


 |
 |
 |
|
 |
 |
 |
|
 |
 |
 |
 |
 |
|||
No New Bone are Needed for Primary Stability of Immediate Implant
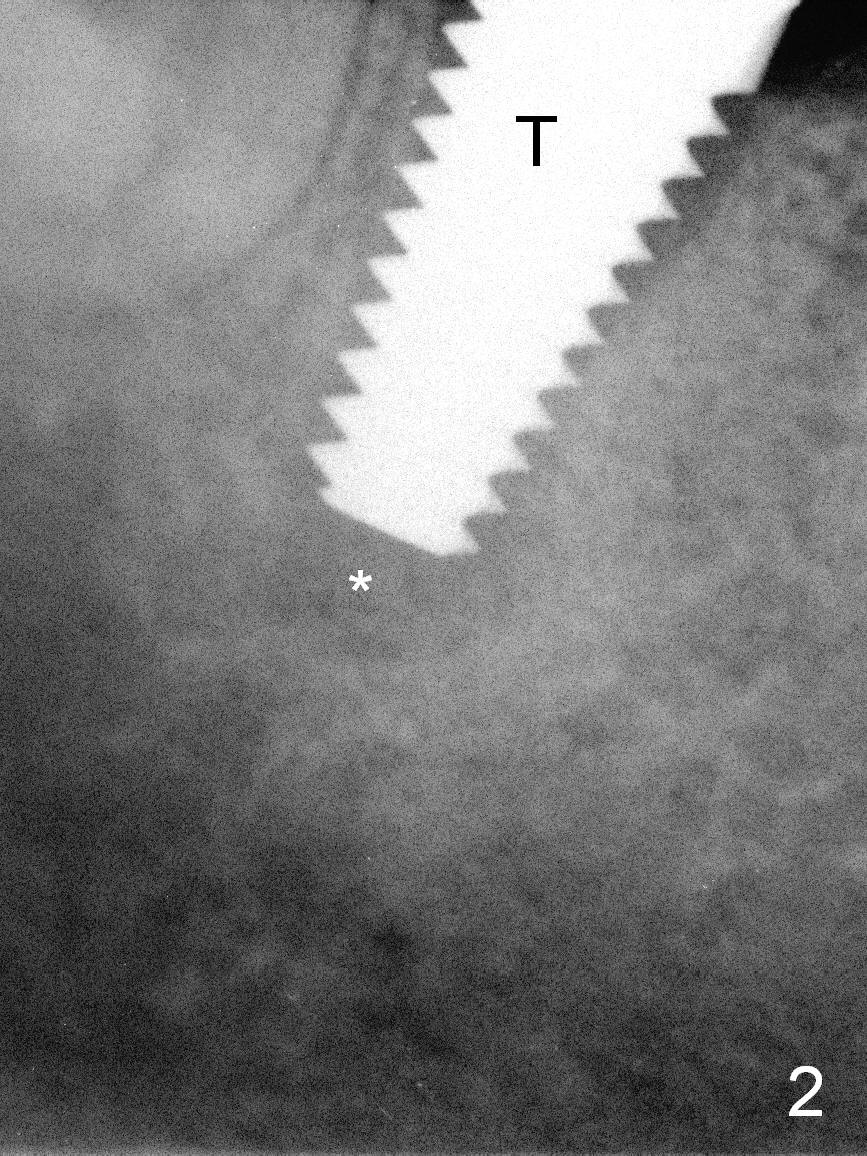
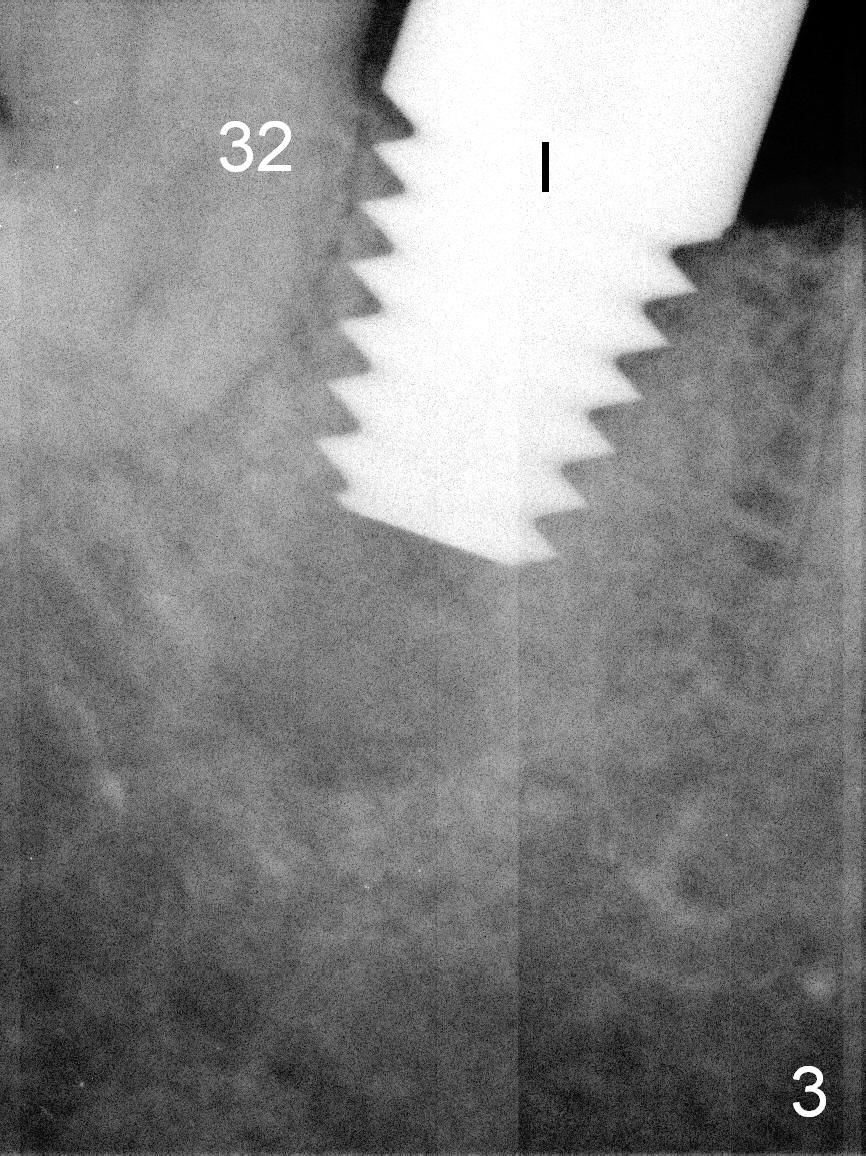
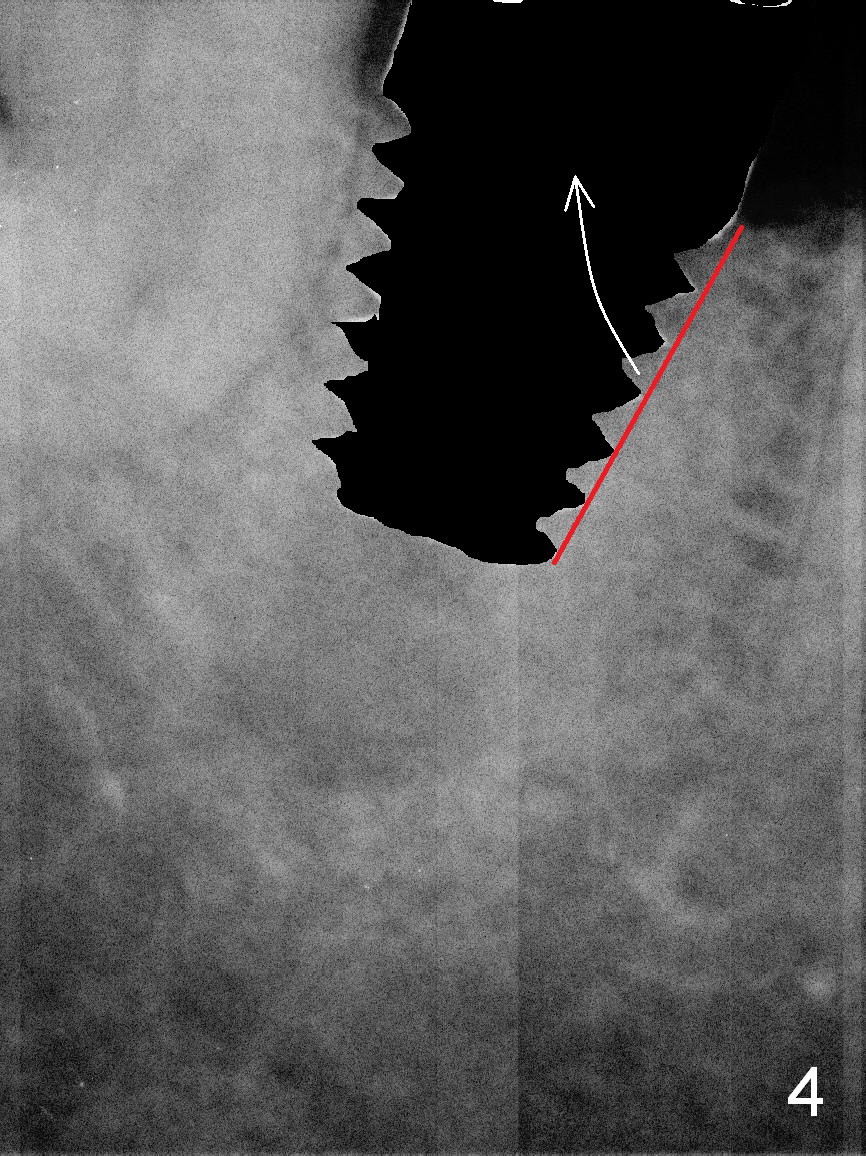
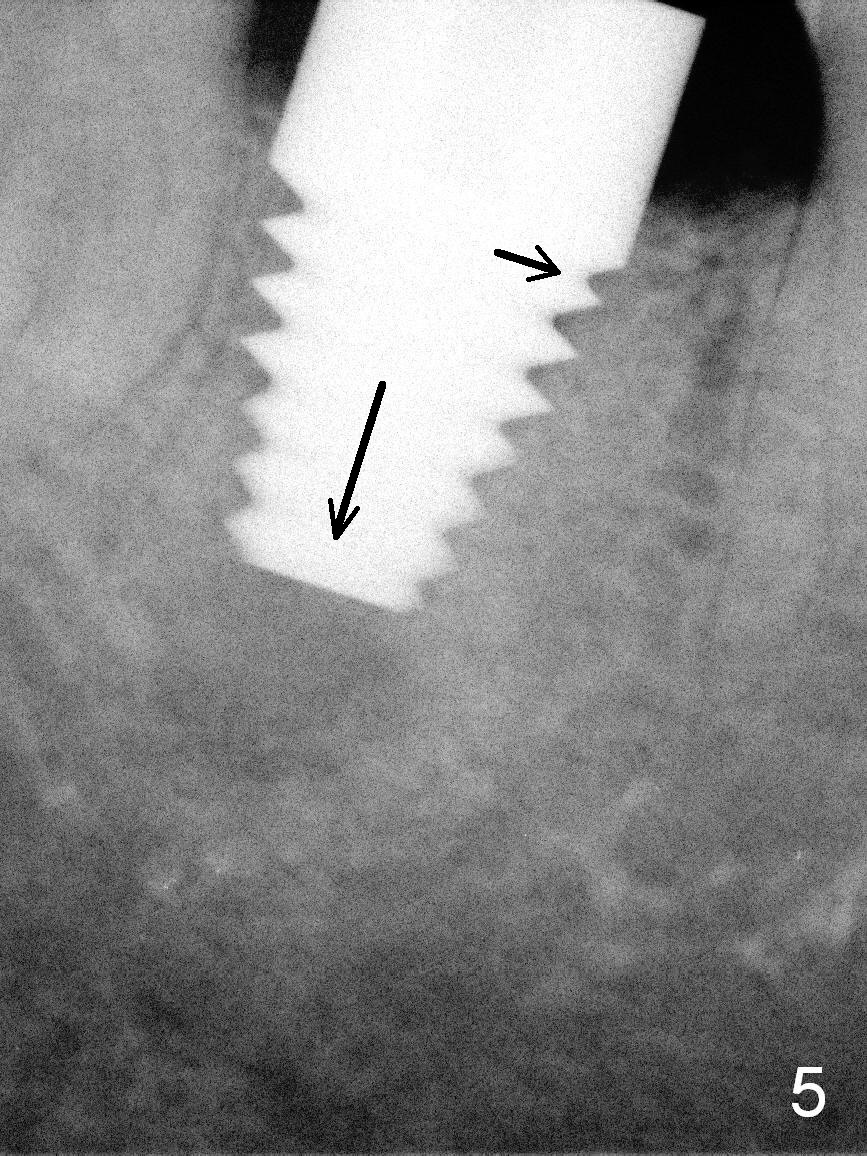
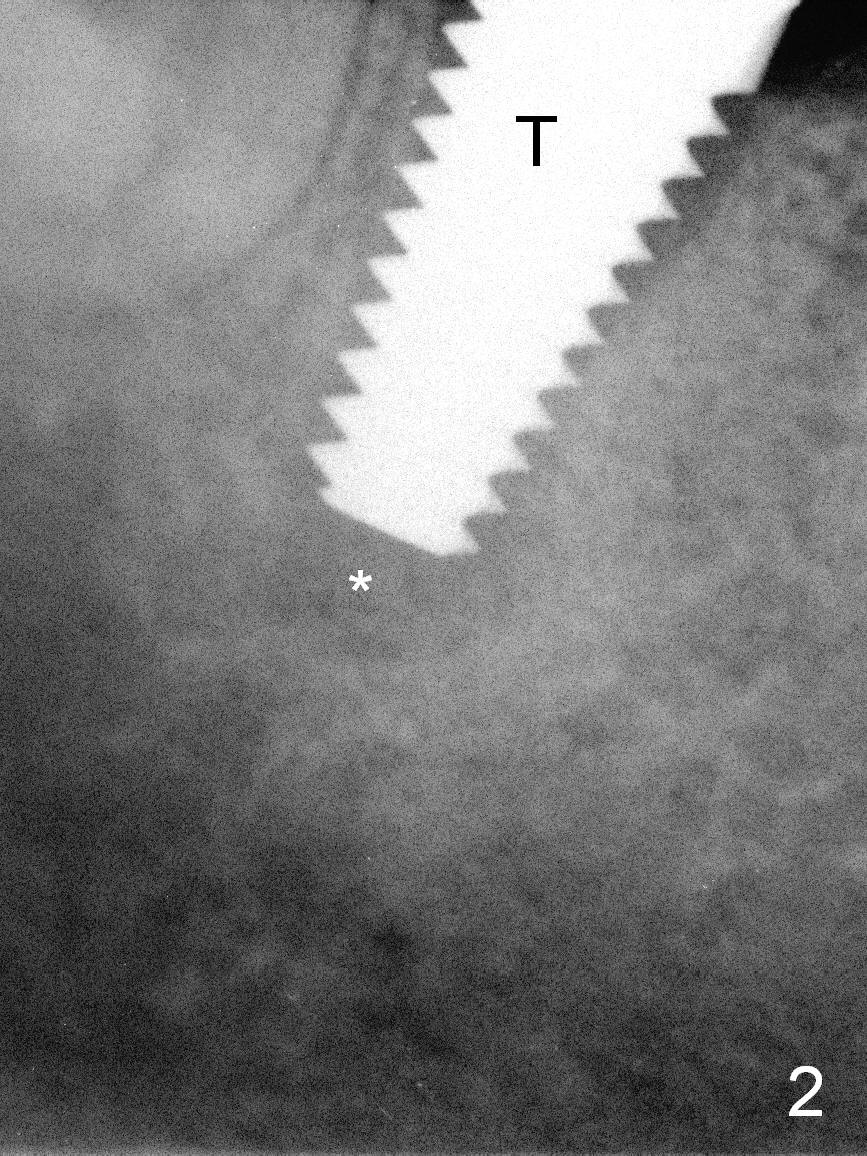
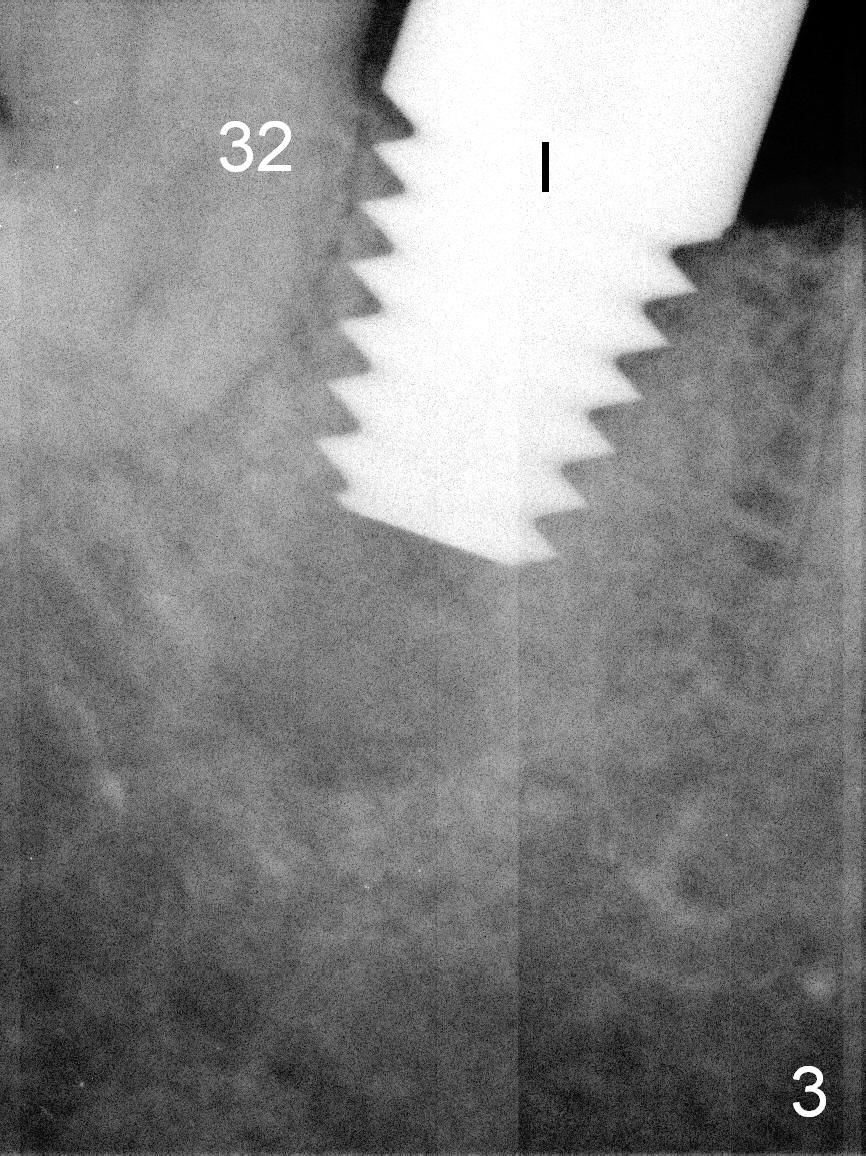
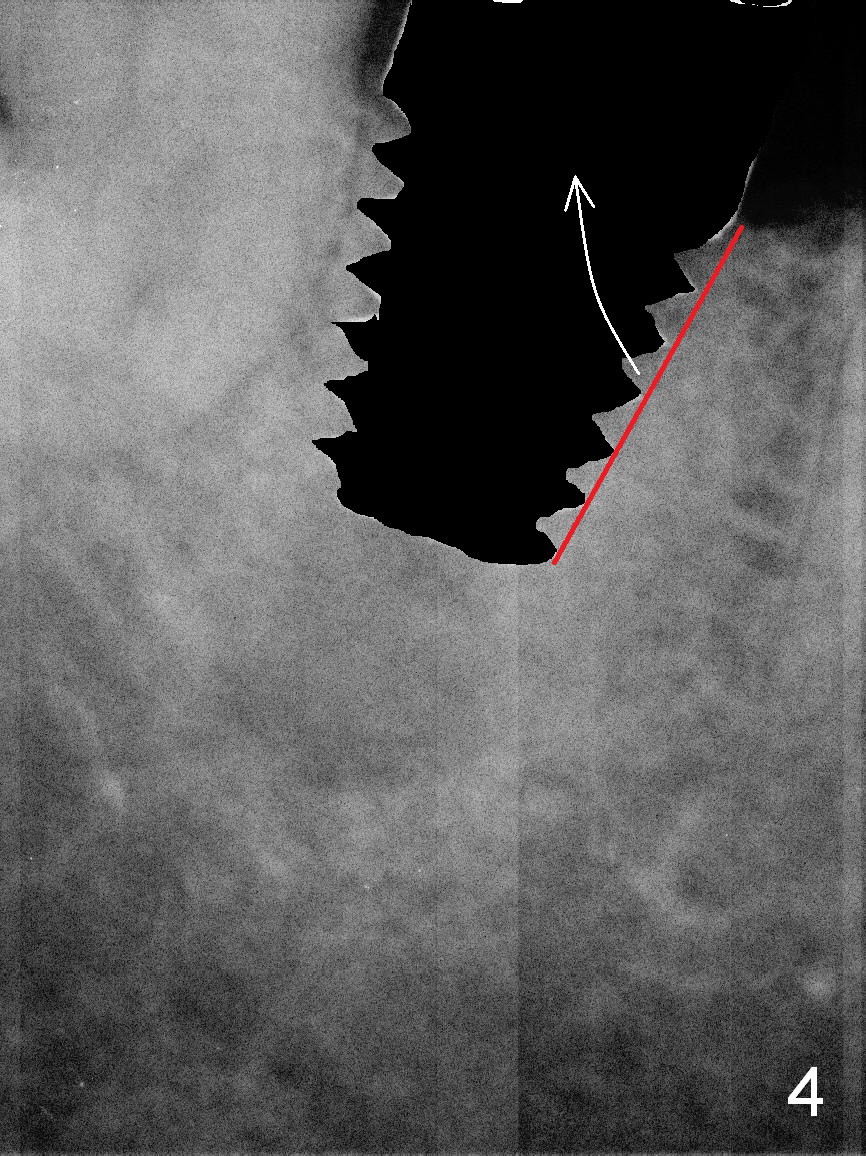
