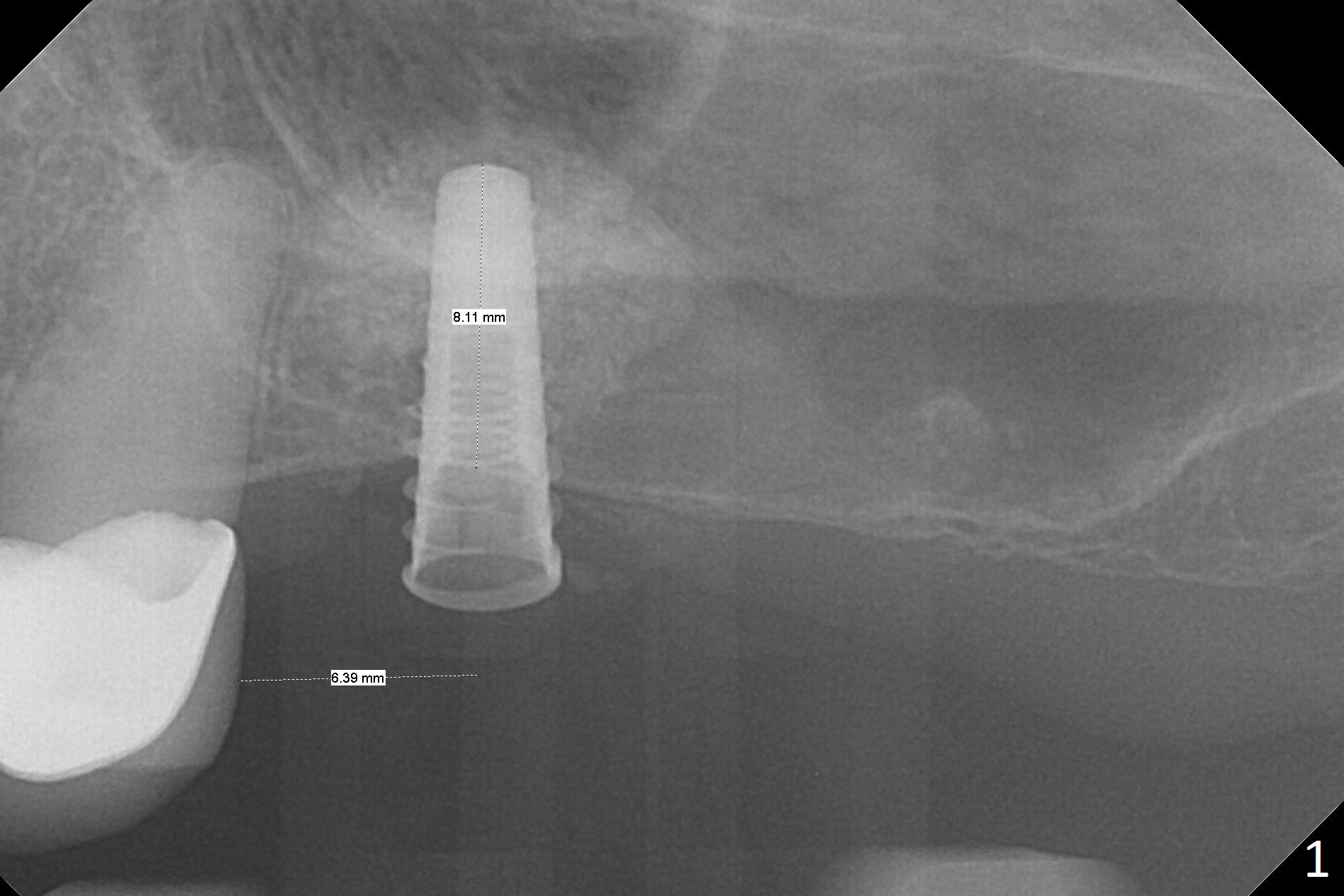
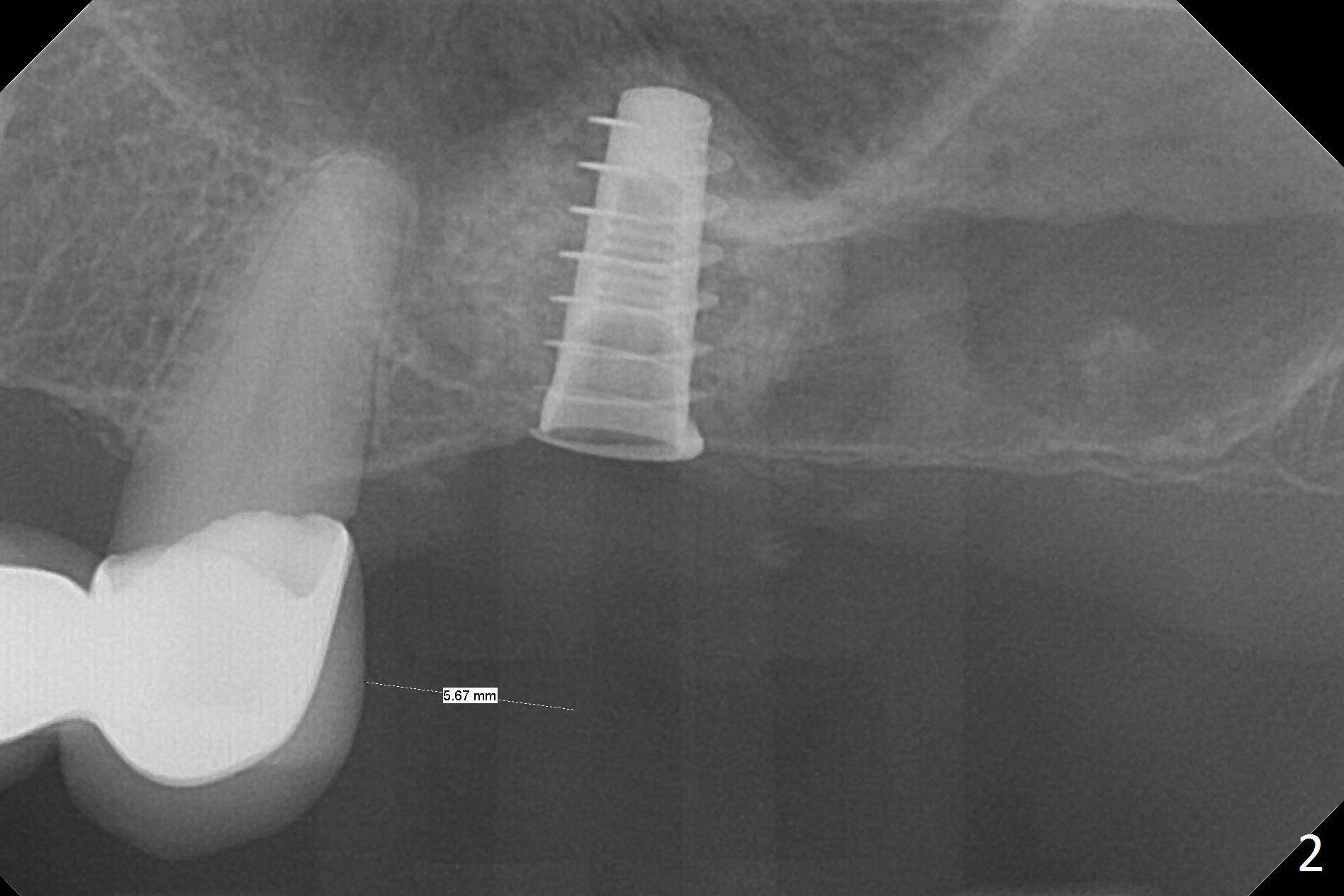
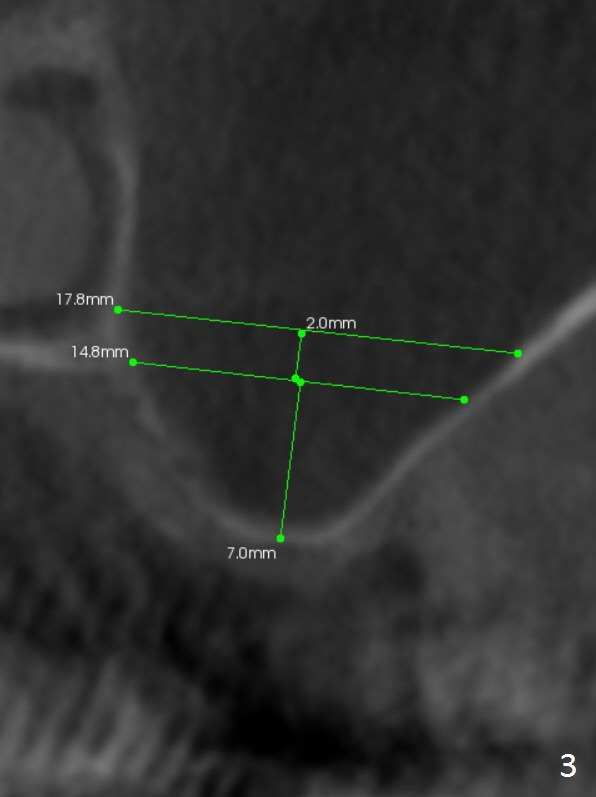
Blood drawing for PRF fails. After NO inhalation and local anesthesia, an incision is made at the narrow ridge of #14. Magic Sinus Lifter is used to elevate the sinus floor for ~ 5 mm, followed by insertion of allograft/Osteogen and 4.0x11 mm dummy implant partially (Fig.1). With approximately 10% more of graft being placed, a 4.5x9 mm IBS implant is placed with insertion torque of 15 Ncm (Fig.2). The shape of the sinus