

.jpg)
 |
 |
 |
|
 |
 |
 |
 |
 |
 |
 |
|
 |
.jpg) |
||
Internal Sinus Lift of 1 mm Bone (M)
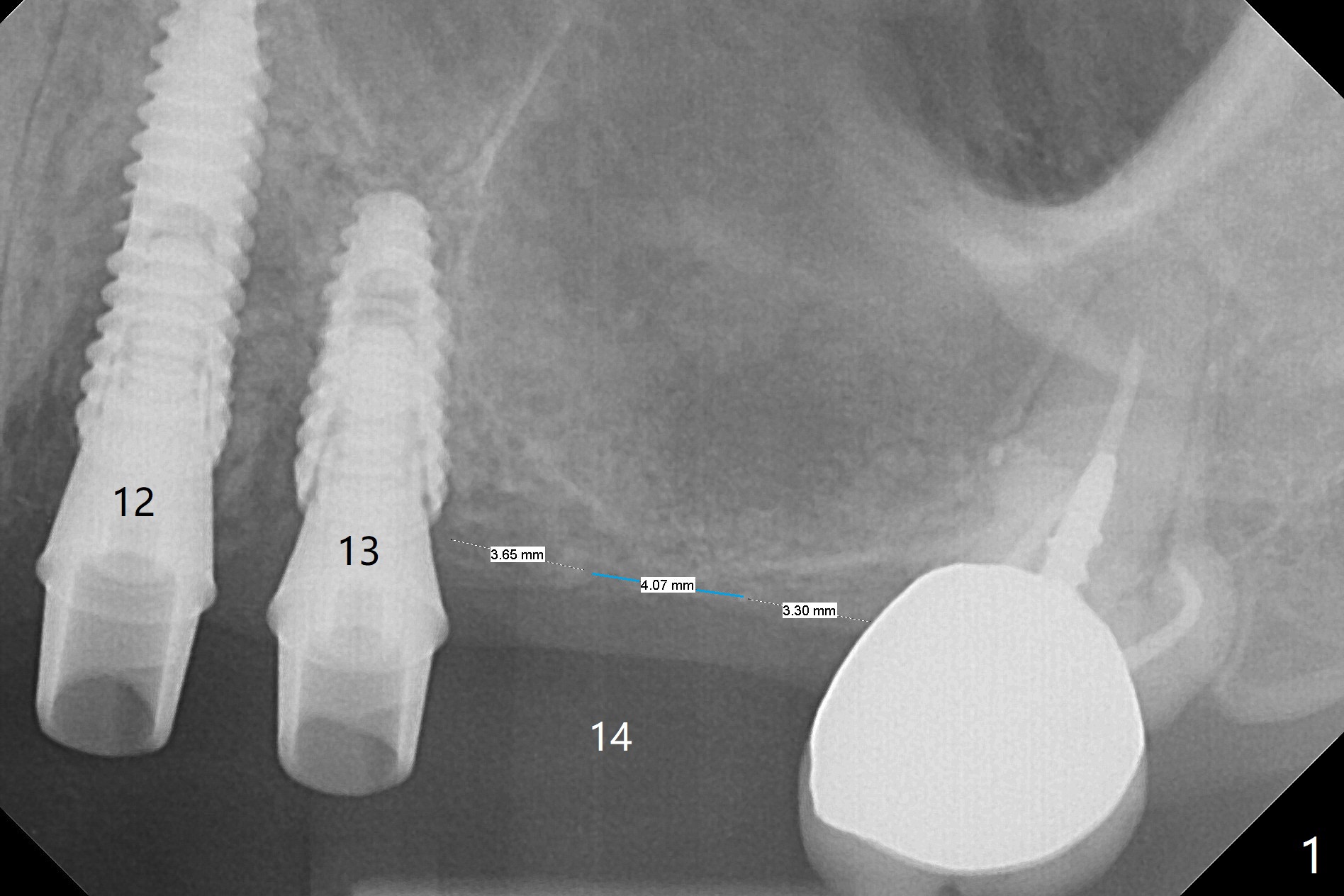
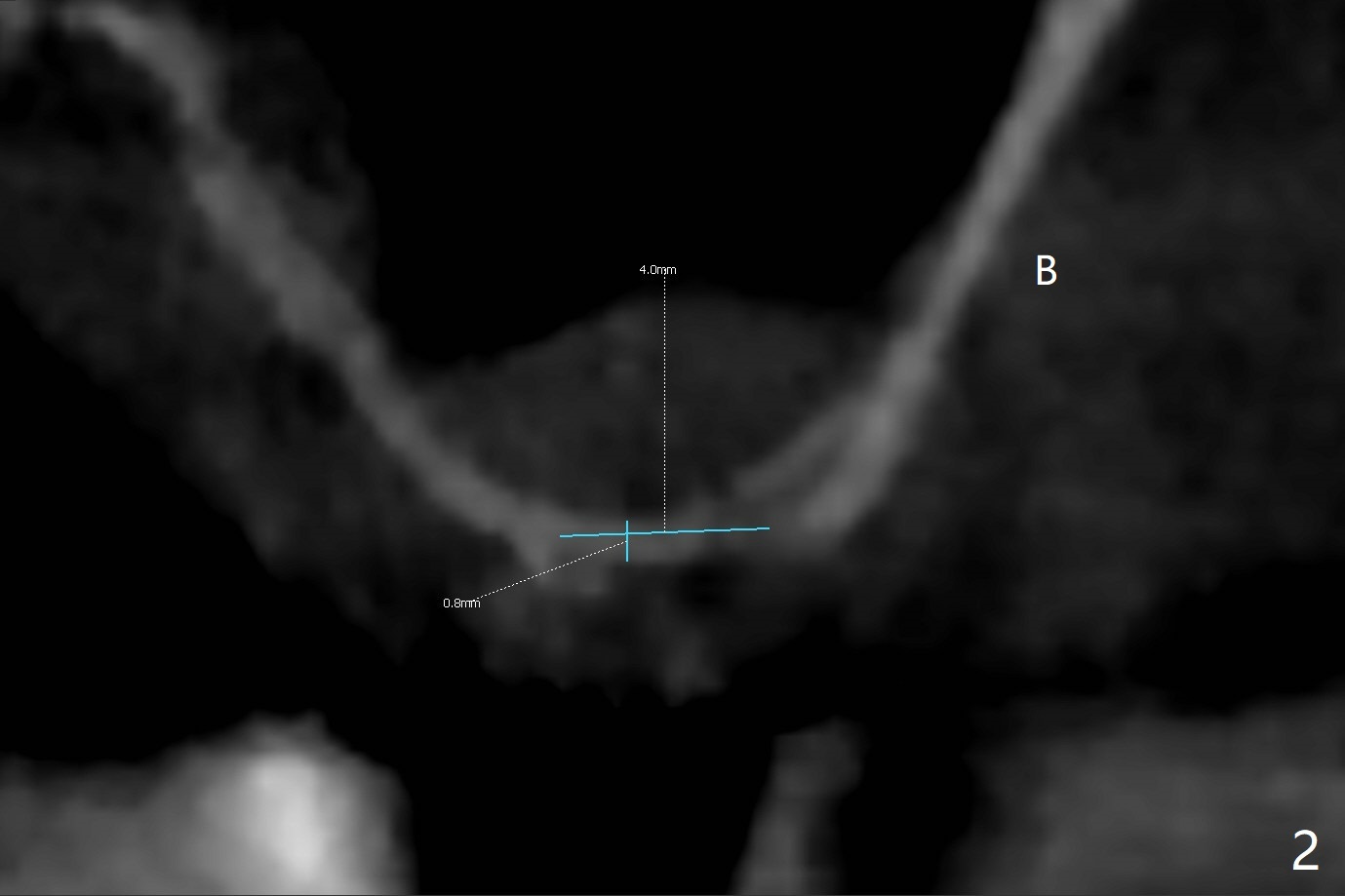
