




 |
 |
 |
|
 |
 |
 |
|
 |
 |
 |
|
 |
 |
 |
|
Emergency Treatment of Periimplantitis
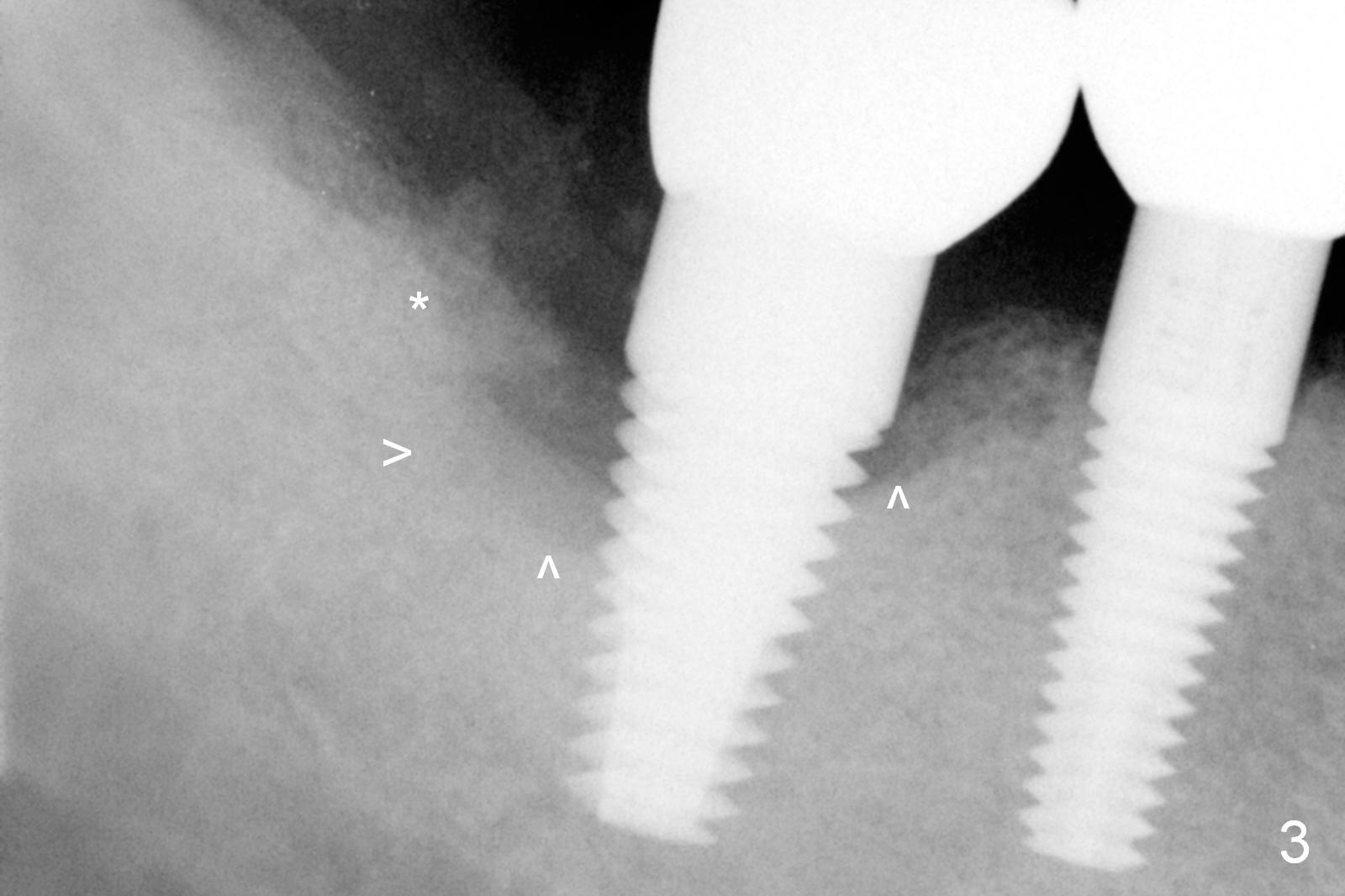
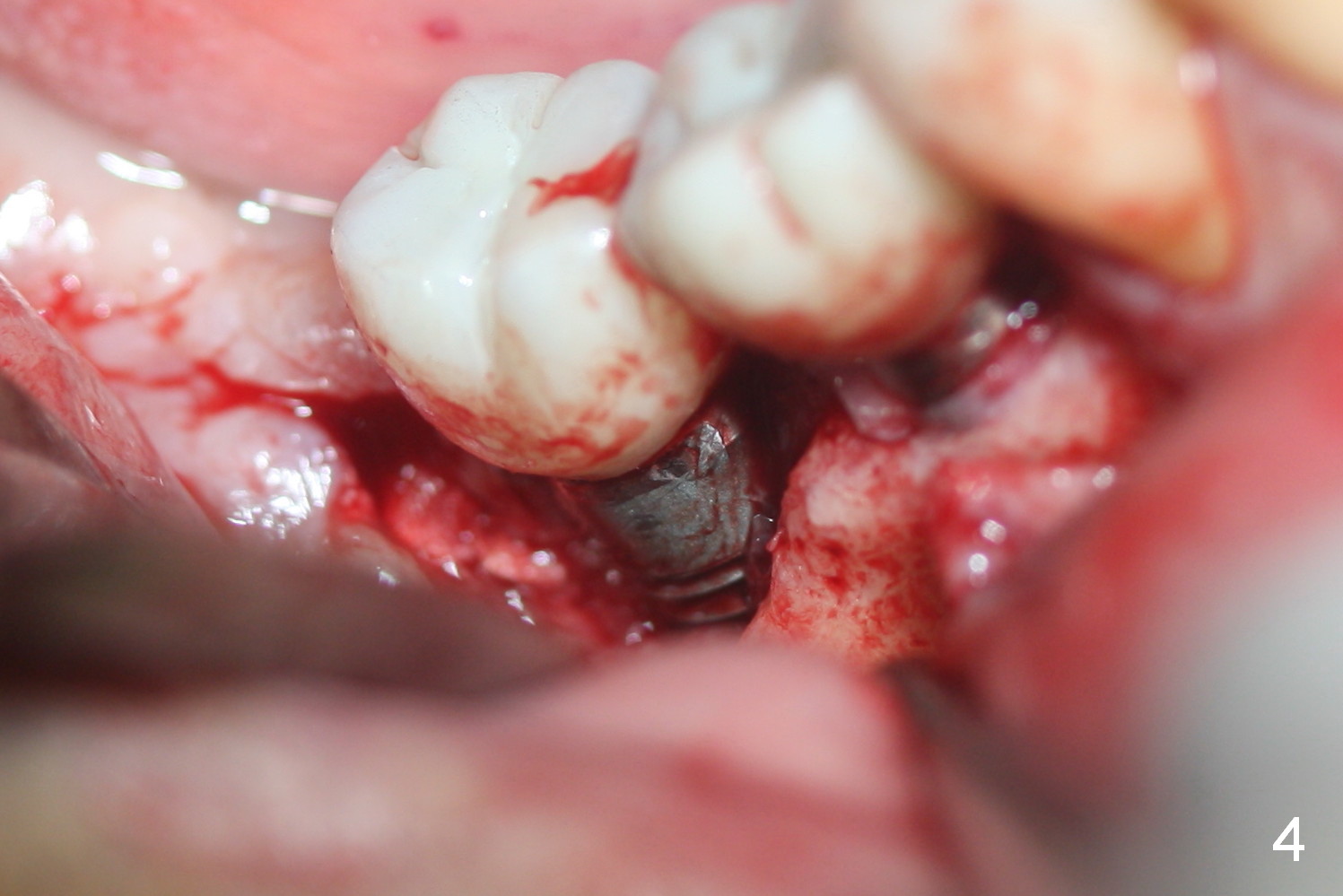
