




 |
 |
 |
 |
 |
 |
 |
 |
 |
 |
 |
 |
 |
Where Does Post-Implant Infection Arise?
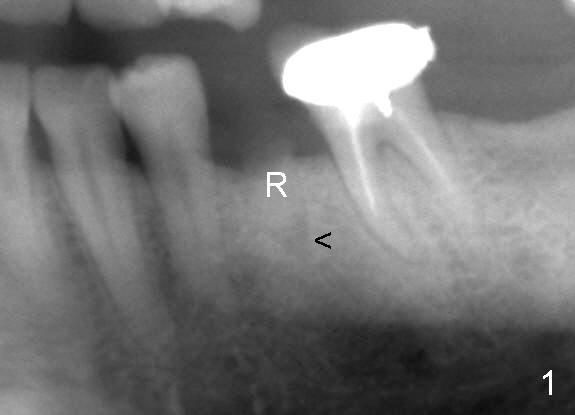
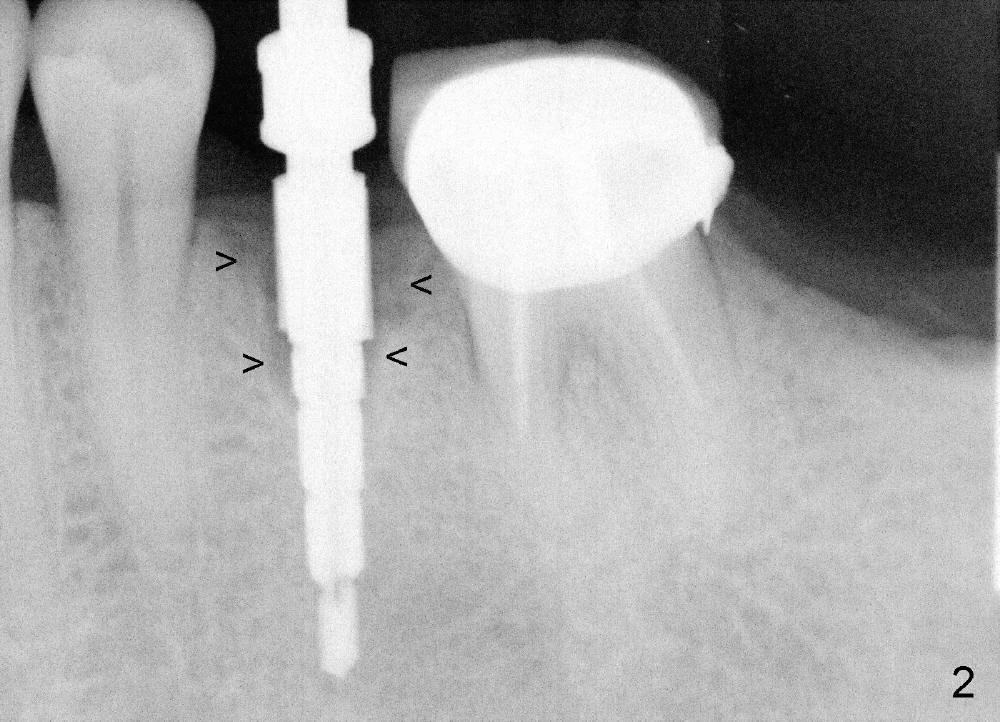
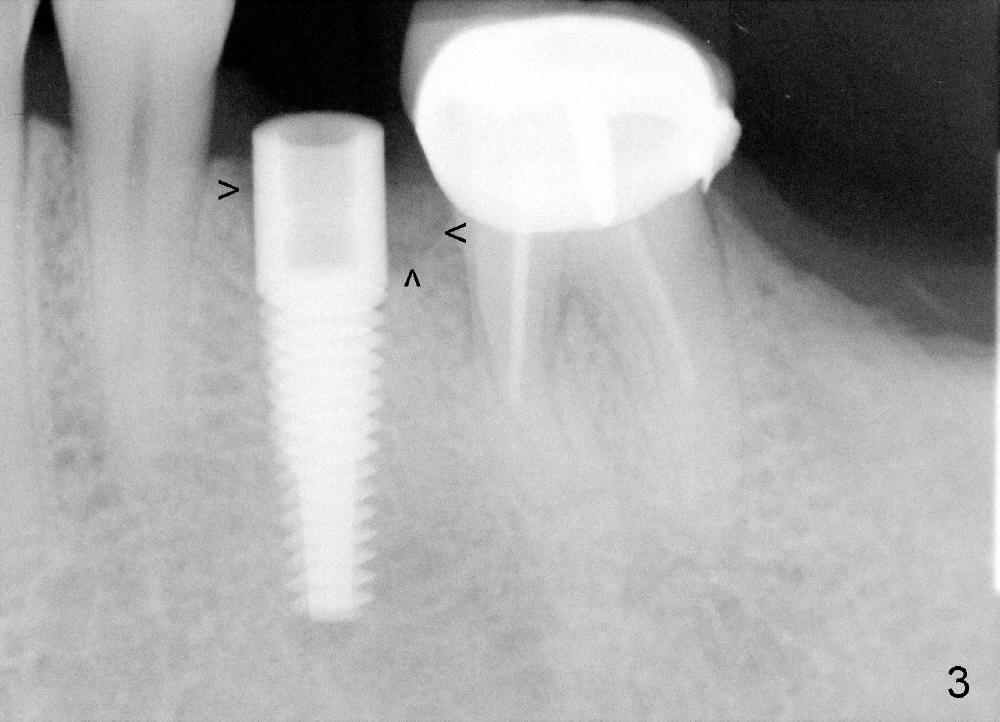
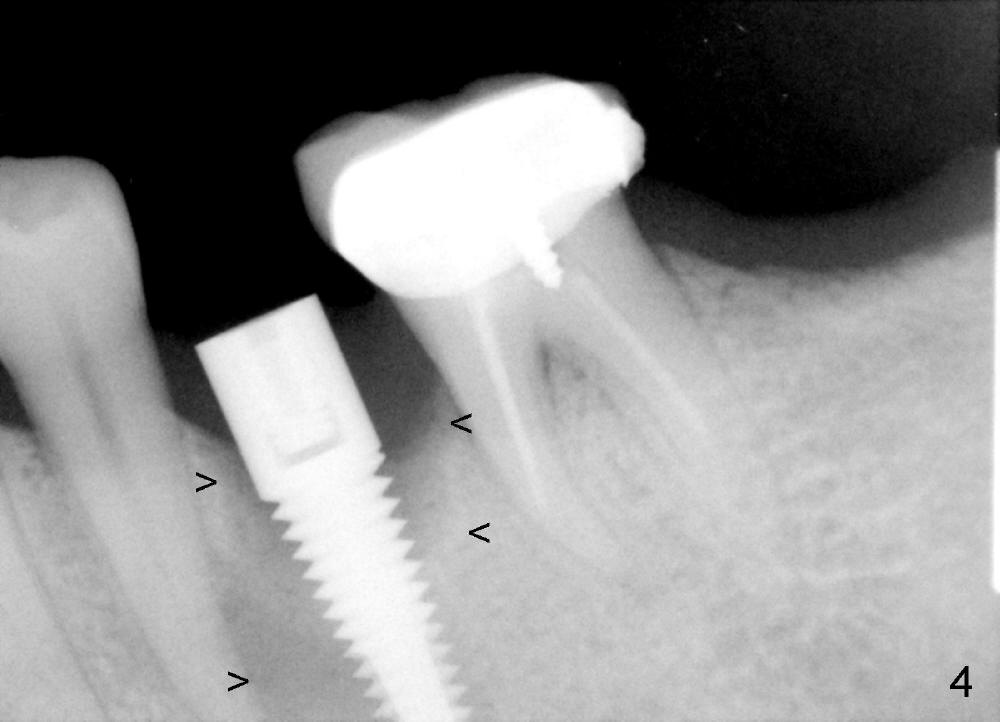
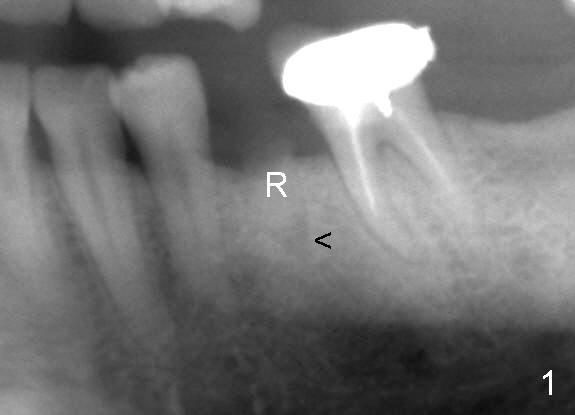
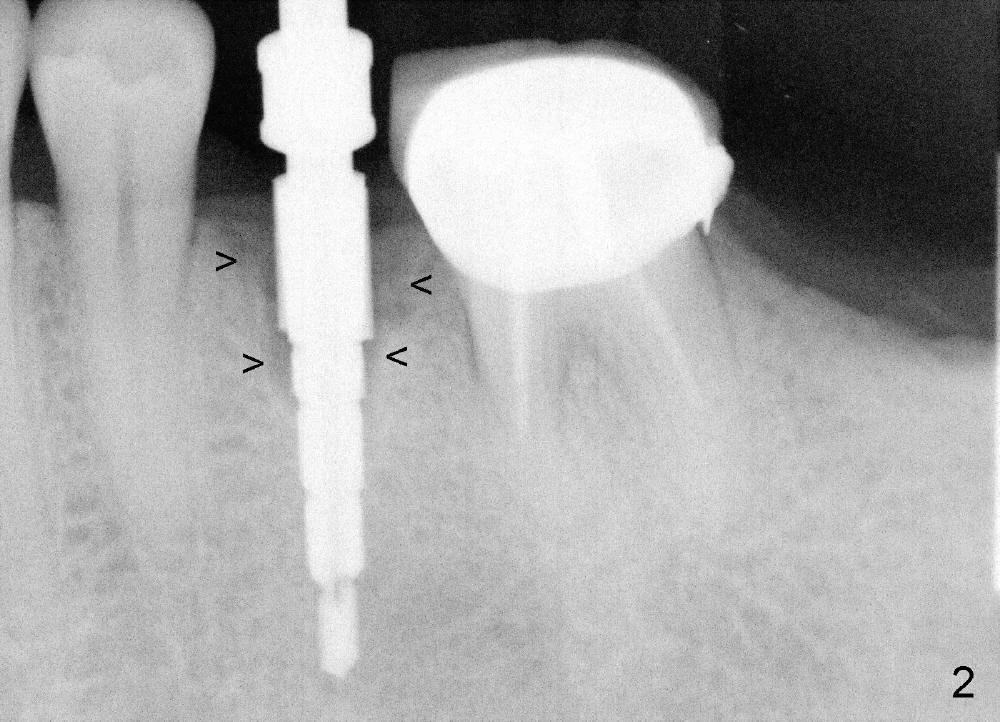