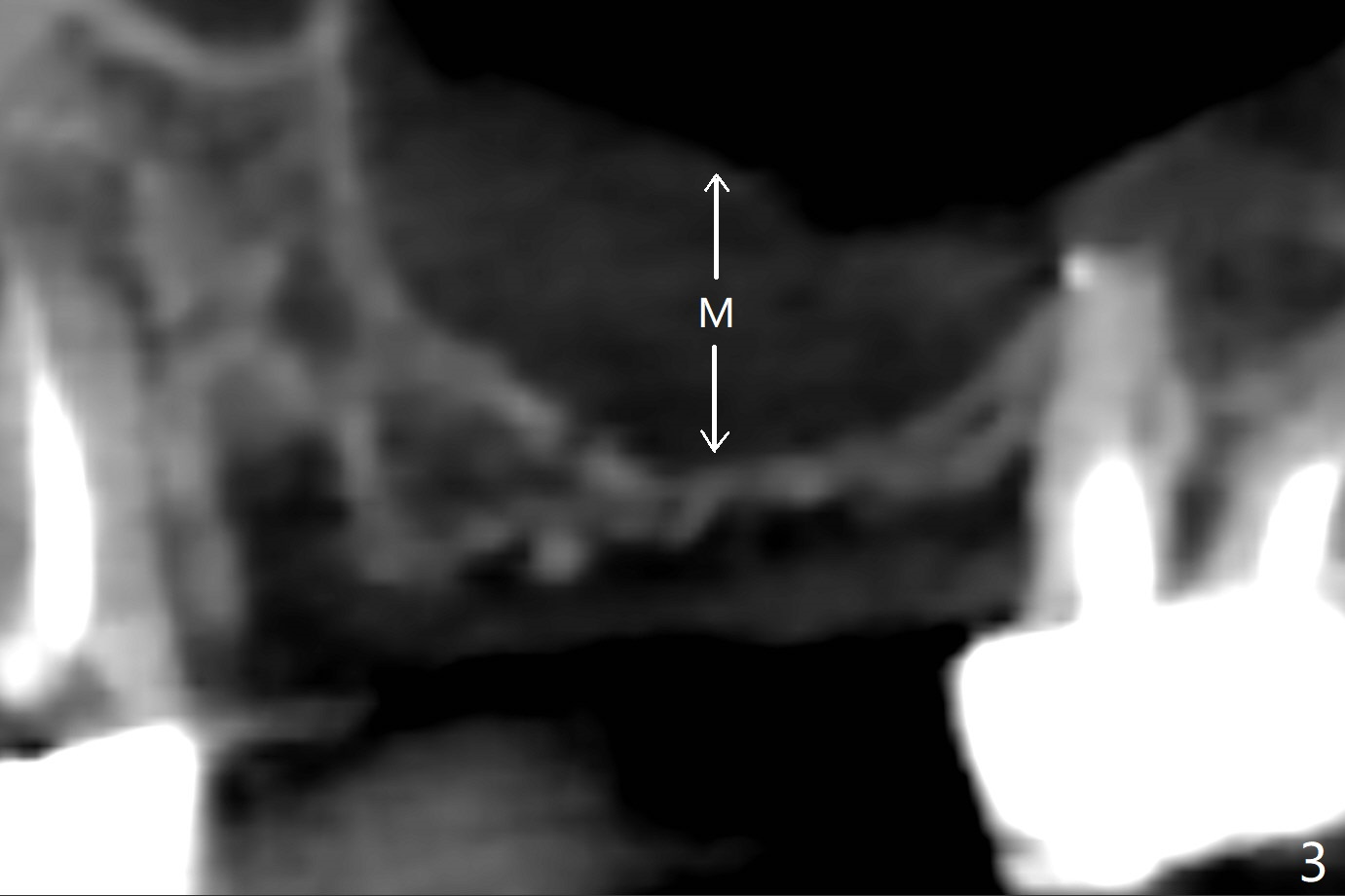
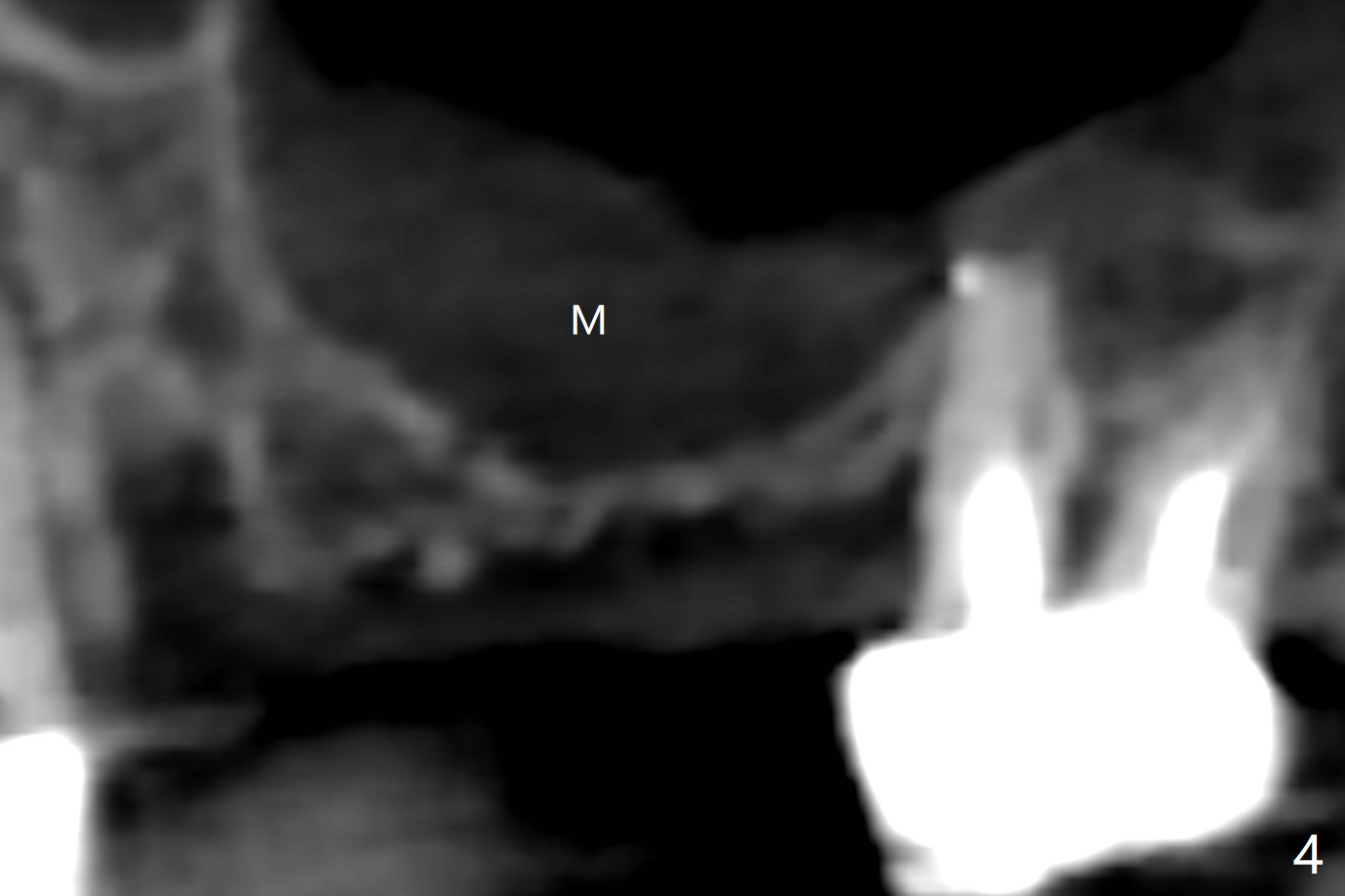
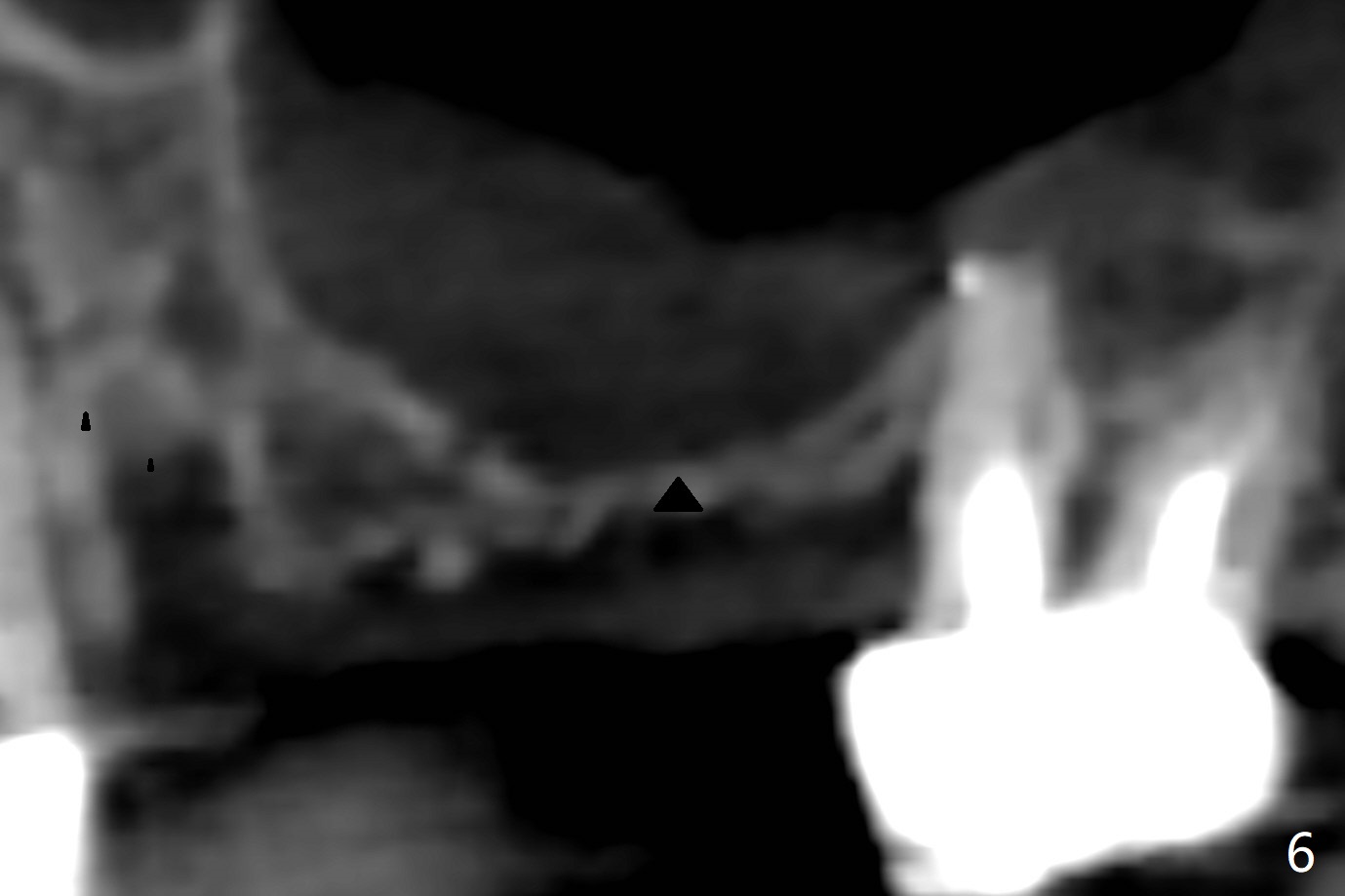
