 |
Protocols to Prevent Periimplantitis of Molar Immediate Implants
Goal: To reduce periimplantitis to <5% 1 year post cementation of final crown
Introduction: It appears that the incidence of peri implantitis associated with molar immediate implants is relatively high, probably due to poor oral hygiene (back in the mouth), poor visibility, complex anatomy and severe lesion. Although there is no cosmetic issue, it is difficult to treat.
Protocols
1. Which molar is more likely to develop periimplantitits, 1st or 2nd, upper or lower?
2. The most critical point to prevent periimplantitis is to place an implant within the confinement of the bony socket. In the esthetic zone, an immediate implant should be placed as palatal as possible so that there is 2 mm gap buccal to the implant. The same principle must be applied to the posterior immediate implant.
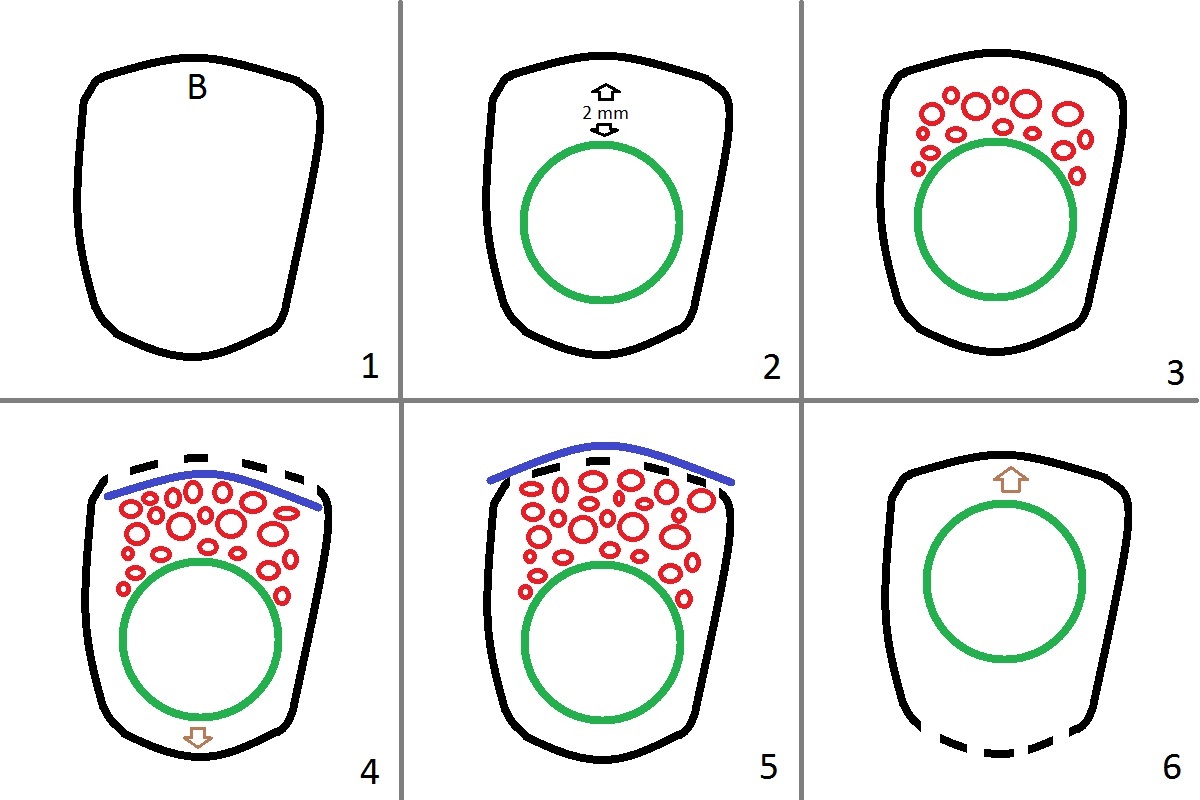
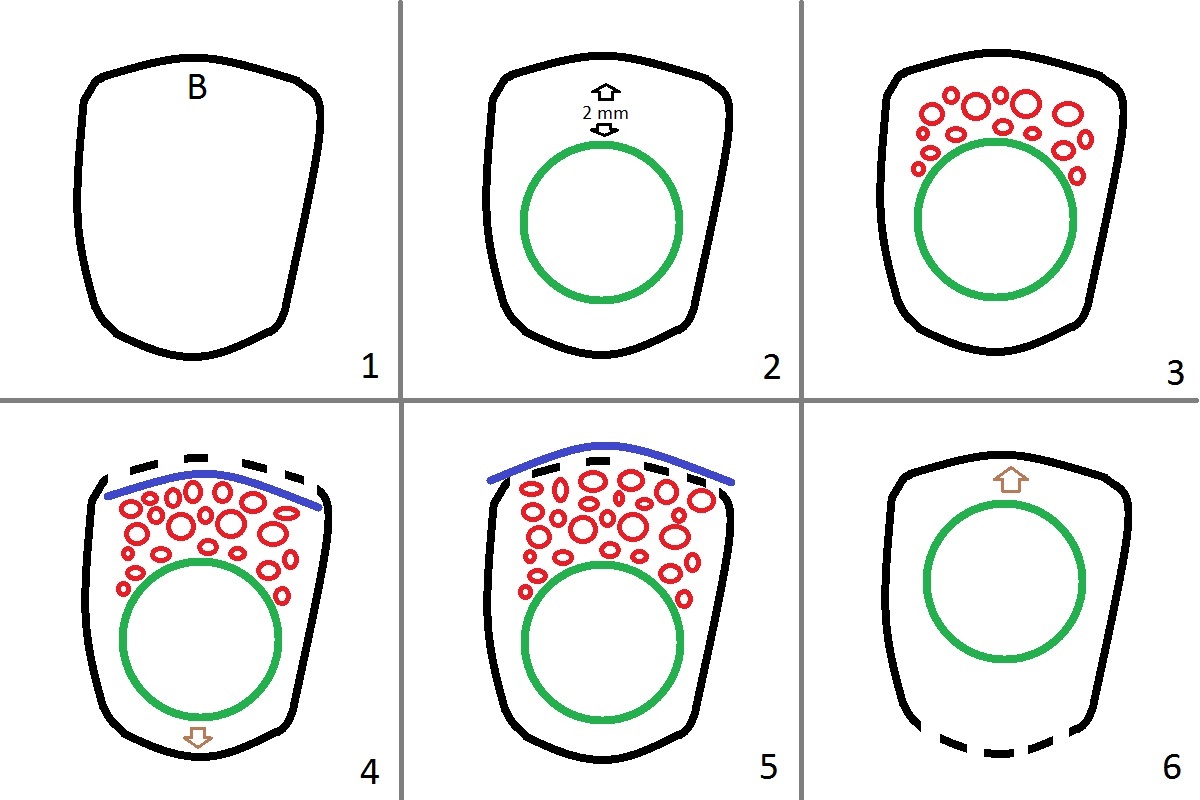
Fig.1 is an occlusal view of an upper molar socket with buccal (B) on the top. When the socket wall is intact, place an implant slightly palatally with 2 mm gap (Fig.2) so that fair amount of bone graft can be placed (Fig.3 red circles). If the buccal plate is defective (Fig.4 dashed line), the implant should be placed further palatal (arrow) so that there is more buccal gap to be filled with bone graft. A piece of collagen membrane is placed either inside the socket for flapless approach, Fig.4 blue curved line) or buccal to the buccal mucoperiosteum (Fig.5, flap approach (incision)). When the palatal wall is defective (Fig.6), the implant should be placed buccally (arrow).
3. Tissue- or bone-level implant: The gingival height of tissue-level implants is fixed (3 mm). If the crestal bone is not even to large extent, it would be prudent to use bone-level implant and place it as deep as possible. Its cemented abutments have various lengths of cuff: 1-5 mm. If bony defect is limited, place a reasonable diameter implant with primary stability so that the implant will be most likely in the middle of the socket if the initial osteotomy entrance in the middle of the socket. To have the best emergency profile and reduce the chance of food impaction, place an abutment as large as possible. In case the bony defect is extensive, use a tapered or cylindrical tissue-level implant, since the largest one is 8 mm, vs. 7 mm for bone-level one.
