

,%20graft.jpg)

 |
 |
 |
 |
 |
|
 |
 |
 |
 |
 |
|
,%20graft.jpg) |
 |
 |
 |
||
 |
|||||
Septal Slope of Upper 2nd Molar
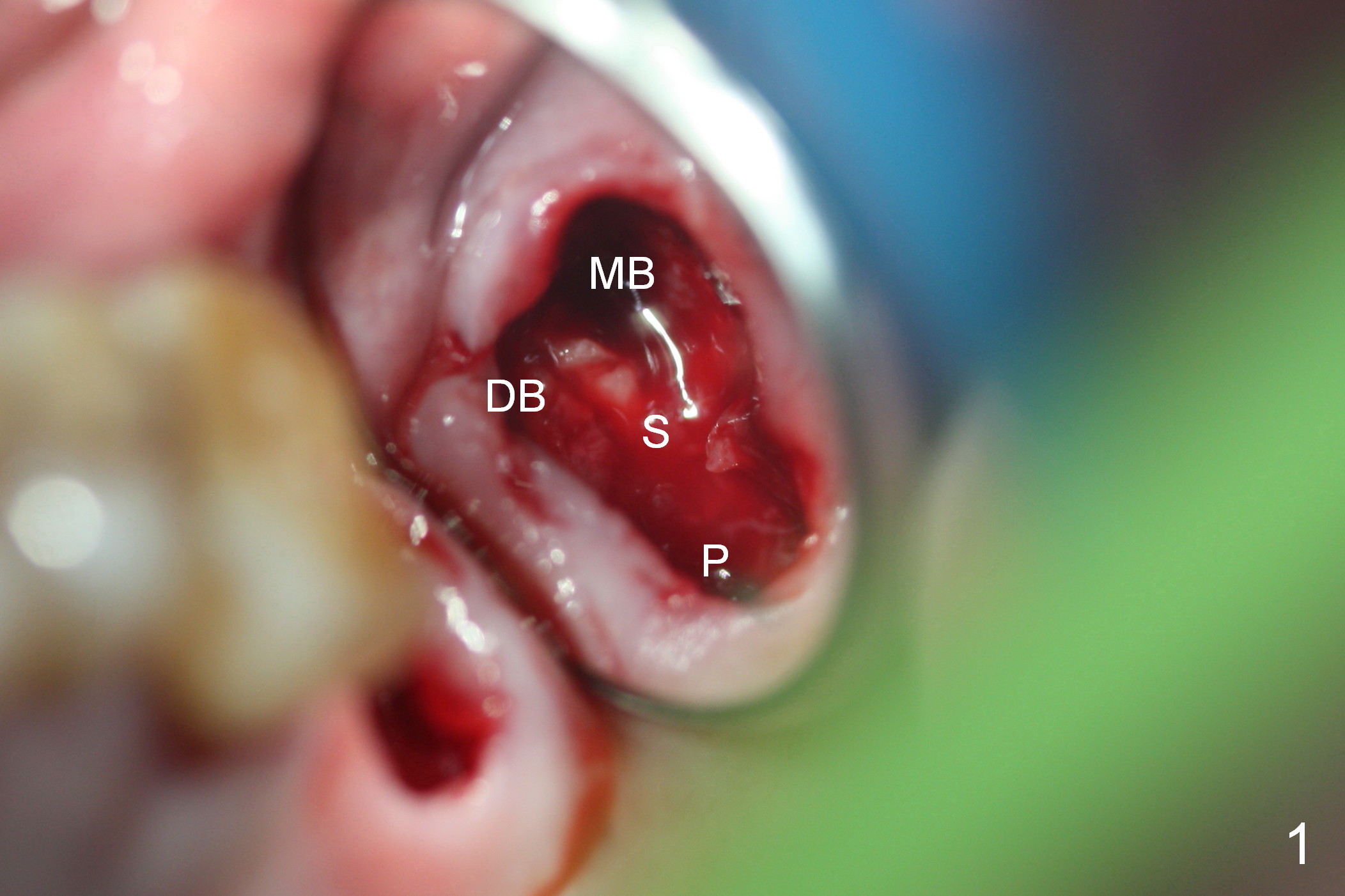
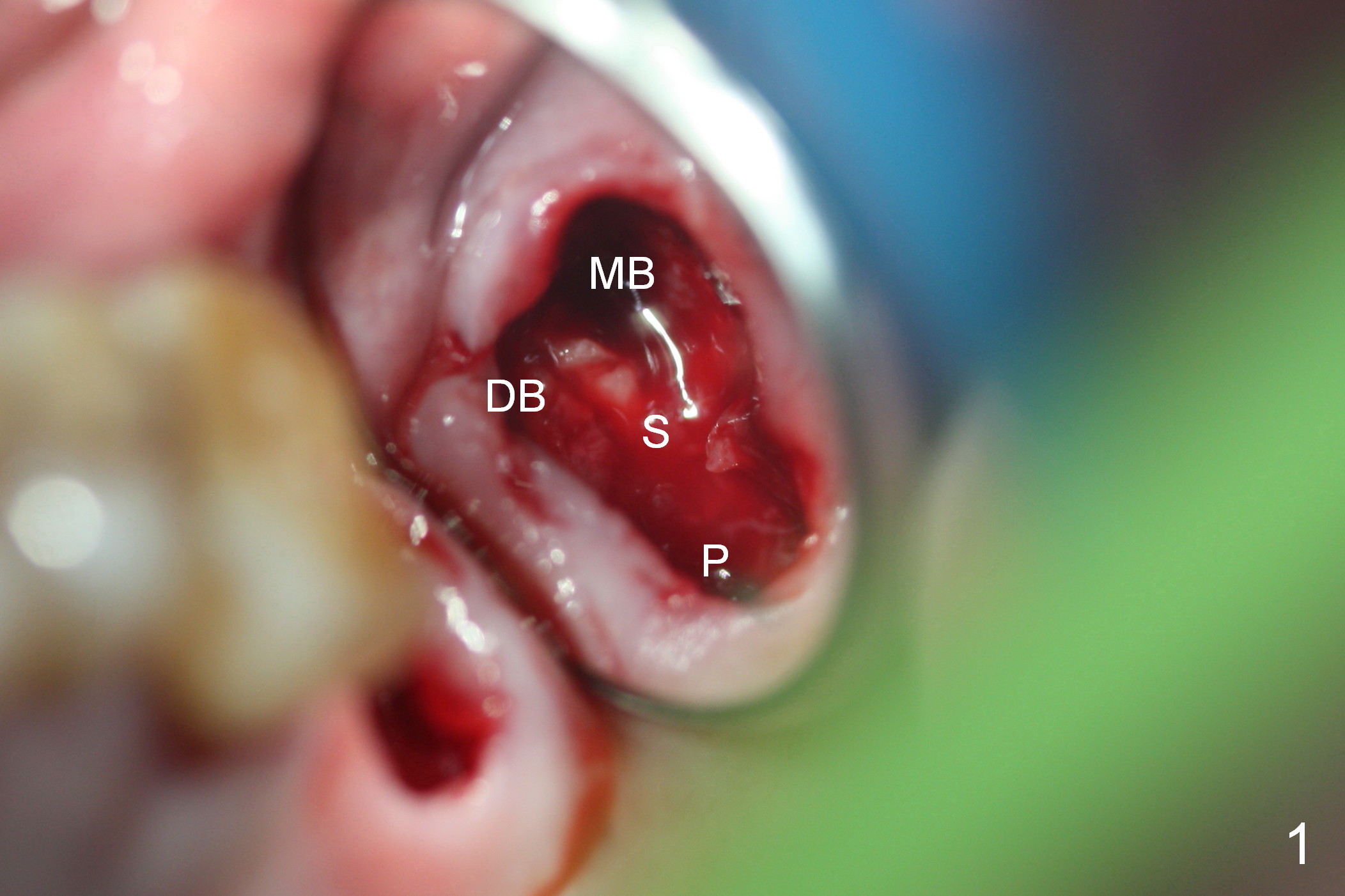
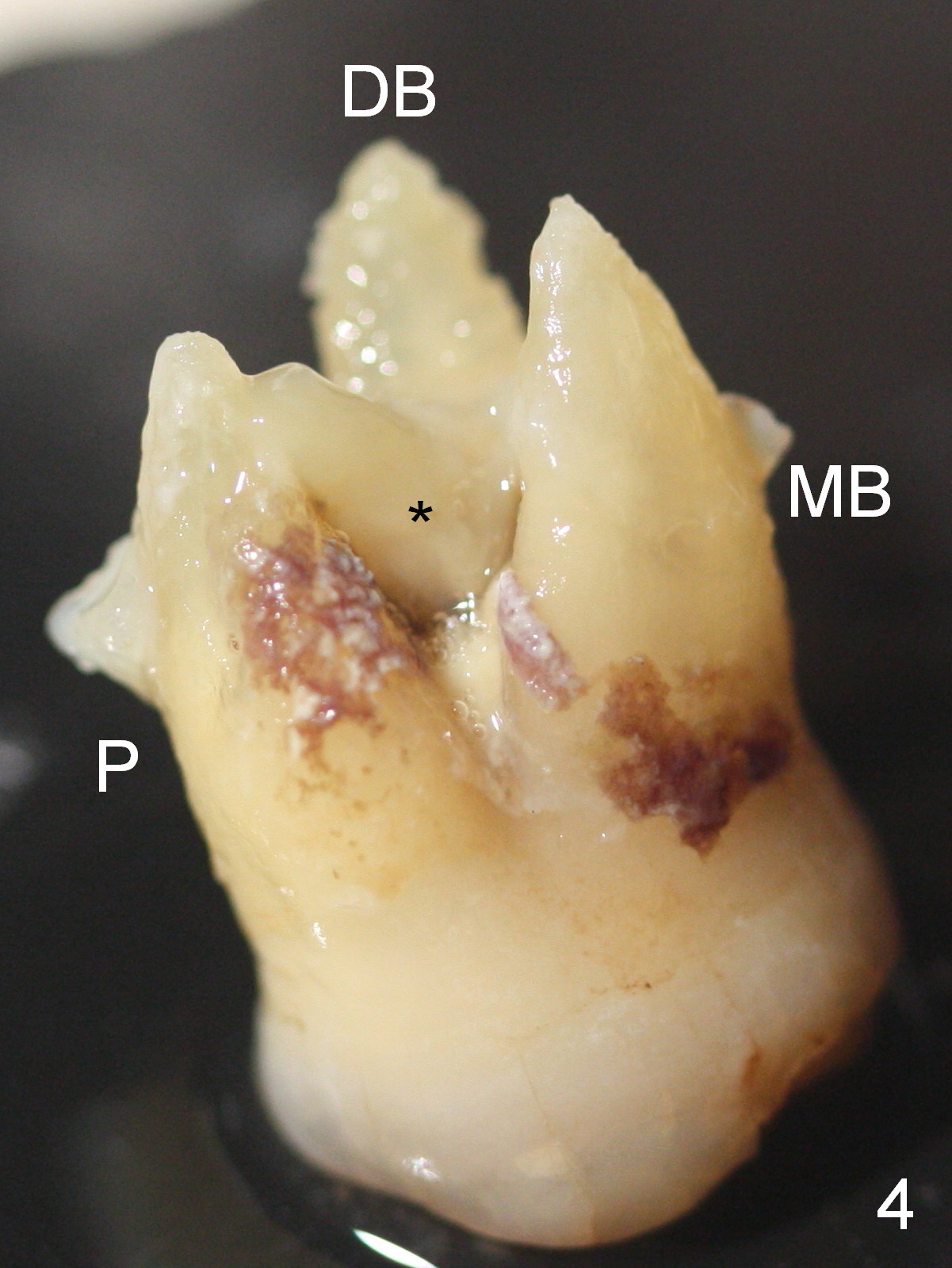
When the maxillary 2nd molar is extracted, there are 3 distinct sockets (mesiobuccal (Fig.1 MB), distobuccal (DB) and palatal (P); the septum (S) is large and oblique (so called septal slope). Most of the upper 2nd molars have less furcation with smaller septum.