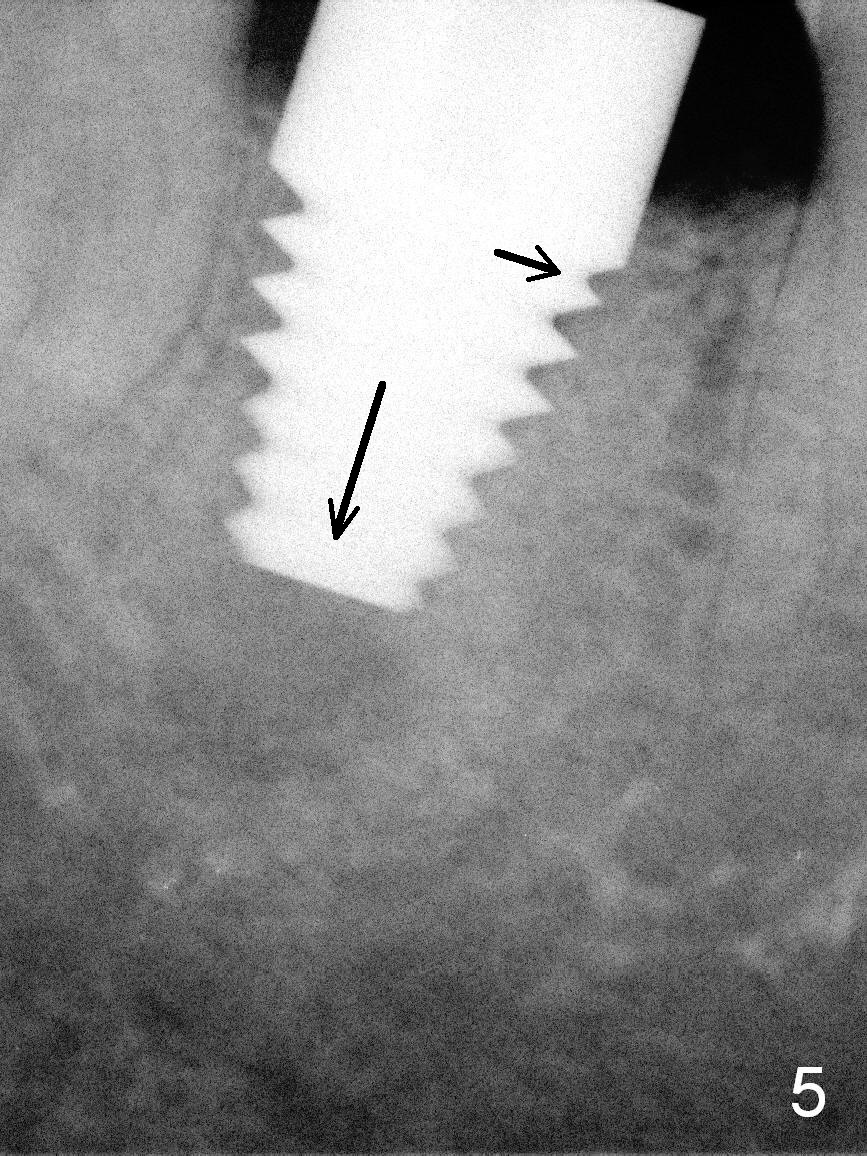
There is a fistula mesiobuccal to the tooth #31 (Fig.1 <). There is mild discomfort when the tooth is being extracted after infiltration anesthesia with Mepivacaine 54 mg, Septocaine 68 mg, Epinephrine 17 mcg. The apical granulation tissue is sensitive to touch (Fig.2 *) and it may be closely associated with the Inferior Alveolar Nerve. A 7 mm tap is gently inserted with barely stability (Fig.2 T). After block anesthesia with Lidocaine 34 mg, Epinephrine 17 mcg, a 8x14 mm implant is inserted with stability (Fig.3 I), but not as deep as the 7 mm tap, because of severe pain. In addition, the implant is close to the tooth #32. Then block anesthesia is administrated with Bupivacaine 9 mg, Epinephrine 9 mcg. The apical granulation tissue is still too sensitive to be curetted. The implant is removed and the mesial bone is removed with 4 mm reamer on the side, not the tip (Fig.4 red line and arrow). The implant is placed to a more desired depth (Fig.5 downward arrow). It is also placed a little mesially (transverse arrow). The insertion torque is > 60 Ncm. Postop there is no paresthesia.