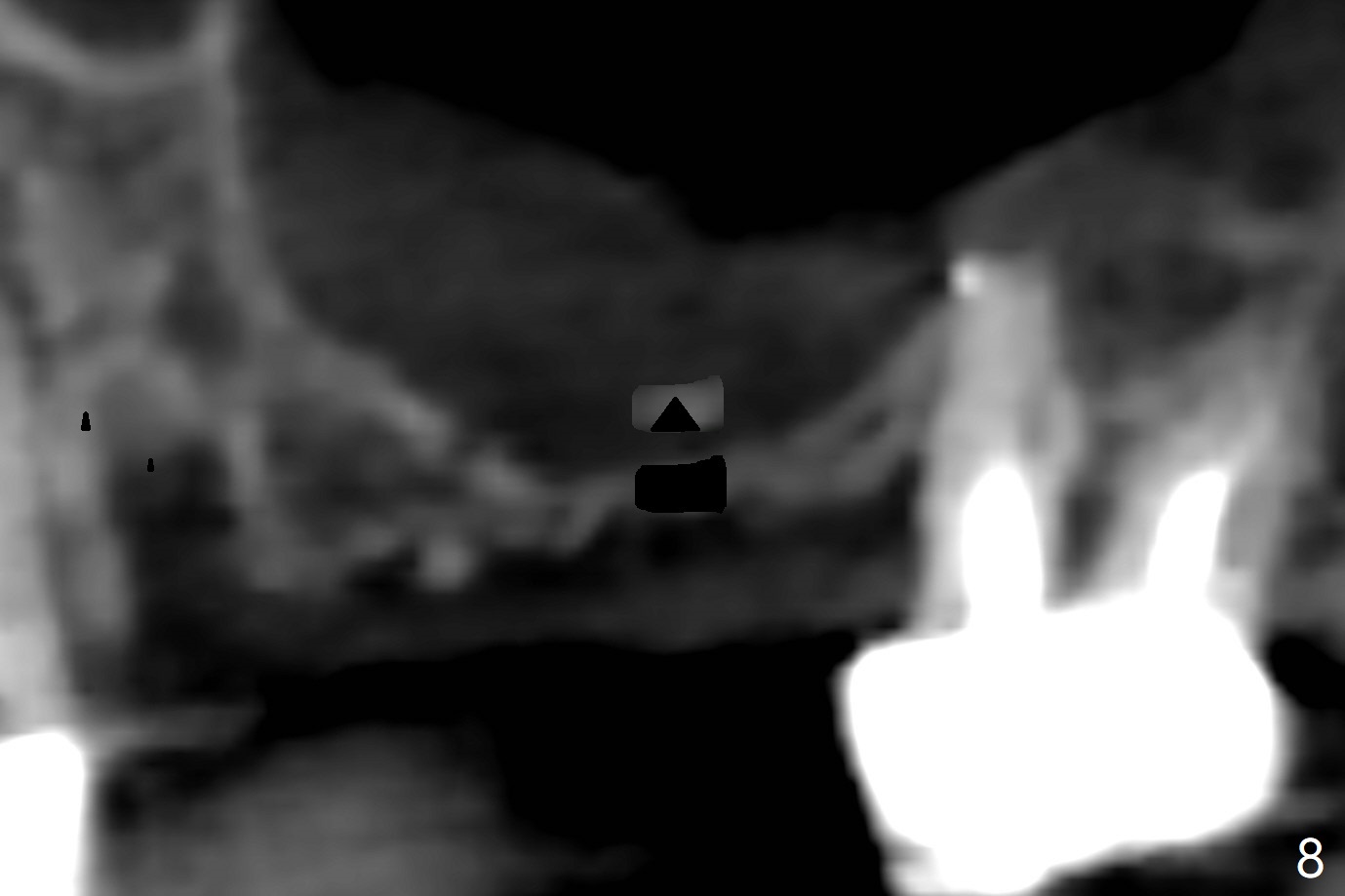
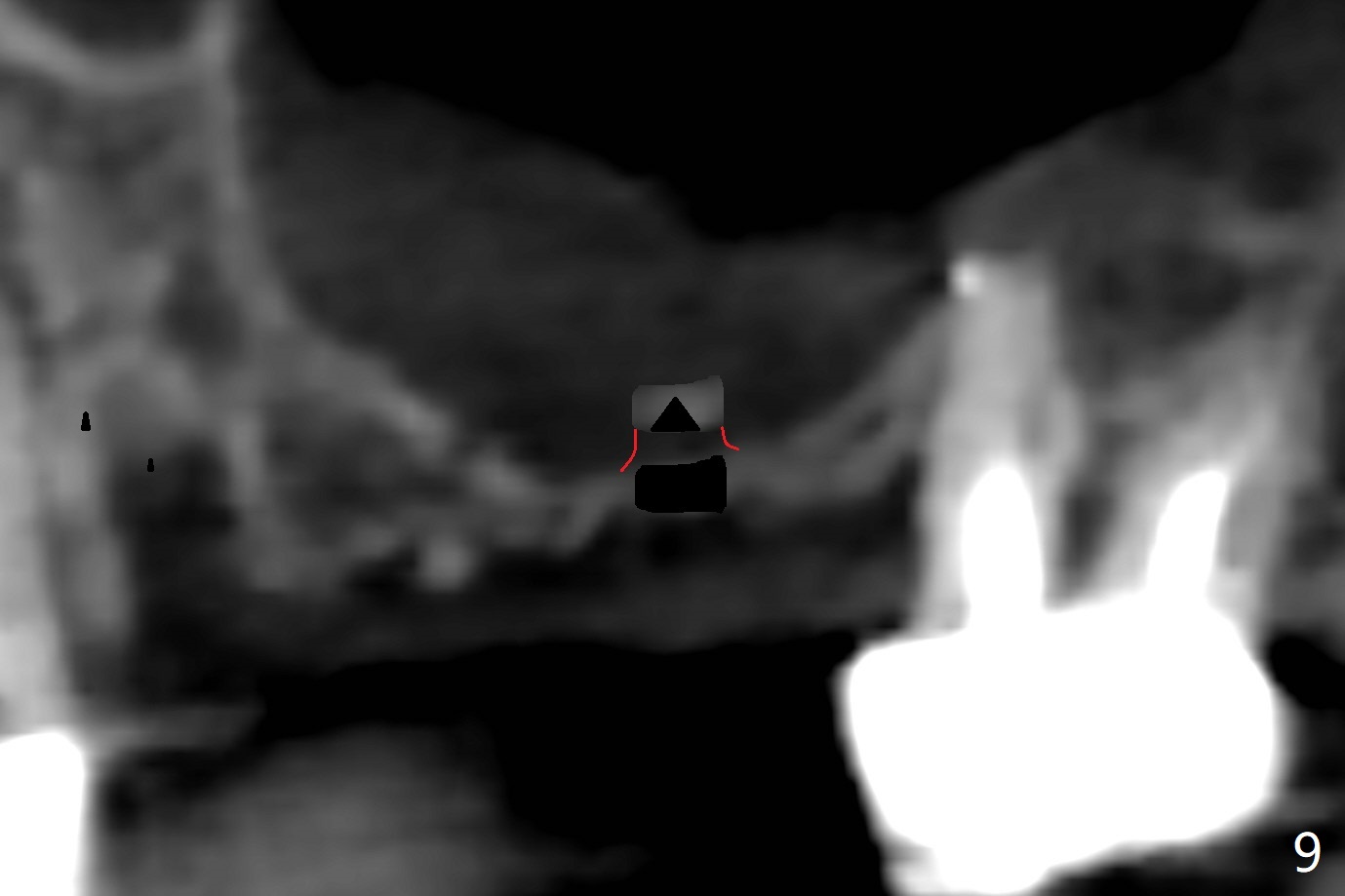
