







 |
 |
 |
 |
 |
 |
 |
|
 |
 |
 |
 |
 |
 |
 |
 |
Change Osteotomy Position
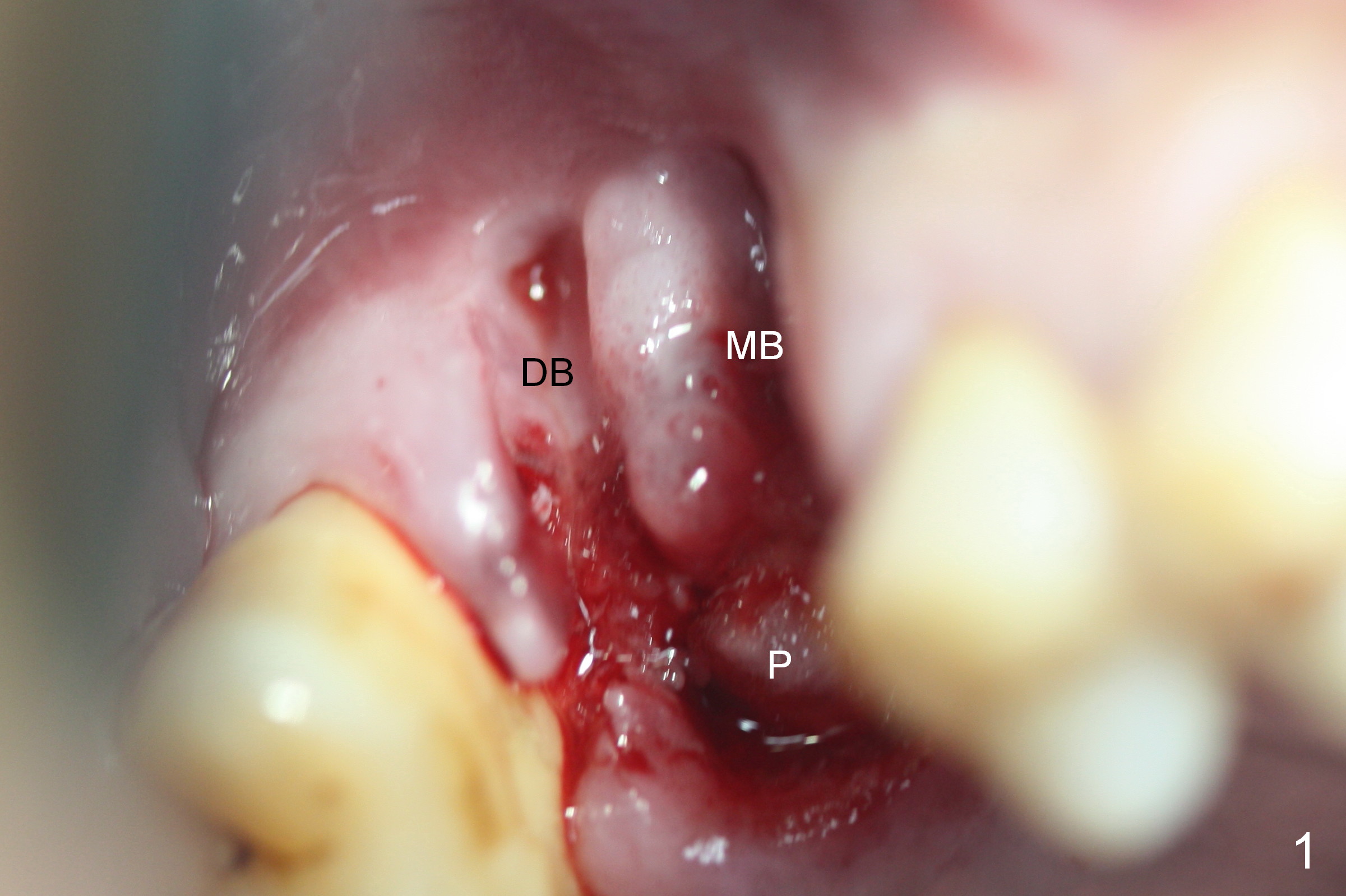
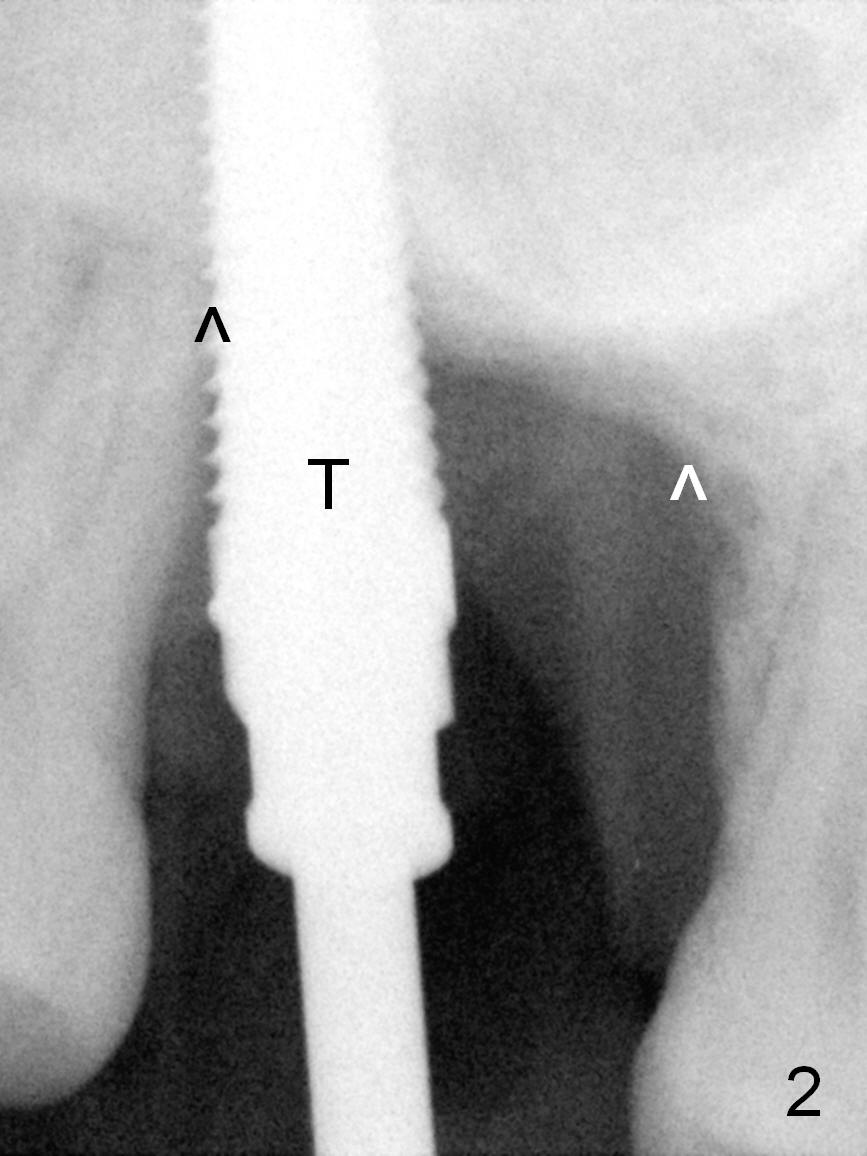
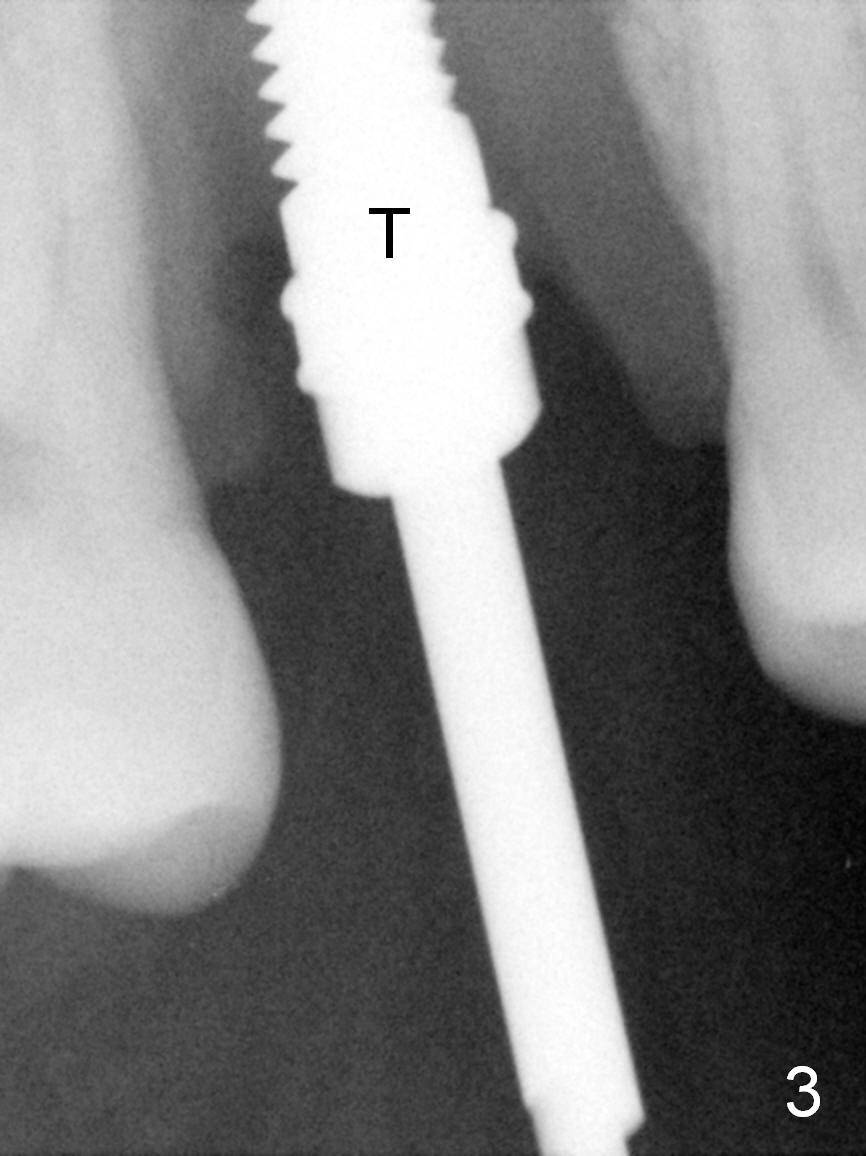
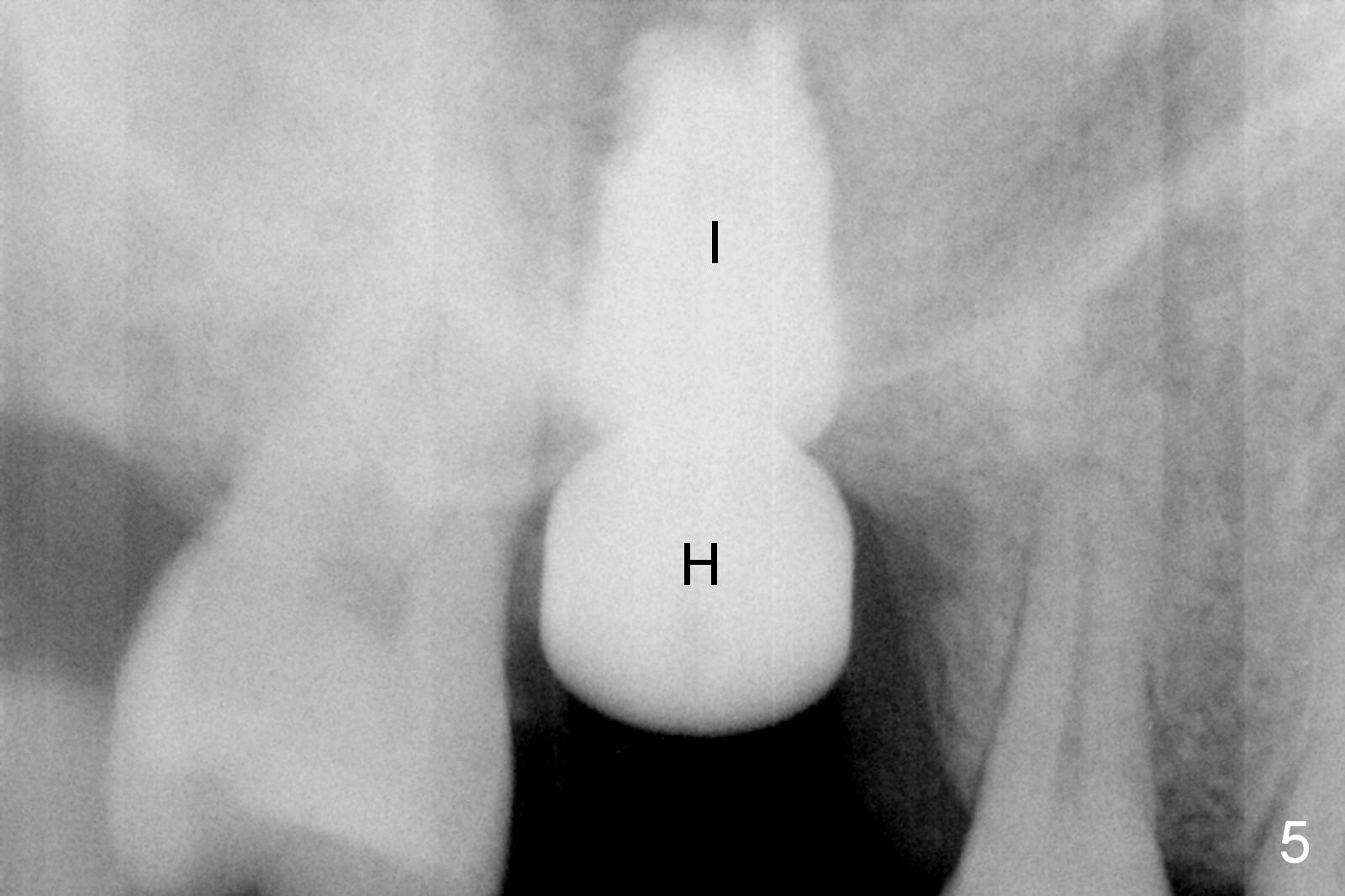
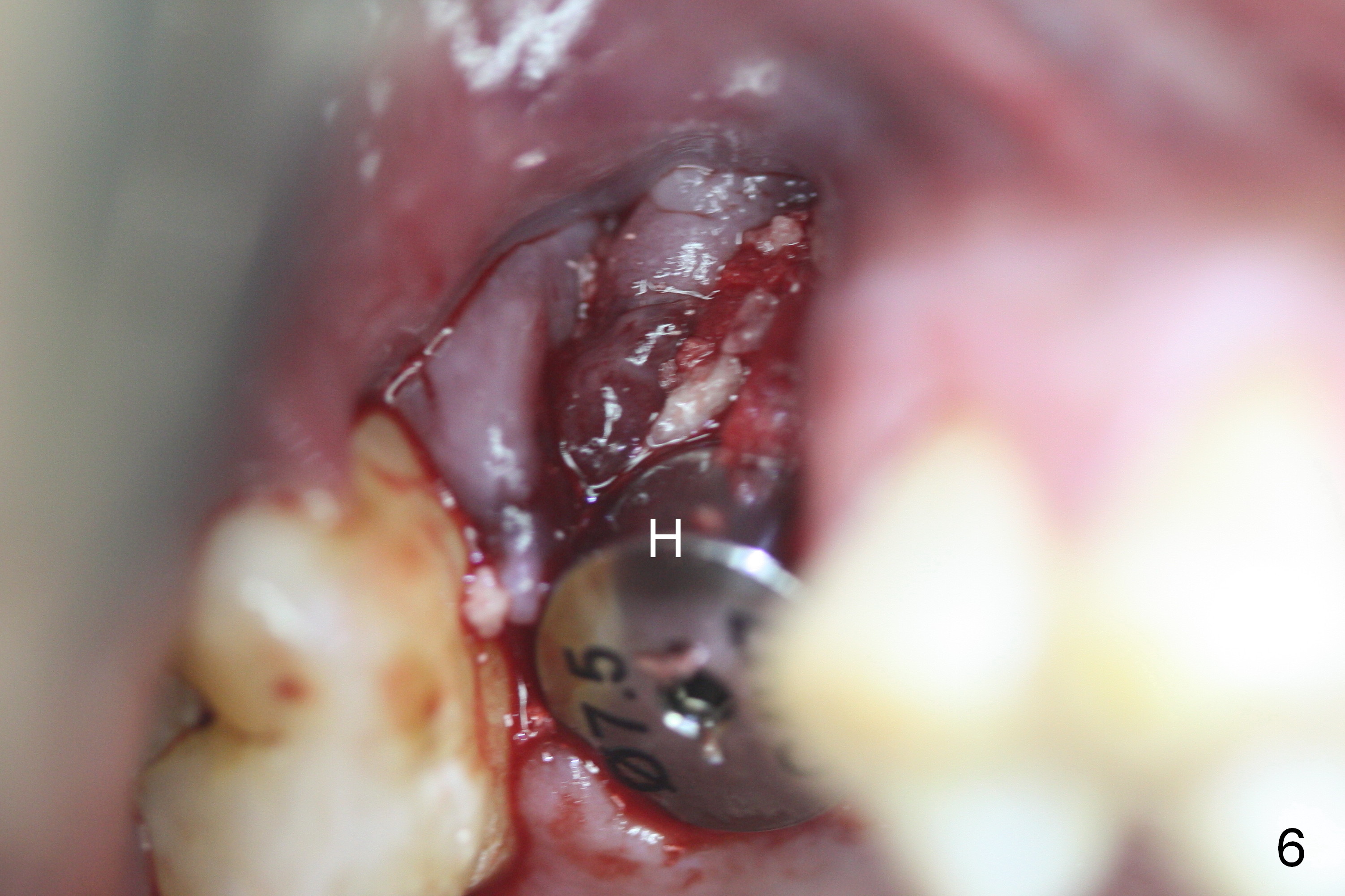
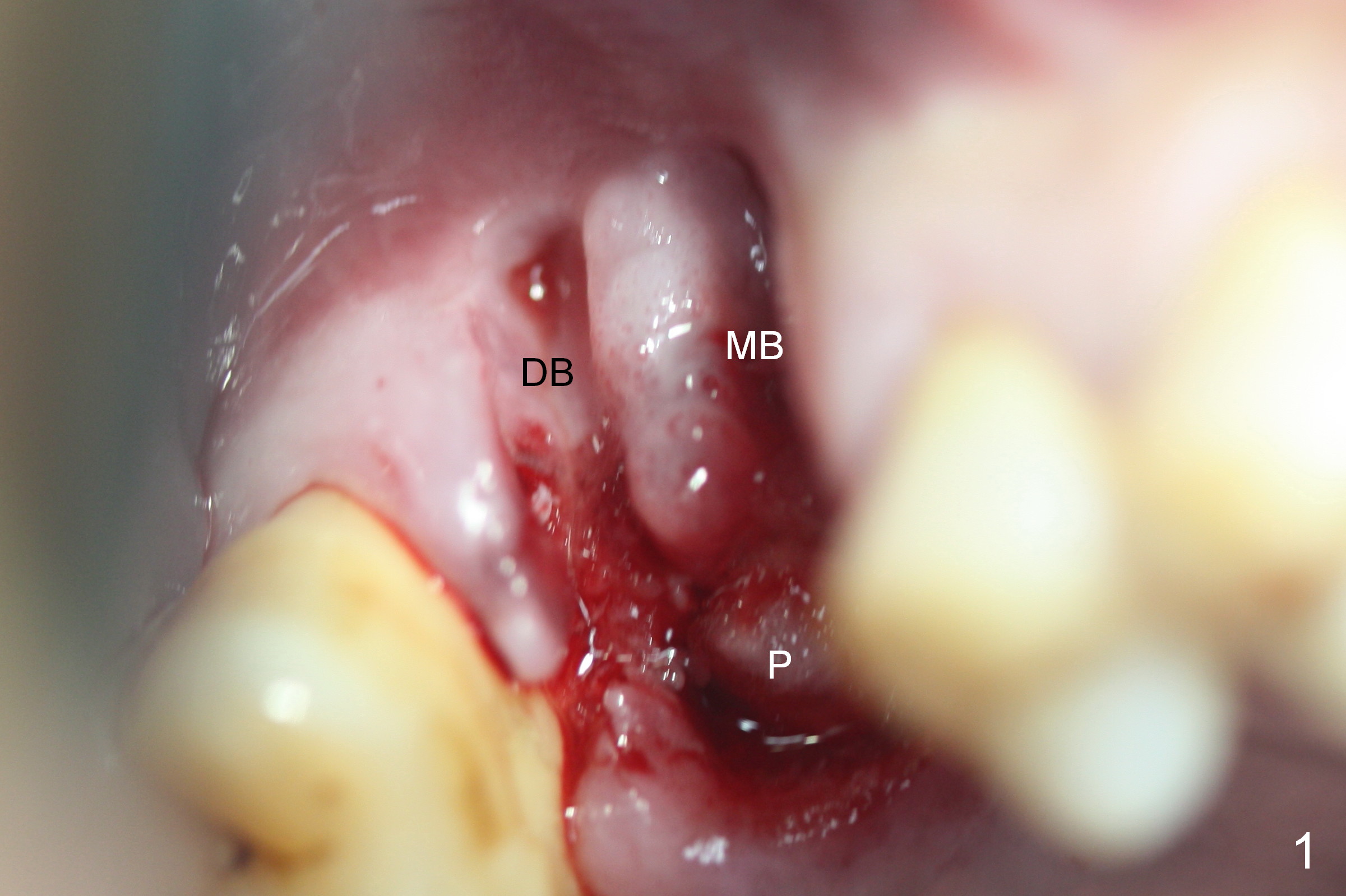
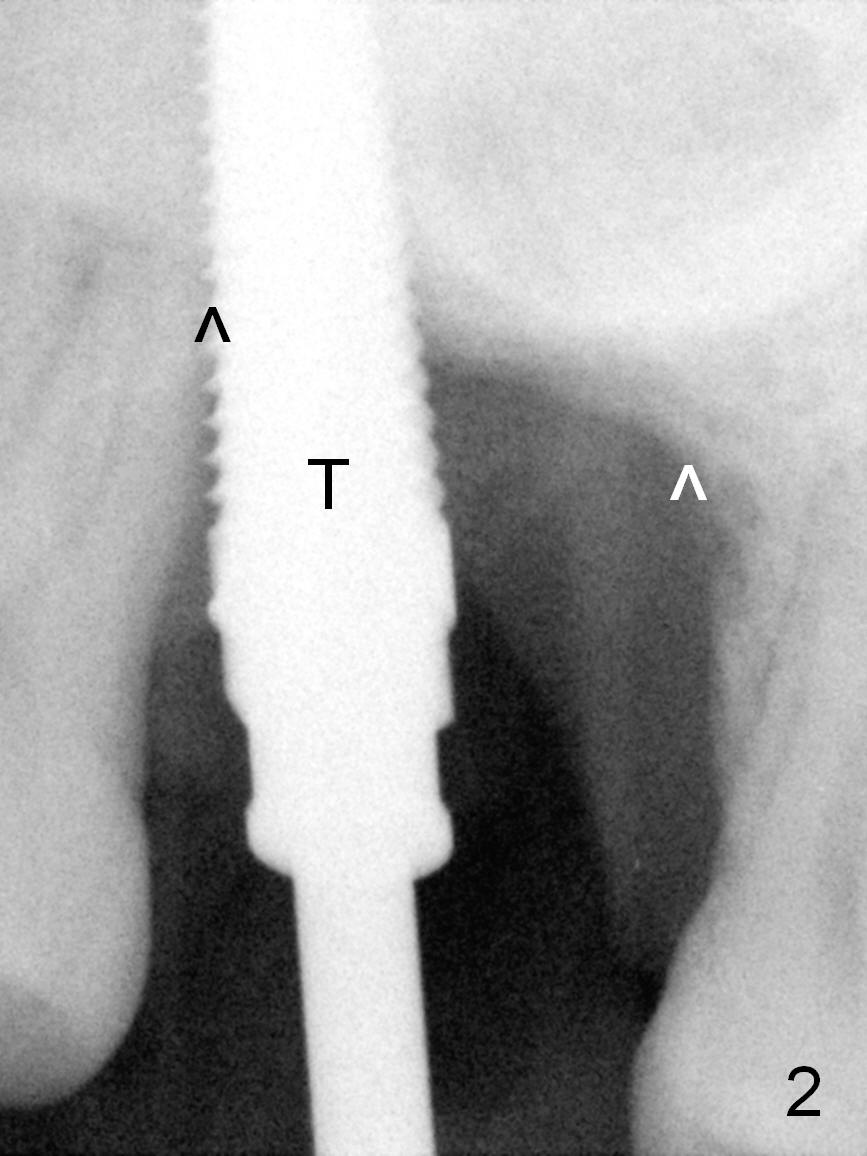
