




 |
 |
|
 |
 |
 |
 |
 |
 |
 |
 |
 |
 |
 |
Warning Signs of Paresthesia Associated with Implant Placement
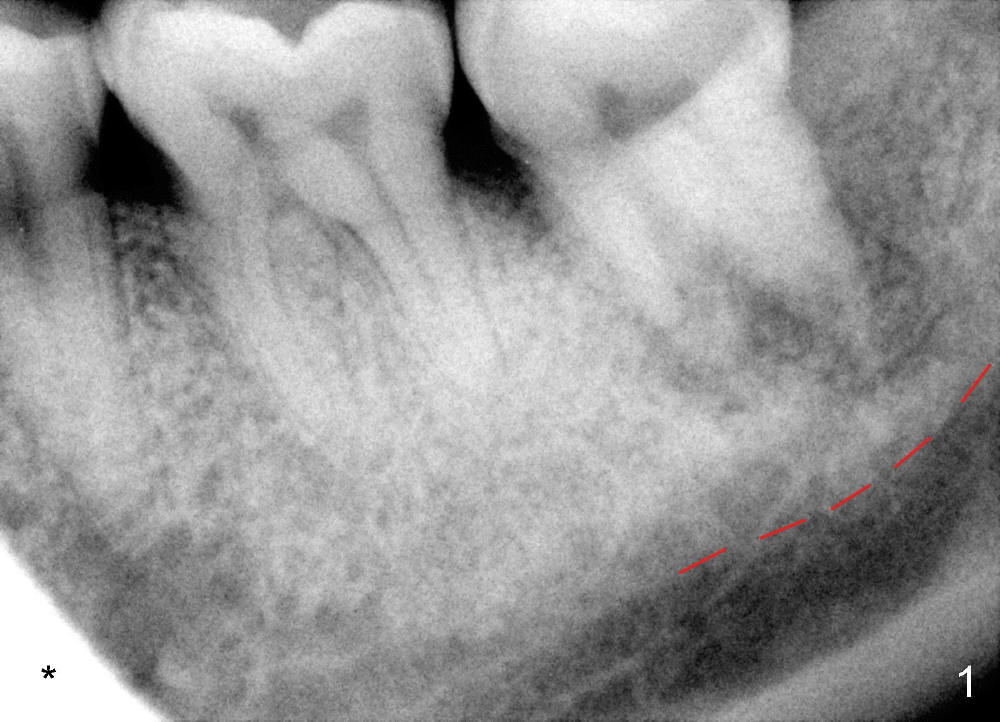
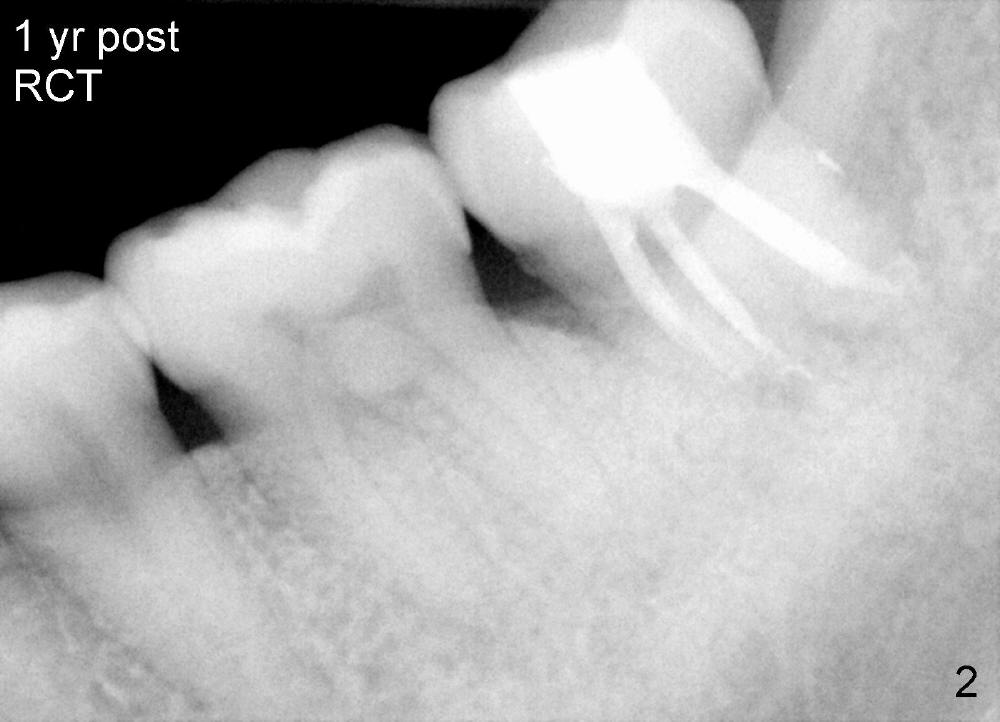
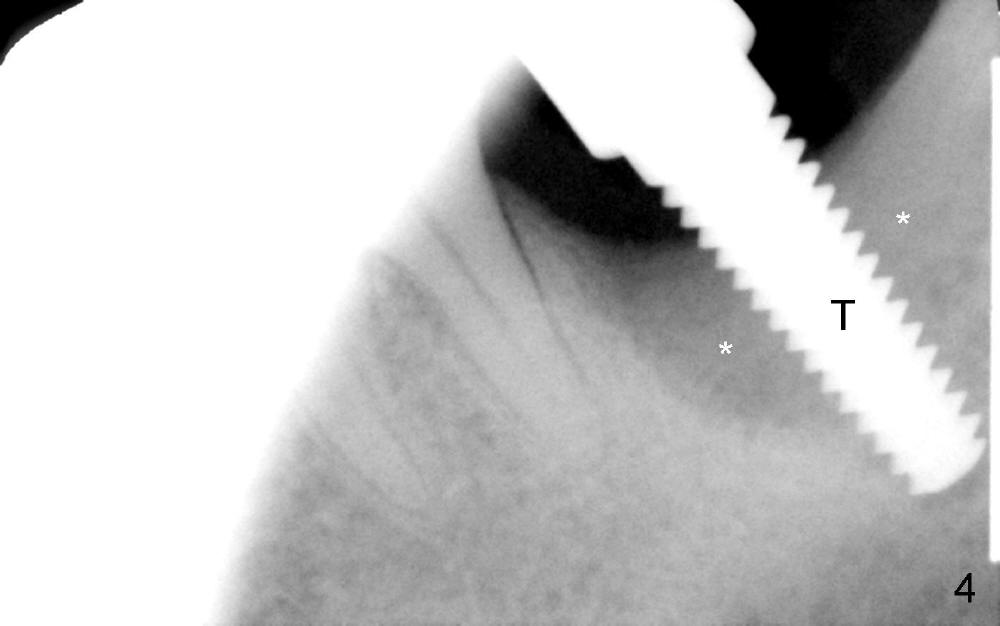
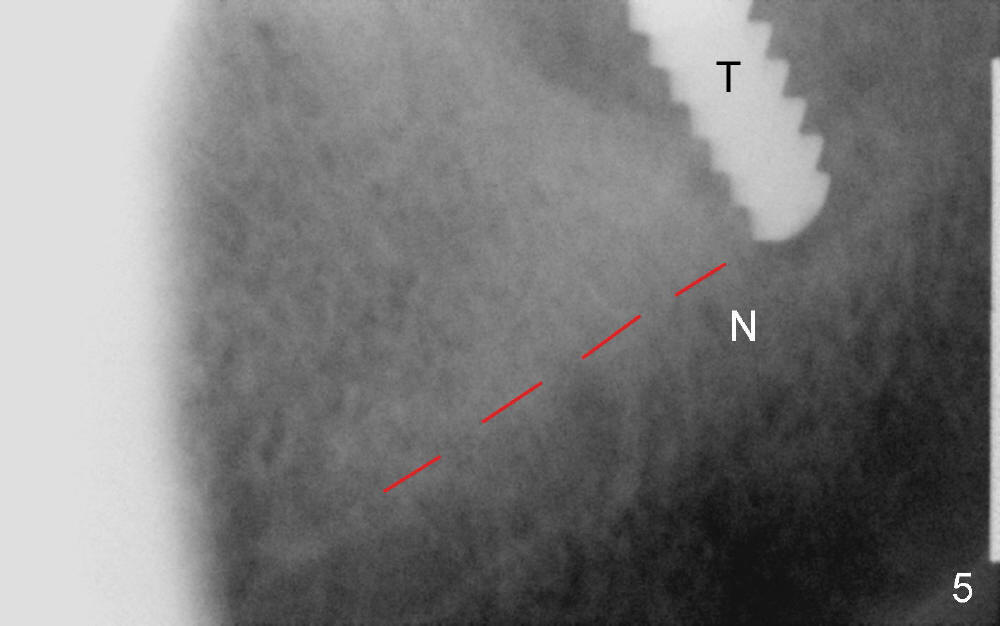