suggests that the primary stability is derived from the contact between the implant and the sinus floor (Fgi.3, preop CBCT coronal section). Approximately .5 mm implant threads are exposed buccodistopalatally, which are covered by allograft and collagen membrane before suturing. There is one episode of nasal discharge postop. The wound dehisces without sign of infection (Fig.4 (1 month 1 week postop)).
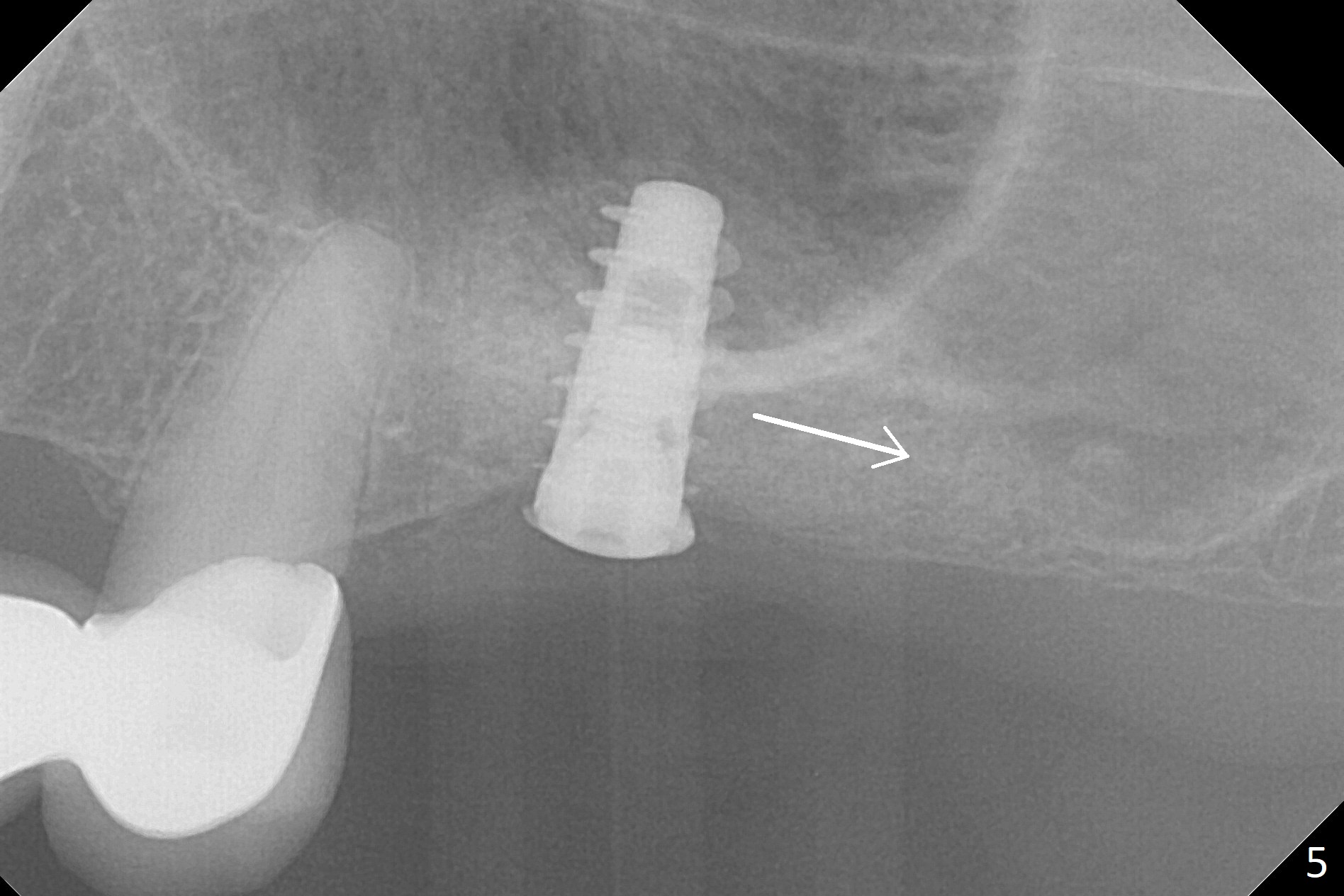
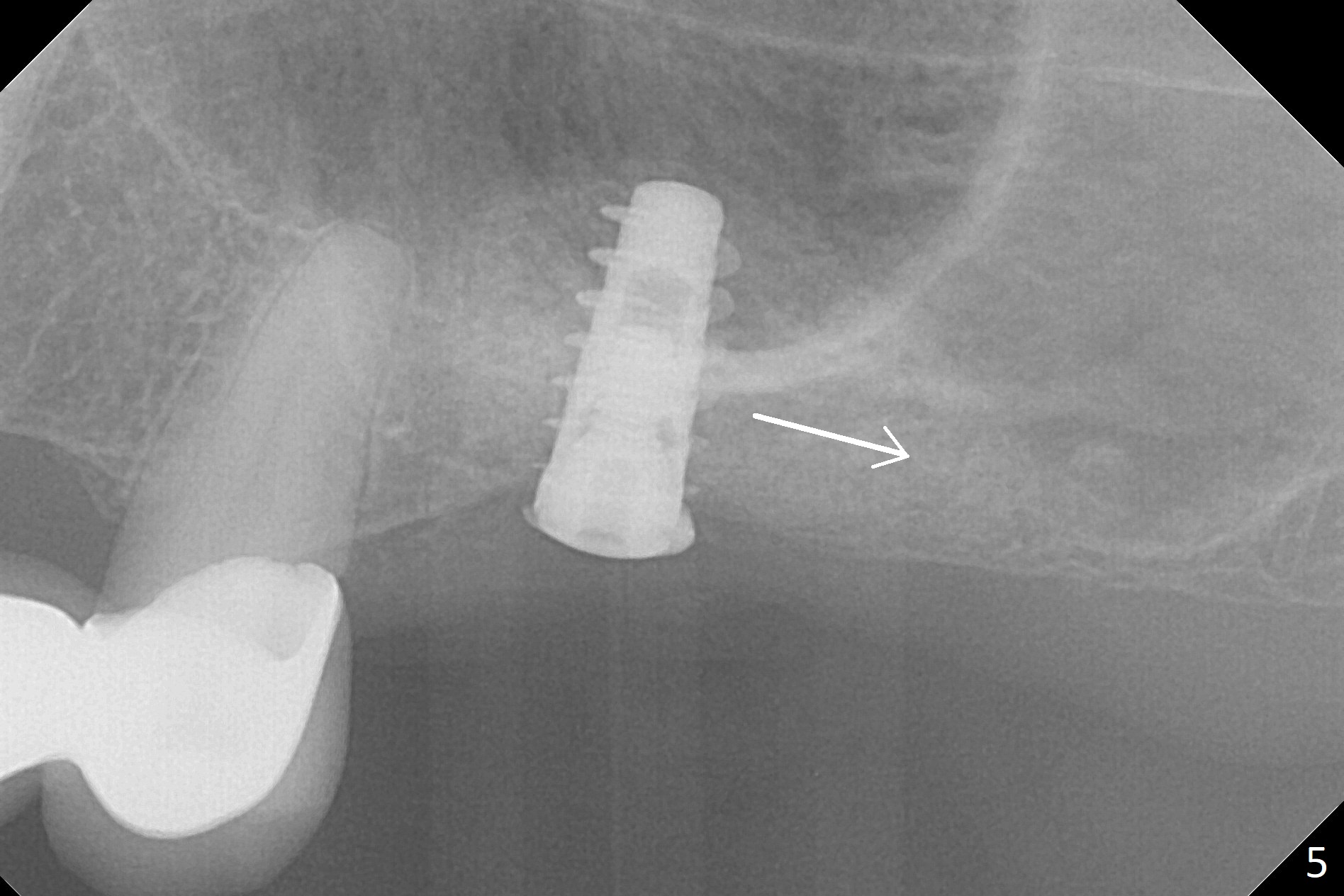
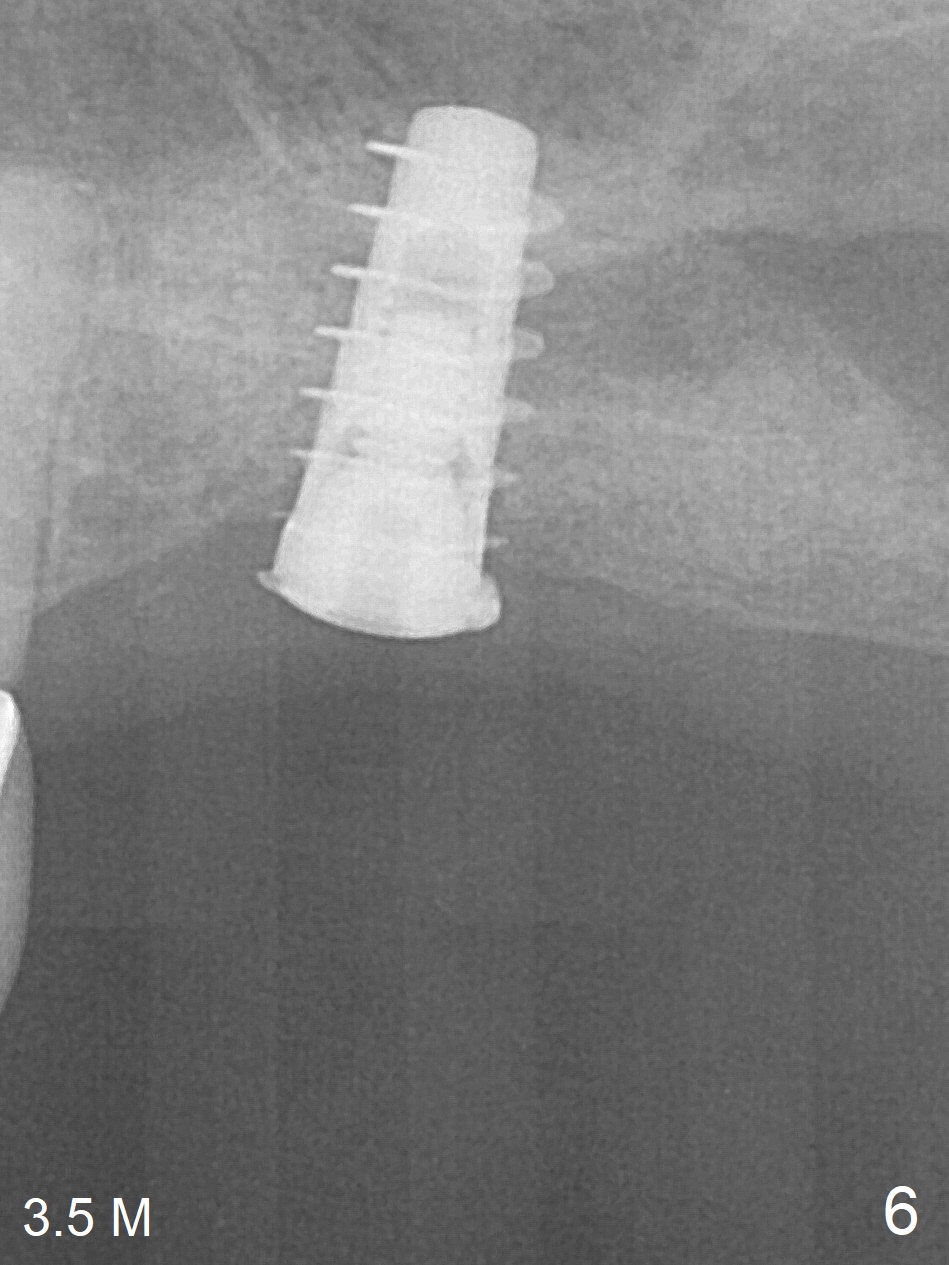
The bone graft appears to move distal 1 month 20 days postop (Fig.5 arrow), while the implant seems to be extruded with implant exposure. The patient feels pain when the healing screw is being removed or tightened. The distal migration of the bone graft may lay foundation for future implant placement at #15. Bone density around the implant remains the same (Fig.6), while the wound reduces nearly 3.5 months postop (Fig.7). The healing screw cannot be turned without causing pain. Can the implant at #14 be retorqued to be seated deeper 3-4 months later?