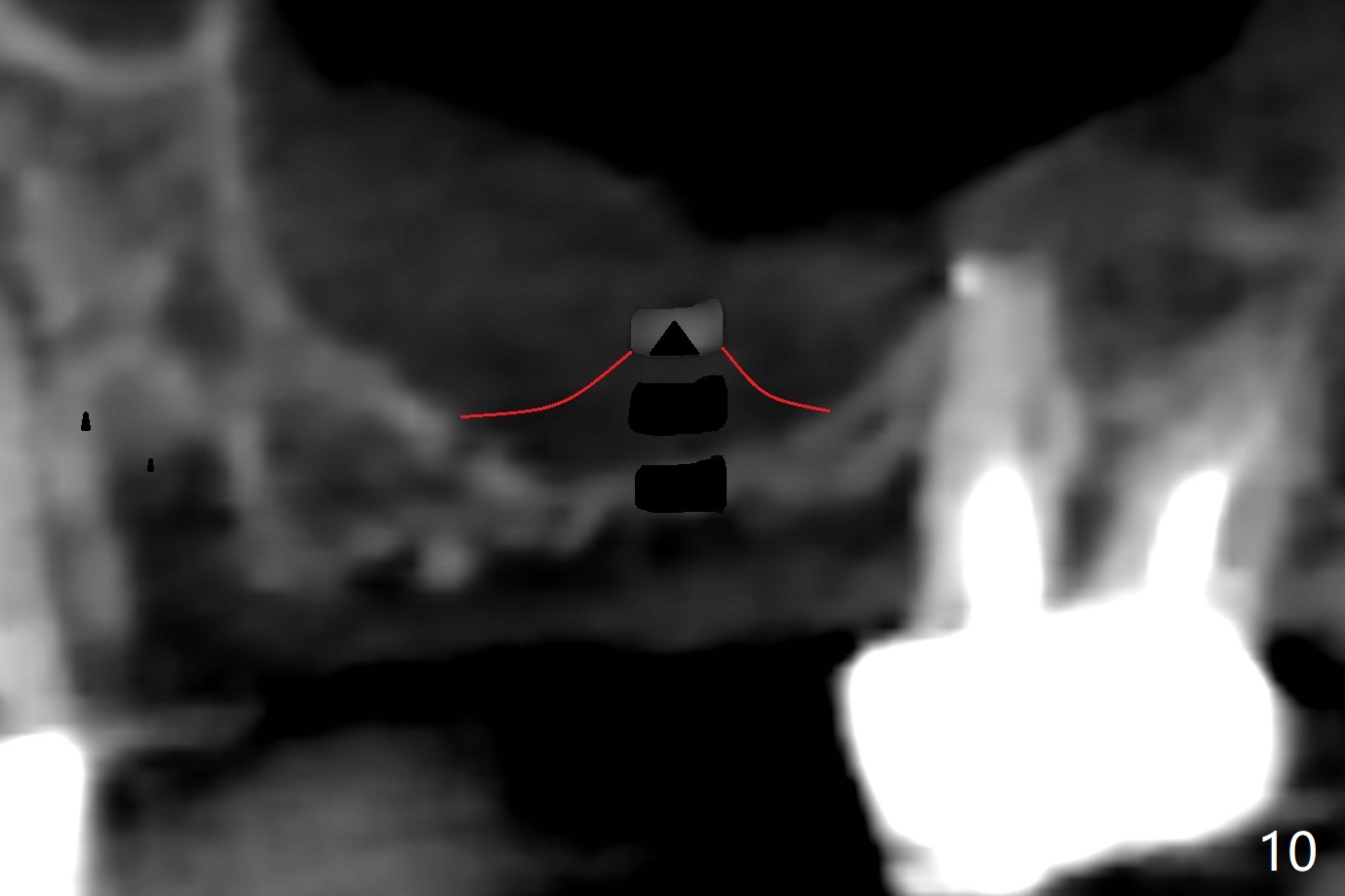
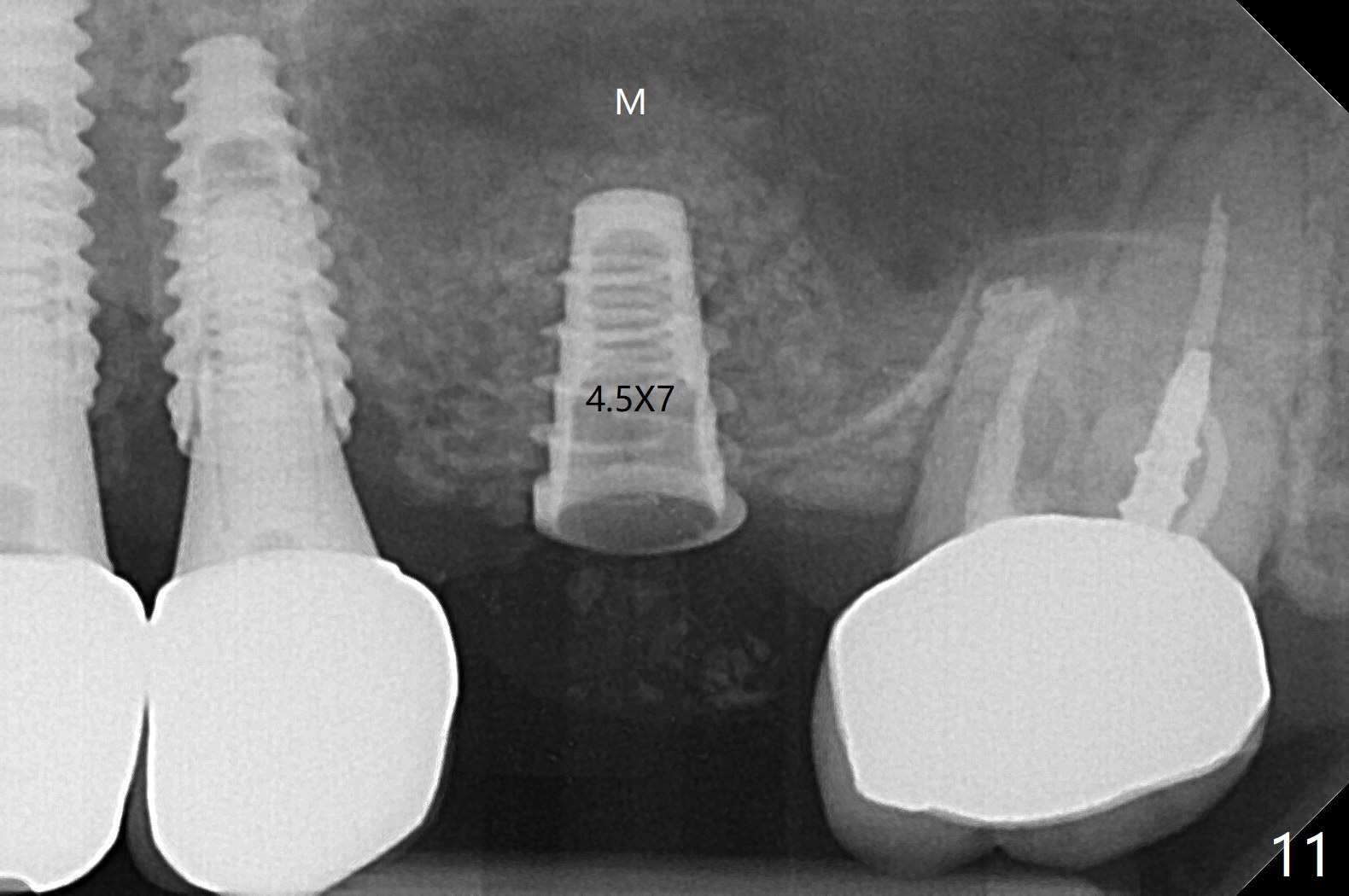