In brief, an immediate implant could be placed without new bone for primary stability. The implant does not need to extend the whole length of the socket. The diameter of the implant should be a little larger than the socket.
Periapical granulation tissue is sensitive to probe after block anesthesia. It may be close to the Inferior Alveolar Nerve. It is not curetted. One week postop, the periapical fistula has reduced (data not shown). The pain has also decreased each day postop. Postop antibiotic is used ~ 10 days. According to Gargiulo et al, inflamed tissue was removed from the socket walls, but not intentionally removed from periapical lesions, if present.
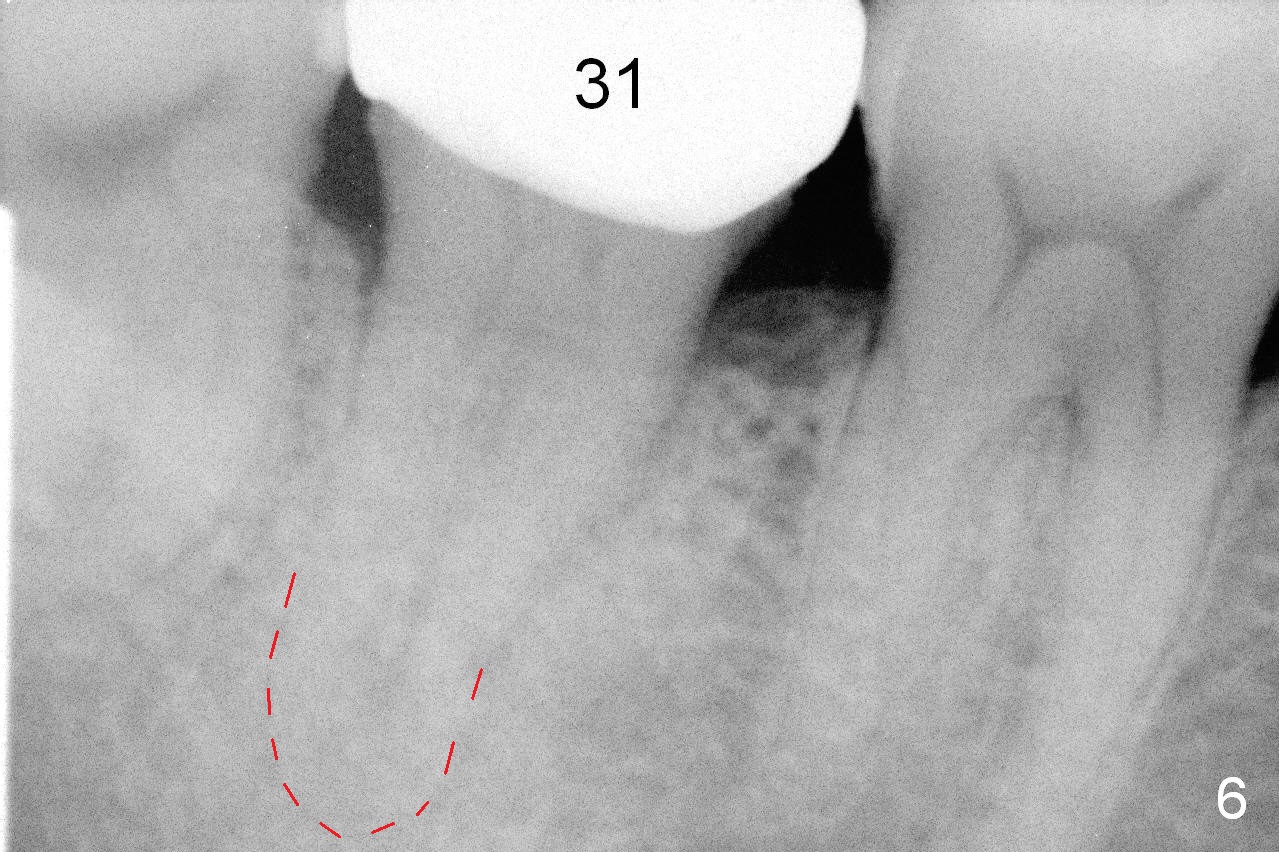