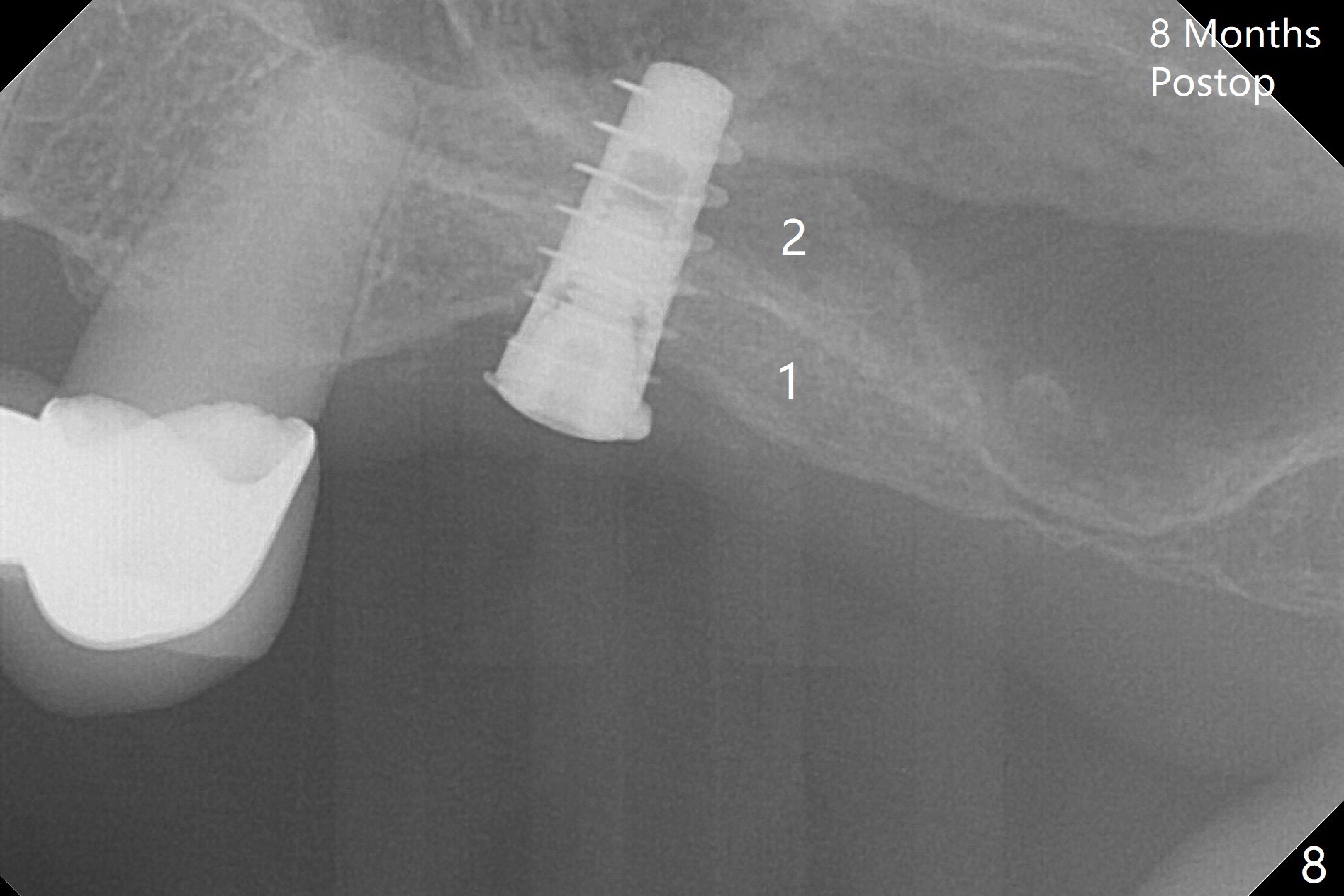
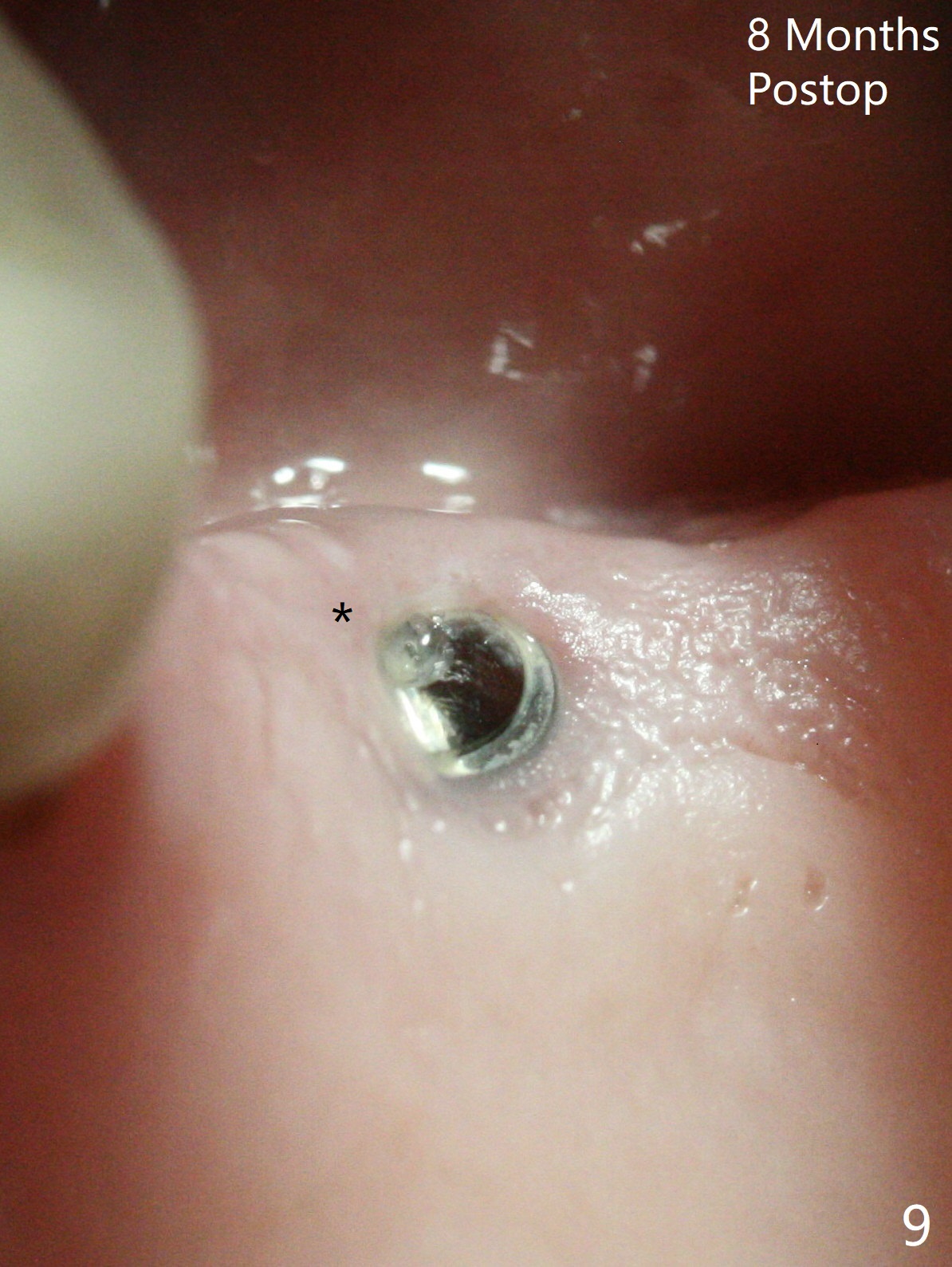
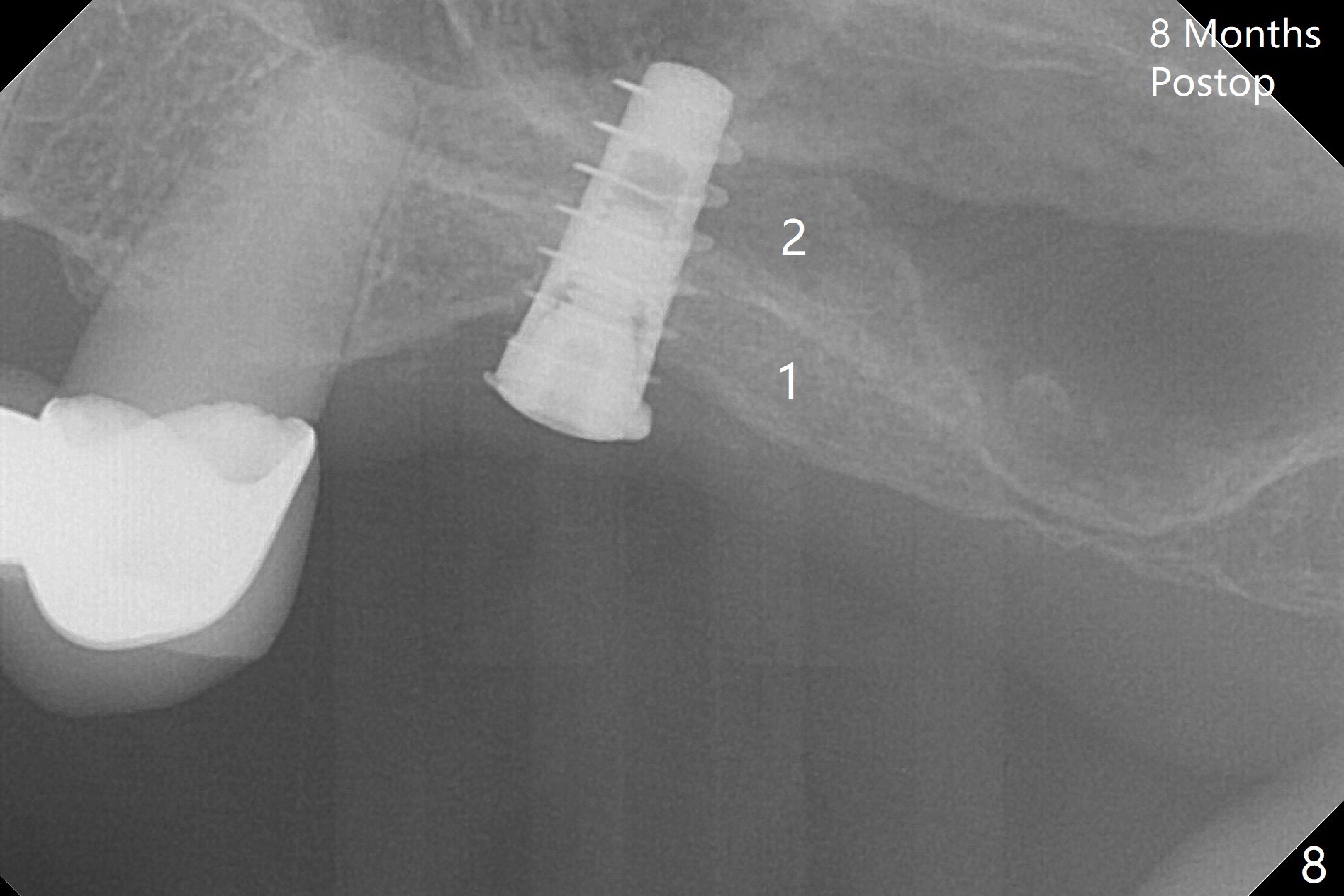
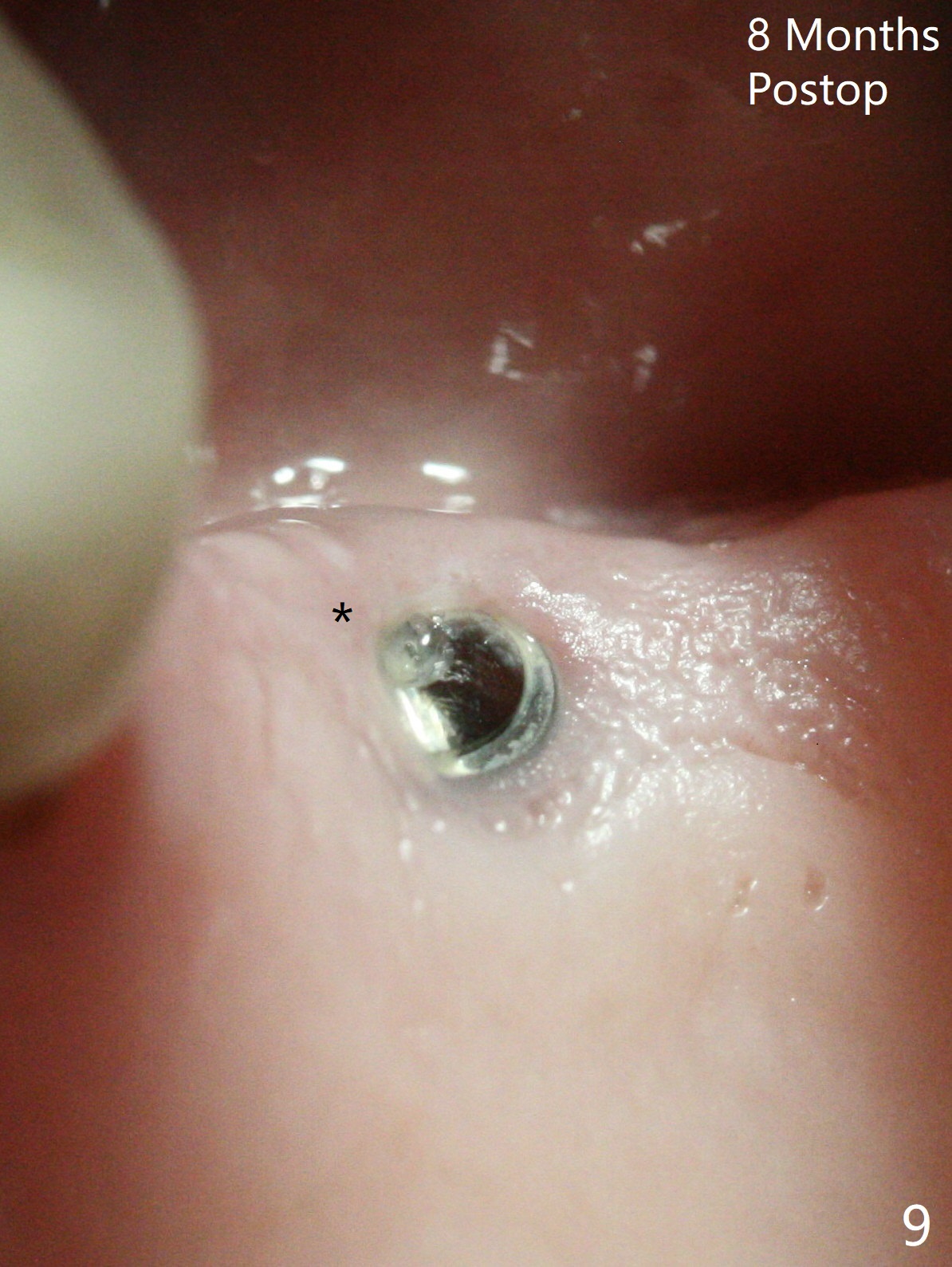
There are two layers of the bone, one (1) being denser than the other (2) 8 months postop (Fig.8). After local anesthesia, the healing screw is removed; the implant is found to be stable. A 6x4(2) mm pair abutment cannot be inserted due to blockage of the mesiobuccal gingiva (Fig.9 *). Instead a 6x2 mm healing abutment is placed. Since the implant is placed too superficial, use a 1 mm cuff abutment.