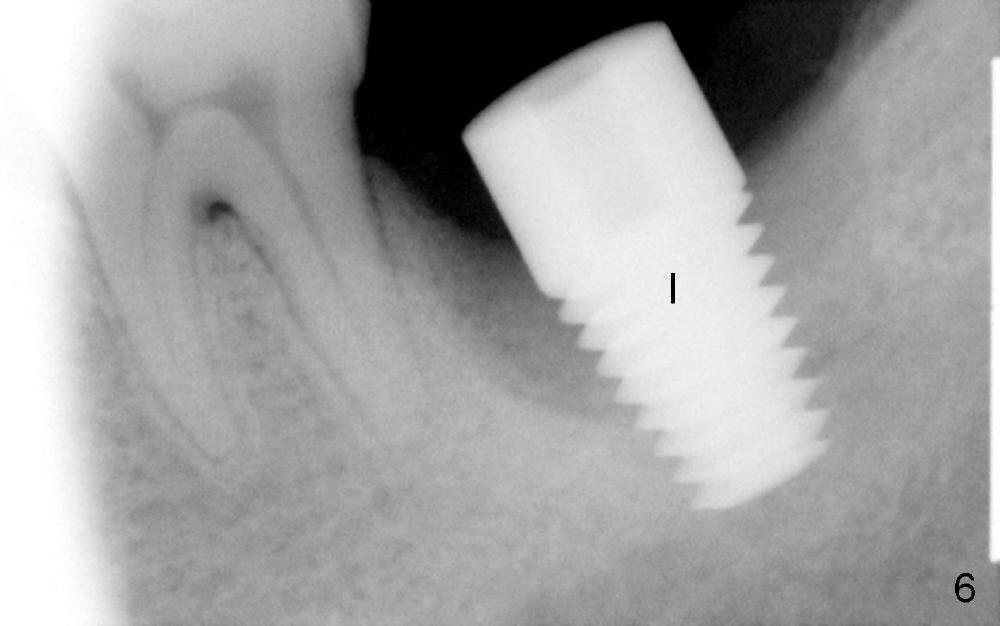
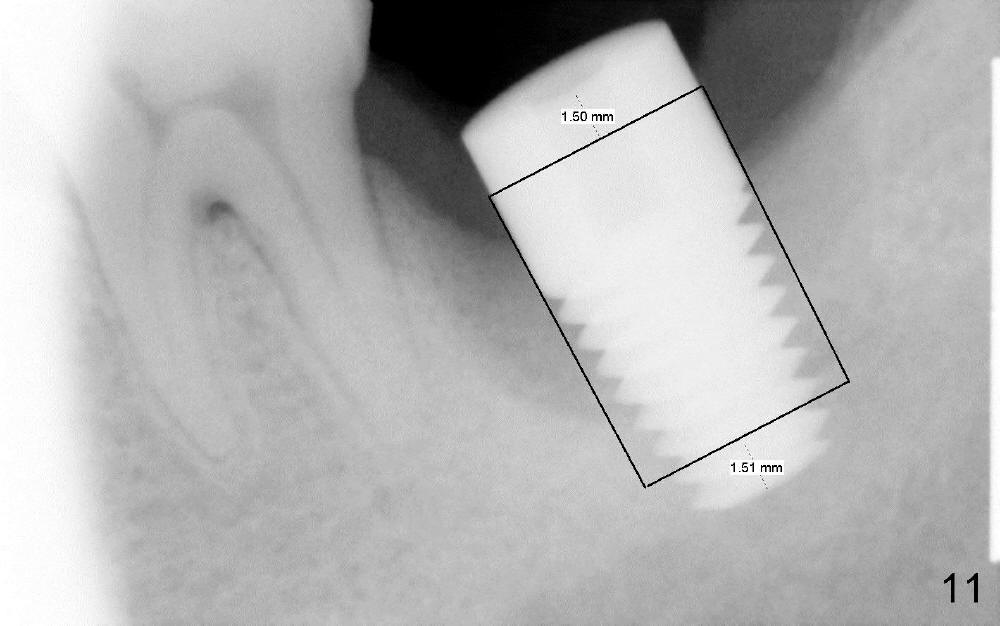
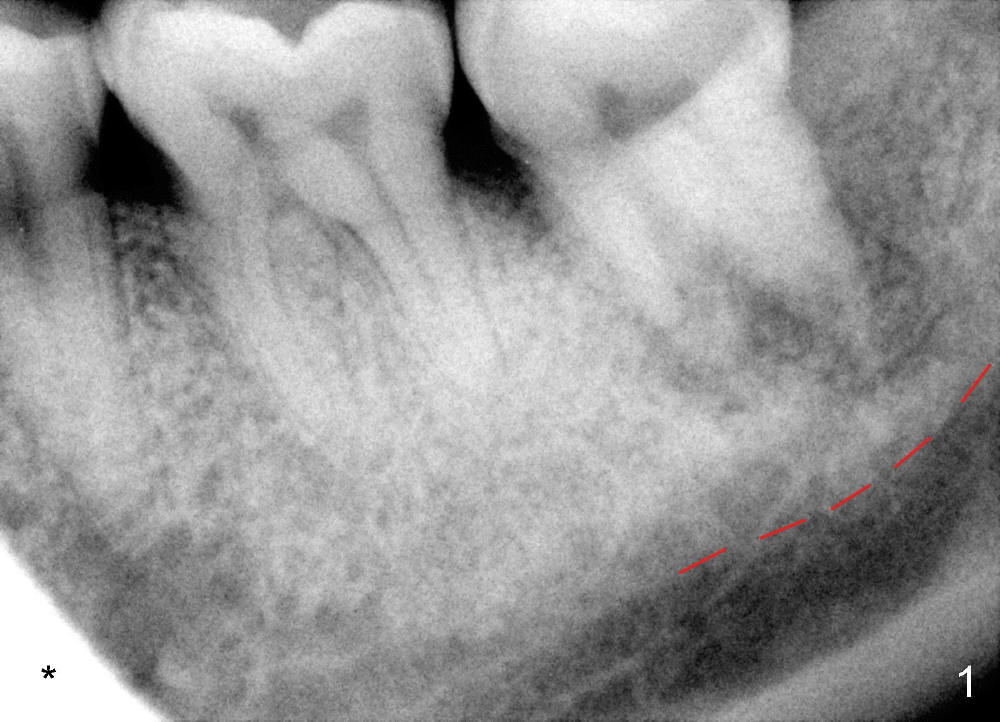
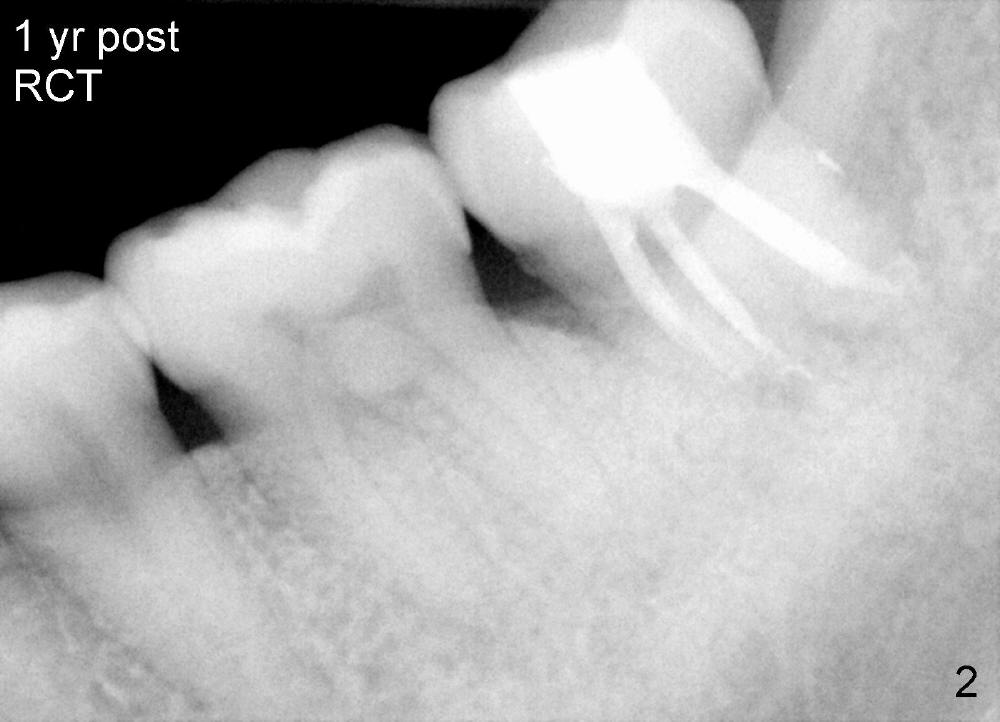
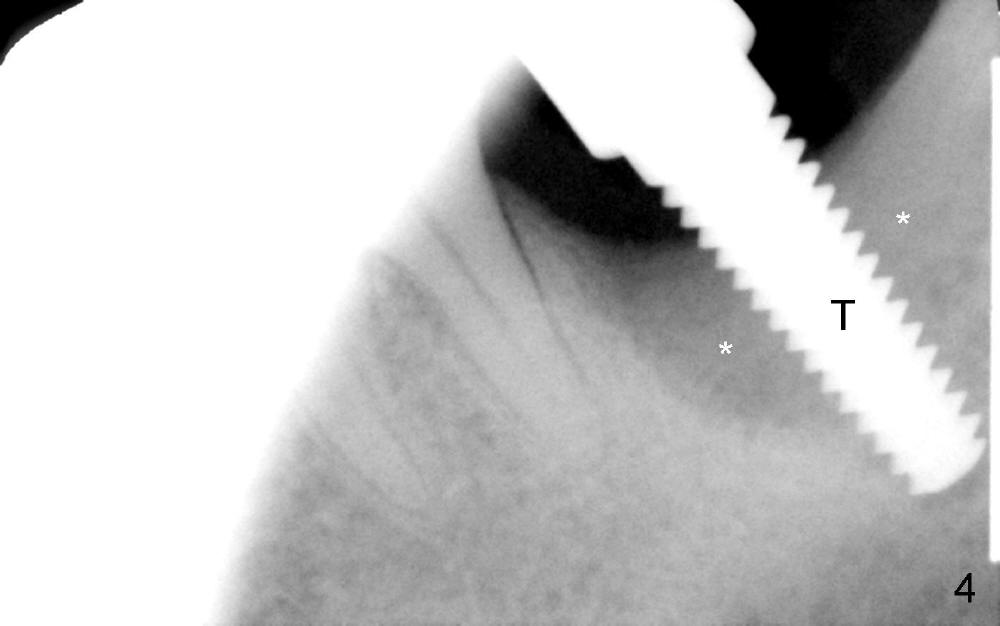
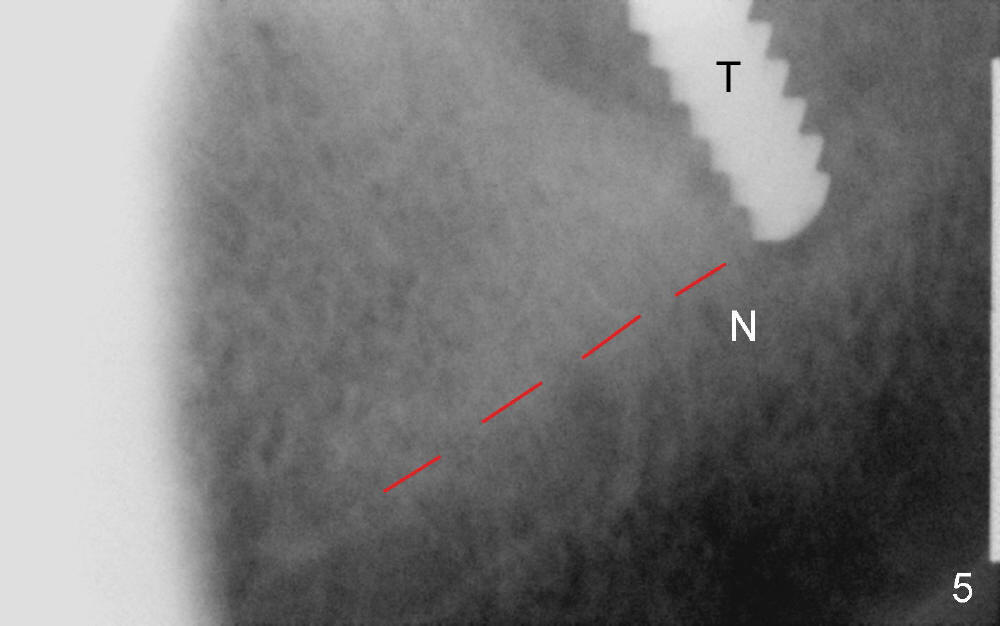
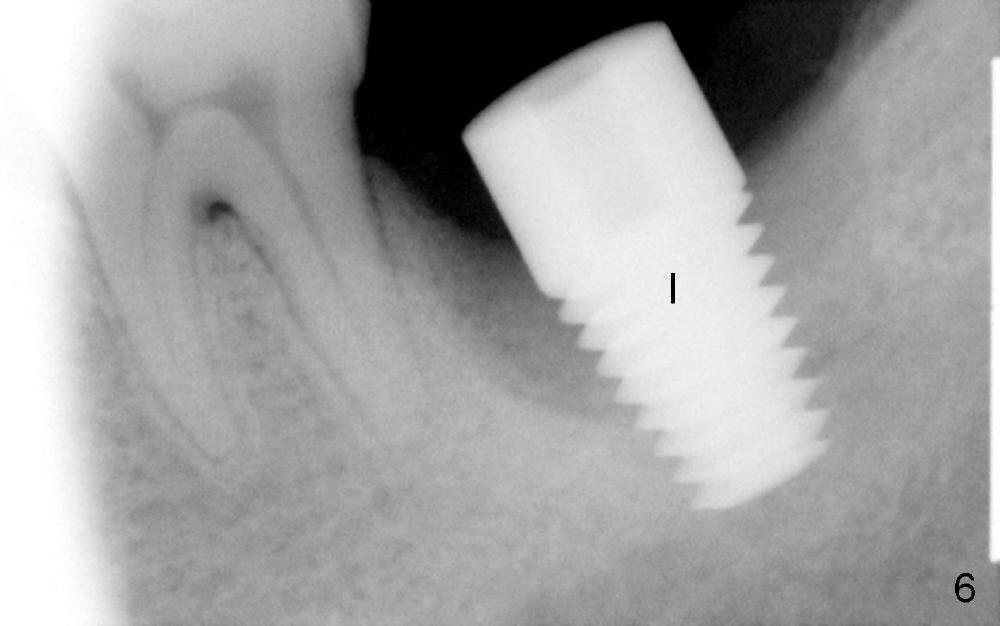