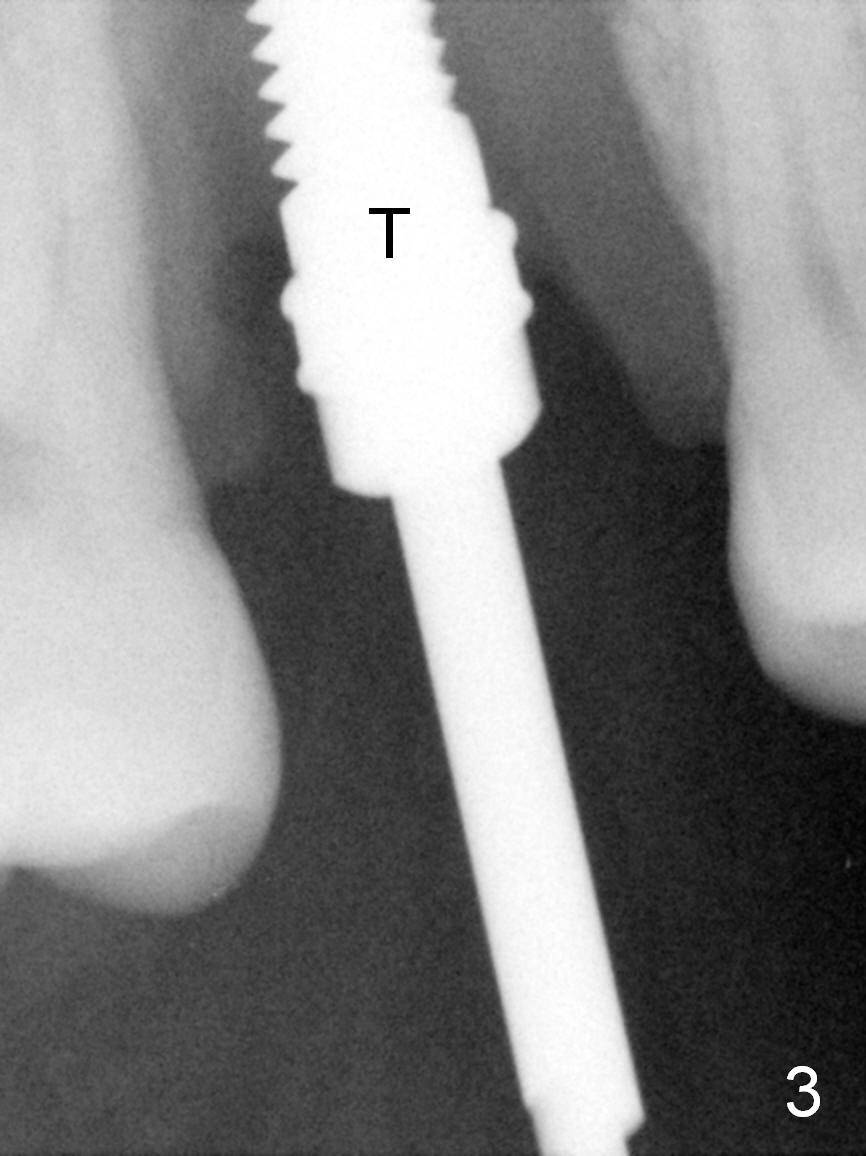
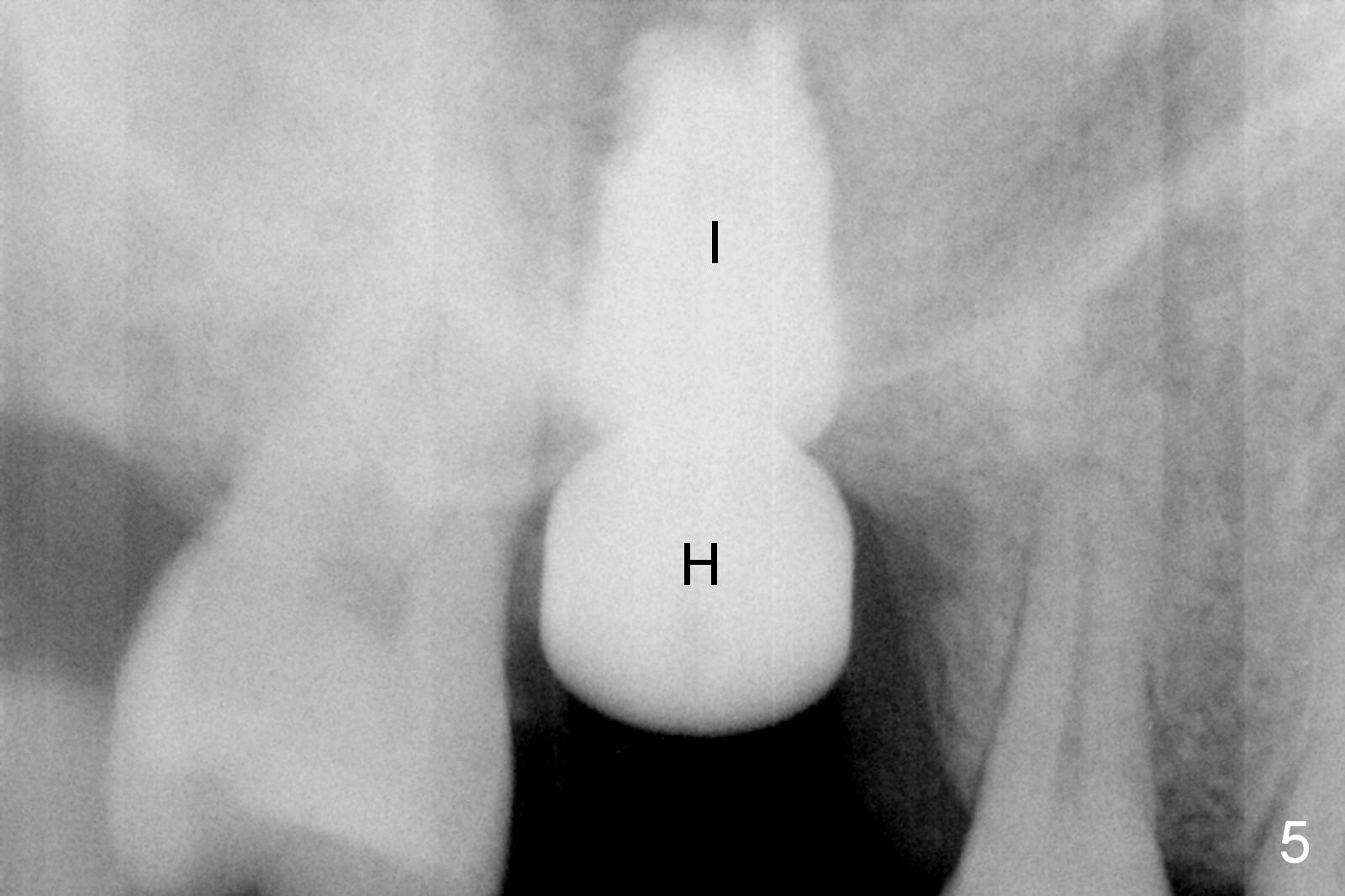
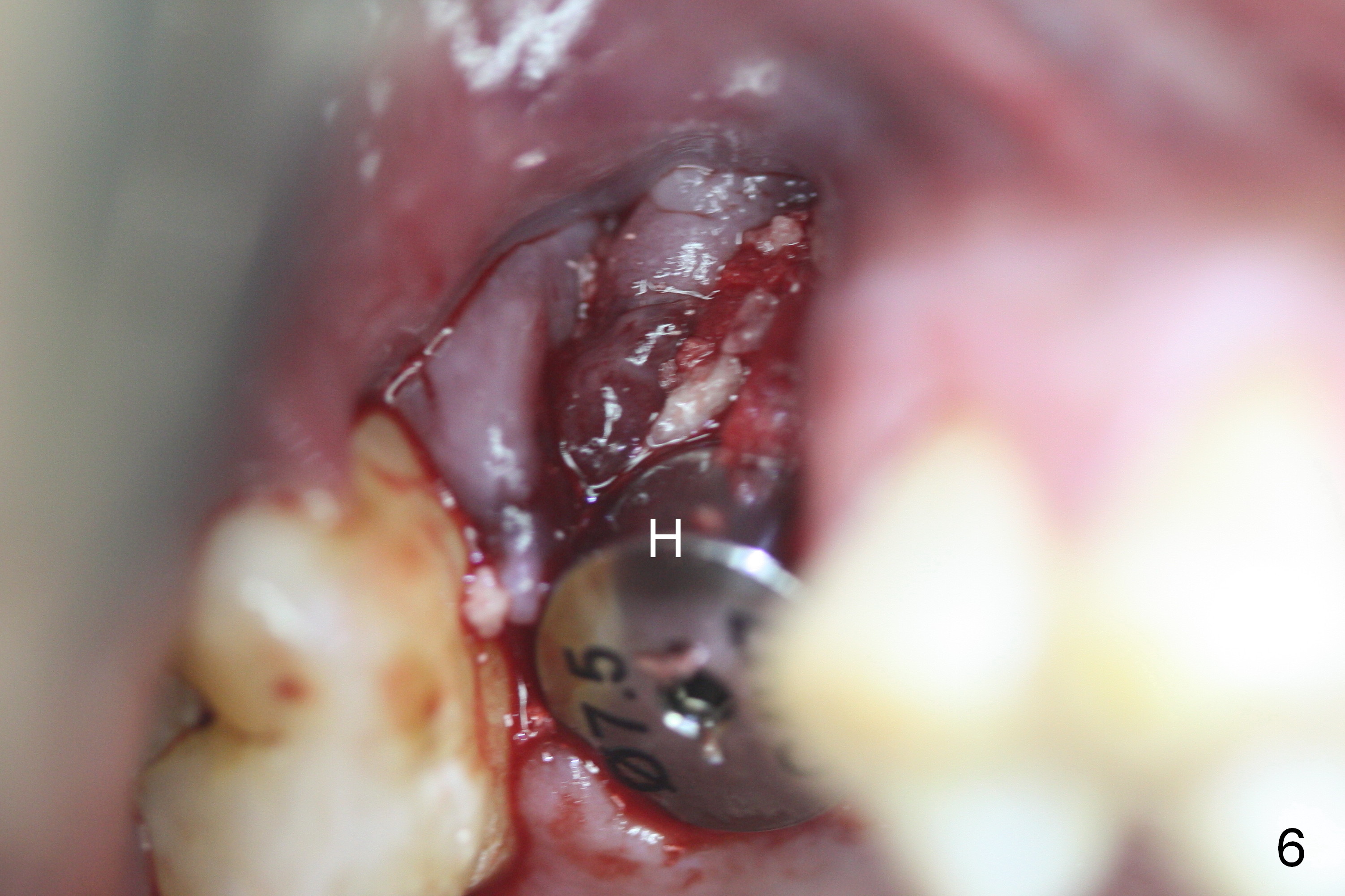
Fig.1 shows the extraction socket with 2% Xylocaine/1:50,000 Epinephrine gauze in the palatal (P) socket (MB: mesiobuccal; DB: distobuccal). The palatal socket is shallow and wide with the septal wall being lower than the the palatal wall. Osteotomy is initiated with a