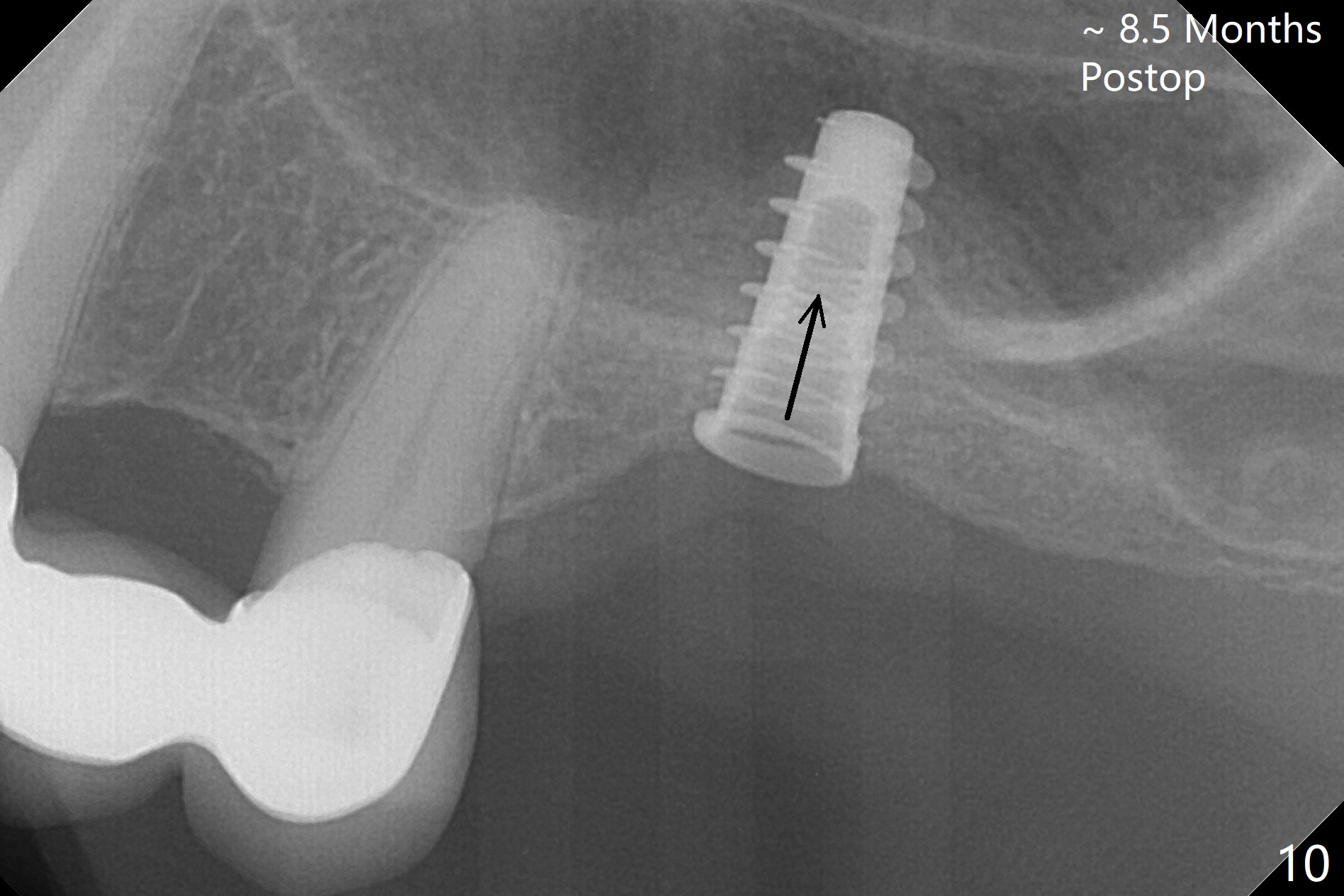
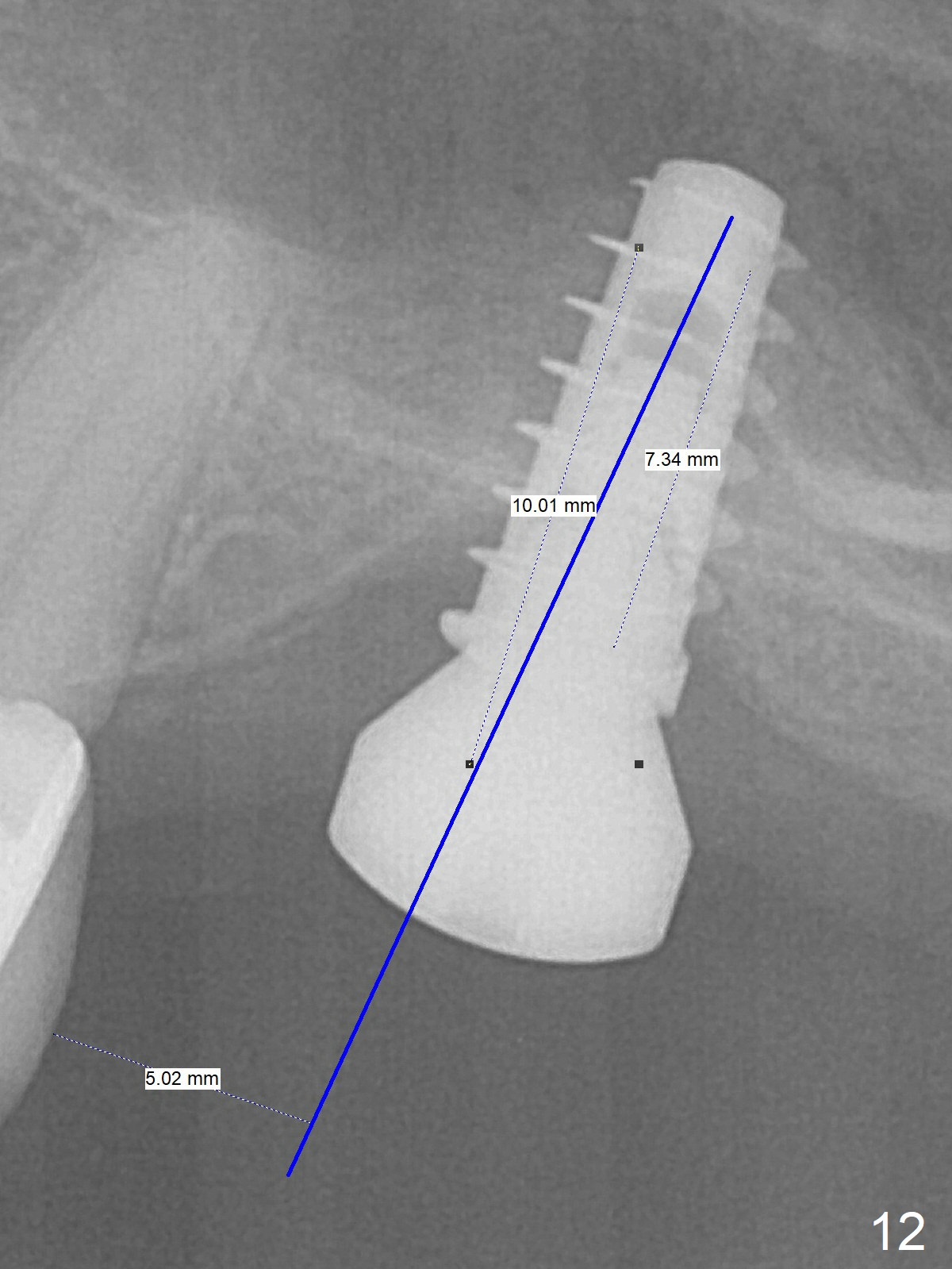
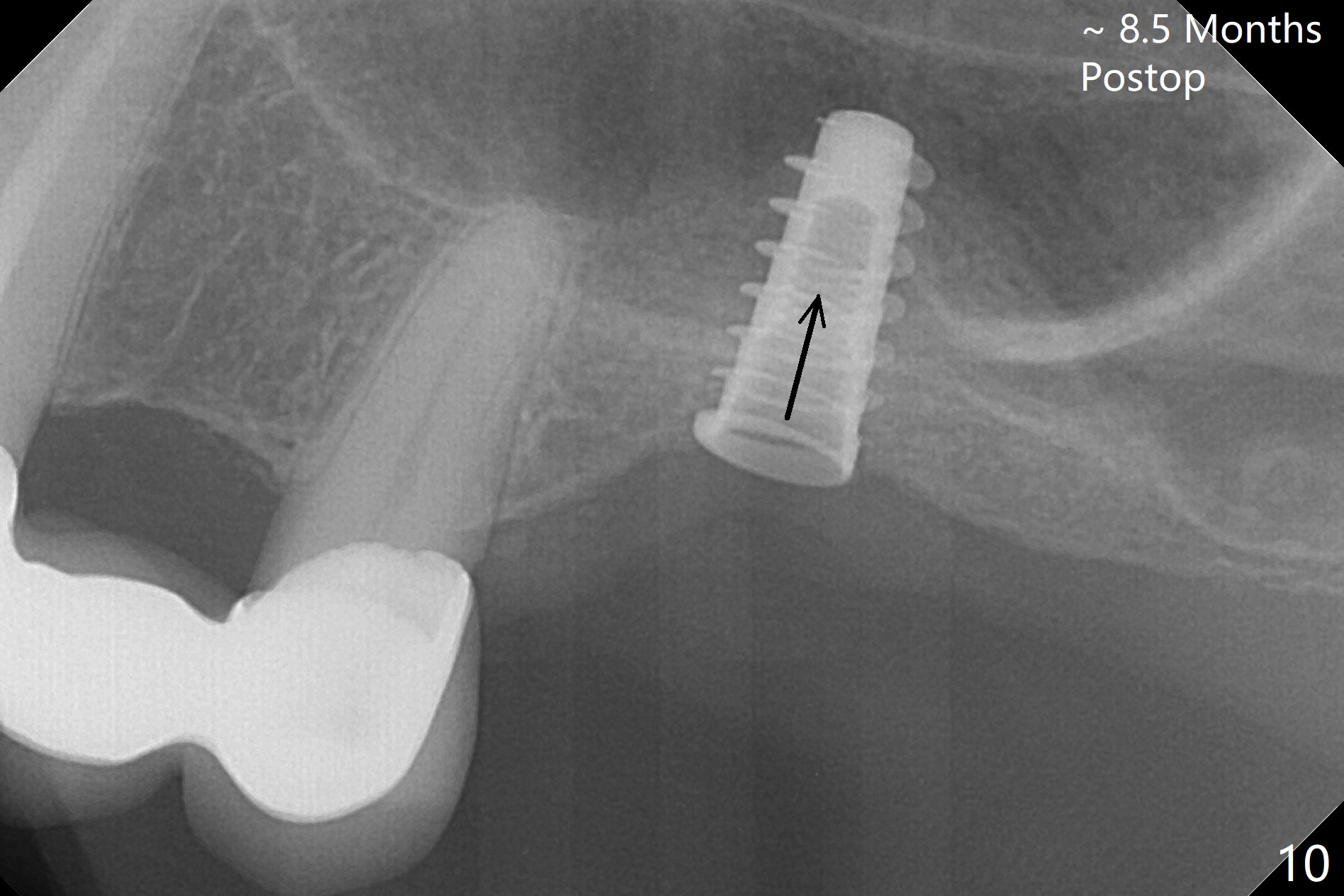
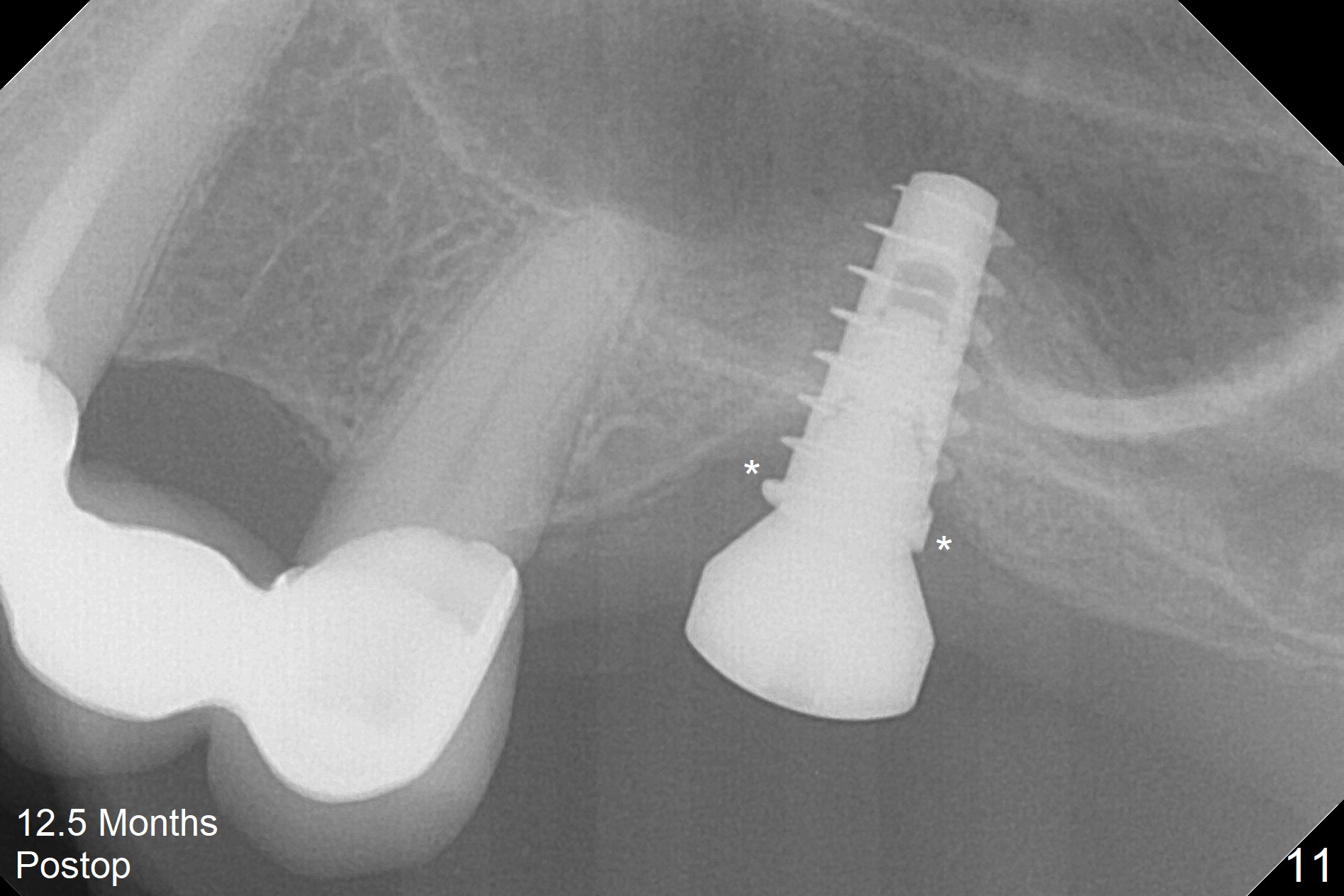
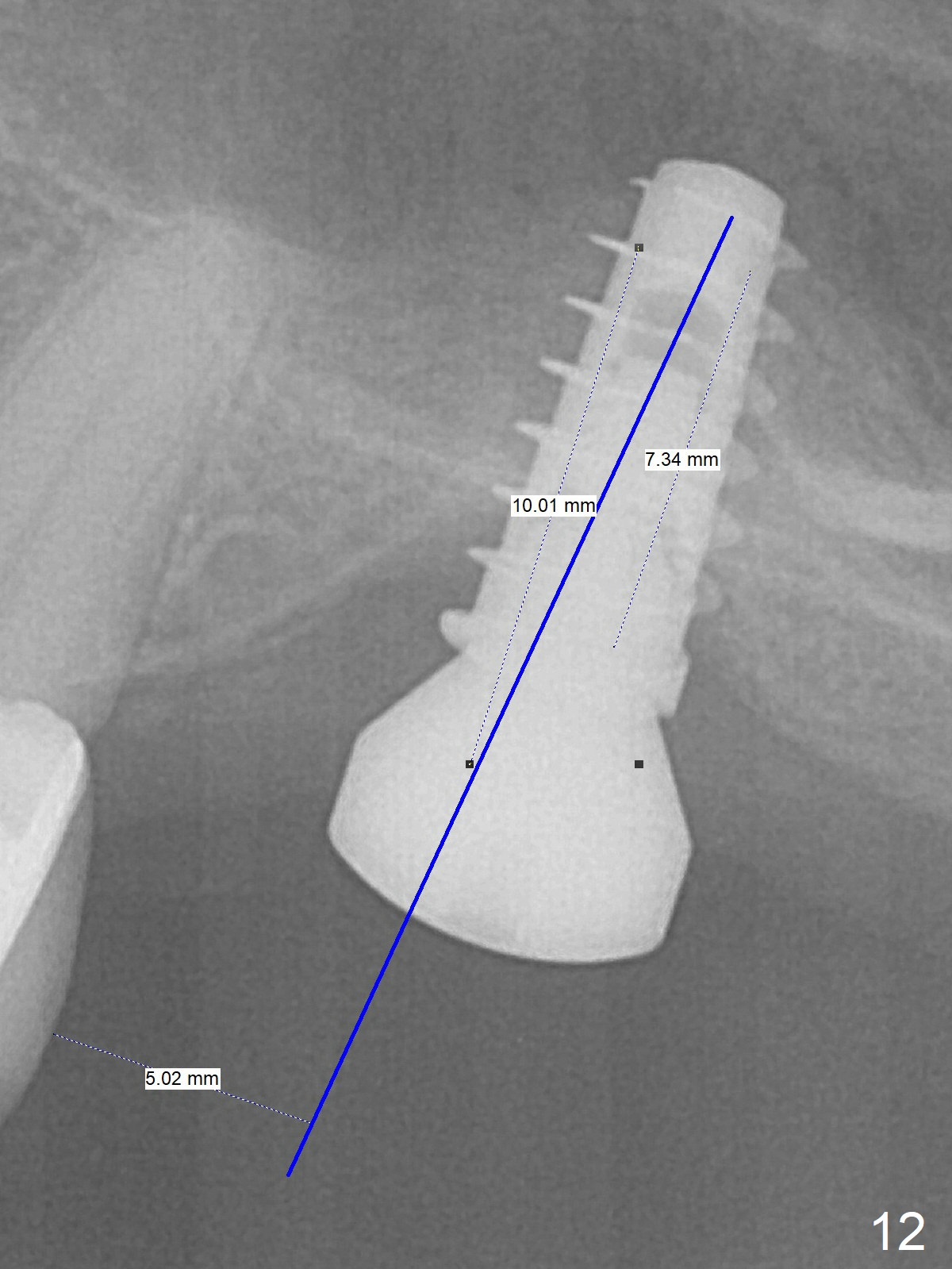
Three weeks later (approximately 8.5 months postop), the implant is found to be able to rotate when a 6.5x5.7(1) mm pair abutment is tightened with local anesthesia (there is pain associated with healing screw removal). After removal of the latter, the implant is placed deeper by hand retightening (Fig.10 arrow). Is it a better idea to use a new larger implant instead? The patient (53 years old) is scheduled to return for follow up in 3 months. In fact she returns 4 months later. The implant remains unstable and tender with loss of the crestal bone (Fig.11 *). It will be replaced with an implant (larger in diameter (5-6 mm), but shorter (7.3 mm after 5x10 mm dummy) with SLA surface after debridement and bone graft. Change the trajectory so that the coronal end will be more mesial (Fig.12 blue line). Use a healing screw and try to close the wound. In fact the patient reveals history of osteoporosis.
Return to
Upper
Molar Immediate Implant,
Course
2
3
4
CMC
提升
Xin Wei, DDS, PhD, MS 1st edition 05/08/2017, last revision 03/28/2021