Osteotomy starts buccomesial to the middle of the septal slope (Fig.2 white circle). As the osteotomy enlarges sequentially, it shifts more or less to the center of the socket (Fig.3 yellow circle).
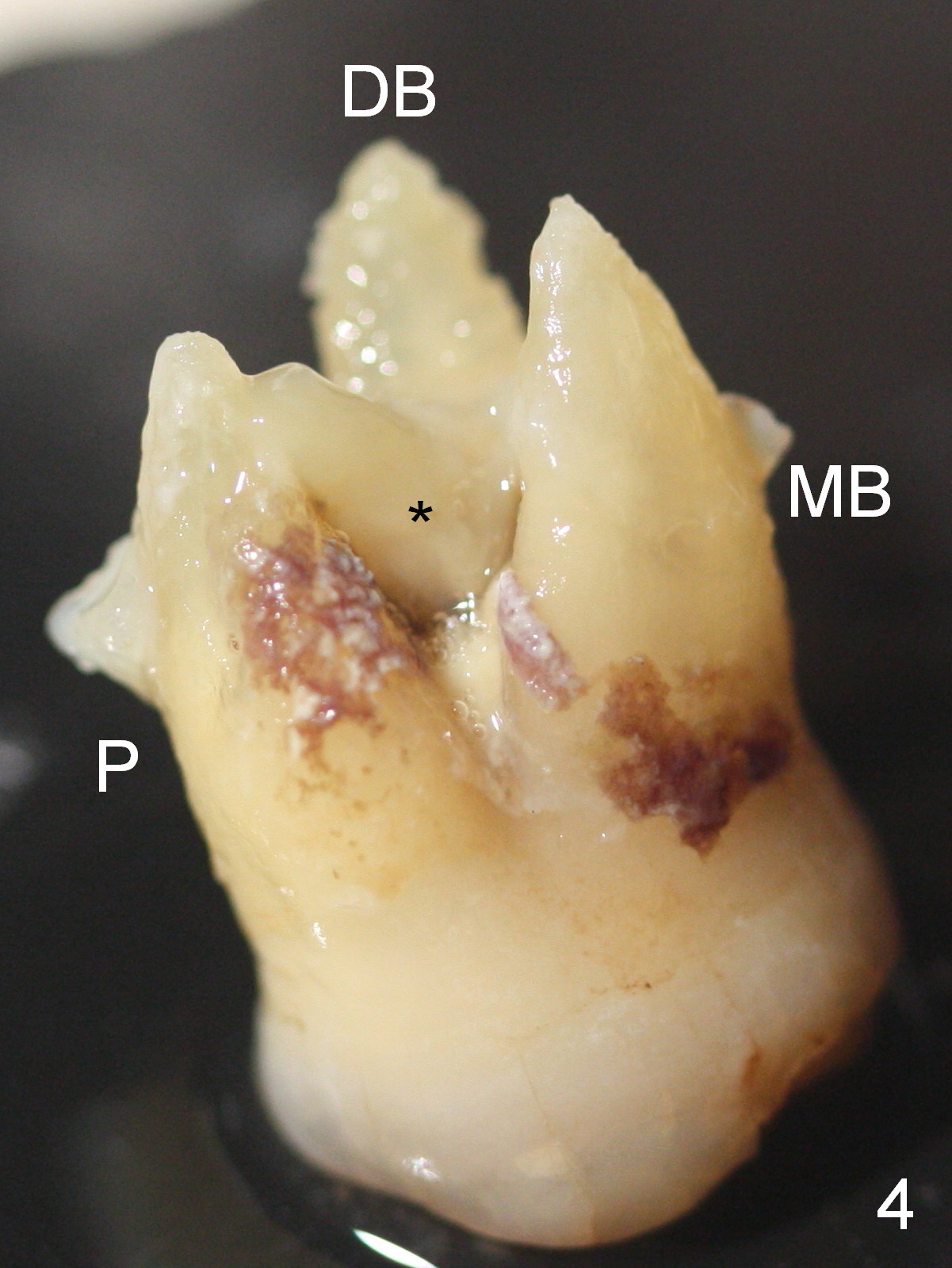
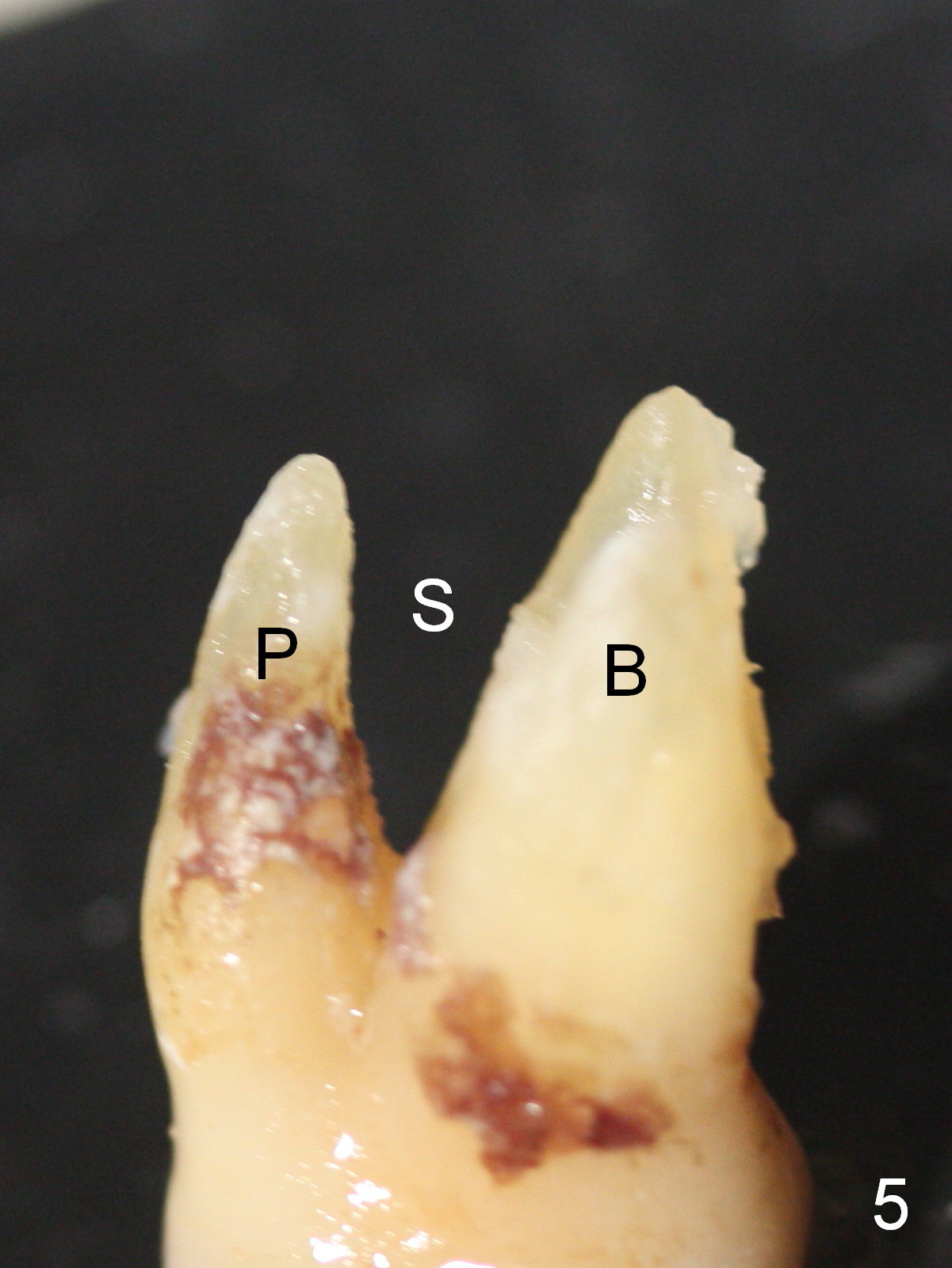
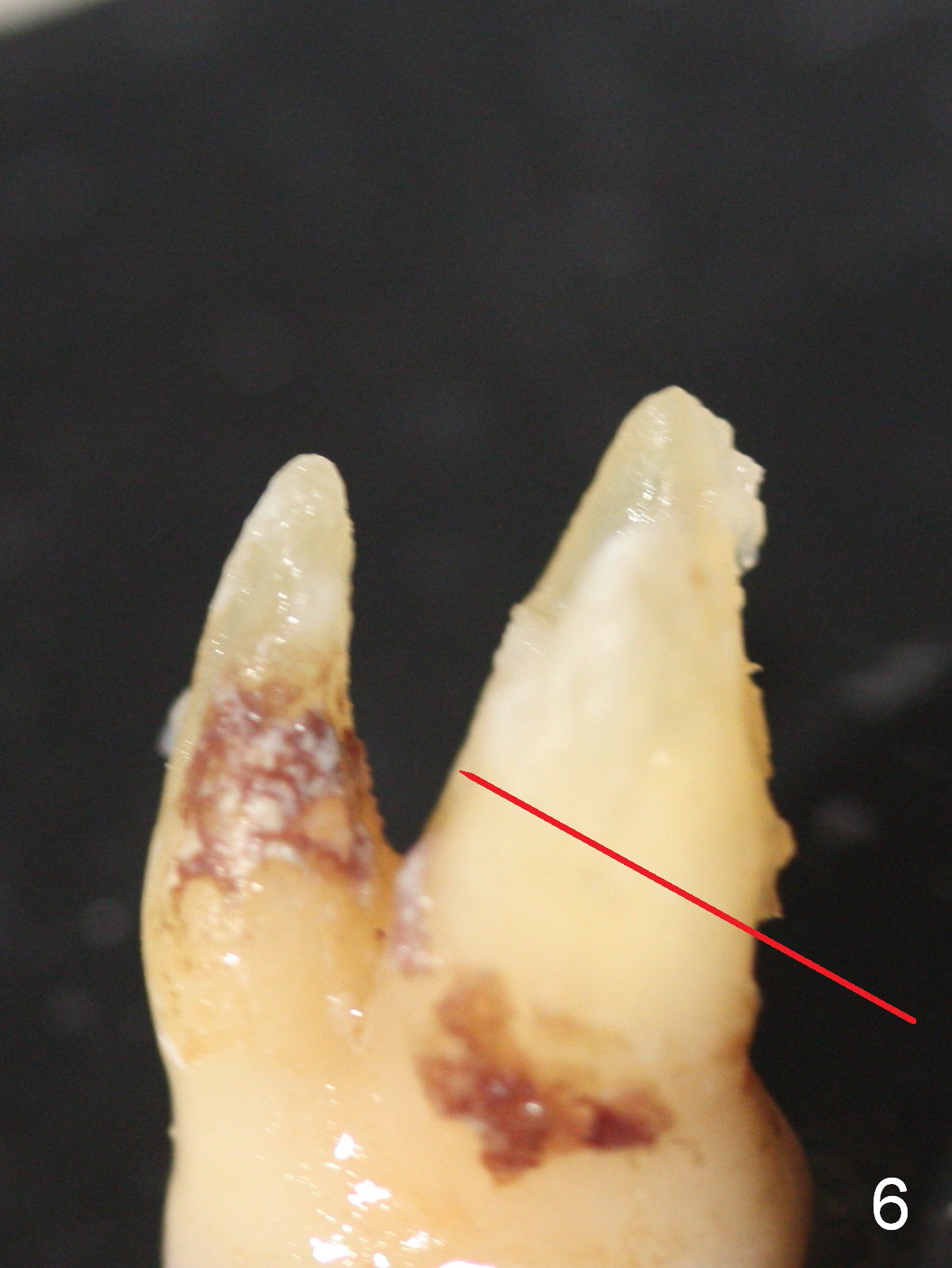
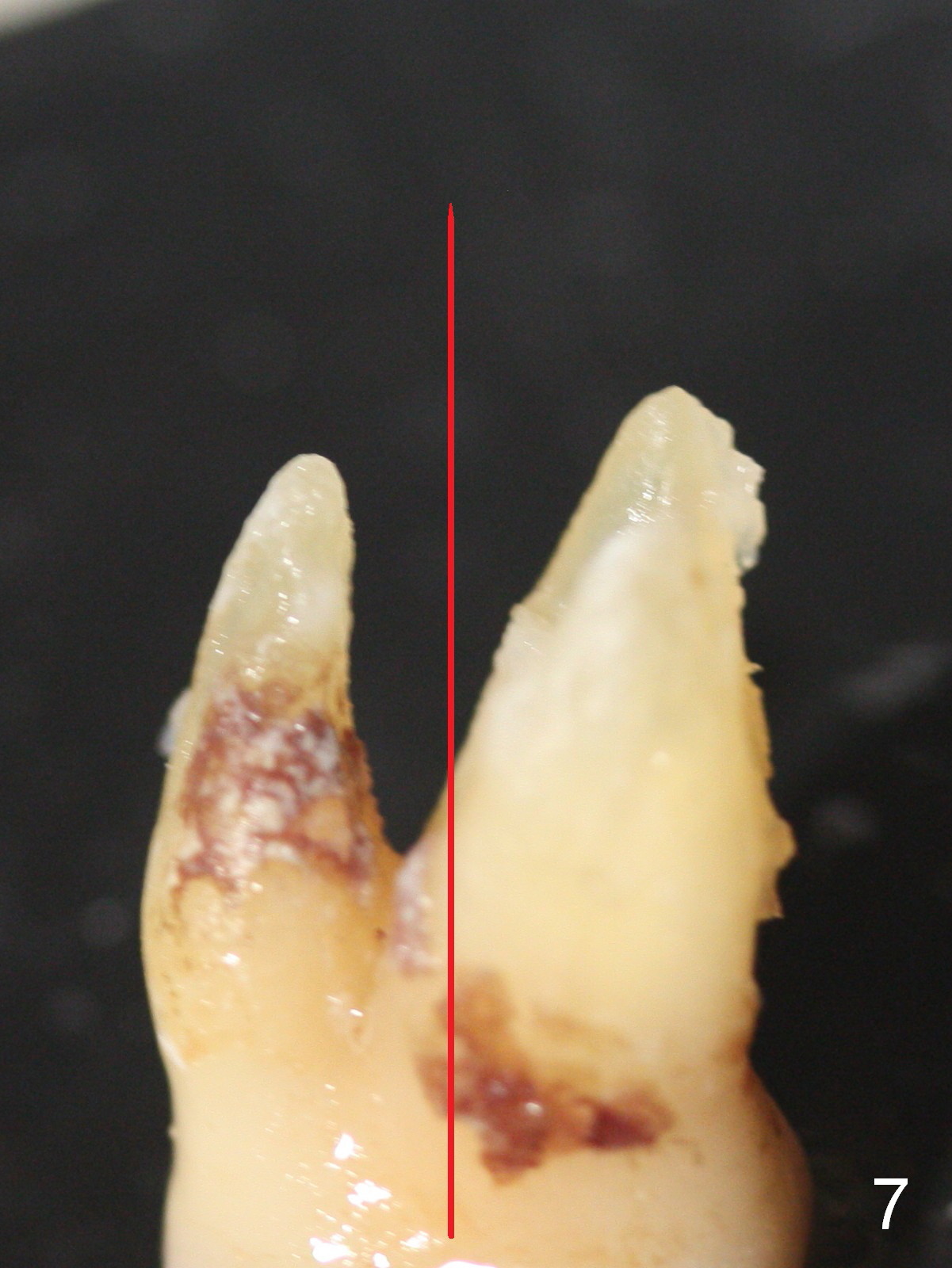