series of tapered osteotomes, followed by a 4.5x20 mm tap (Fig.2 T). A new osteotomy is formed mesiobuccal to the earlier one (Fig.3). At this moment, there is bone between these two osteotomies, but the last tap (4.5x20 mm) is not stable. Larger taps have to tried (6x20 mm, 7x17 mm, still not stable). Then these osteotomies have started to merge with the second one too buccal. Effort has been exerted to create a third osteotomy palatally without success; visibility is poor due to hemorrhage from the previous osteotomy sites. In spite of these maneuvers, there is no sign of sinus membrane perforation. A least tapered type of implant in the office is placed (Fig.4 I); the insertion torque is 15 Ncm; there is more bone mesially (*) than distally. No bone graft is used for sinus lift in case of sinus membrane perforation, but it is applied around the coronal portion of the implant. Healing abutment is used instead of immediate provisional (Fig.5 H: 7.5x4 mm). Perio dressing is placed to cover the wound. The dressing is dislodged 4 days; the distobuccal socket appears to have healed (Fig.8 black *), while the mesiobuccal one not (white *). New perio dressing is applied. The mesiobuccal gap is reducing with minimal implant exposure (Fig.9,10 <) 20 days postop. The patient remains asymptomatic. The implant/healing abutment remain stable. He is planning to return for follow up 3 months postop. PA or right sided panoramic X-ray will be taken. If there is no mobility of the implant, the latter will be