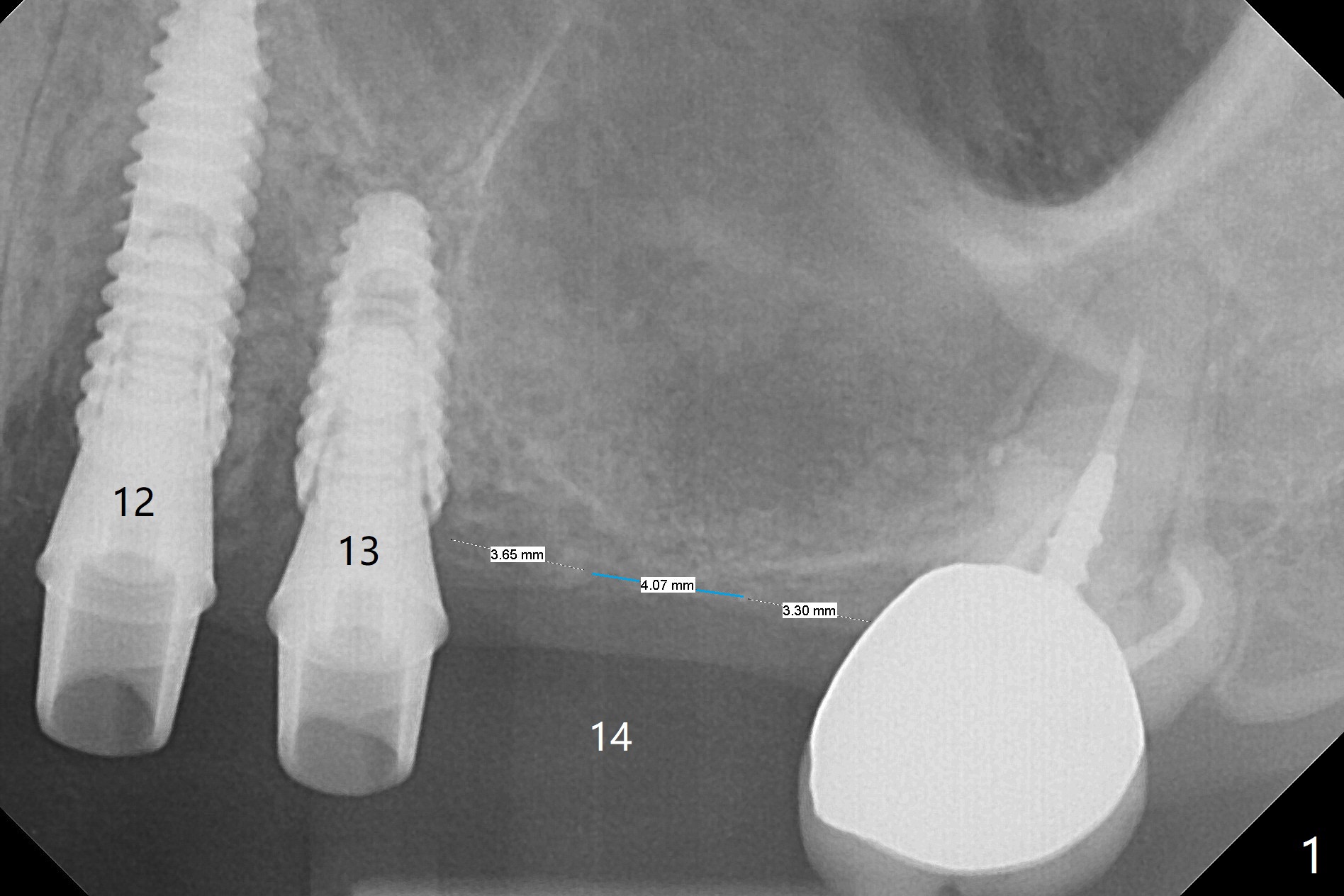
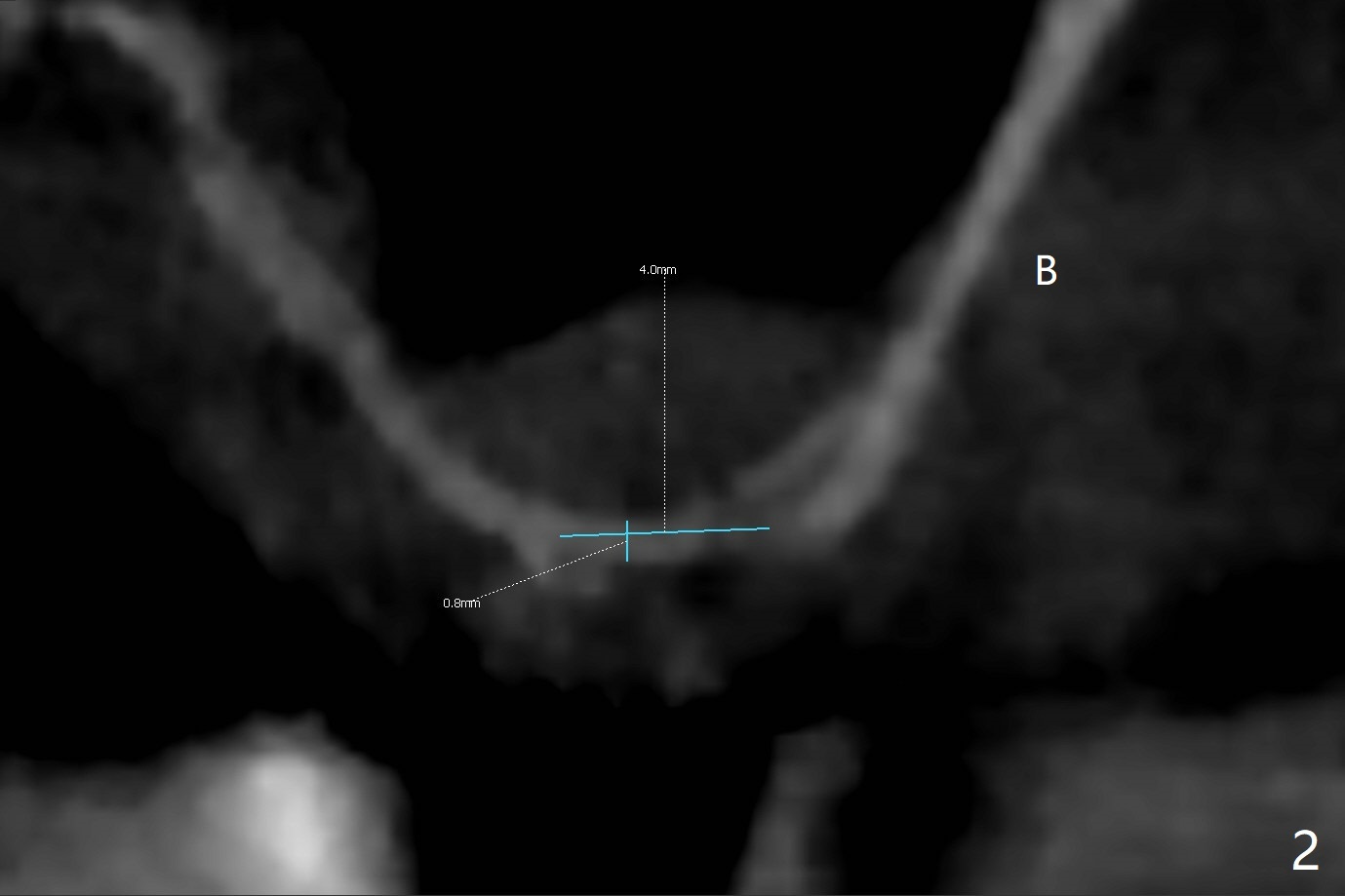