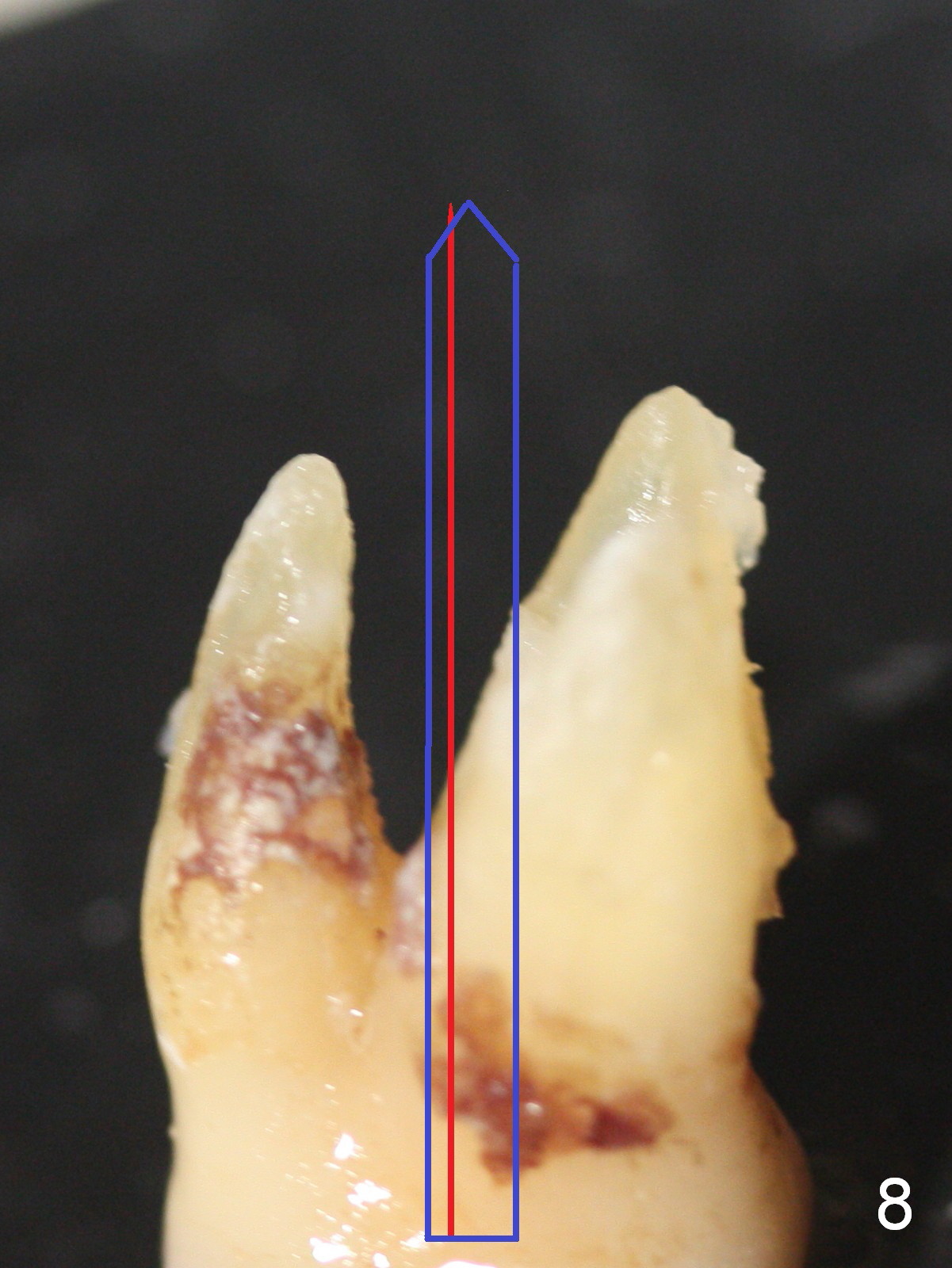
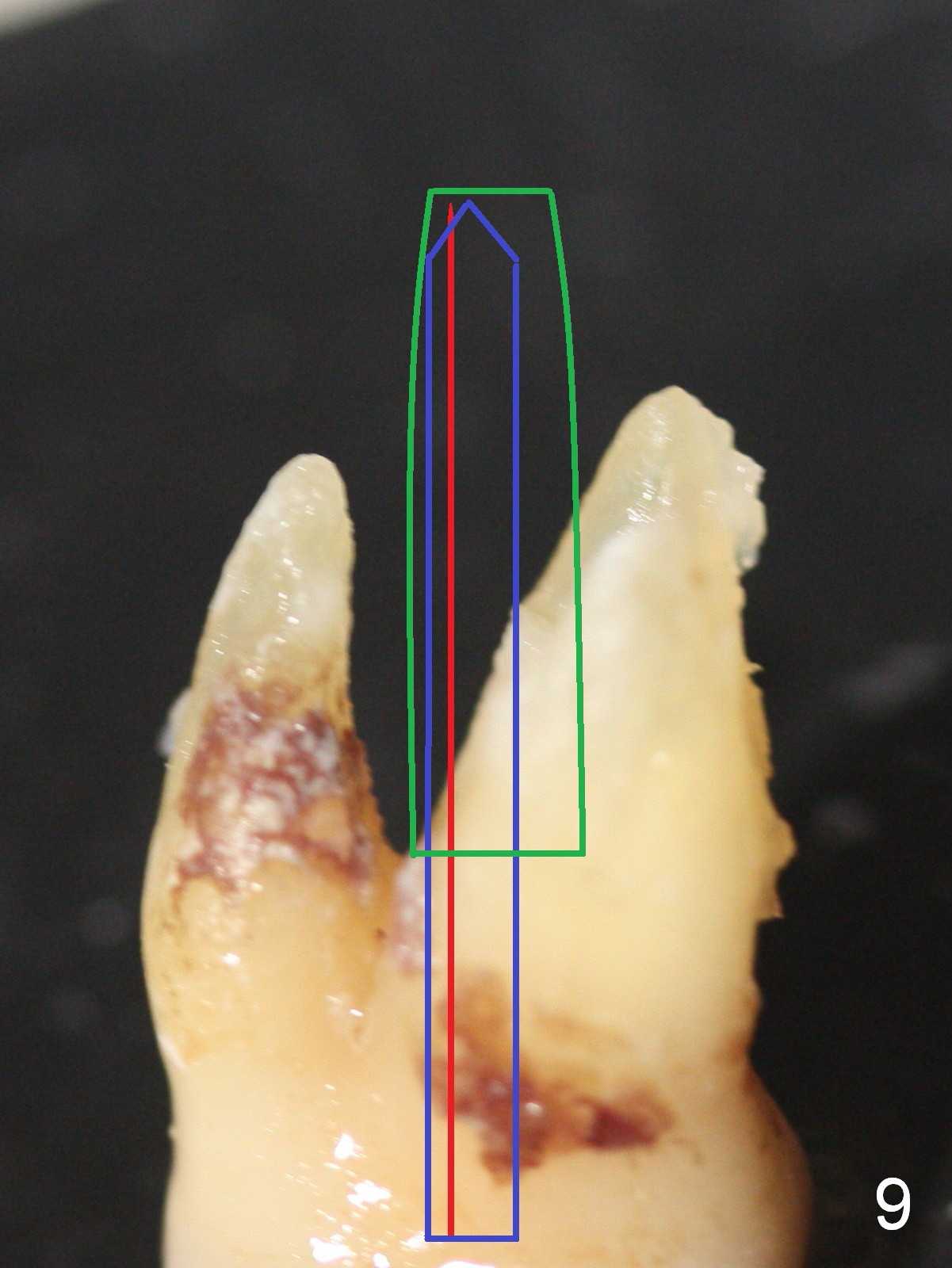
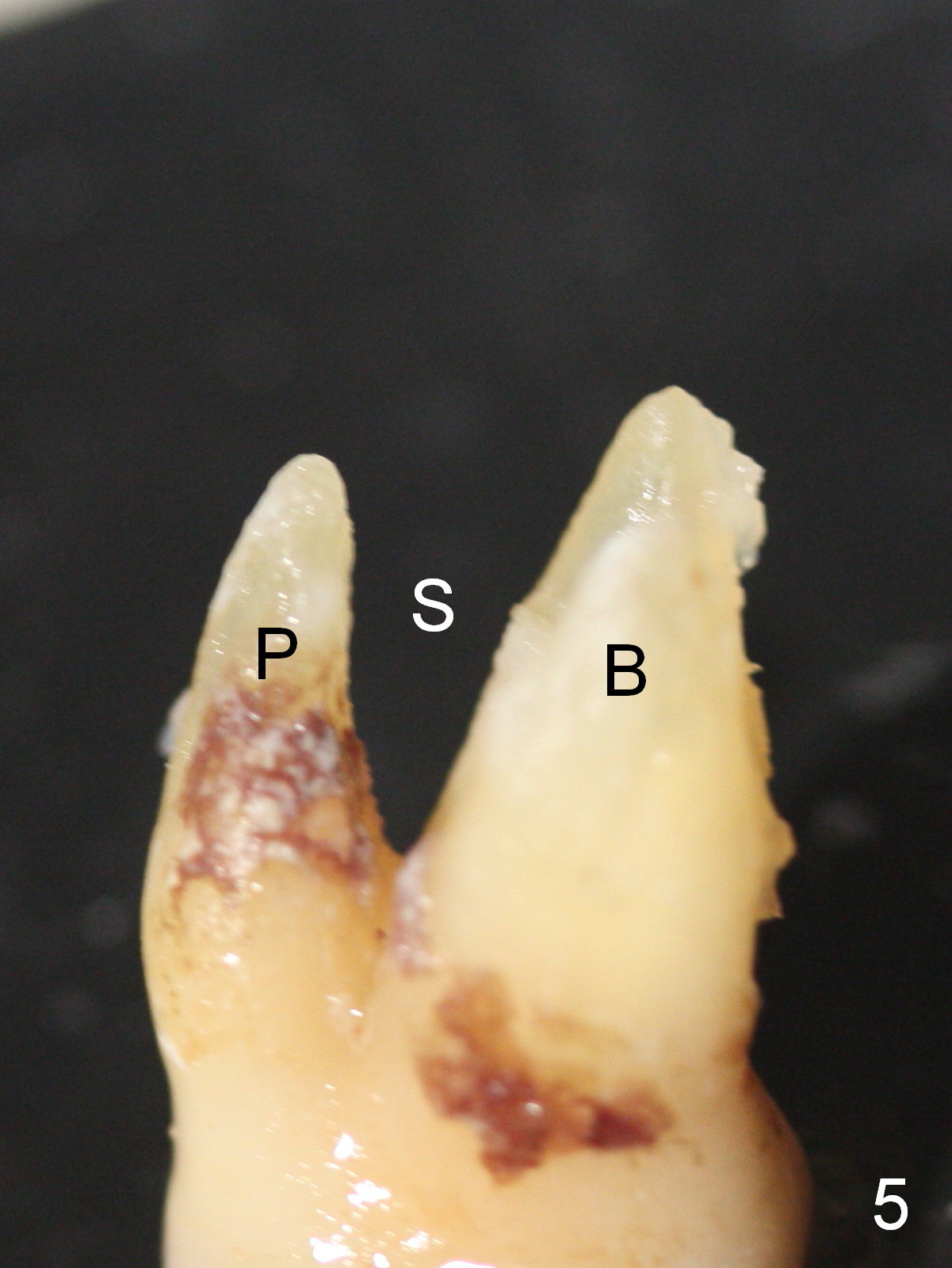
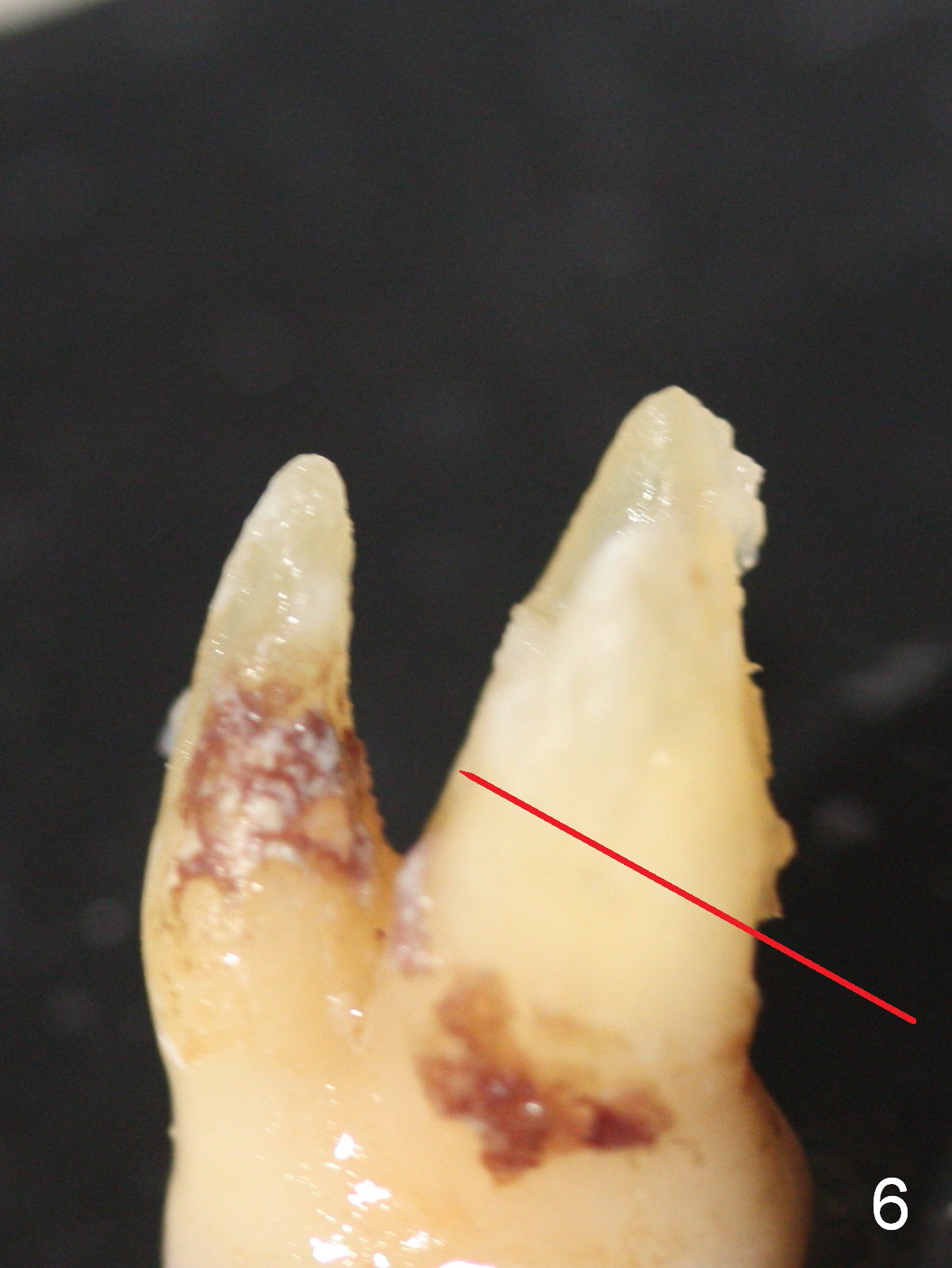
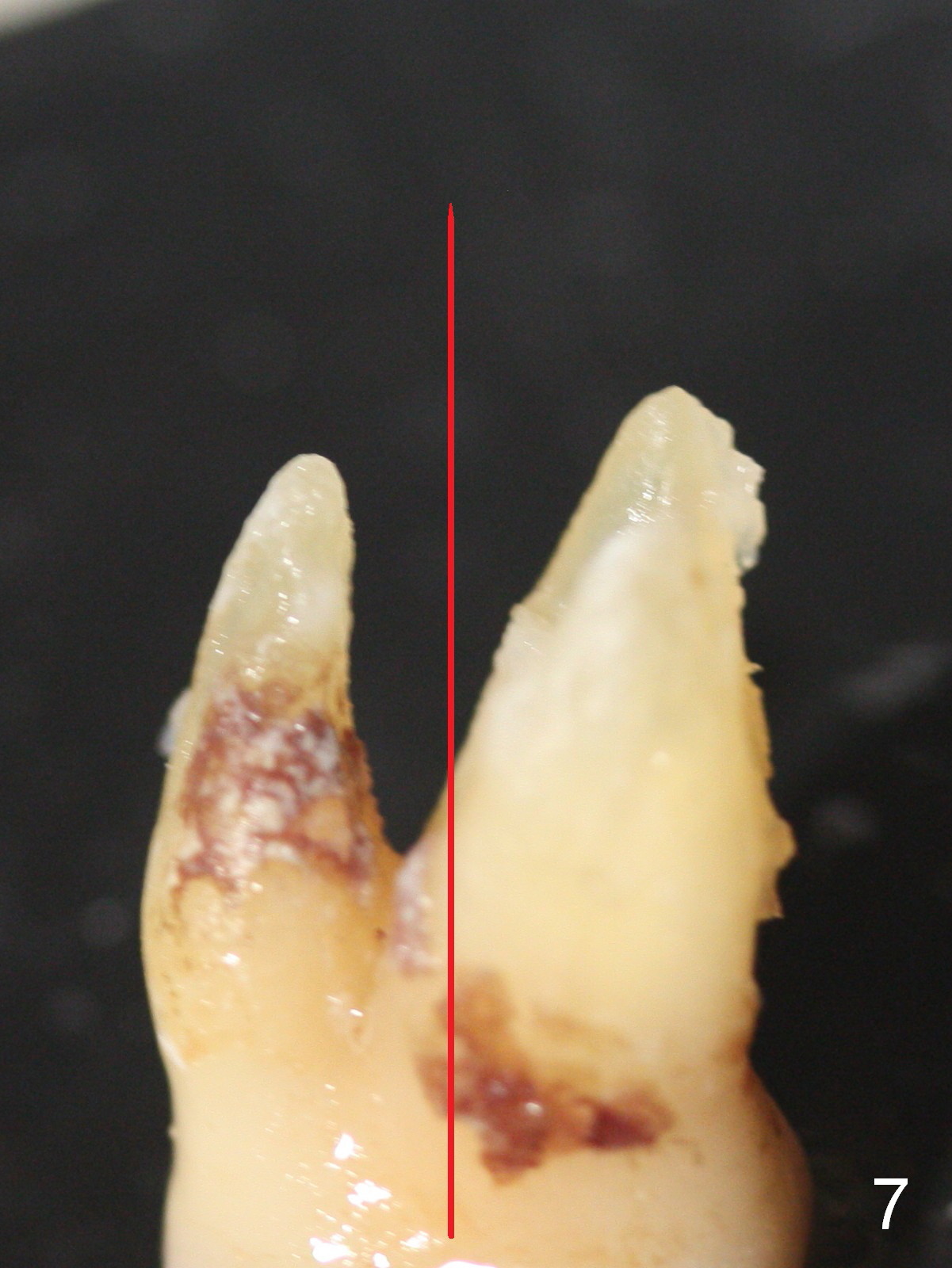
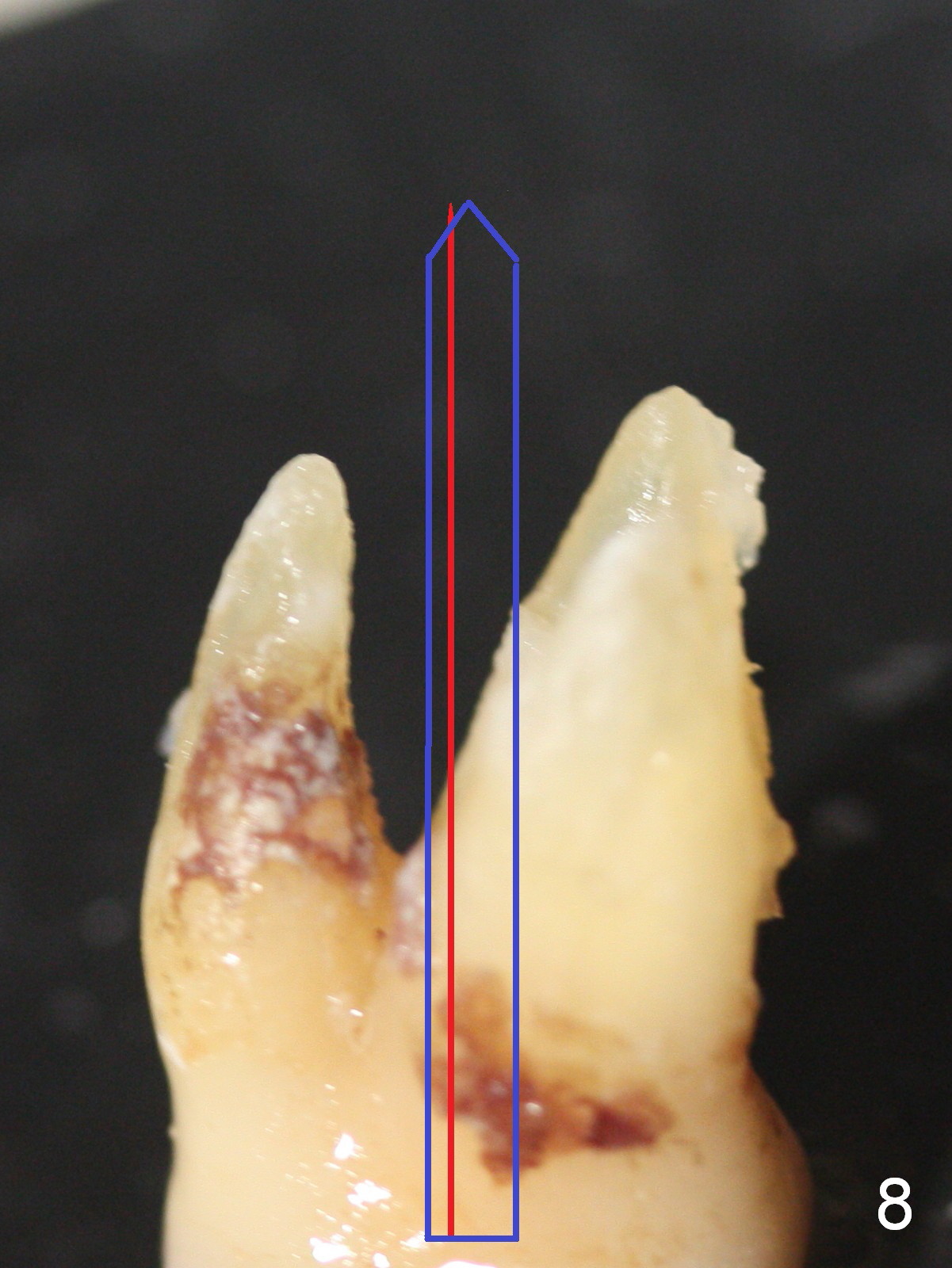
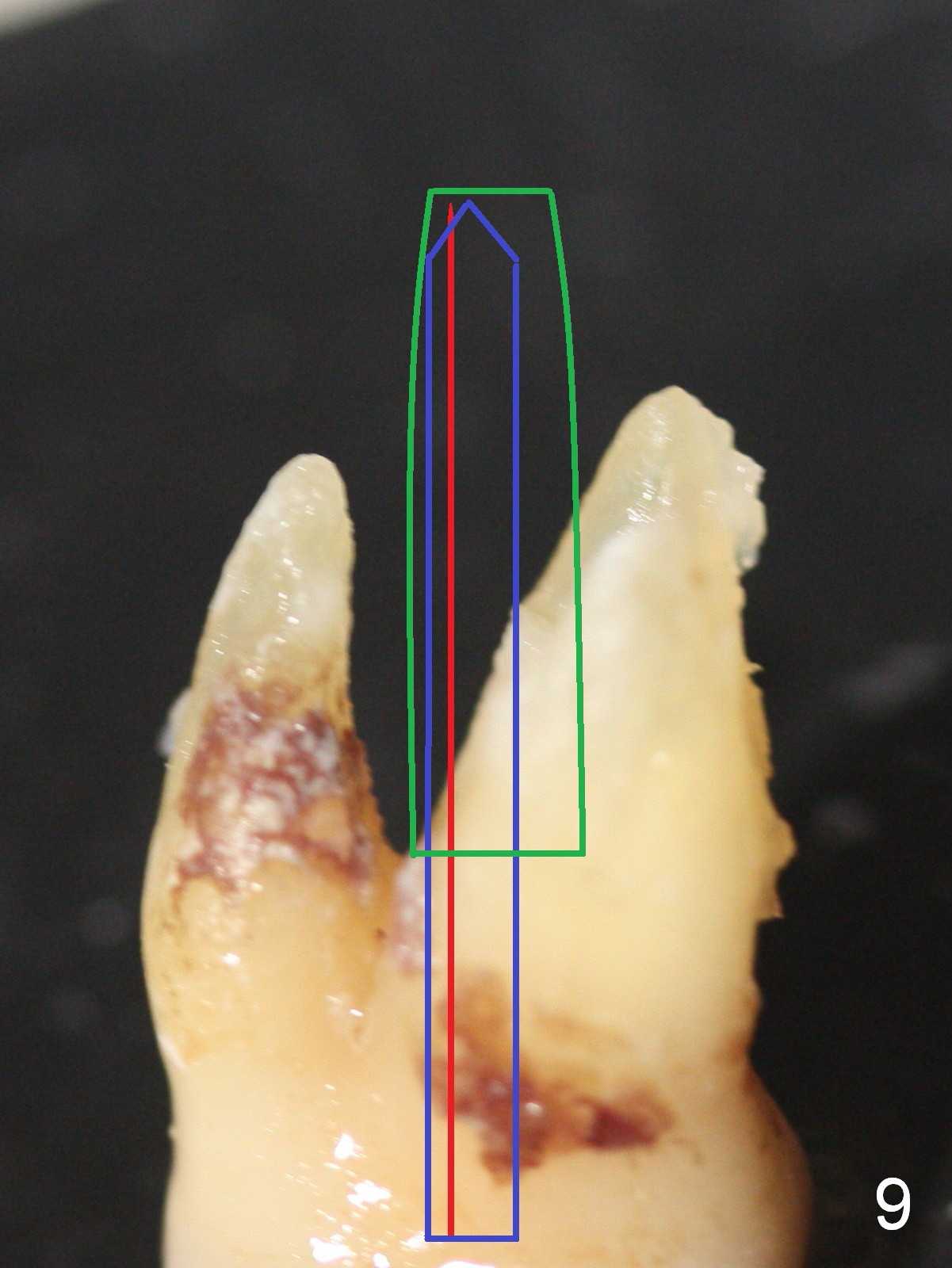
To appreciate the shifting, let us study the extracted tooth with granulation tissue in the furcation (Fig.4 *). With removal of the granulation tissue and turn of the tooth is Fig.5: pretend that the tooth has been extracted; between the buccal (B) and palatal roots is the septum. To make entrance to the slope, the drill should be placed perpendicular to it (Fig.6 red line). Once penetrating the bone, the drill changes its axis, parallel to that of the tooth (Fig.7). As the osteotomy increases (Fig.8 blue arrow), it shifts buccally due to the slope. Taps and implant (Fig.9 green outline) continue the tendency when they are being placed. Apply appropriate force on the drills, taps and implant to counteract the tendency if necessary.