restored permanently. A long abutment with long cuff may be used because of severe bone loss preop.
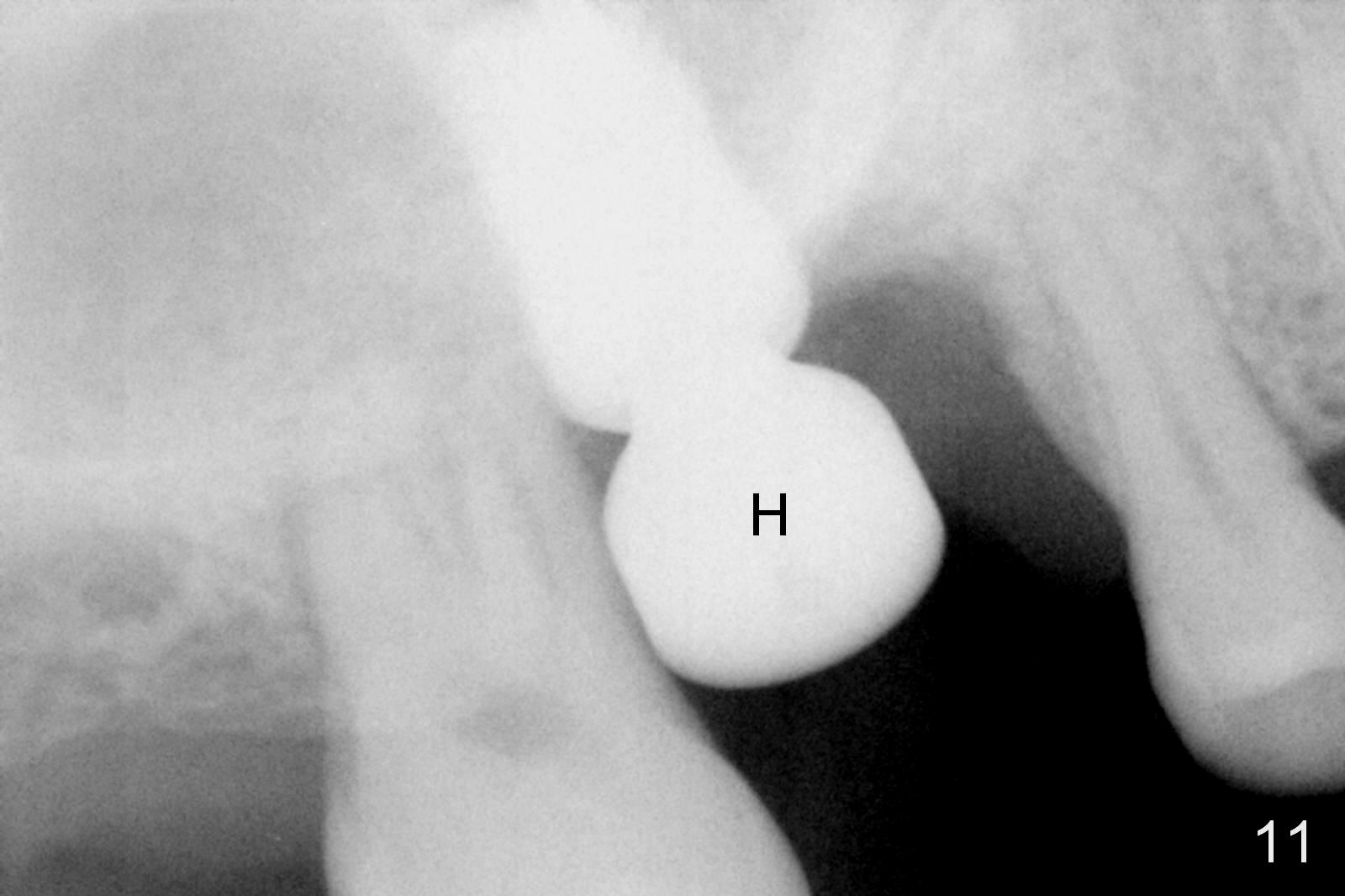
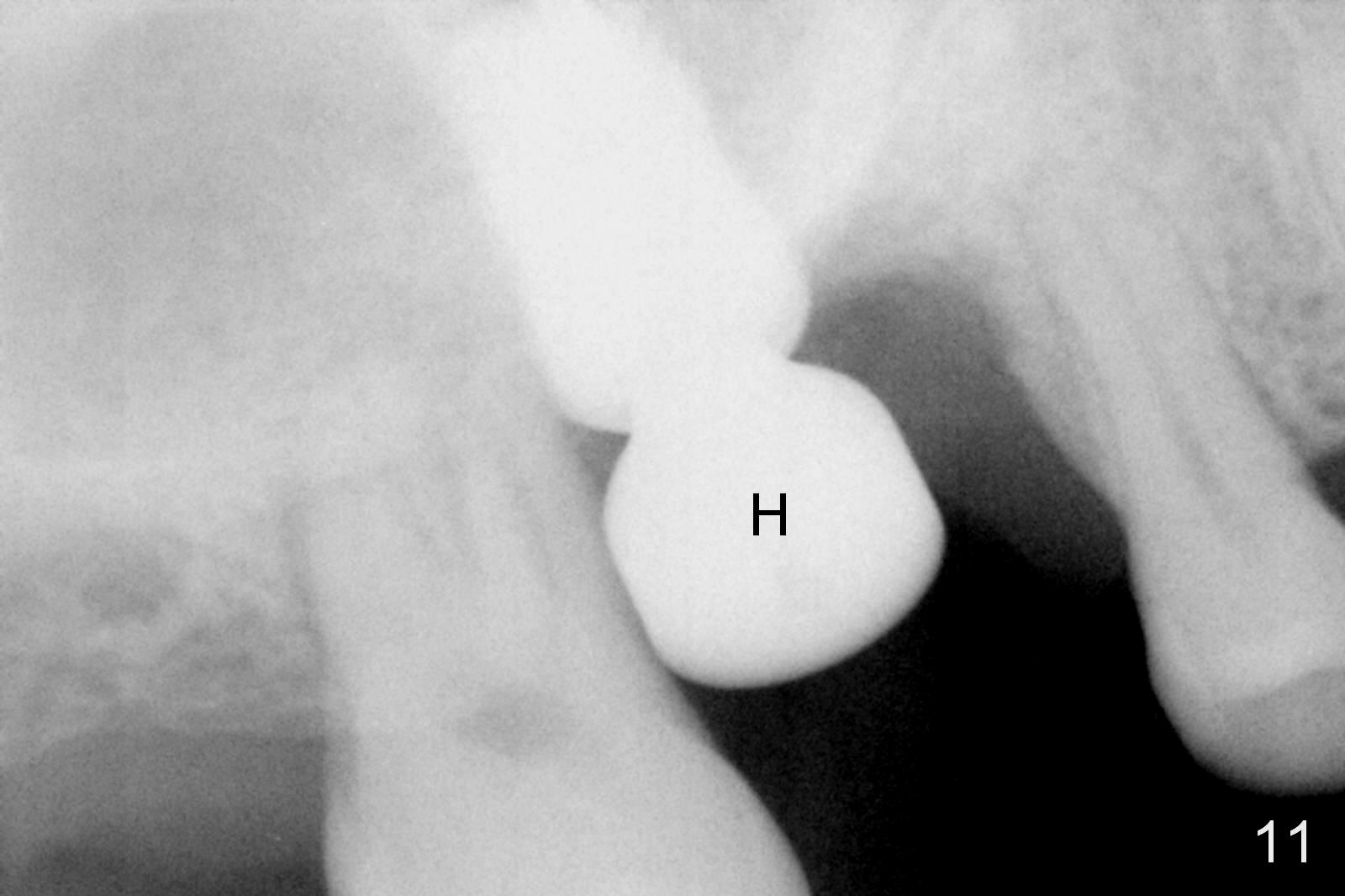
There is no abnormal bone loss around the implant 2.5 months postop (Fig.11 (H: healing abutment)). When the healing abutment is removed 3 months postop, the surrounding gingiva looks healthy (Fig.12).