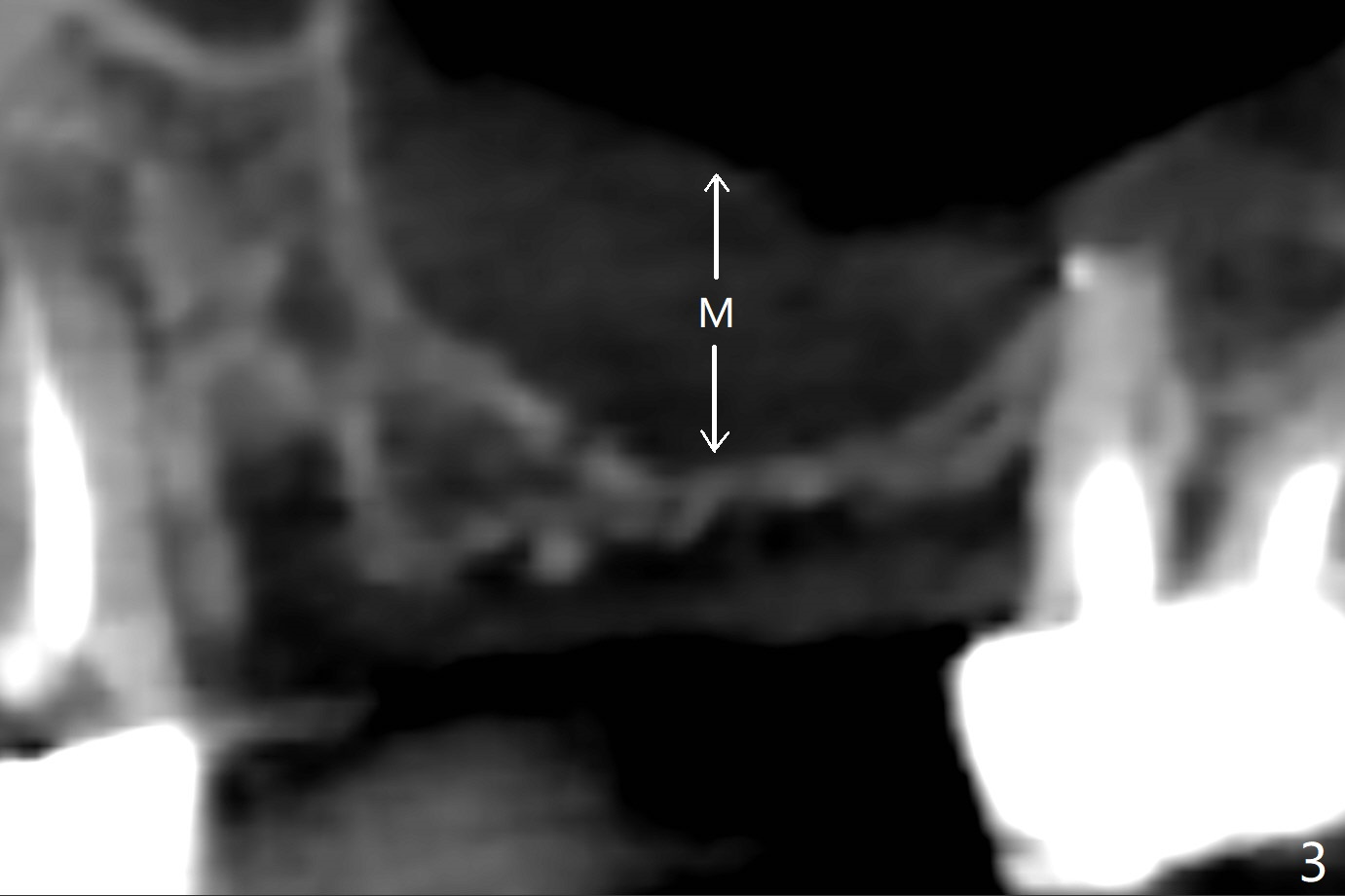
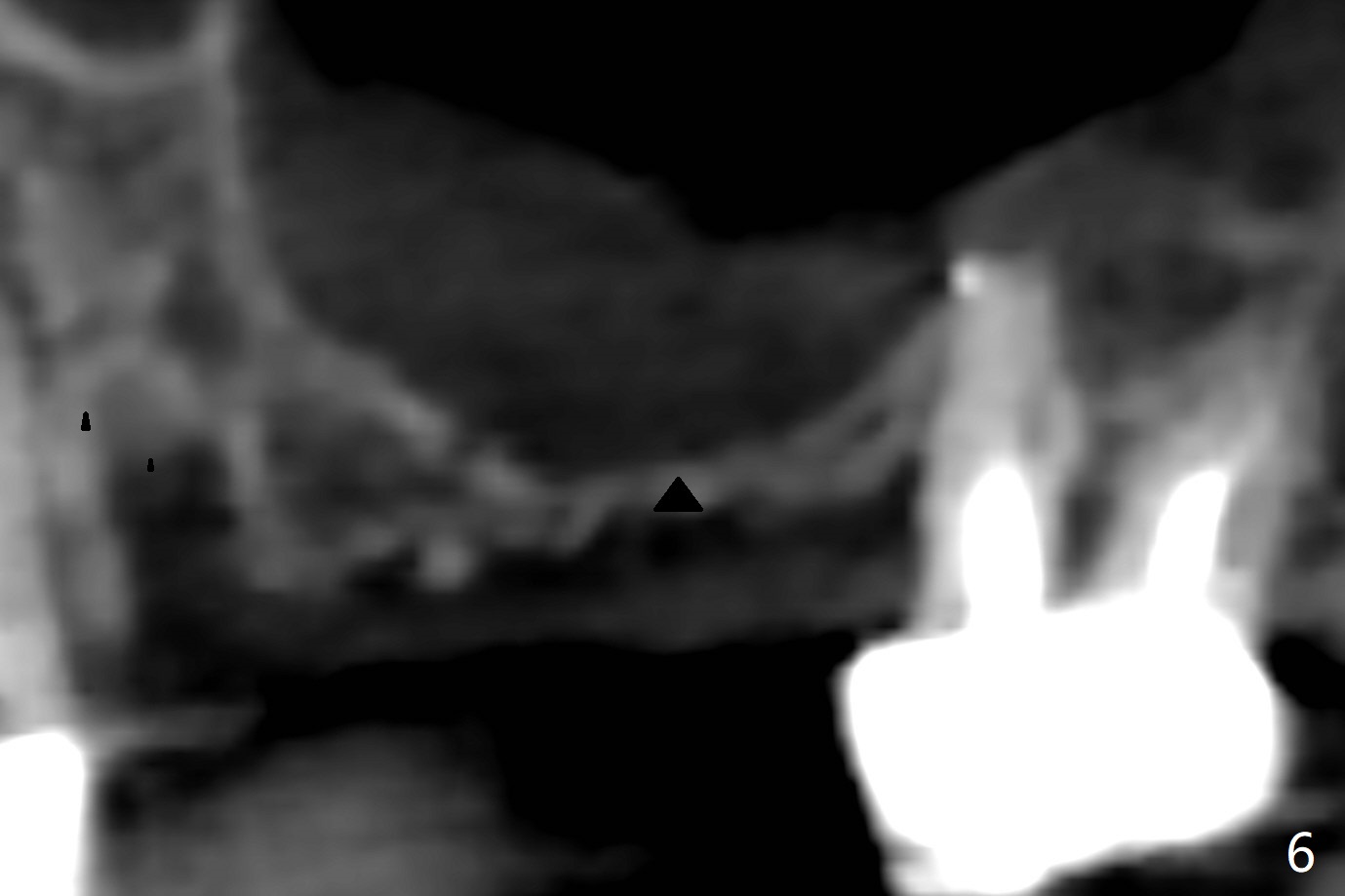
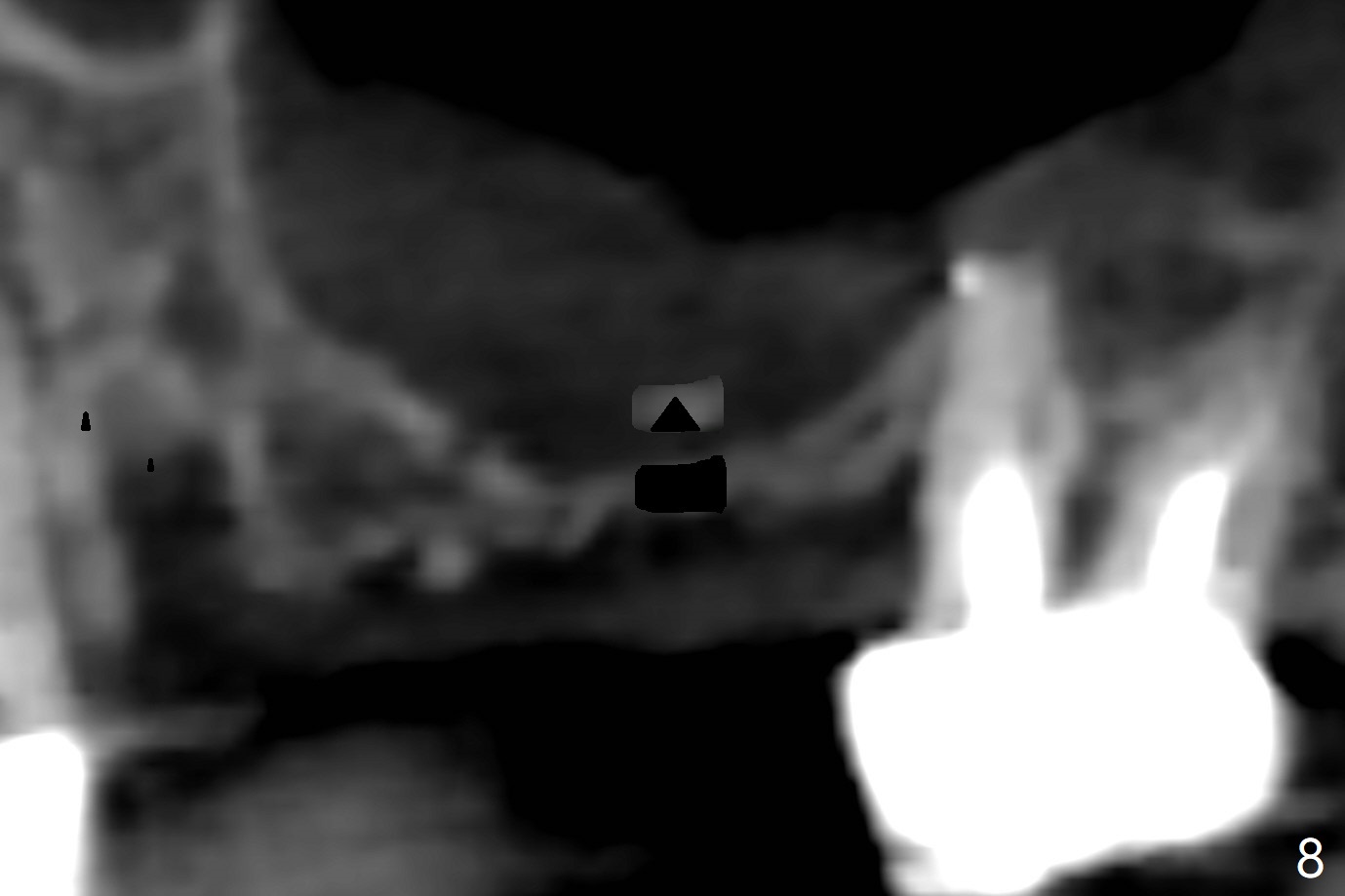