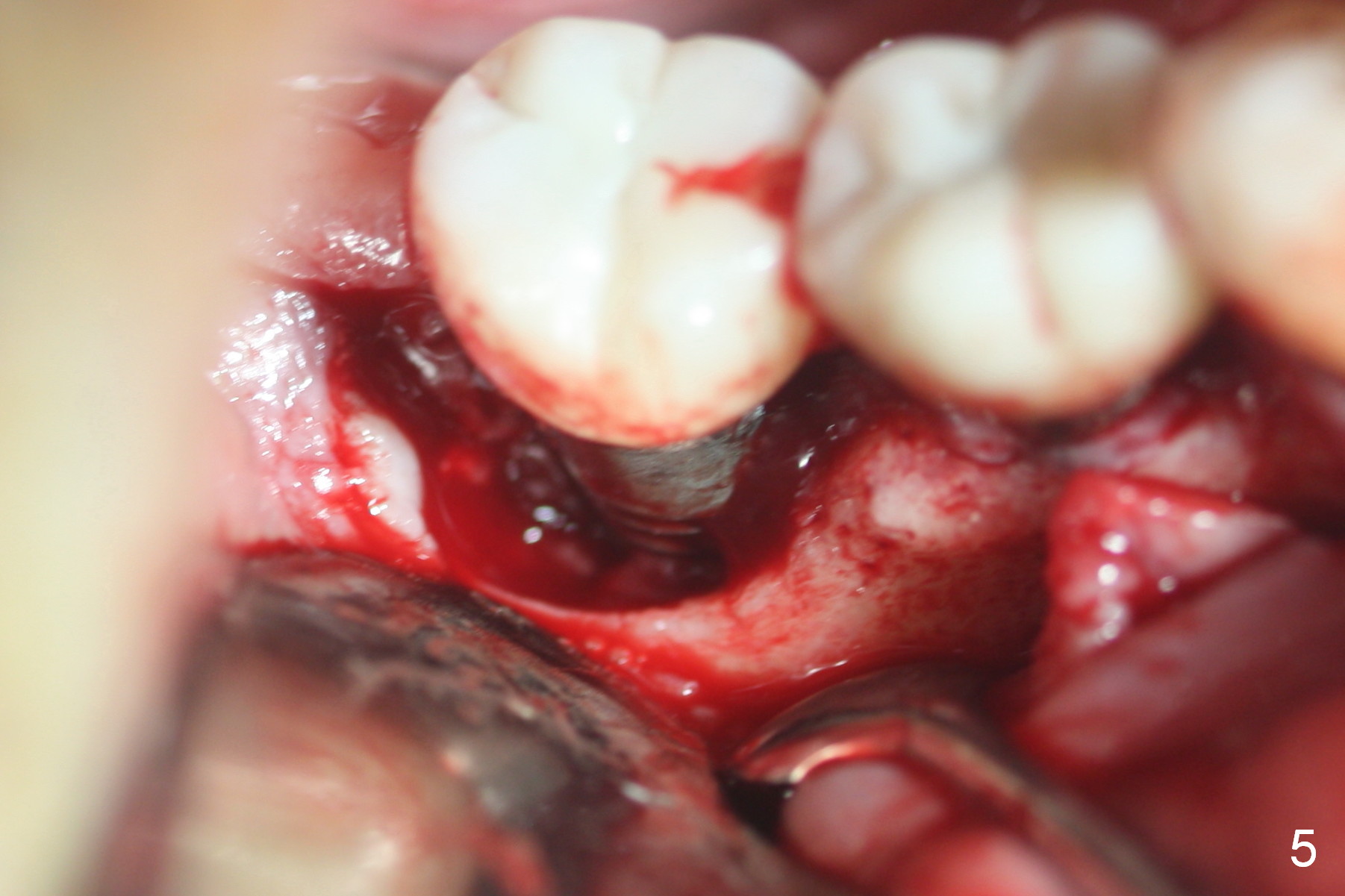
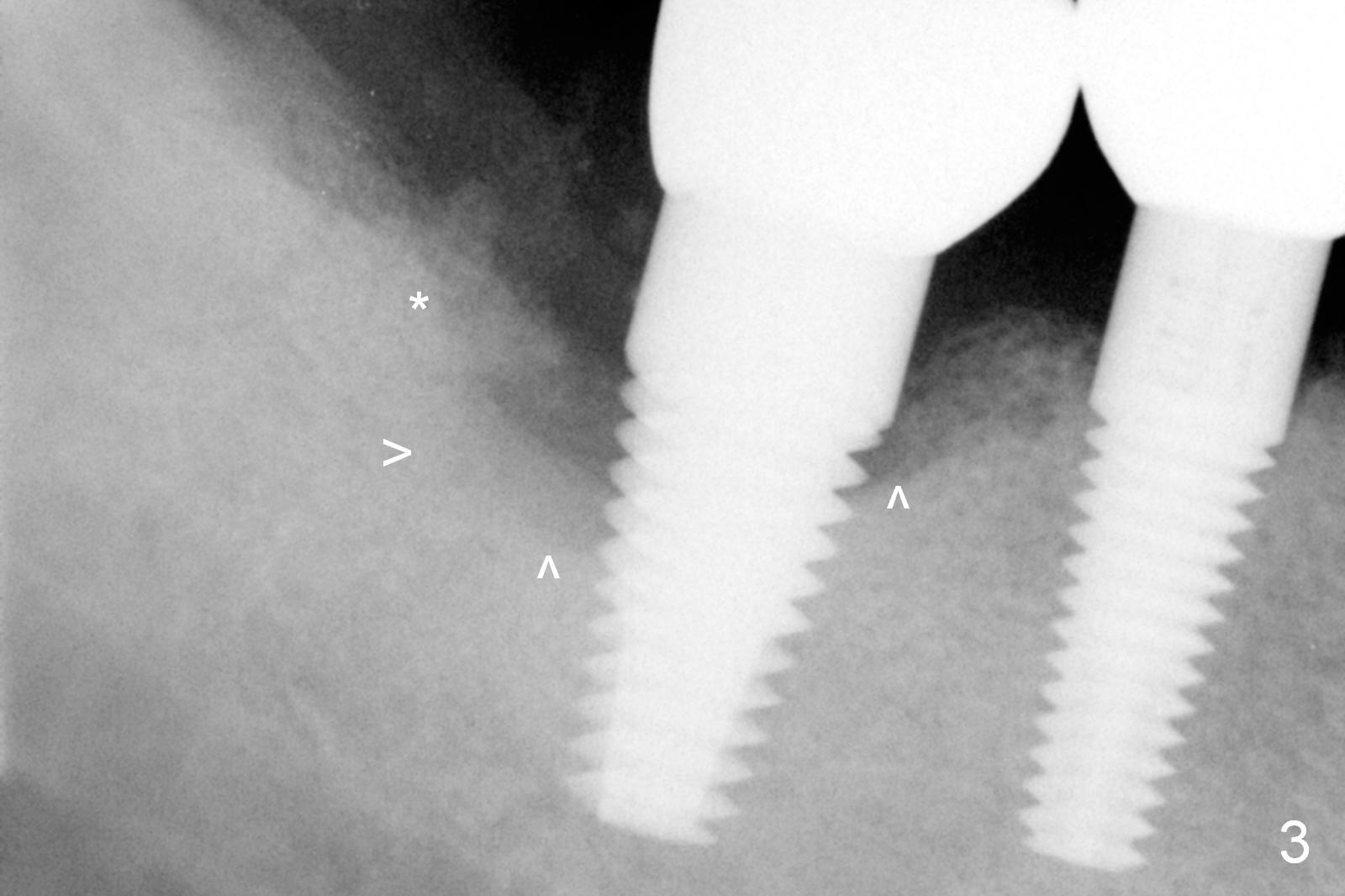
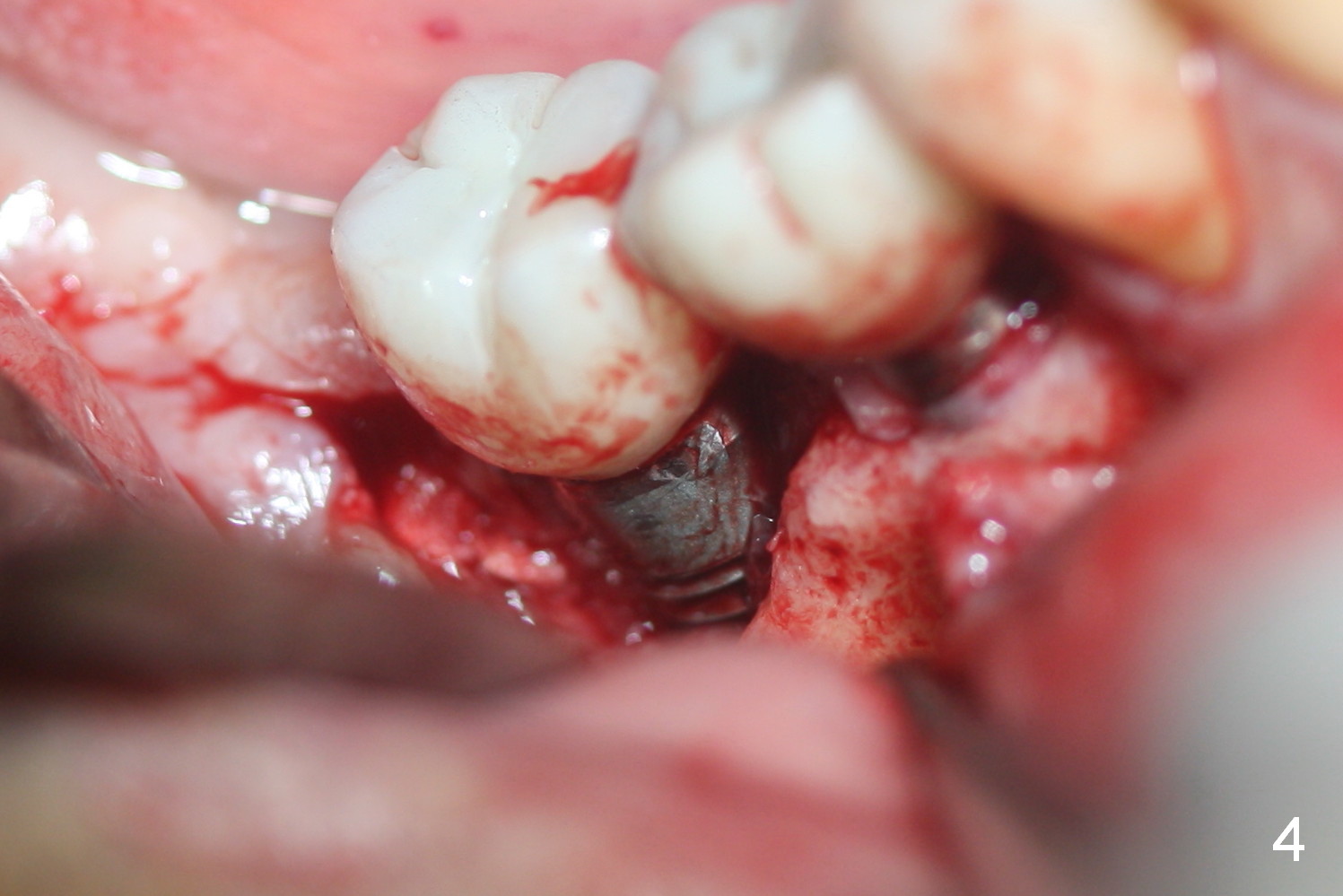
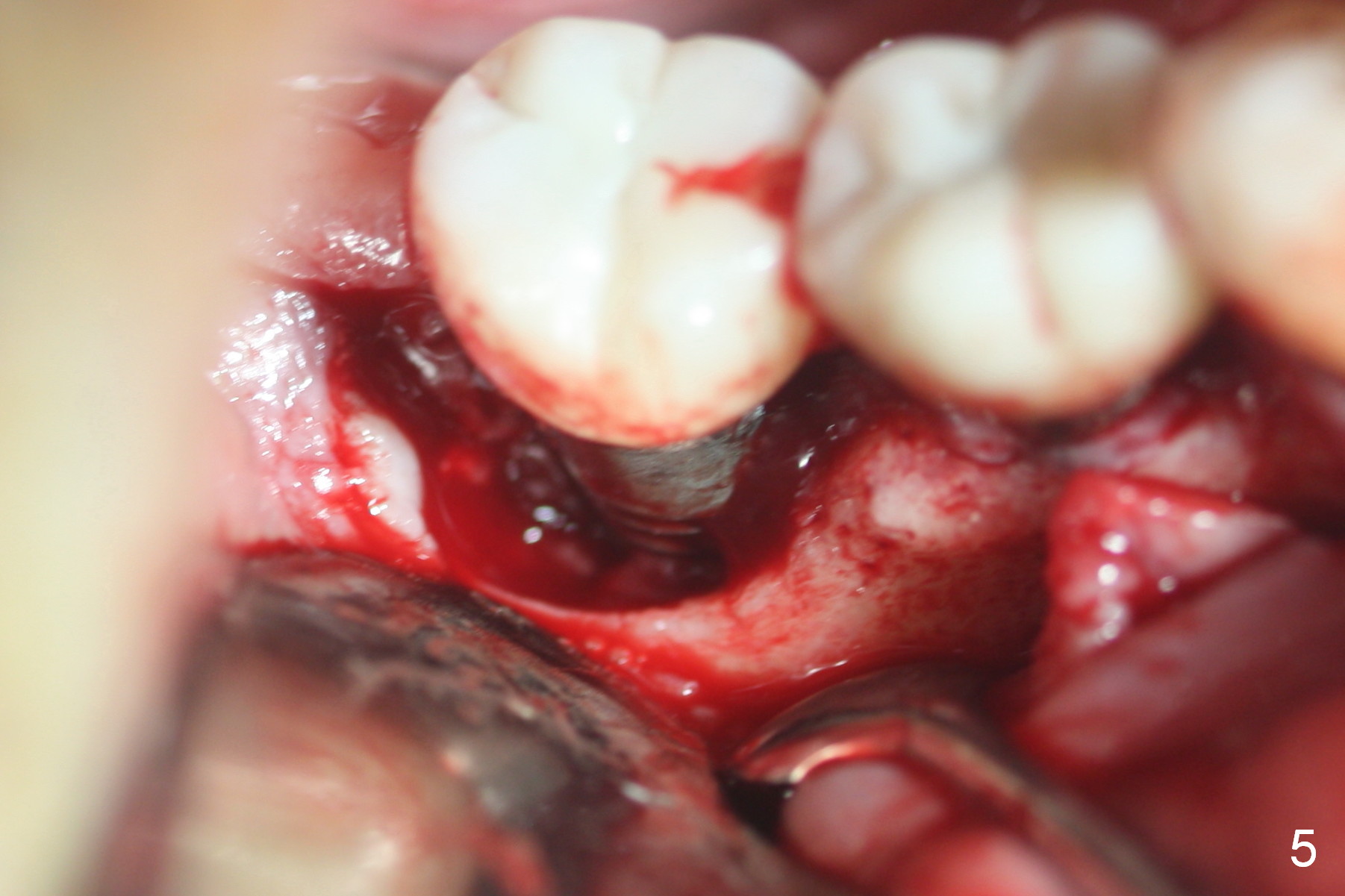
Eleven months post cementation, an acute type of periimplantitis develops at the site of #31 (Fig.1,2 (*)). A crater-like defect forms around the implant (Fig.3 arrowheads), which is confirmed when the buccal flap is raised (Fig.4,5). After granulation tissue removal and use of Titanium brush, the implant surface is clean (Fig.6) and ready to accept bone graft (Fig.7 *).
