




 |
 |
 |
||
 |
 |
 |
 |
|
 |
 |
|||
Lower Premolar Implant Malpositioning
A 55-year-old lady (WJ) complains of palpation pain in the buccal vestibule over #29 implant, 5 months postop (immediately before cementation, Fig.4 *). Is the implant placed too buccally or there is buccal plate resorption after placement?
Fig.1 shows preop condition, whereas Fig.2 immediately post placement. In fact there is a space lingual to the implant of #29 (*). At that moment, the buccal margin is within normal limit (arrowheads). Ideally, the malpositioning can be corrected immediately. The implant should have been removed, repositioned and placed at the right position and trajectory. It is possible that attention was being paid to the depth of the osteotomies, because of proximity to the Mental Loop.
Four months and a half, the buccal margin has to be extended (Fig.3 ^). A month later, gingival recession becomes more obvious (Fig.4 ^ with exposure of the rough surface of the implant). Occlusal view demonstrates the buccal position of the implant and abutment at #29 (Fig.5). CBCT will be taken to confirm the malpositioning. If it is confirmed, the abutment and implant will be removed and un-torqued. The lingual bone will be removed; osteotomy will be also extended apically cautiously. The same or longer implant will be placed immediately. Probably two 1 piece implants will be placed at the same time at the site of #30, since the ridge is narrow.
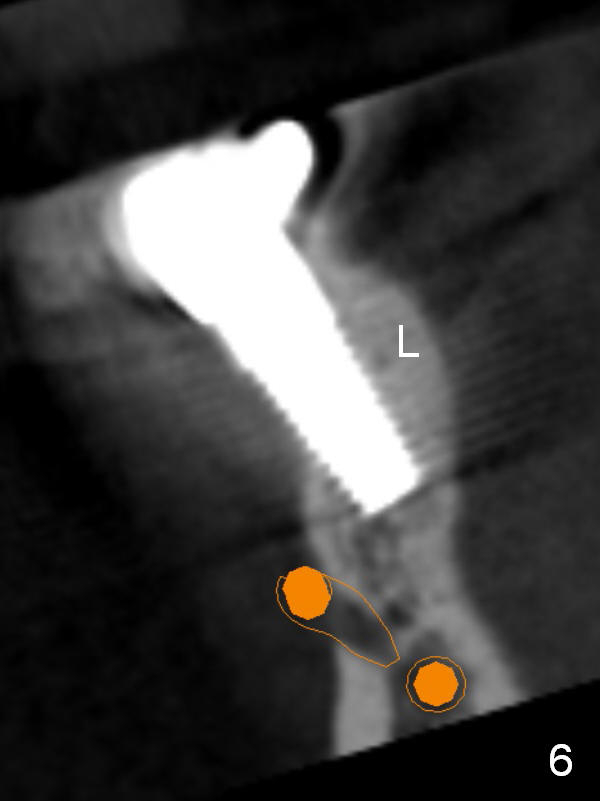