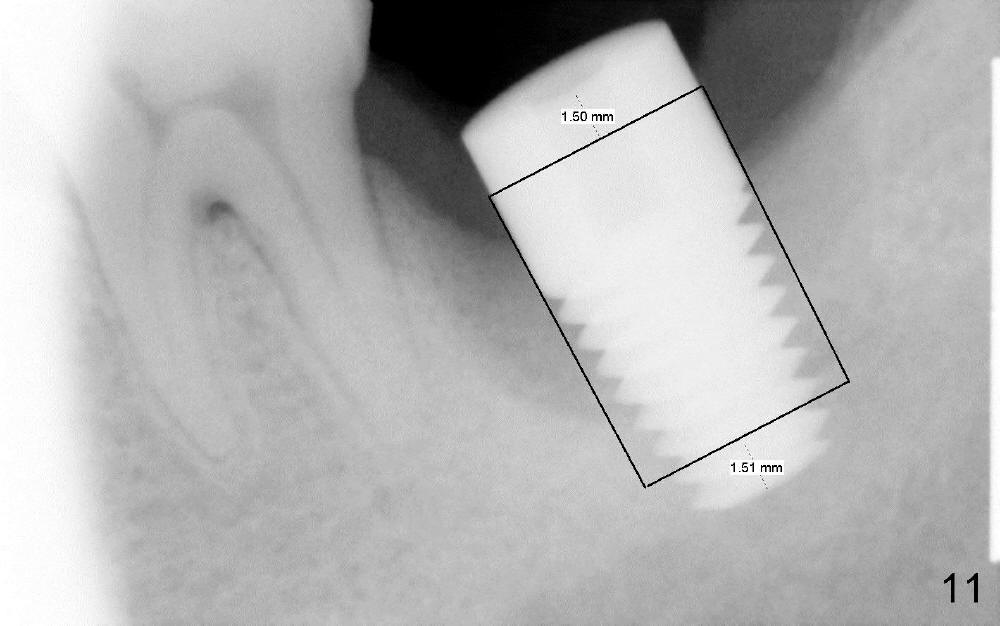
The lower left 2nd molar of a 45-year-old lady has perio-endo disease (Fig.1). The patient is not only very nervous, but also active in gag reflex. It is difficult to take good preop PA (Fig.1 *: ). Root canal therapy is performed. A relatively good PA is taken 1 year postop, again due to gap reflex (Fig.2). The tooth is still nonsalvageable (Fig.3). The last PA is taken 3.5 years before extraction and immediate implant. Infiltration anesthesia is administrated first. The patient experiences pain during early stage of osteotomy, but she does not report readily. Block anesthesia is added. Intraop PAs are taken with difficulty (Fig.4,5 with #1 sensor; 5 mm tap in place). Invasion of the inferior alveolar canal is not noted (Fig.5 dashed line). Oozing is a little more than expected. This is ignored. A 7x14 mm tapered implant is placed; the upper border of the inferior alveolar canal is not intact (Fig.6). Paresthesia area is defined next day (Fig.7). The implant is reversed for a few turns. Paresthesia area is reduced 19 days later (Fig.8). The implant is not stable. Follow up PAs are taken with difficulty (Fig.9-11). It appears that a shorter cylindrical implant is more appropriate for this case (Fig.11). The implant is stabilized with splinting with questionable result (Fig.12).