How to prevent periimplantitis when there is a large and deep defect with a low buccal plate?
Raise the buccal flap after extraction, place an implant as lingual and deep as possible and cover the exposed threads with bone graft and collagen membrane securely.
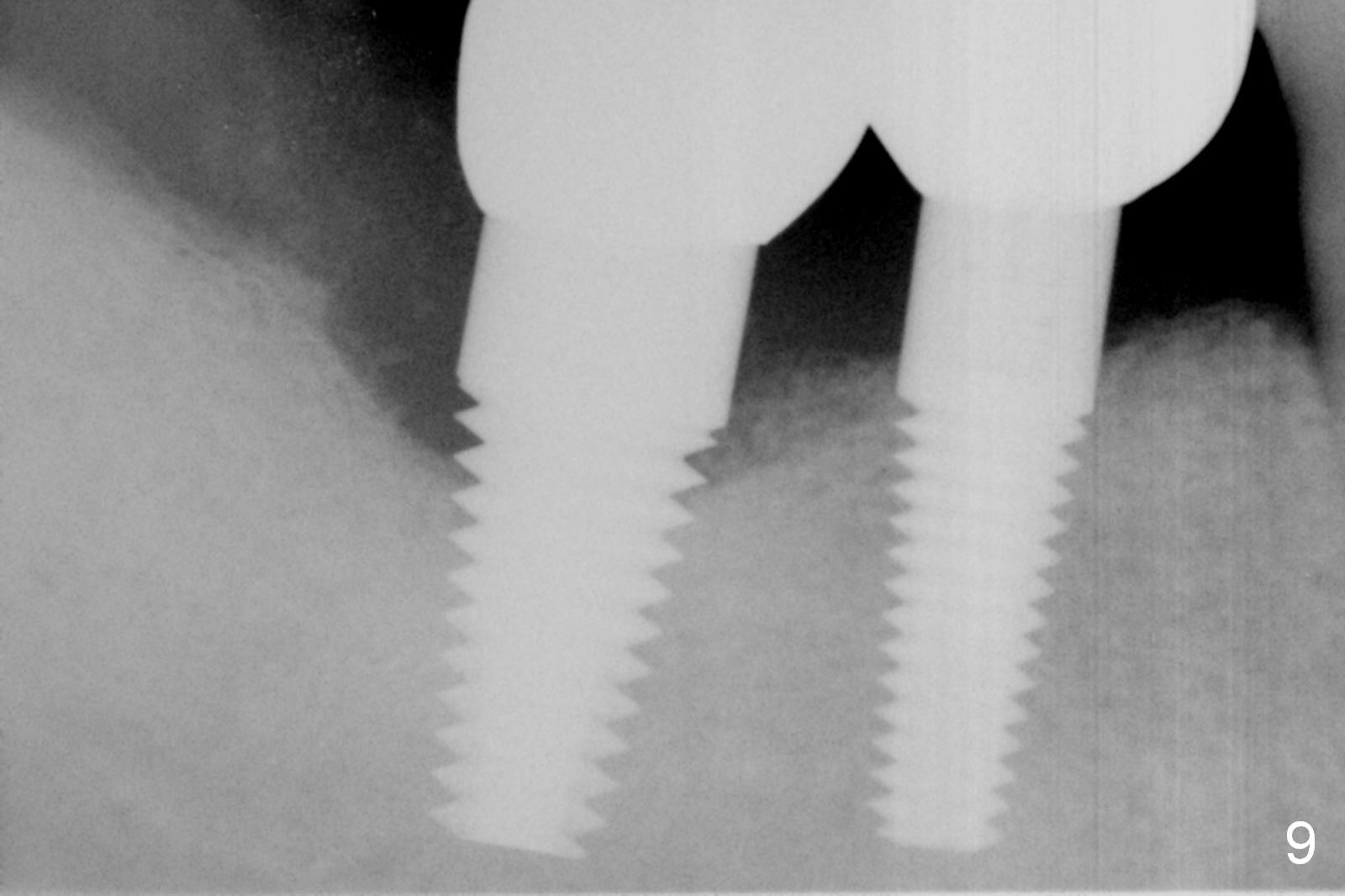
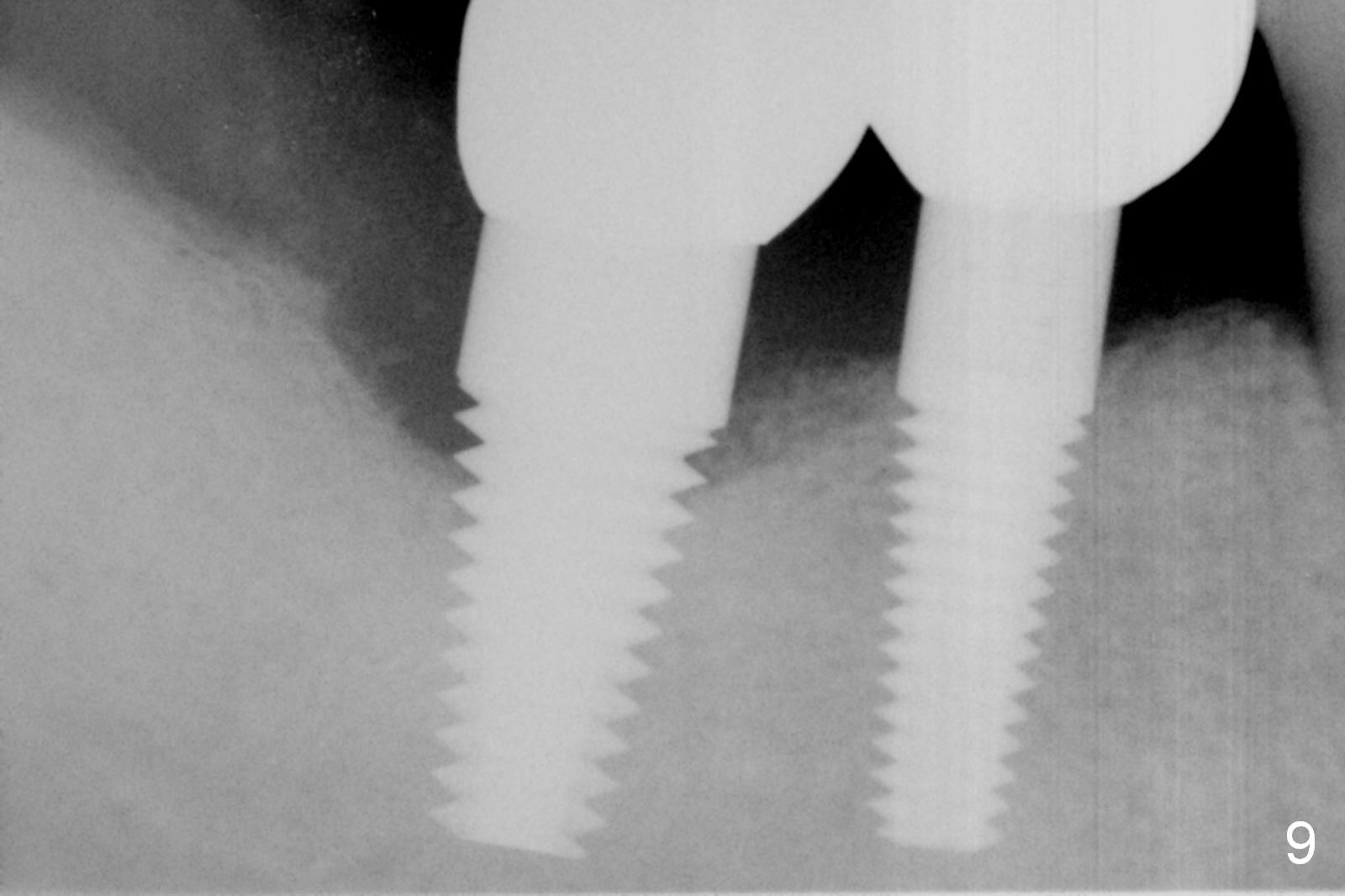
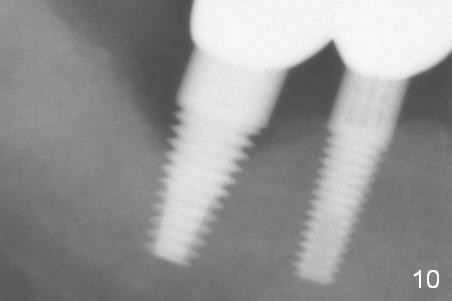
There is no pain postop. The site is examined 3 months postop (Fig.8) when the patient brings his wife for checkup. There is a gap