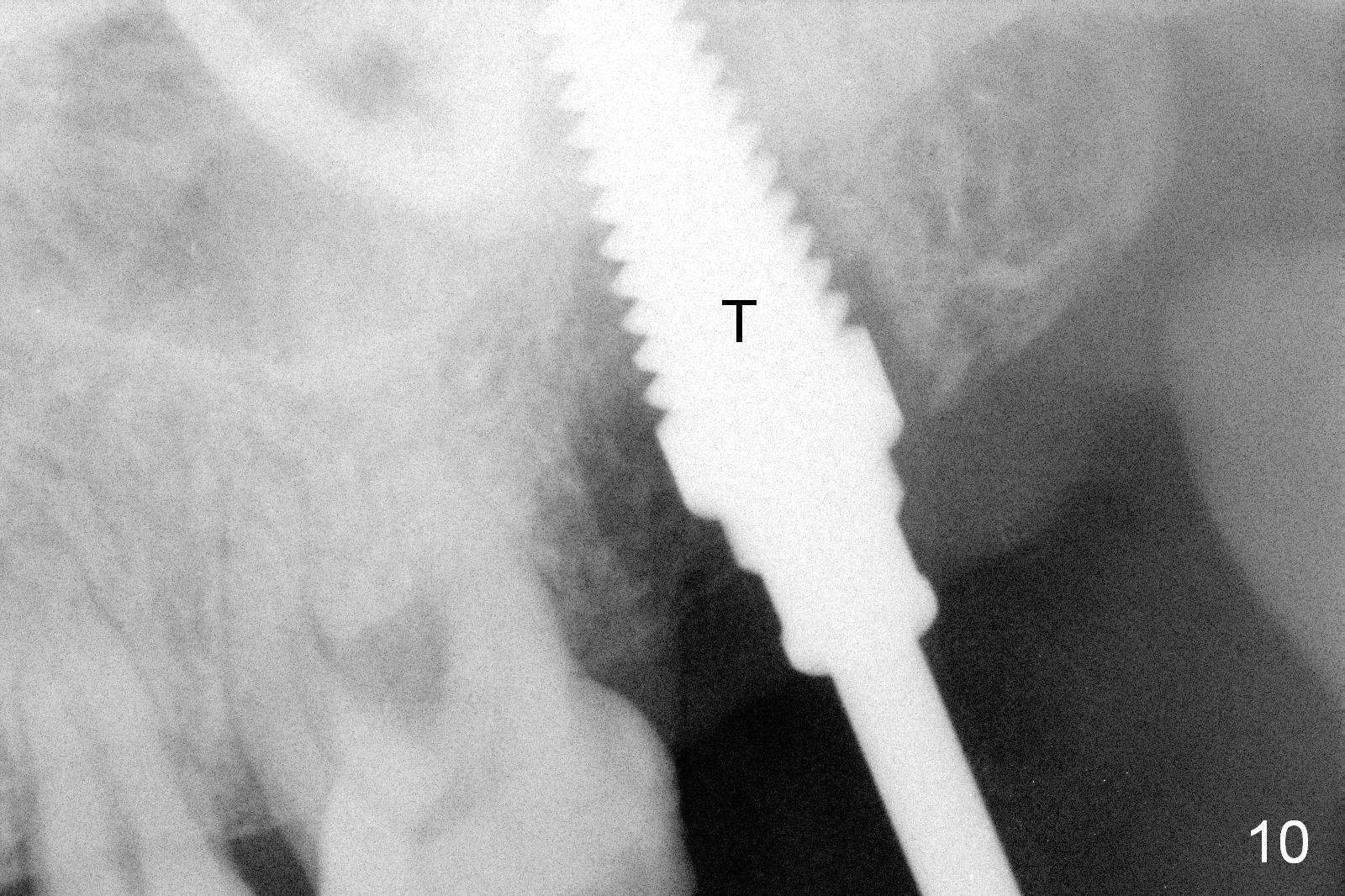
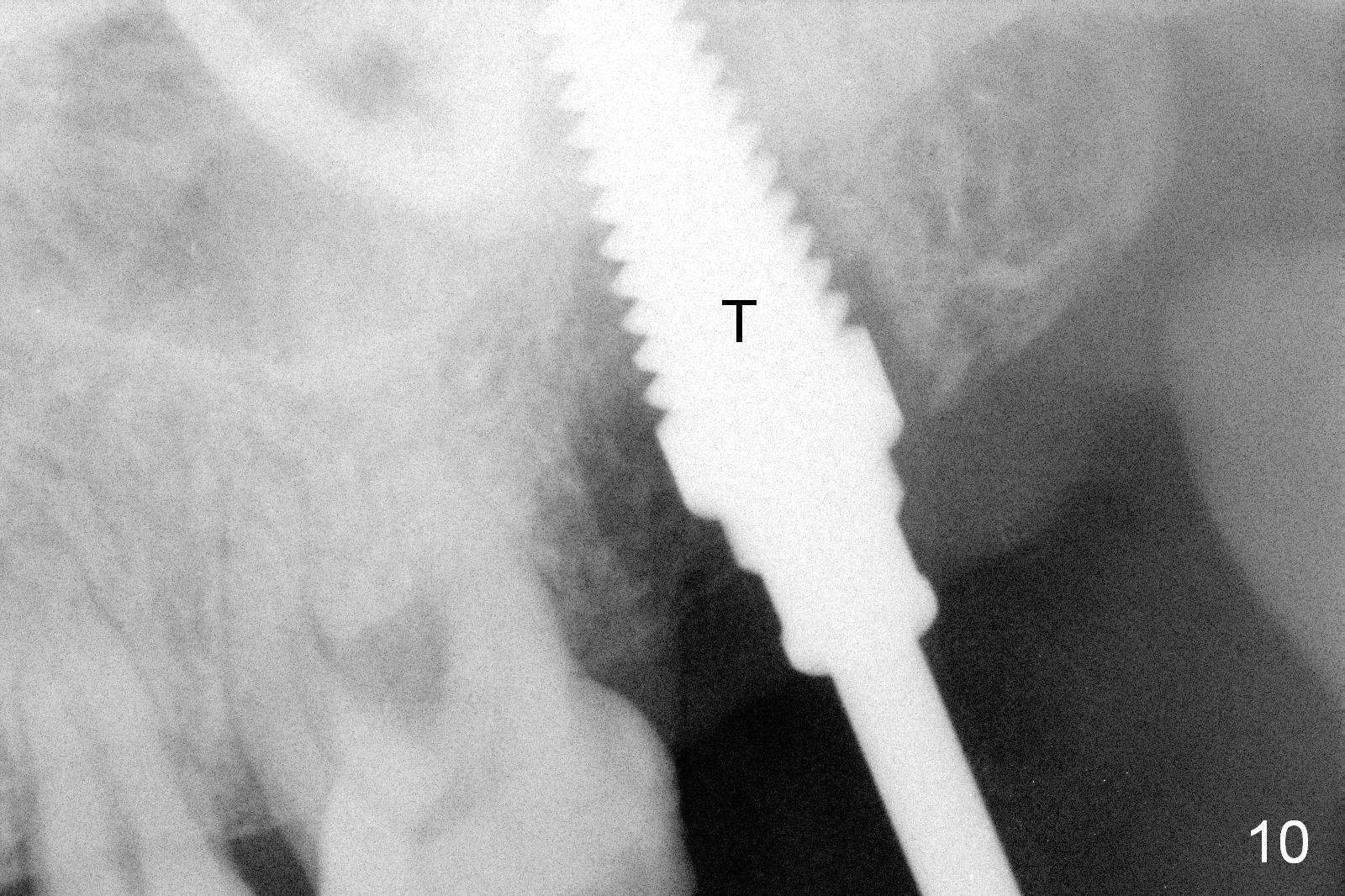
Fig.10 shows a 6 mm tap (T) in the socket; Fig.11 6x12 mm implant (I), 7.5x4(2) mm cemented abutment (A) and bone graft (*). An immediate provisional is fabricated to close the socket completely.