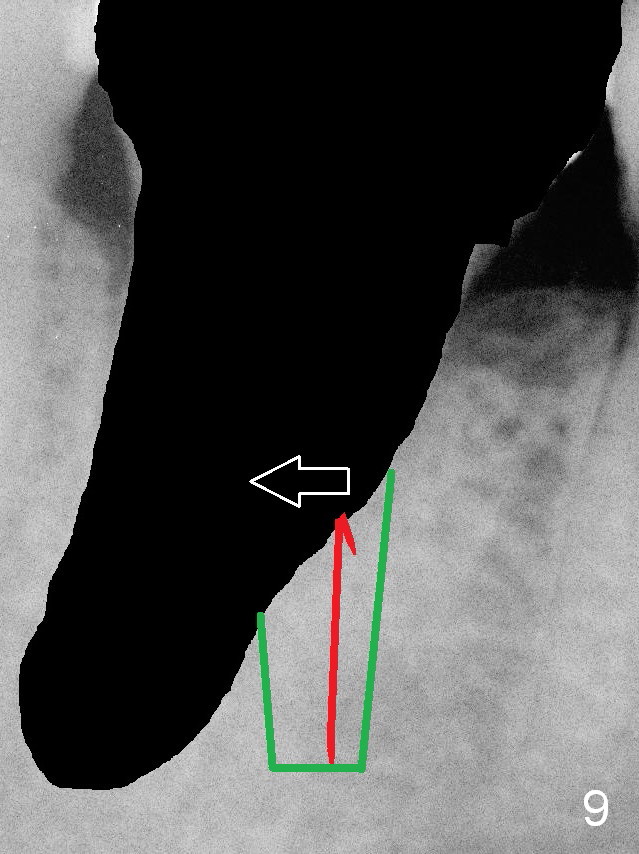
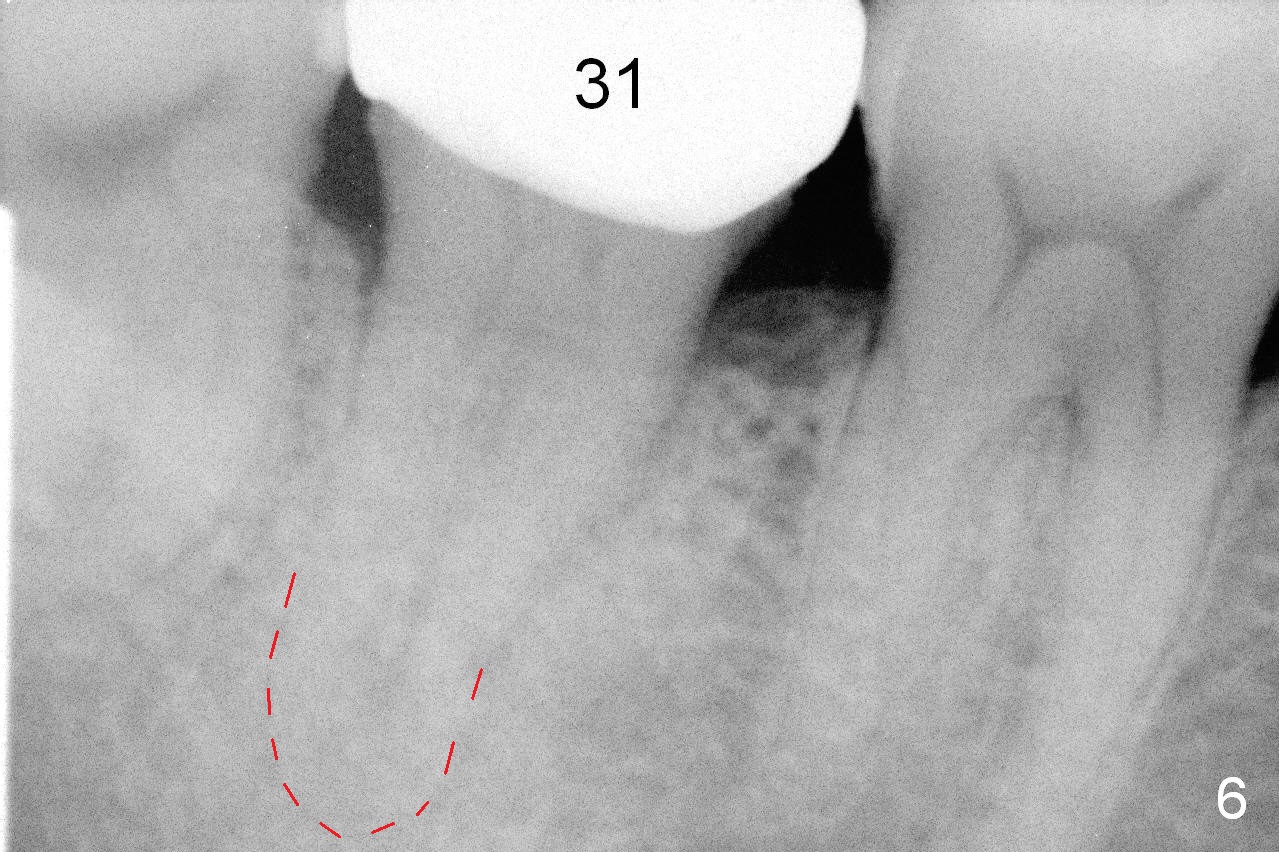
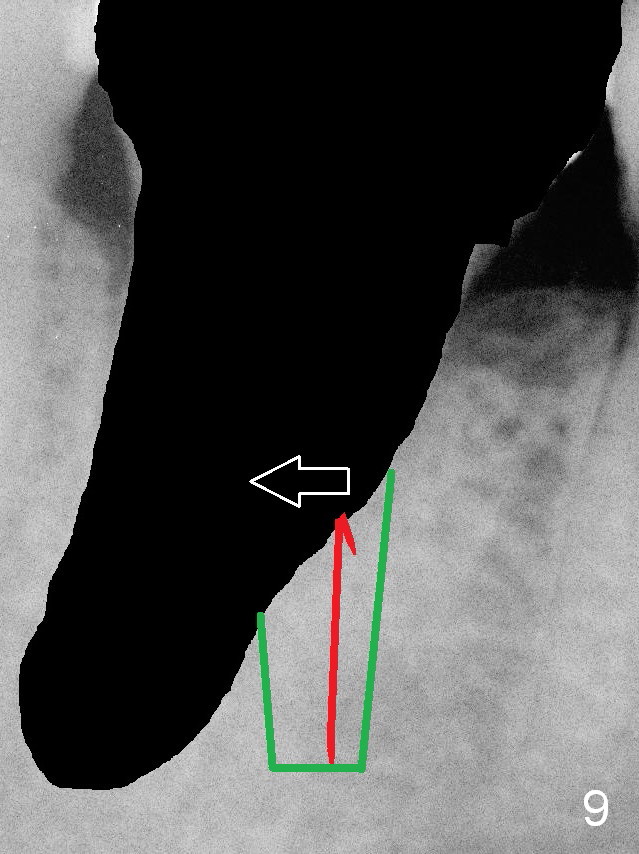
To place the implant more ideally, let us review preop PA (Fig.6). The root of the tooth #31 is close to that of #32. After extraction (Fig.7 black area), osteotomy should not follow the original socket, instead going into the mesial wall of the socket obliquely initially (red line). Once engaged, the drill turns in the long axis of the tooth (Fig.8). As the osteotomy increases (Fig.9 green area), it is most likely deviated distally (arrow) so that the final position of the implant is more or less ideal. More importantly, we do not have to deal with the sensitive apical lesion.