4. Flapless or flap approaches: Try to use flapless approach routinely. If visibility is poor due to hemorrhage or position, do not hesitate to make an anterior (1 tooth mesially) oblique and envelop incision. With better exposure, the implant will be placed more precisely. Every corner of remaining socket gap can be closed with bone graft. In case of flap approach, collagen membrane and PRF membrane should be used for GBR (guided bone regeneration). In contrast, membrane is not so critical for the flapless approach.
5. Bone graft is the 2nd most important factor in preventing peri implantitiis. It should be carried out in steps. For example, if a bone-level implant is placed deep, place the healing screw or a piece of gauze in the implant well and cover the exposed coronal implant threads until the implant platform with bone graft. Then remove the healing screw or the gauze, place an restorative abutment and place more bone graft until the margin of the abutment. Fabricate an immediate provisional. The latter is the most secure method to keep the graft in place, as compared to a healing abutment, periodontal dressing and flap/suturing (GBR). Effort is exerted to create an environment to deposit and form a layer of bone over the implant threads, not necessarily to reform the buccal or palatal plate.
6. No molar immediate implant is placed until smoke is reduced half a pack per day.
7. Oral antibiotic and Chlorhexidine rinse start 1-2 days preop and continue for 1 week postop. Use Water Pik when the wound heals.
If asymptomatic, exposed threads do not need treatment (bone graft). After bone graft, the covered threads may be re-exposed.
7.
Return to
Upper,
Lower Molar Immediate Implant
Xin Wei, DDS, PhD, MS 1st edition 06/26/2016, last revision 01/19/2018