An implant is placed at the site of #18 in 2 weeks.
Approximately 2.5 months postop, the patient complains of pain palatal to #15 implant. A few days later, a palatal fistula is found with tenderness. It appears that there is infection with possible thread exposure. An incision will be made palatally for cleaning with Titanium brushes and Metronidazole and H2O2 irrigation and bone graft/6-month membrane.
When the patient returns for fistula debridement 4.5 months postop, he does not feel pain. The fistula appears to reduce (Fig.12). Chlorhexidine irrigation is provided through the fistula.
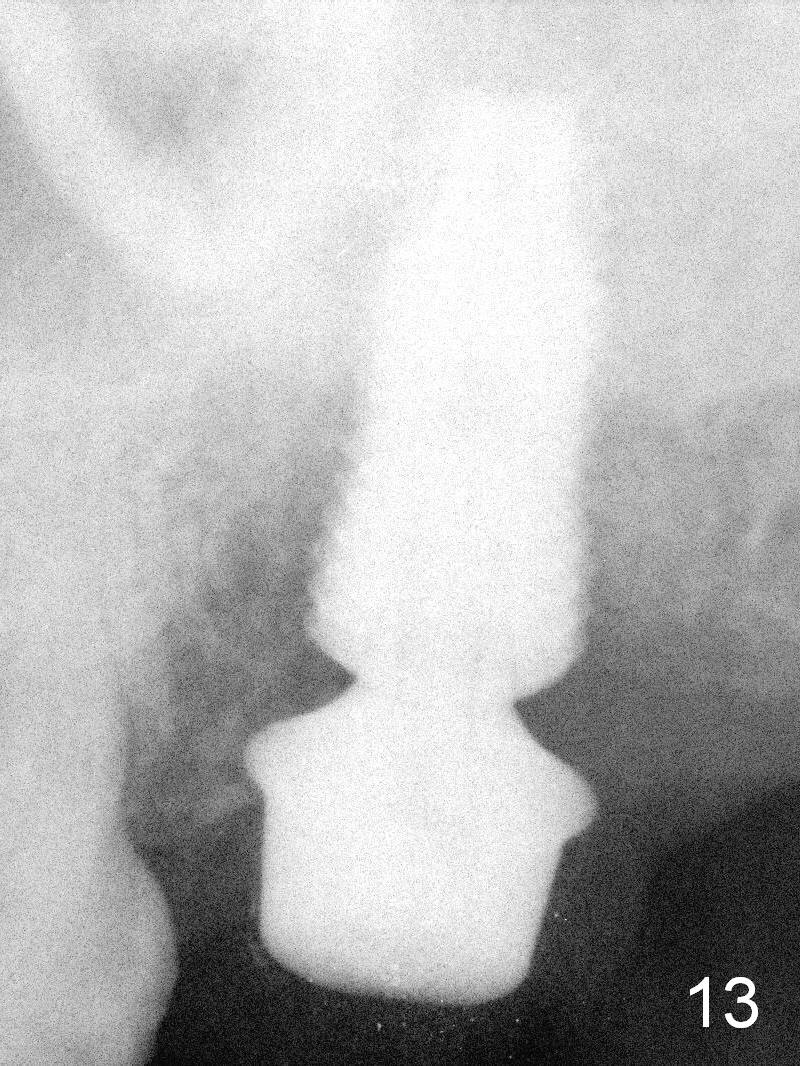
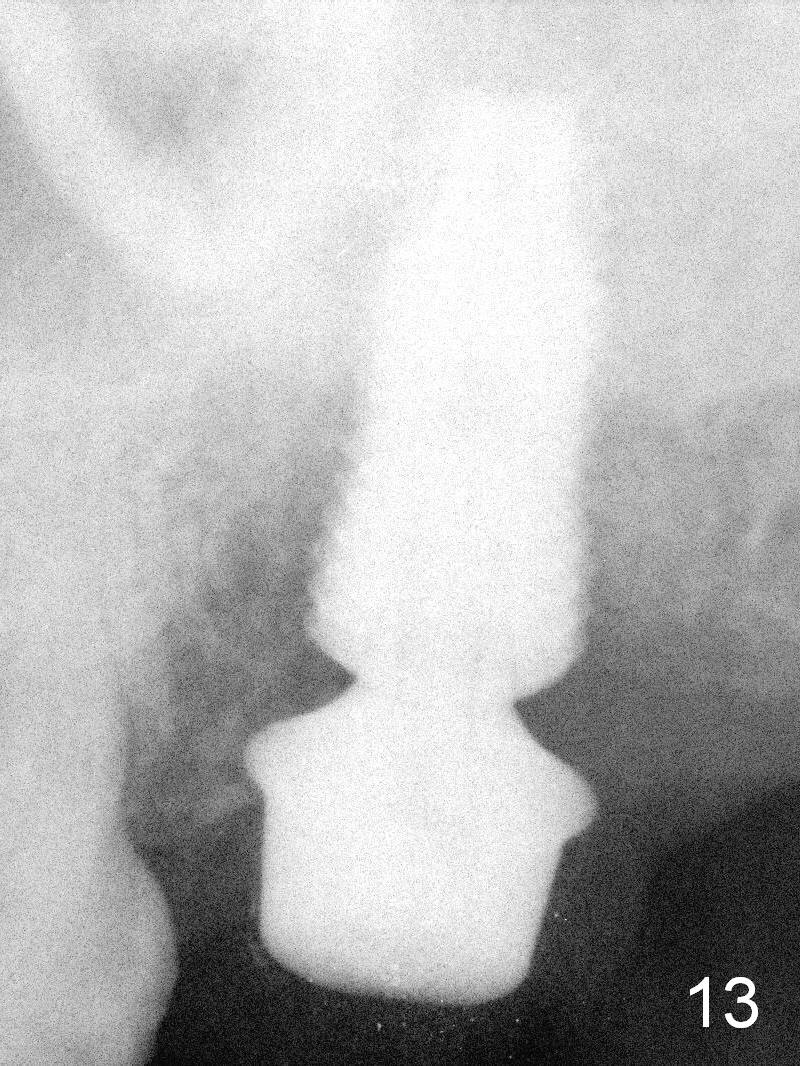
Although there is bone growth mesially radiographically 9 months postop (Fig.13), the mesiobuccal implant (coronally) has no bone contact clinically. Bone graft is placed after debridement with Titanium brush. The abutment is changed to 7.5x4(3) mm.
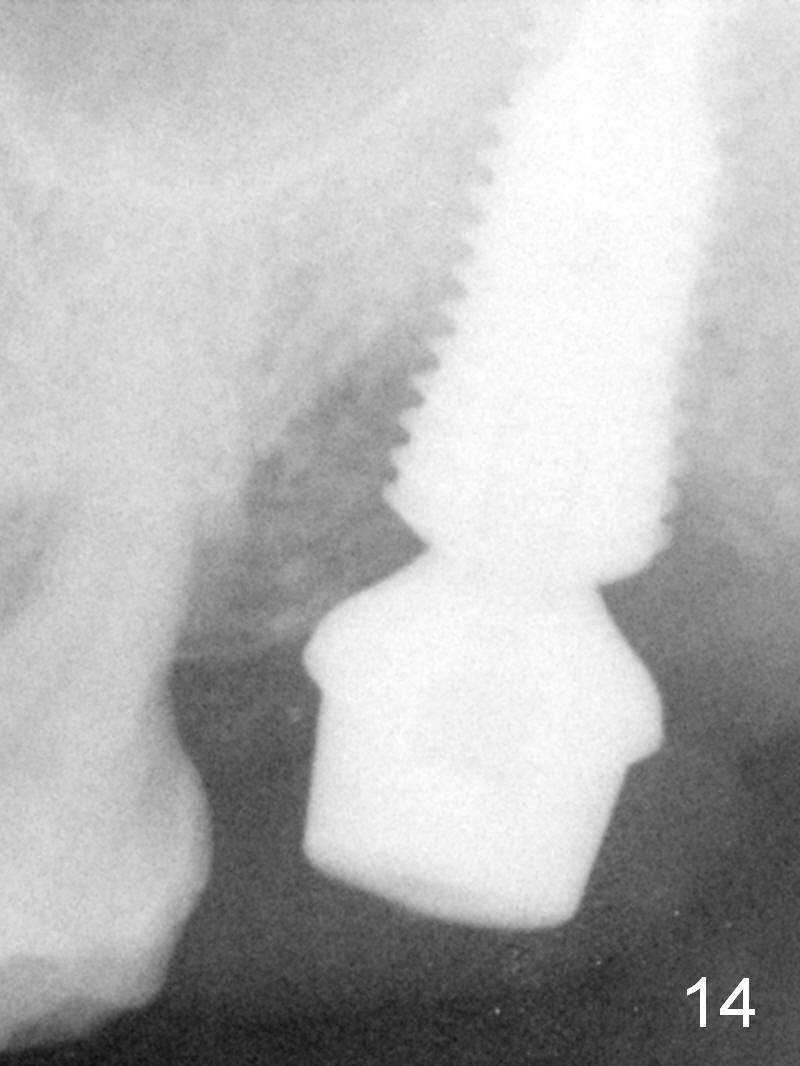
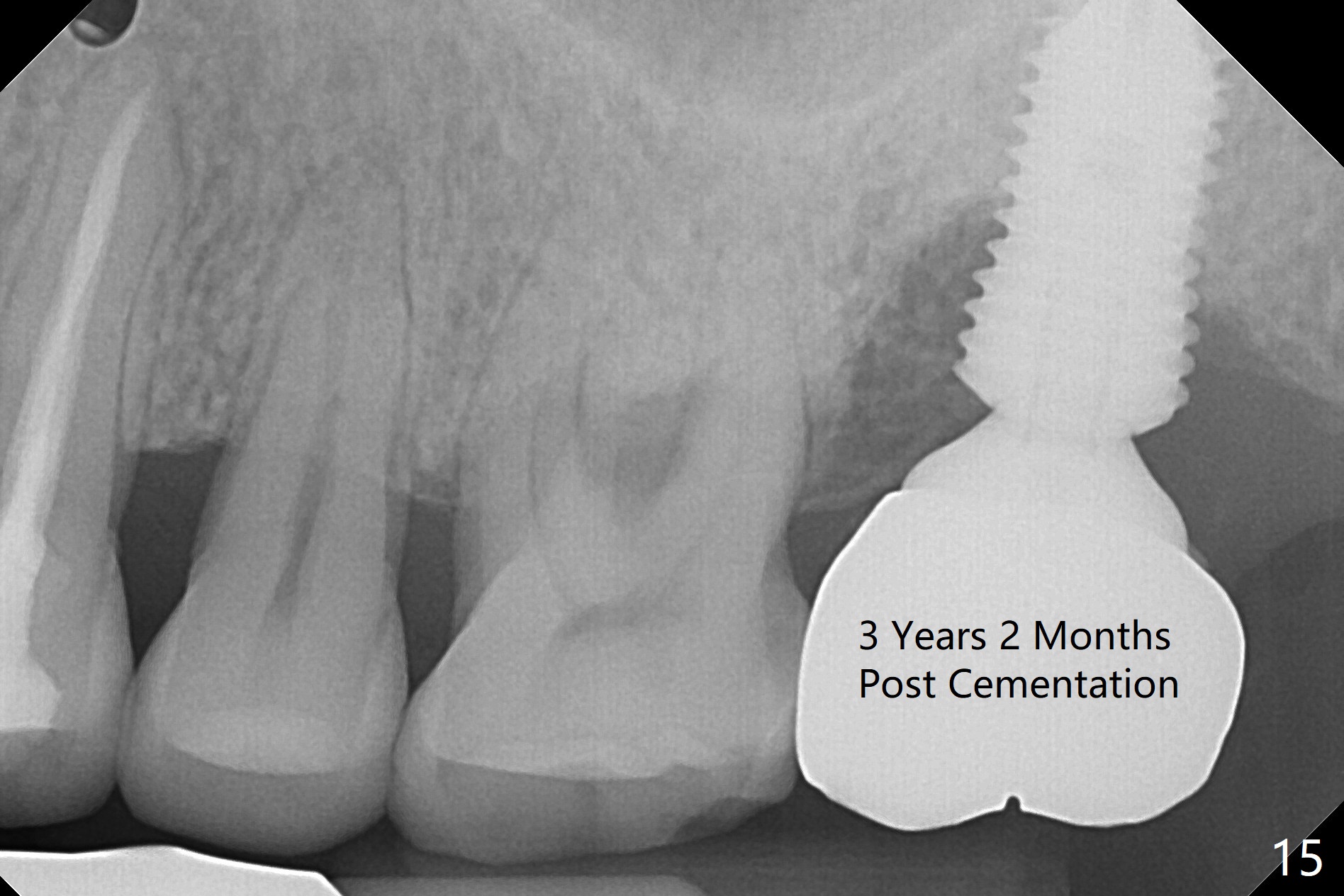
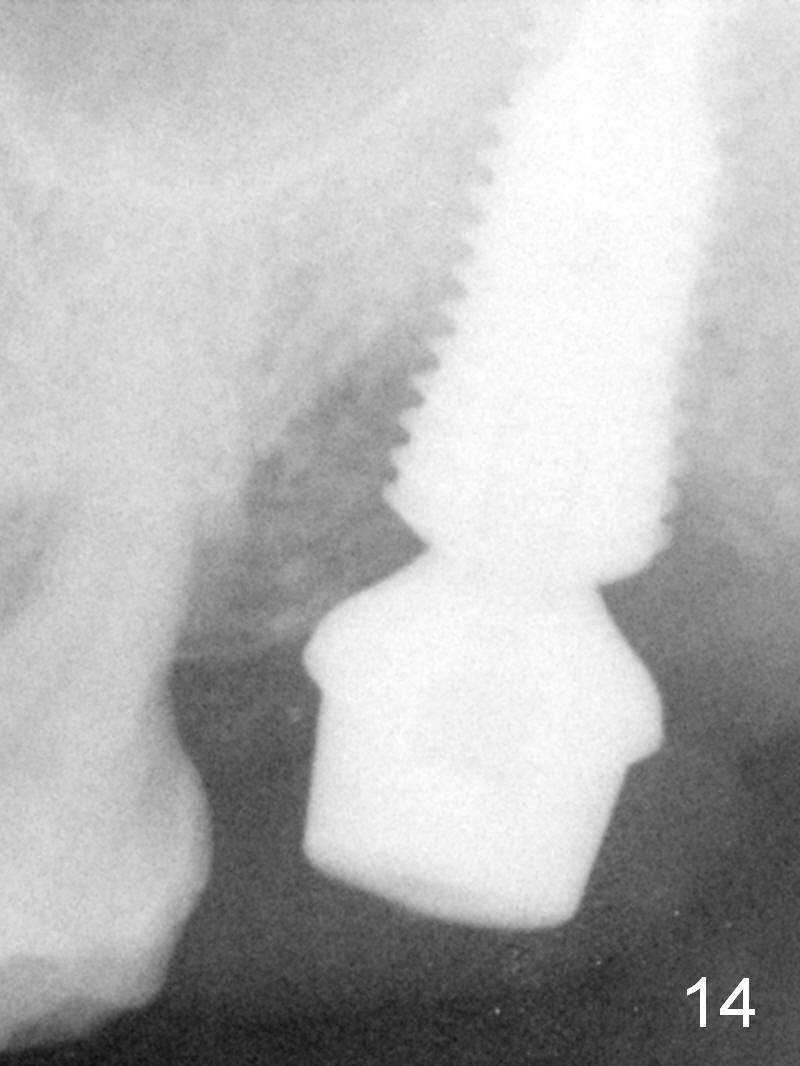