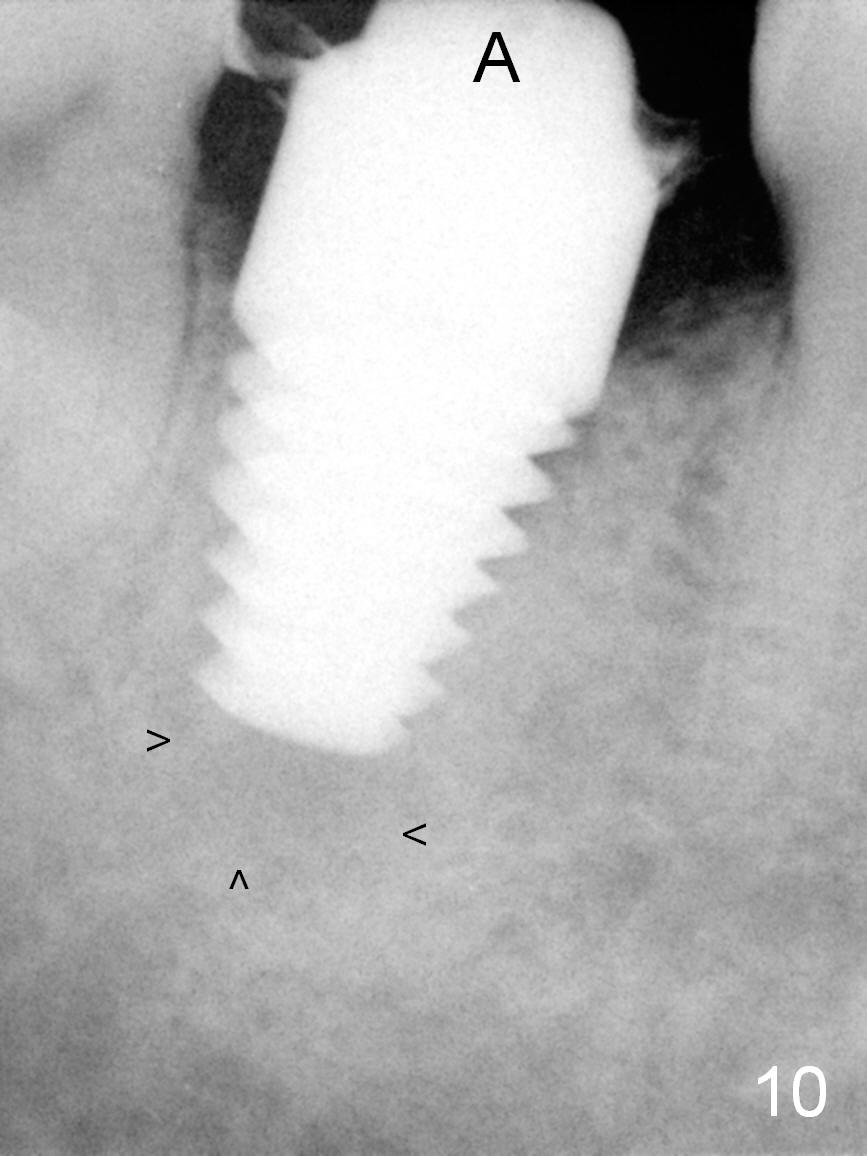
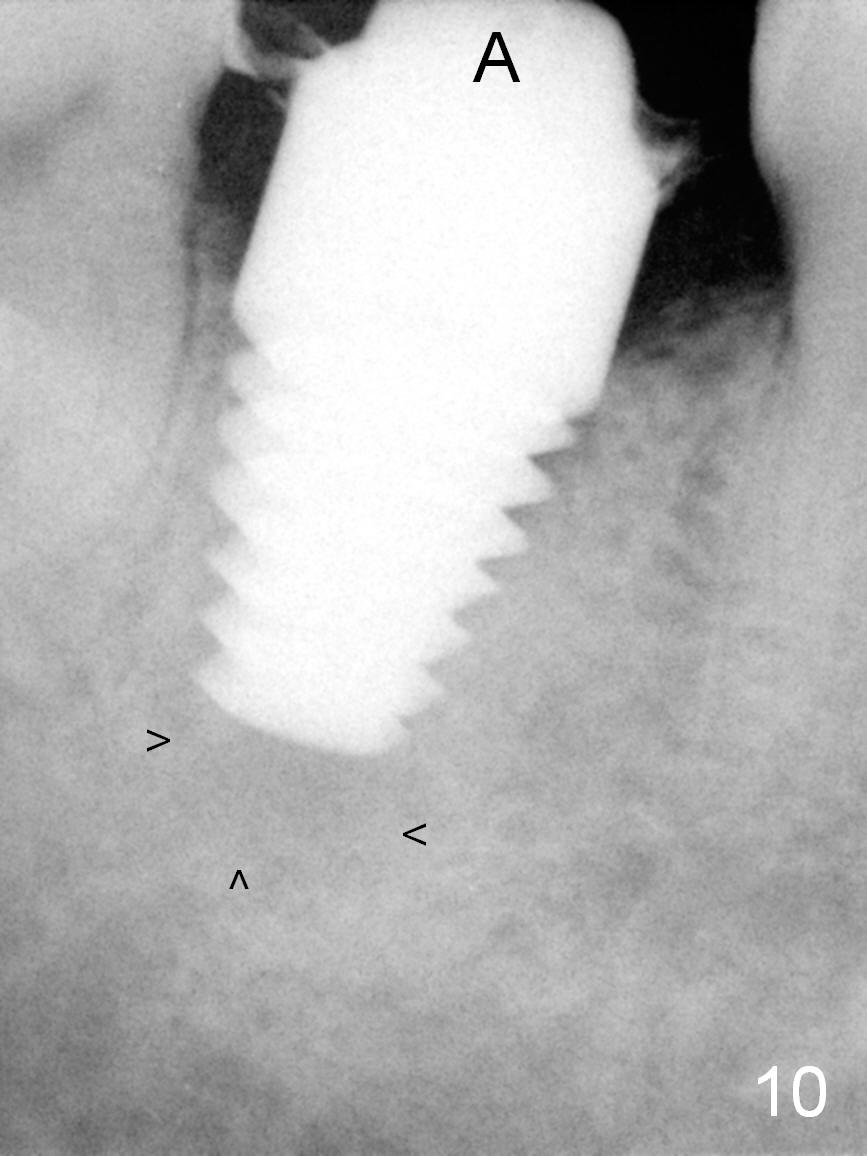
Two months postop, the implant is stable with apparent reduction in size of the apical lesion (Fig.10 arrowheads). Apical lesion appears to be harmless.