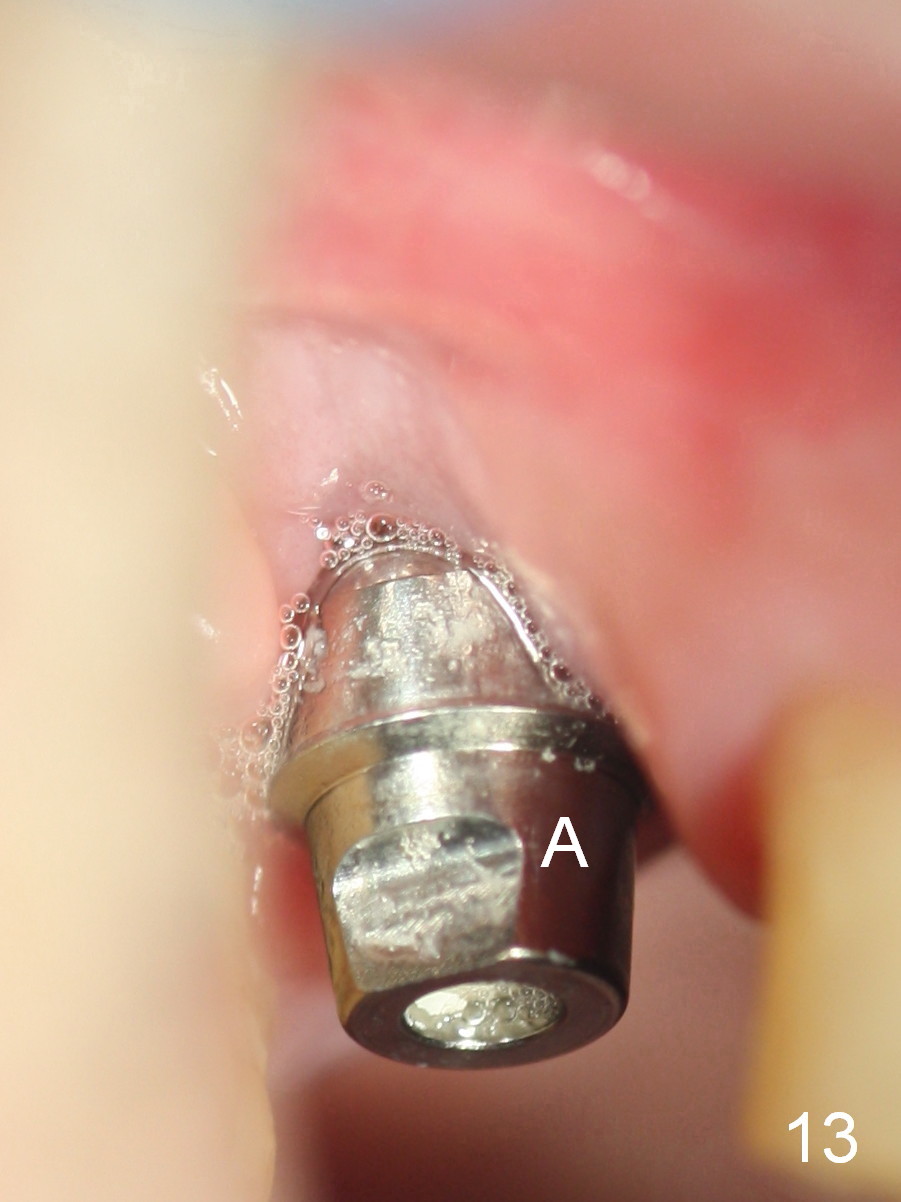
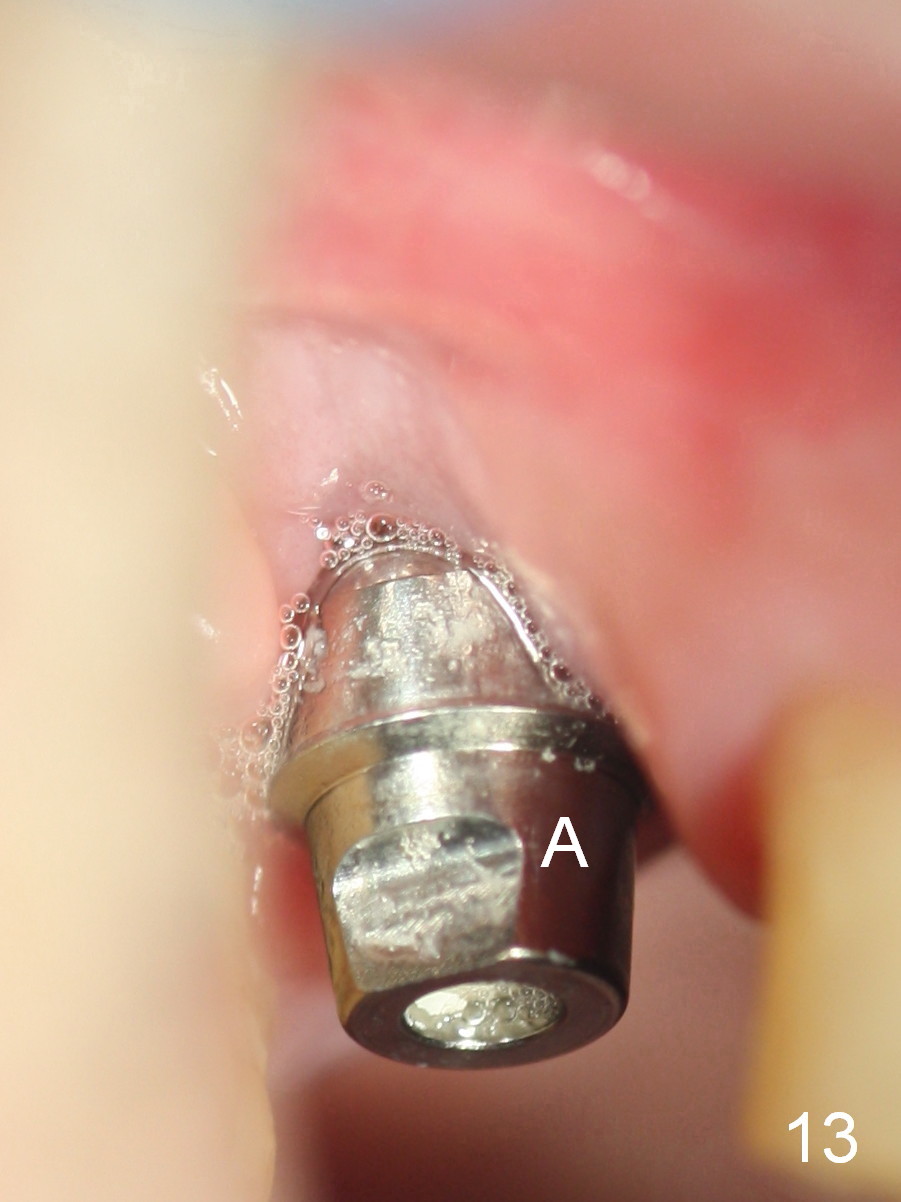
Two weeks later, the patient returns for crown try in. There is mild tenderness over the buccal gingiva, suggesting that the periosteum directly contacts the implant surface (loss of bone graft during healing). Except buccal gingival defect (Fig.13), there is no abnormality around the abutment buccally or palatally (Fig.14 A).
Four weeks post cementation, the patient keeps complaining light tenderness over the buccal gingiva, although the latter remains apparently healthy (Fig.15). A buccal sulcus incision will be made to expose the buccal threads. If the threads are not covered by the bone, place bone graft. Use Titanium brush if needed. Apply Metronidazole. Use a 2nd #15 blade to harvest a palatal graft. Place Hemostatic gauze in the donor site, followed by suture fixation. Open Periodontal Surgery Cassette and use periodontal scaler for #2 and 4. Apply Endogain if necessary. The defect is most likely associated with substantial bony element. No bone, no attachment.
Return to Upper Molar Immediate Implant,
Systemic Diseases
Xin Wei, DDS, PhD, MS 1st edition 08/15/2015, last revision 04/28/2018