In summary, the following are warning signs of potential nerve injury: nervous patient, gap reflex (difficulty in taking PA), pain with infiltration anesthesia, and active oozing from osteotomy site.
How to avoid the complication? Take CBCT for gagging patients. Use shorter implants. Avoid immediate implant when the bone height is questionable and lesion is extensive. There is usually active infection associated with immediate implant. Pain control may be difficult. It may be confused with nerve injury. Do not administrate block anesthesia unless there is distinct clearance. Abort surgery if needed!
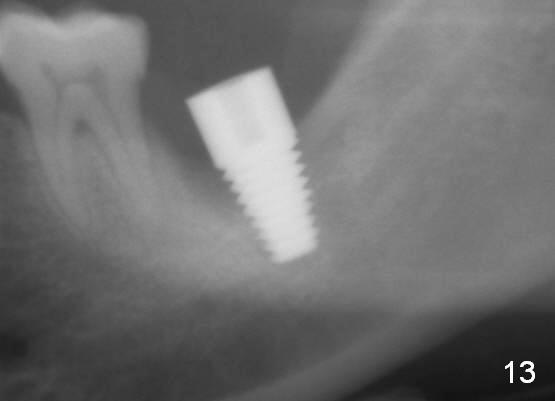
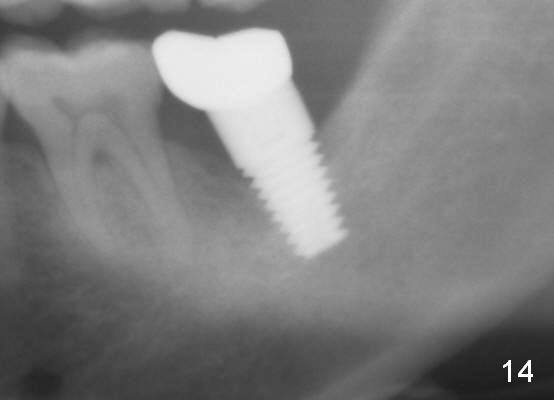
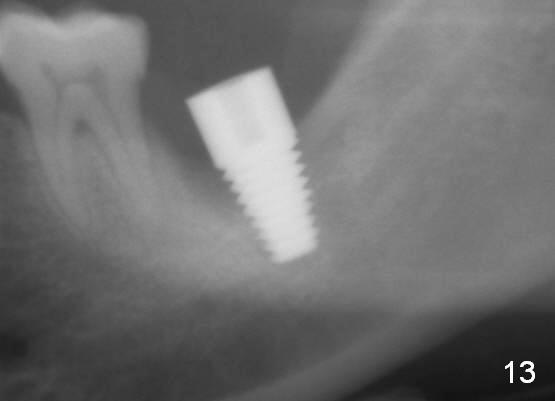
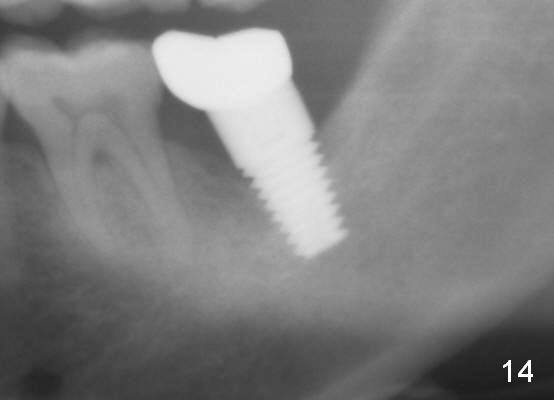
There is bone growth in the mesial socket 1 year postop (Fig.14, as compared to Fig.13 (immediately postop, before back up). Mild paresthesia remains 2 years postop.
Return to Lower Molar Immediate Implant
Xin Wei, DDS, PhD, MS 1st edition 05/04/2014, last revision 01/19/2018