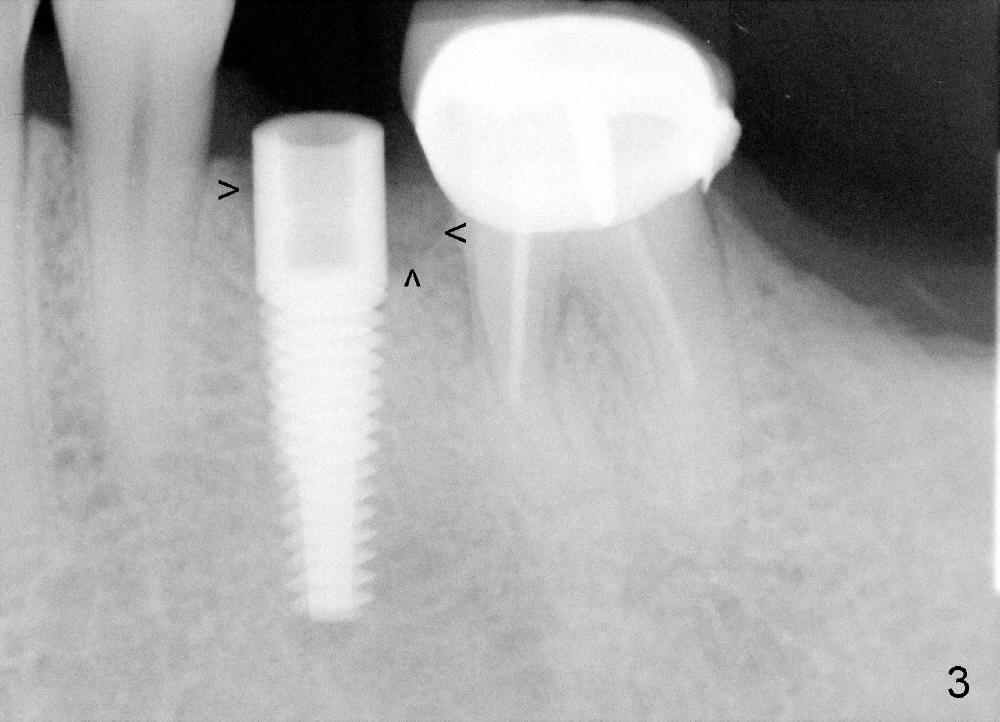
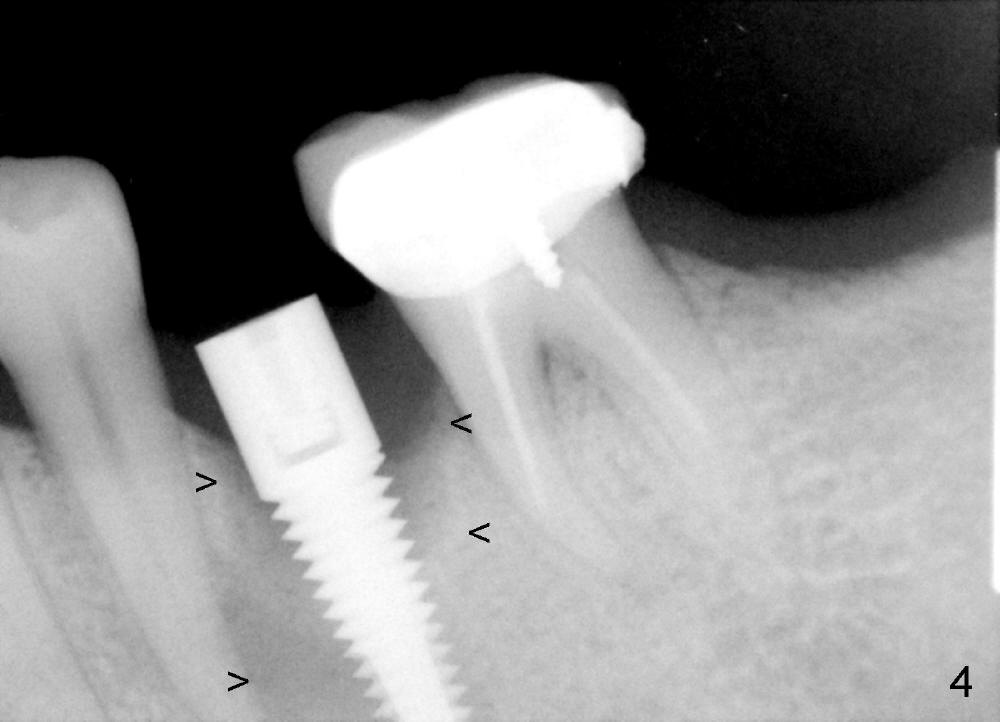
A 44-year-old lady has poor dentition. The tooth #20 has a residual root (Fig.1 R). Immediately after extraction, osteotomy is formed by drills (Fig.2: 3.5x17 mm); a 4.5x17 mm implant is placed (Fig.3 (arrowheads: boundary of the socket)). The patient returns 9 months later with increased radiolucency around the implant (Fig.4) and buccal swelling (Fig.5, asymptomatic). Raising the buccal flap confirms bone loss around the implant (Fig.6). Following debridement, allograft is placed. The source of the infection is unknown.
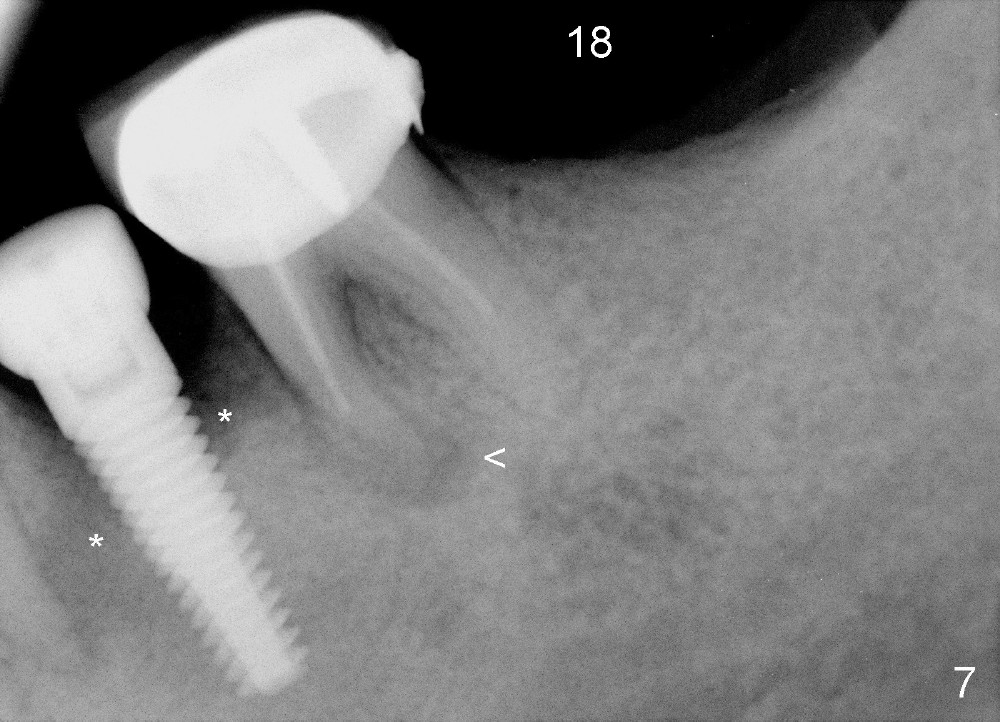
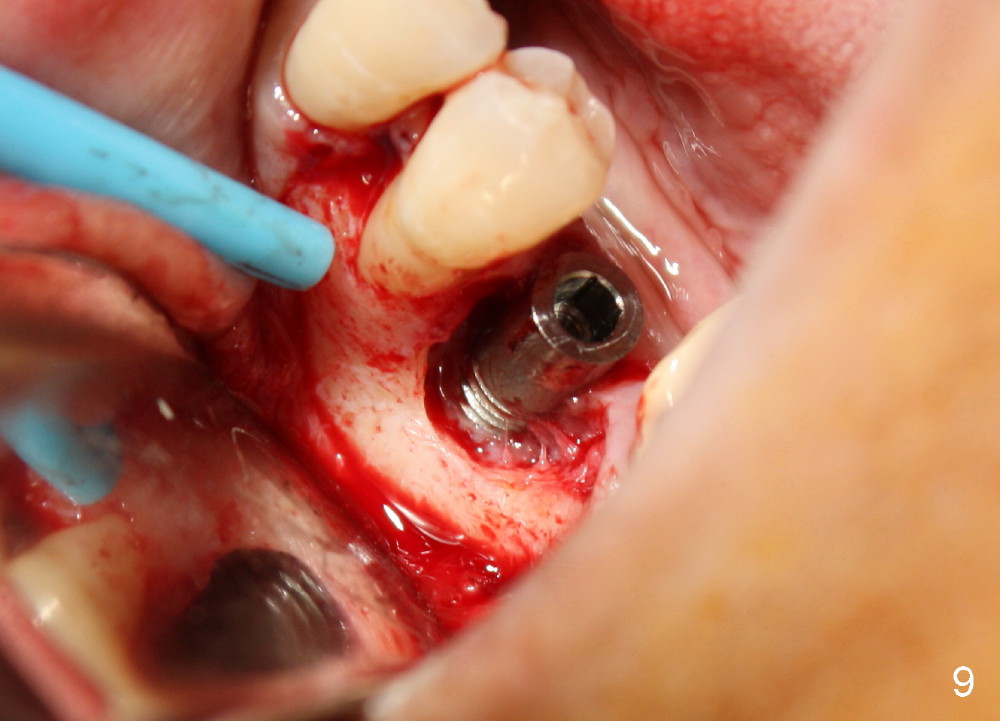
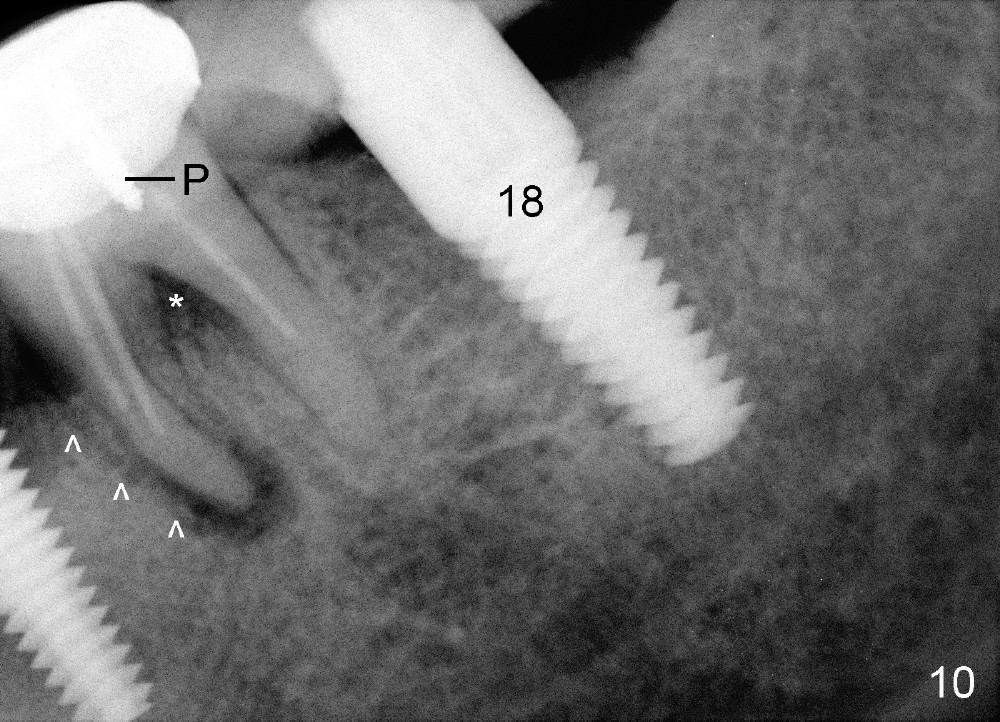
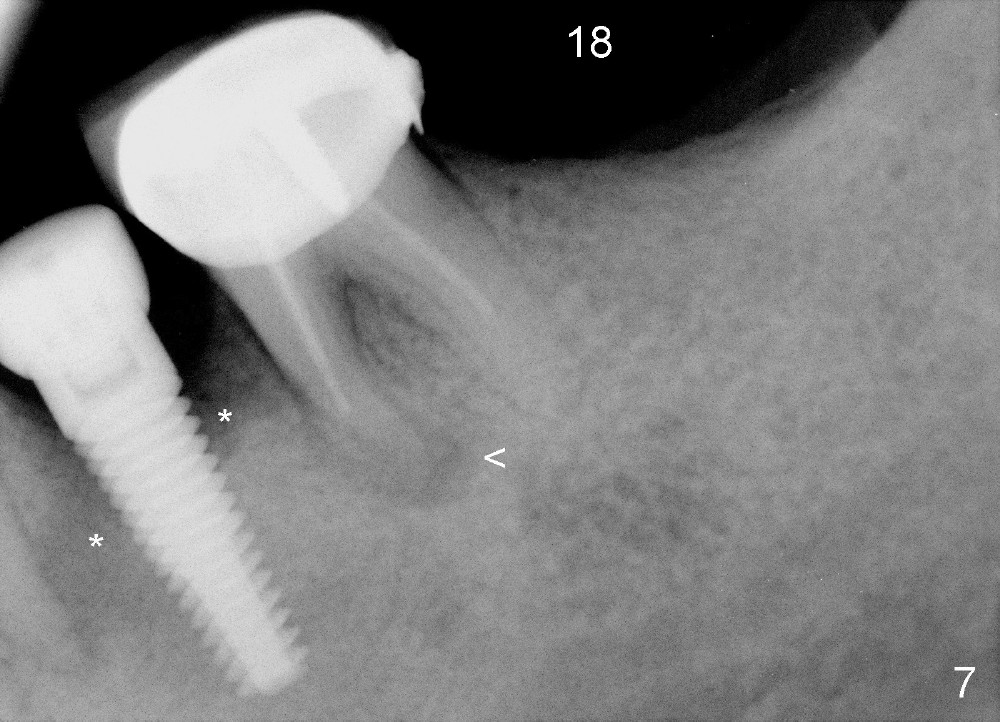
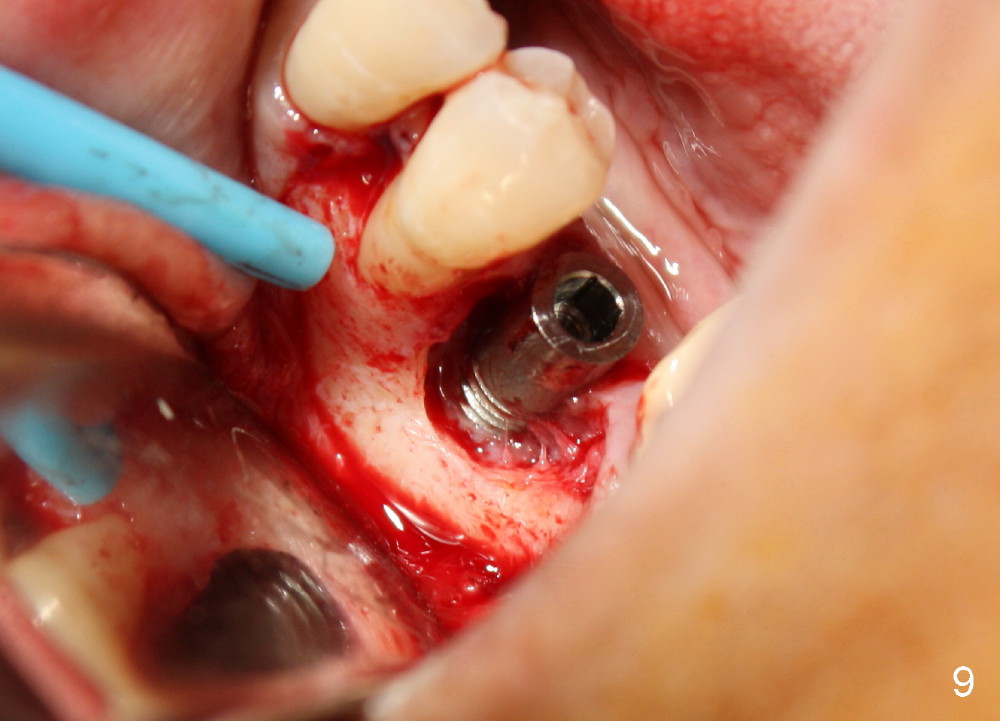
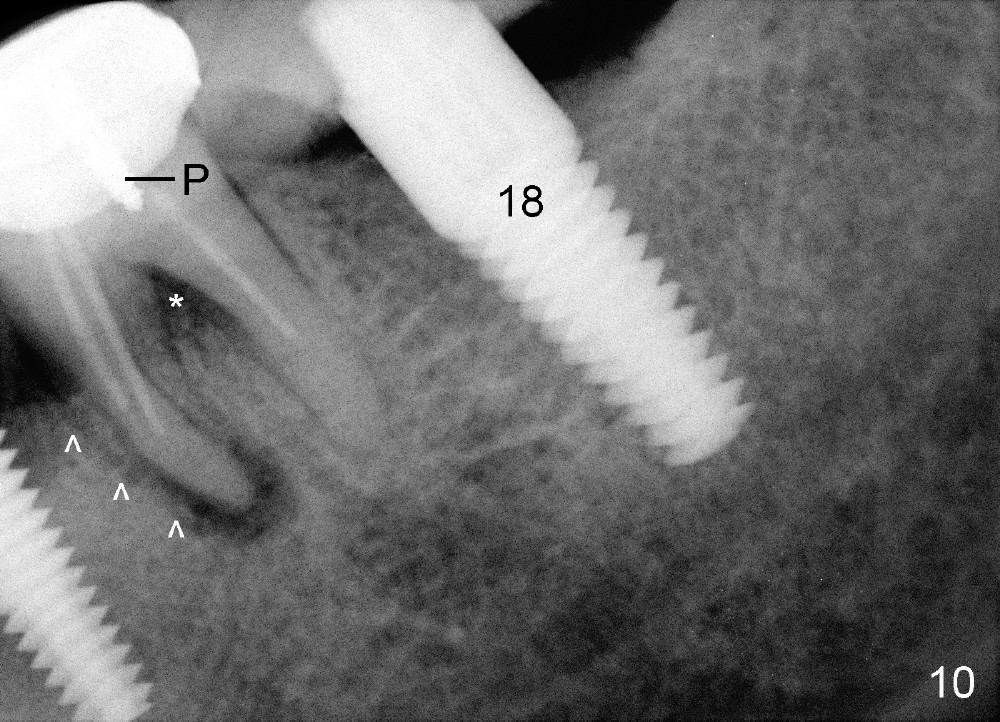
Four and a half months later, an implant is planned for #18 (Fig.7). The preop PA reveals that there is no bone growth around the implant at the site of #20, although the buccal swelling appears less prominent (Fig.8) than before (Fig.5). Without too much thinking, flap is raised for debridement (Fig.9). Autogenous bone graft is harvested from the site of #18 and placed in the defect area. By the time the surgery is done, the possible source becomes obvious: the periapical infection of the mesial root of #19 (Fig.10 arrowheads from primary infection to secondary one). Since there is also a furca lesion, possibly related to the post (P), the tooth has guarded to poor prognosis.