distal, to which a few pieces of bone graft are not attached. It appears that 2 threads are exposed 6 months post graft (Fig.9) and 4 at 13 months (Fig.10). The patient requests retreatment. The latter is either regraft with autogenous bone or remove the implant and replace with bone-level one.
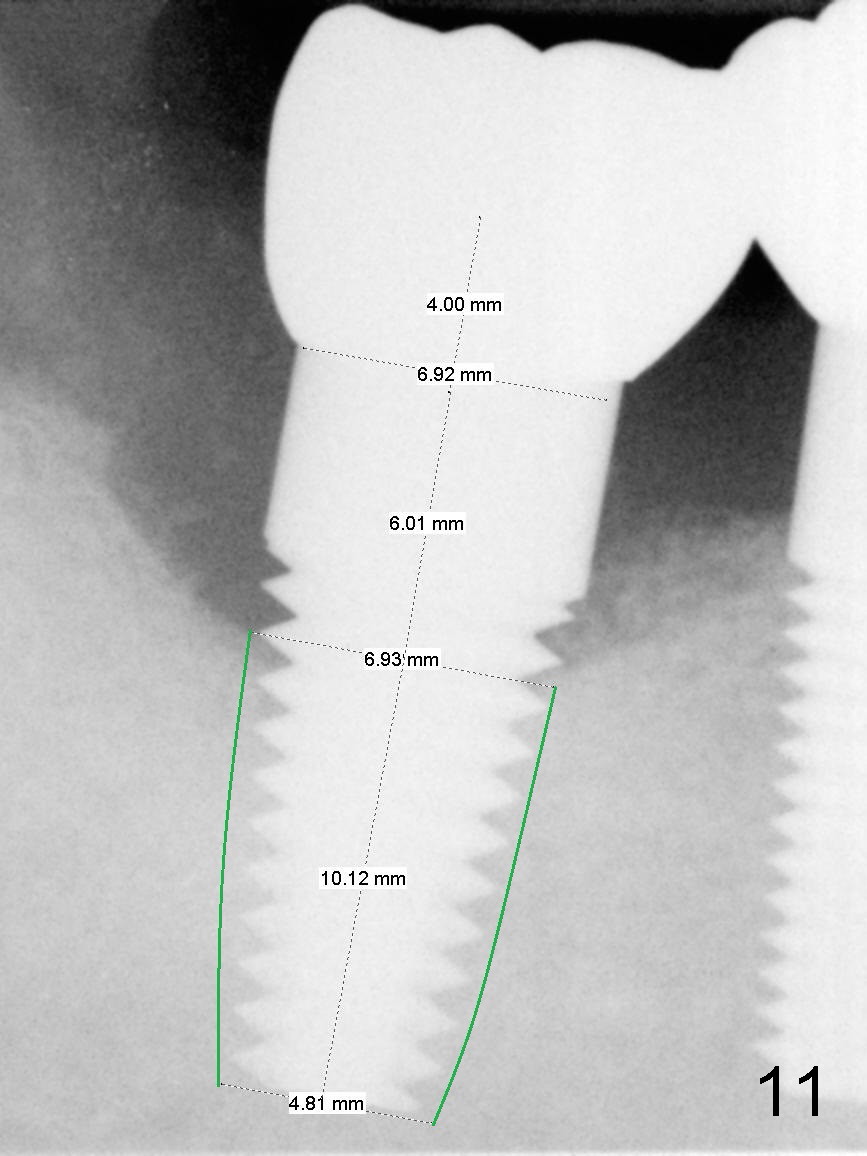
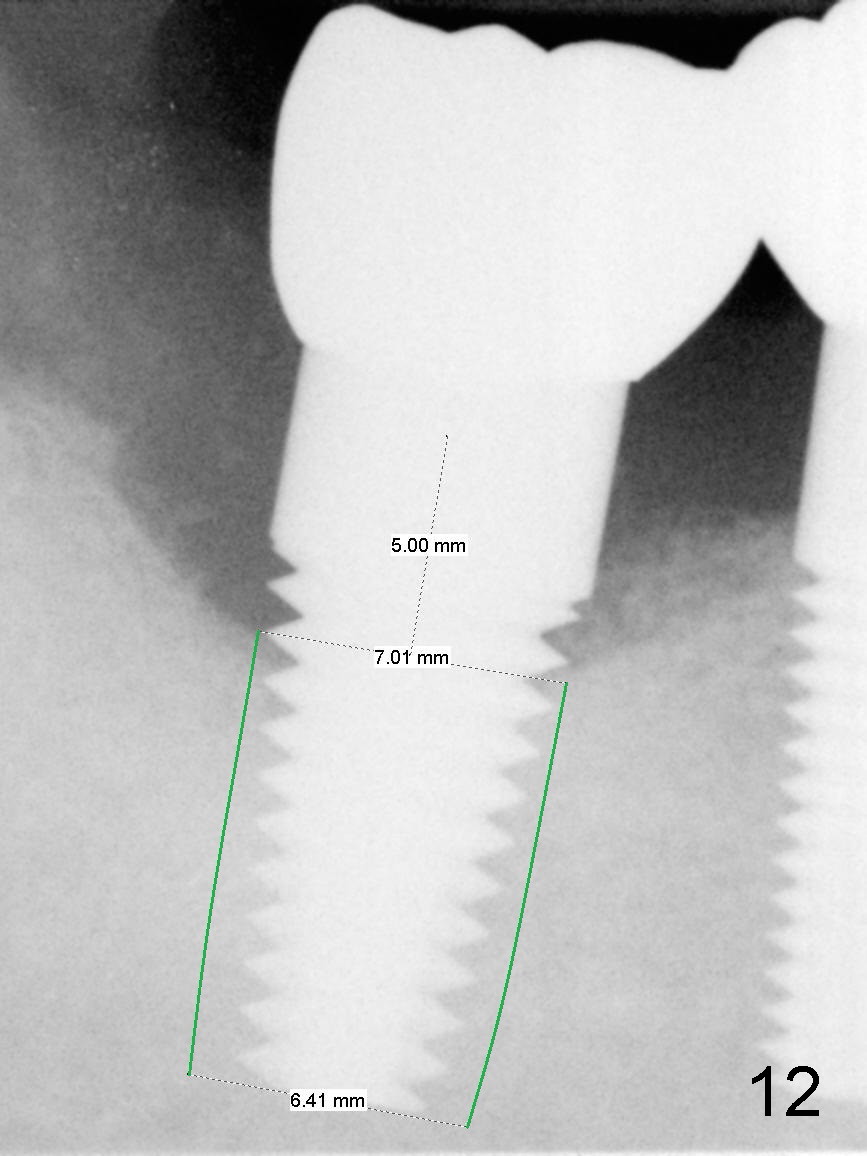
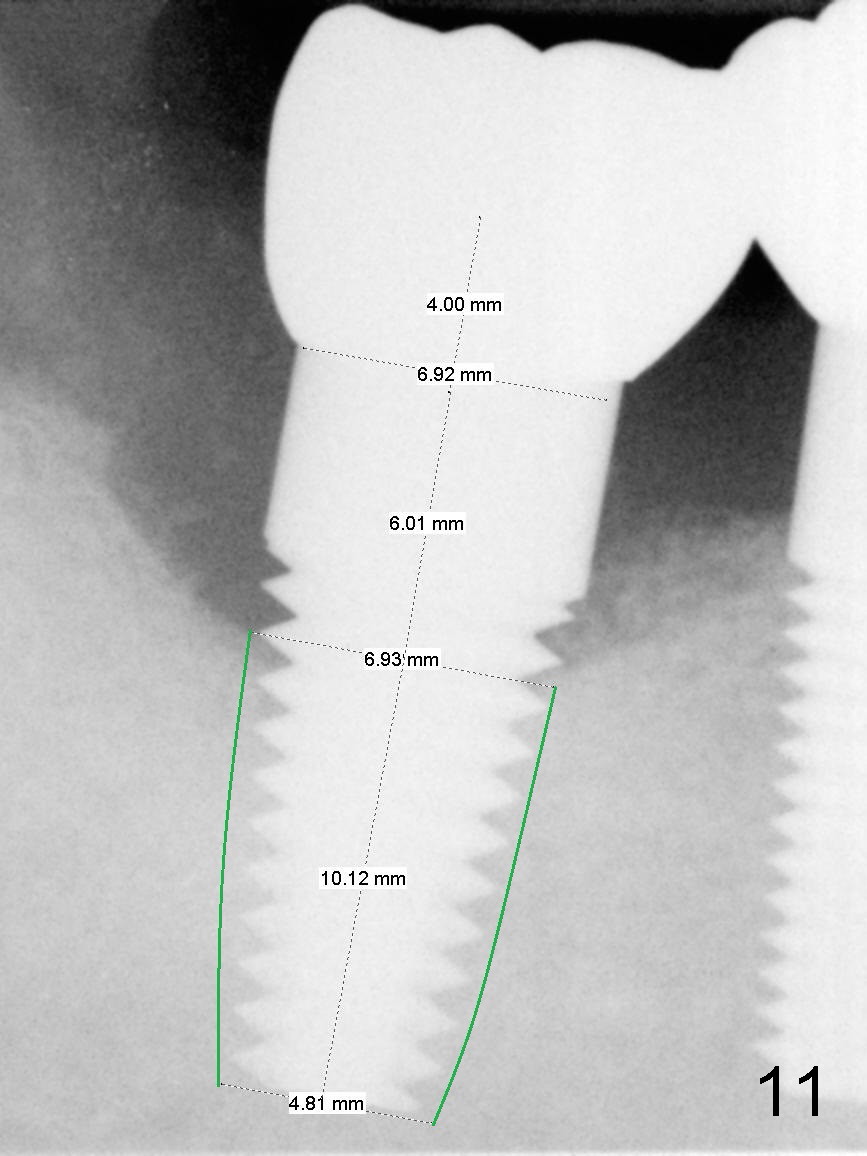
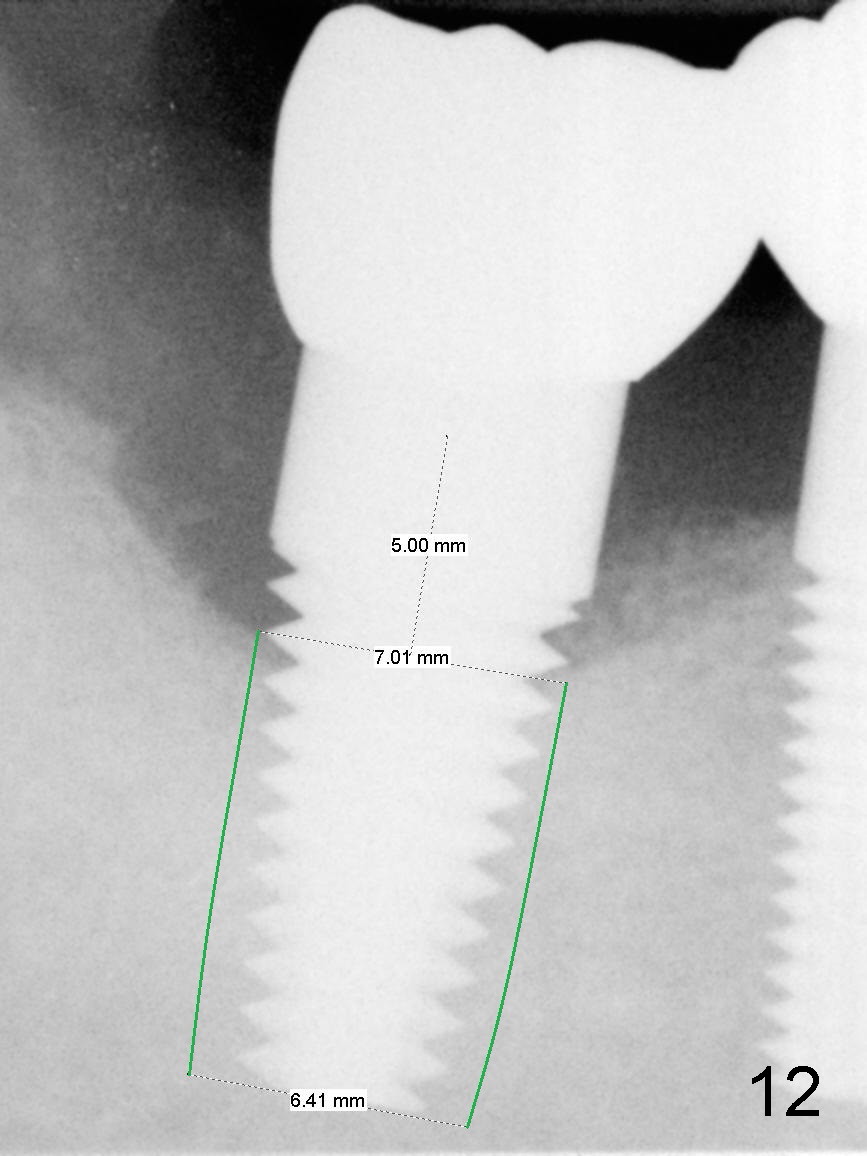
SM will be chosen because it has abutments with the longest cuff (6 mm (Fig.11) vs. 5 mm (UF, Fig.12)). Since the unipost (6 mm 0°) is cemented with Ketac, removing it may be difficult. Still the crown will be sectioned after local anesthesia. Cavitron will be used to remove cement from the Unipost access. Then use Unipost driver to remove the Unipost and Implant driver to reverse the implant.
If the latter fails, make an incision as shown in Fig.4-6 and use elevators to loosen the implant, supplemented by surgical handpiece to deepen the trough. Prepare serrated curette to remove granulation tissue, followed by Metronidazole.
Load SM extra wide taps (5.9-6.9 mm) to form threads and test stability. If the largest tap fails to achieve stability, try UF largest one (7 mm). Note the apical diameter of UF implant is larger than that of SM one (compare Fig.11, 12).
PRF will be prepared to facilitate wound healing. In fact the patient declines blood drawing.
Return to Lower Molar Immediate Implant,
Periimplantitis,
IBS
Xin Wei, DDS, PhD, MS 1st edition 02/12/2016, last revision 03/06/2017