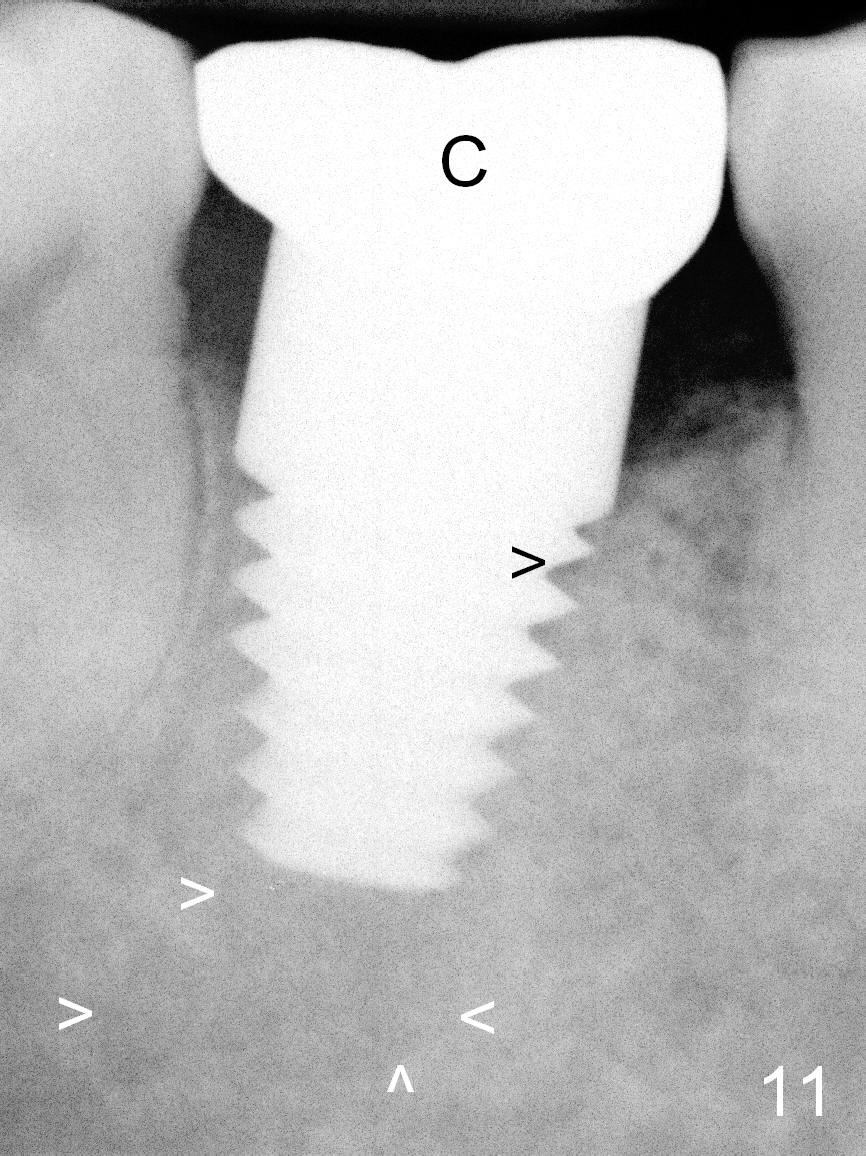
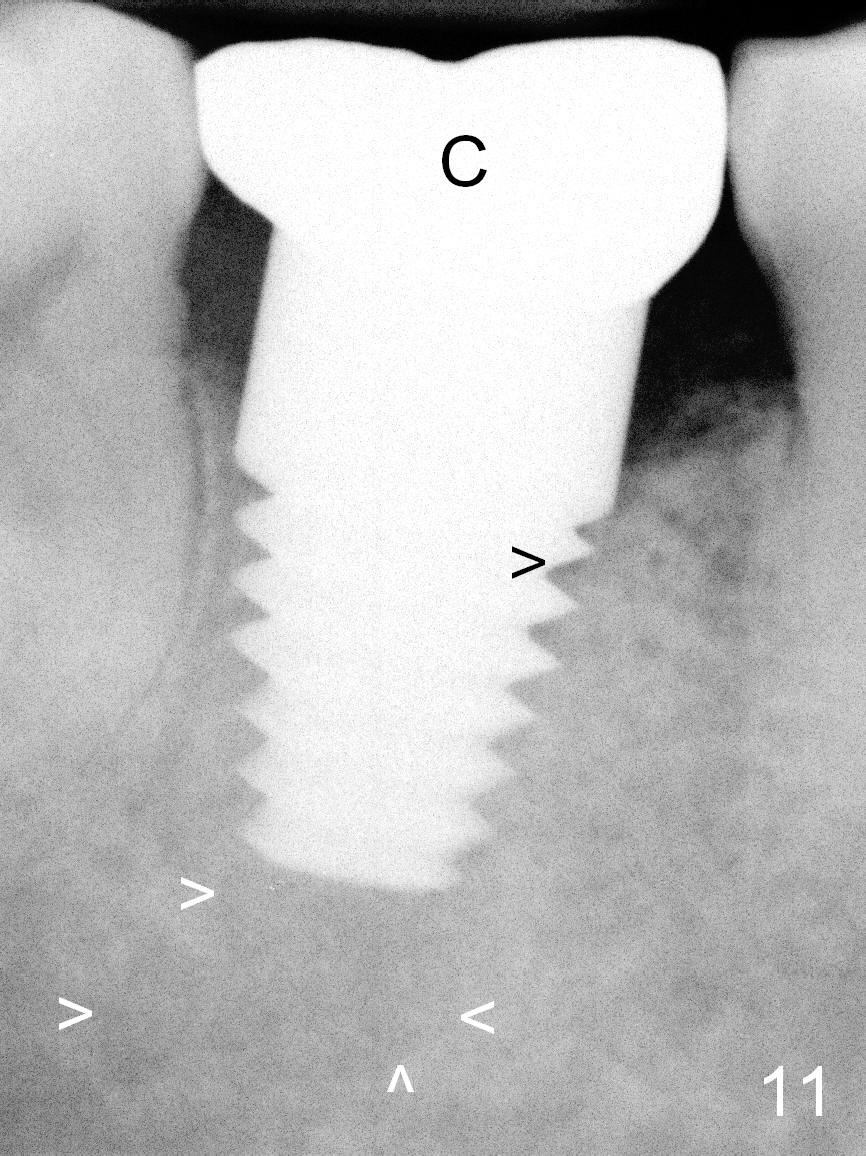
A definitive restoration is cemented 4.5 months postop. The patient returns 2.5 months post cementation (7 months postop) with chief complaint "mild occasional pain around the implant". Clinically there is no sign of infection, although periapical radiolucency does not reduce in size (Fig.11 white arrowheads (C: crown)). Coronally, the bone density increases (black arrowhead).
Return to Lower Molar Immediate Implant
Xin Wei, DDS, PhD, MS 1st edition 05/22/2015, last revision 01/19/2018