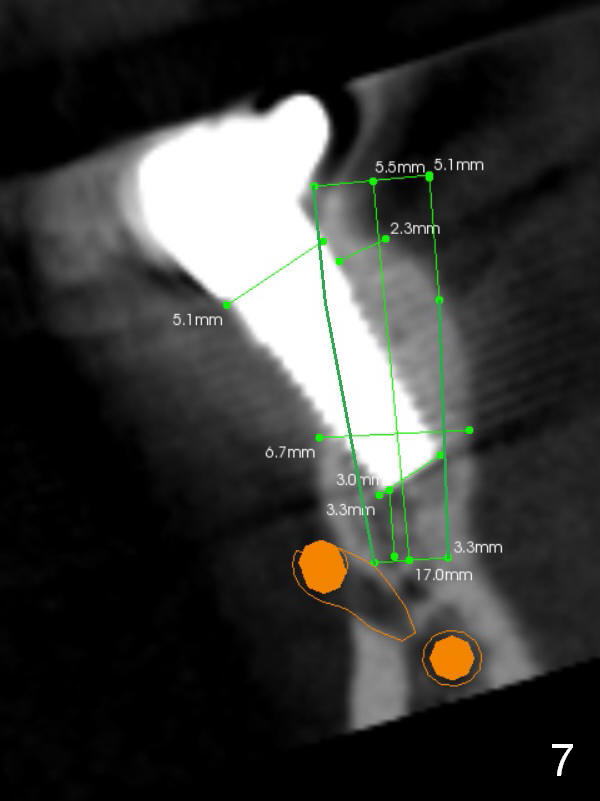
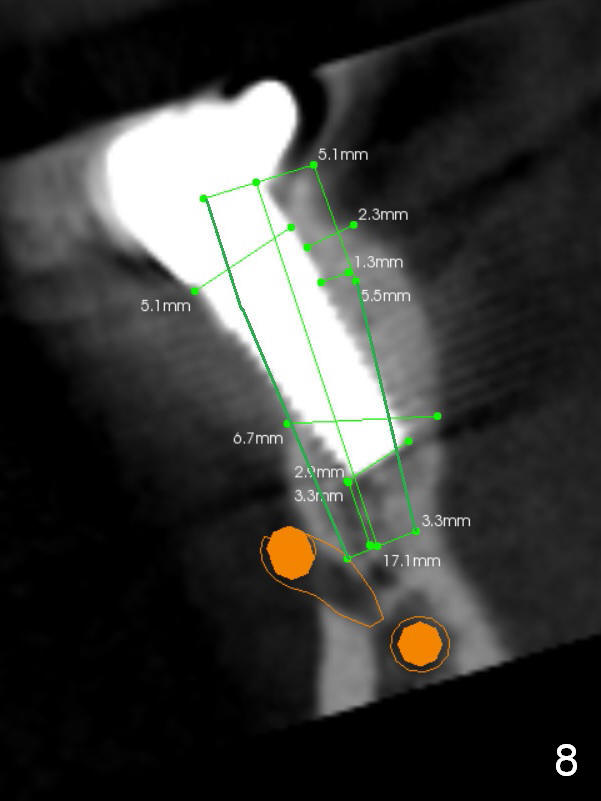
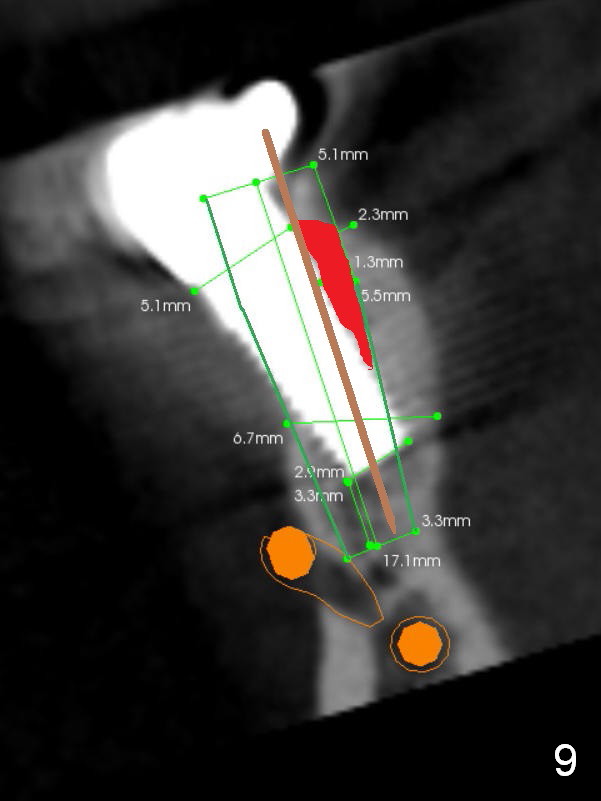
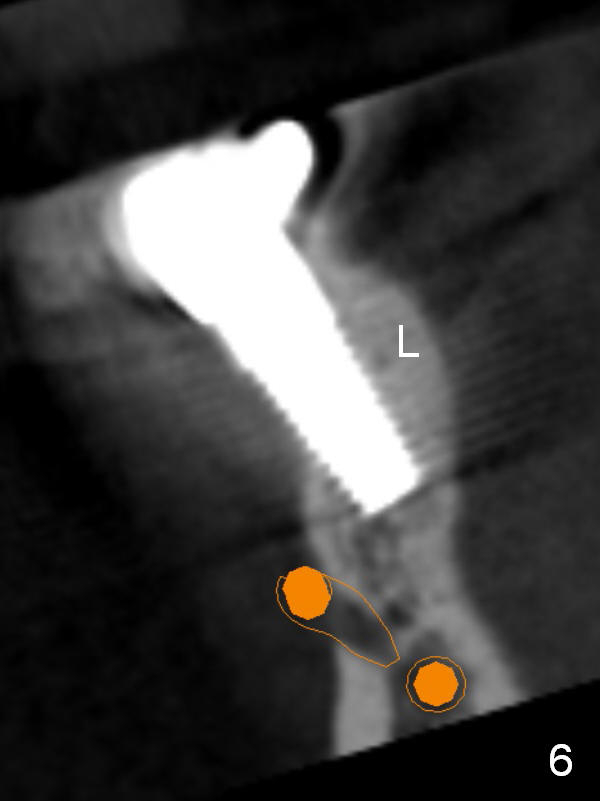
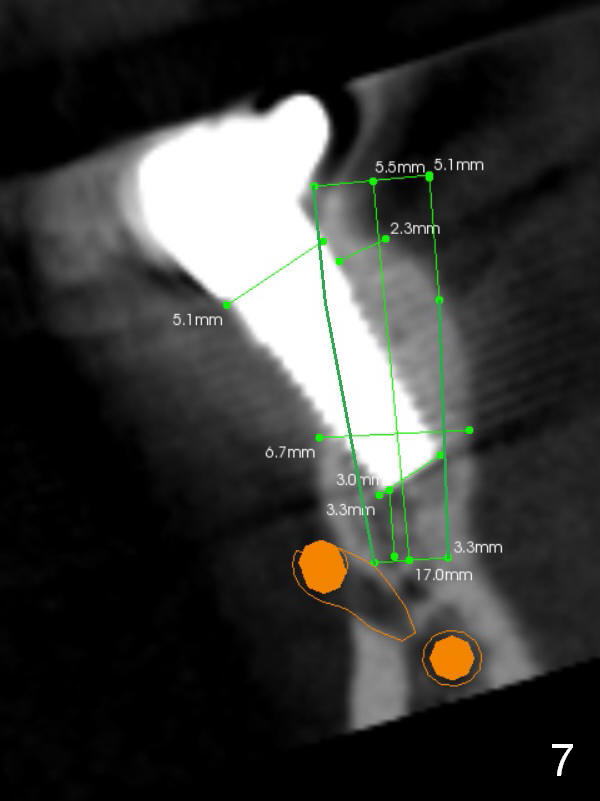
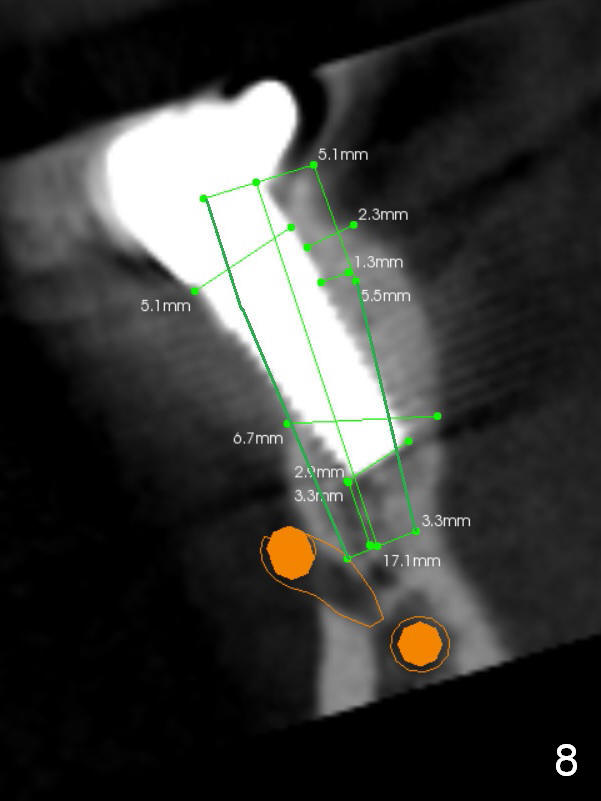
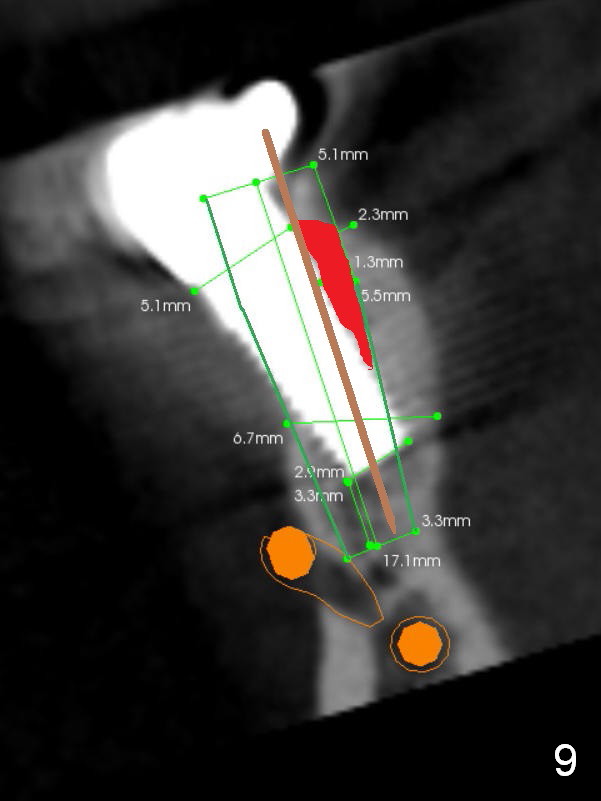
CBCT confirms buccal malpositioning (Fig.6, coronal section at #29). It can be corrected immediately (Fig.7,8). It appears that the latter correction is more appropriate. After implant removal, the buccal aspect of the lingual plate is removed (Fig.9 red area) before starting a new osteotomy site and deepening it (brown line).
Return to
Lower Premolar Immediate Implant,
CT F-U
Xin Wei, DDS, PhD, MS 1st edition 09/27/2015, last revision 04/04/2018