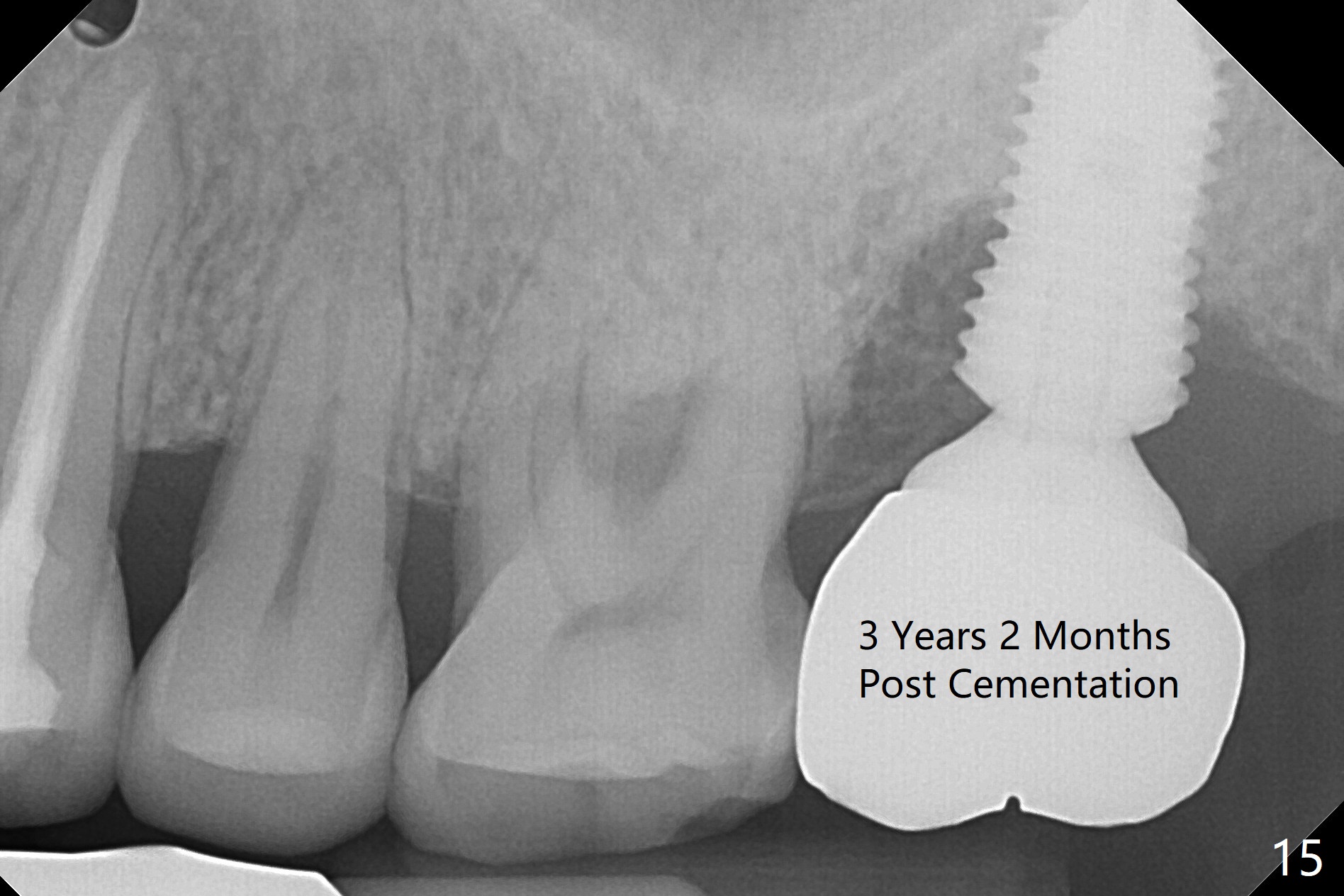
One month 20 days post 2nd grafting, the gingiva looks normal. Note large bone graft particles are placed deep and next to implant threads (Fig.14). In one word, to prevent periimplantitis associated with immediate implant, place bone graft deep and next to implant threads before placing an abutment. The patient complains of tenderness superficial to the mandibular body (probably supramandibular lymph node). Exam shows purulent discharge from the buccal sulcus of the site when probing, consistent with bone loss 3 years 2 months post cementation (Fig.15). Draw blood for PRFx2 for sticky bone. The crown/abutment will be removed through the access hole. Incision will be made to expose the threads for Titanium brush. Place healing screw, sticky bone, PRF and 6-month membrane or 8x8 BioXclude. 4-0 PGA suture closes the wound.
Return to Upper Molar Immediate Implant,
Peri-implantitis
Trajectory II
劈开术
Xin Wei, DDS, PhD, MS 1st edition 08/25/2015, last revision 04/08/2021