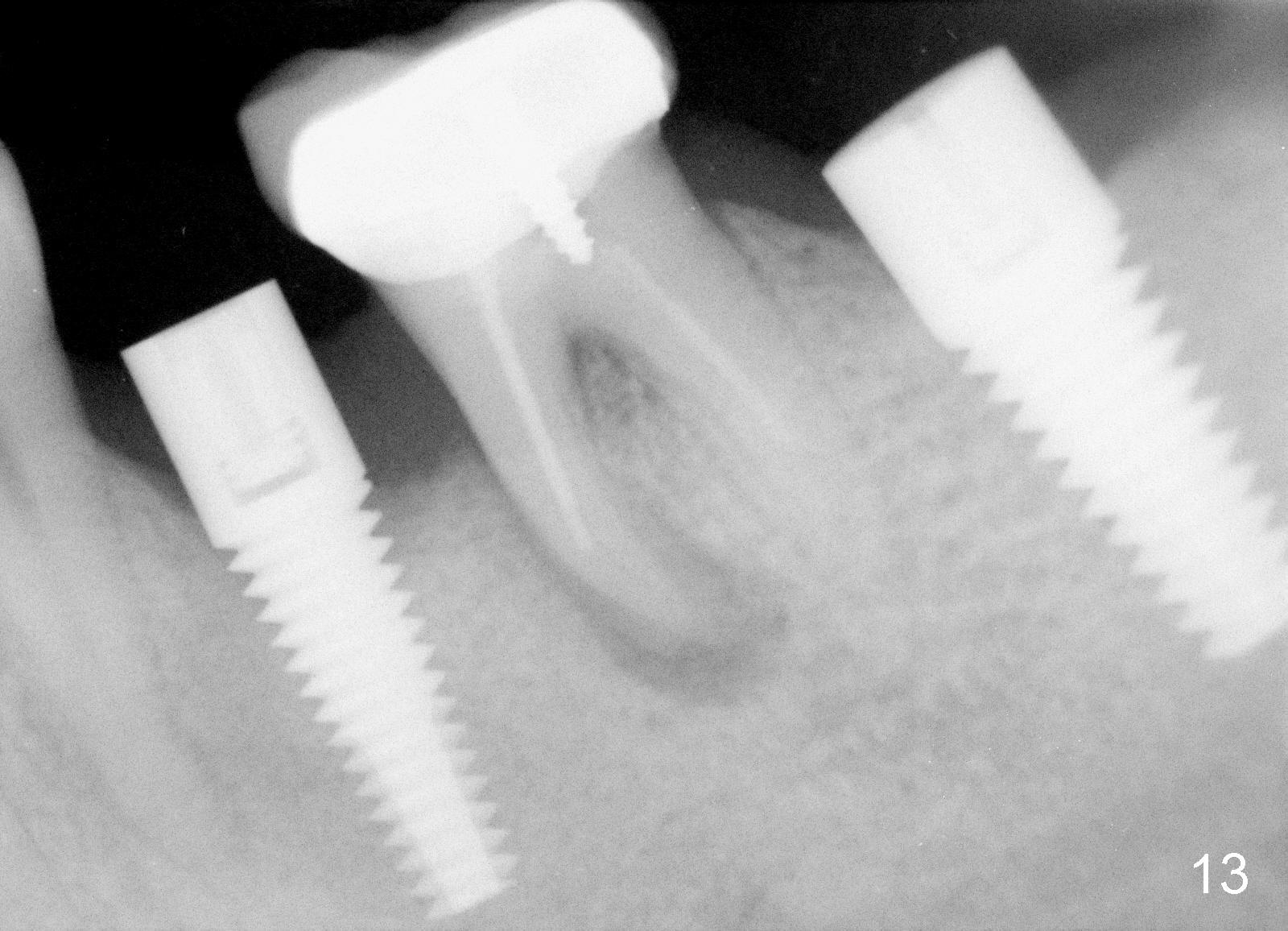
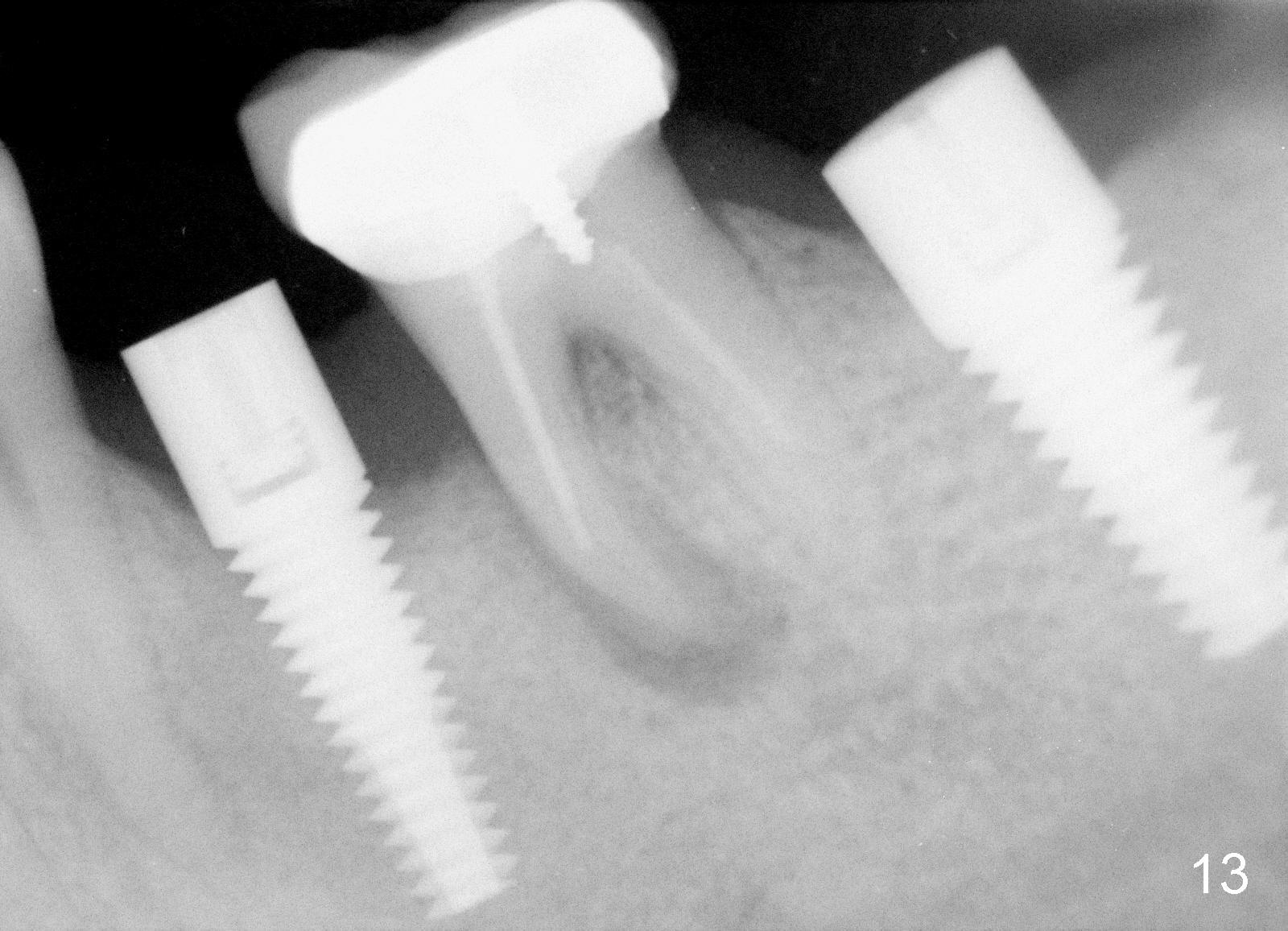
Twelve days post 2nd debridement, the wound does not heal normally. Out of desperation, Arestin is placed incompletely in the mesiobuccal pocket of #19. Fortunately, the wound heals at the site of #20 one month later (Fig.11). No infection is observed 4 months post 2nd debridement (Fig.12,13). Eventually the tooth #19 becomes symptomatic. Extraction and immediate implant is planned. In case the implant at the site of #20 fails, a cantilever bridge is fabricated using the posterior 2 implants.
Return to Implant Placed
Next to
Infection Site or Not,
Lower Bicuspid Immediate Implant
Bone Graft
Xin Wei, DDS, PhD, MS 1st edition 09/25/2014, last revision 04/19/2015