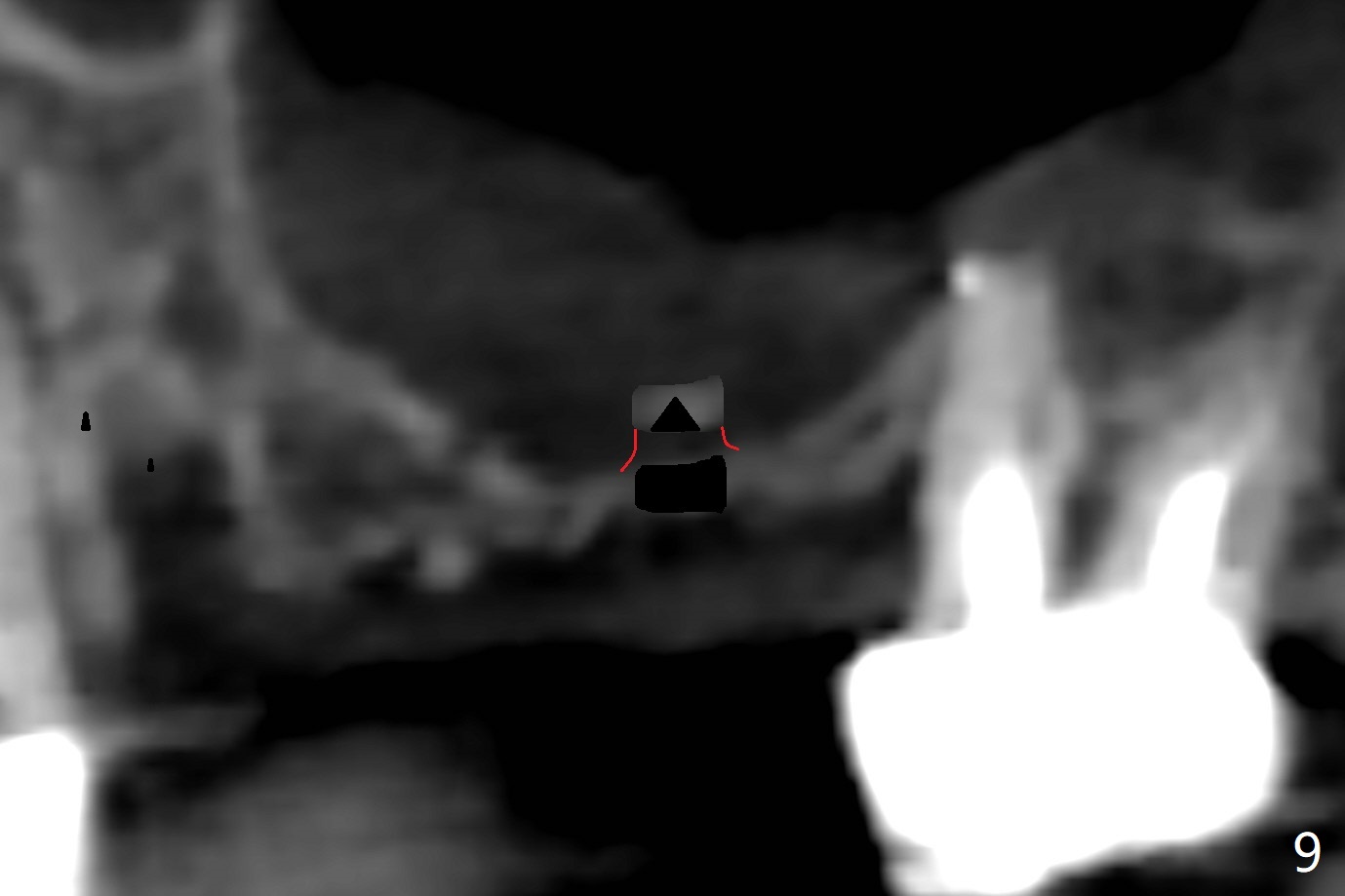
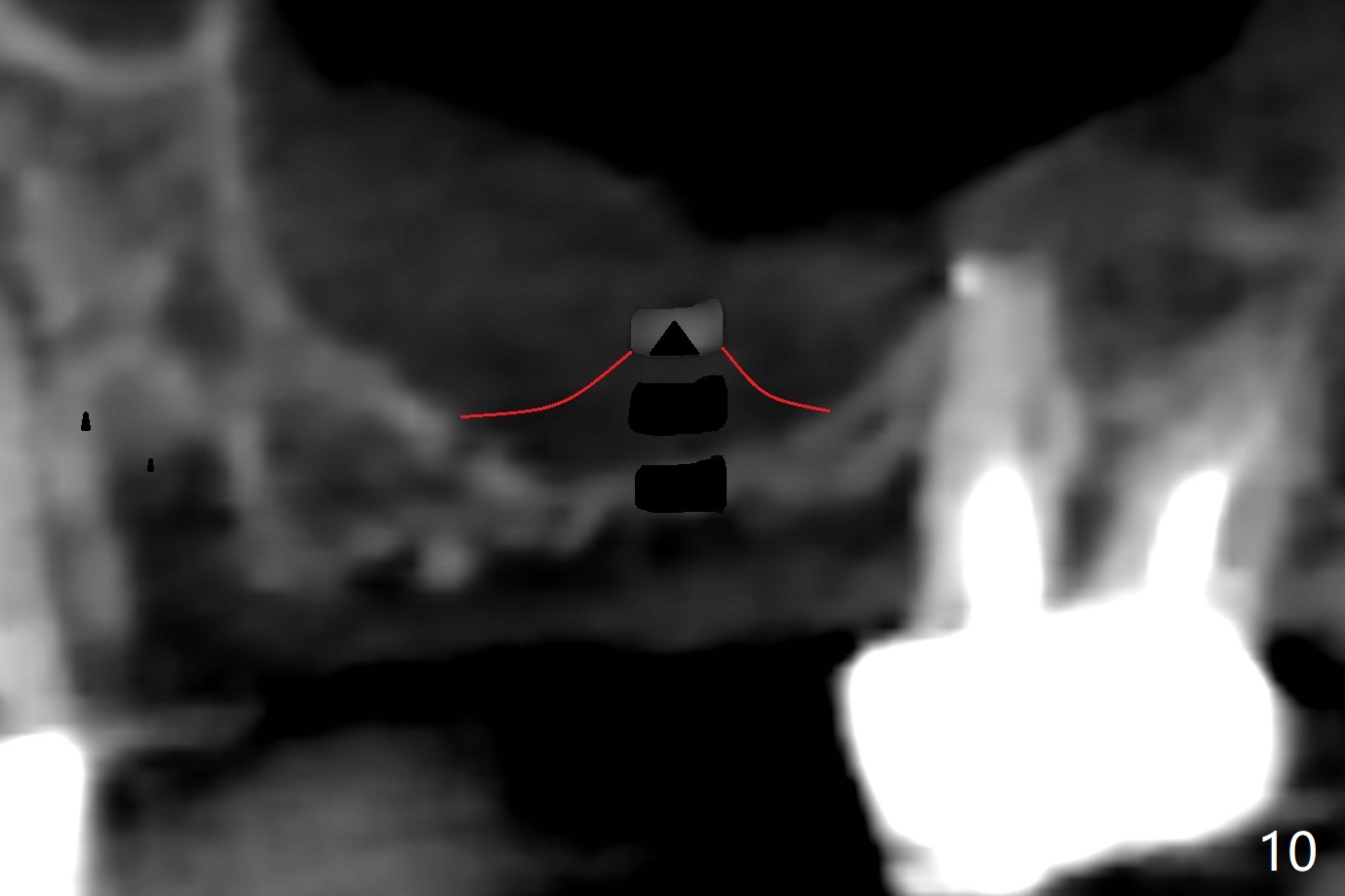
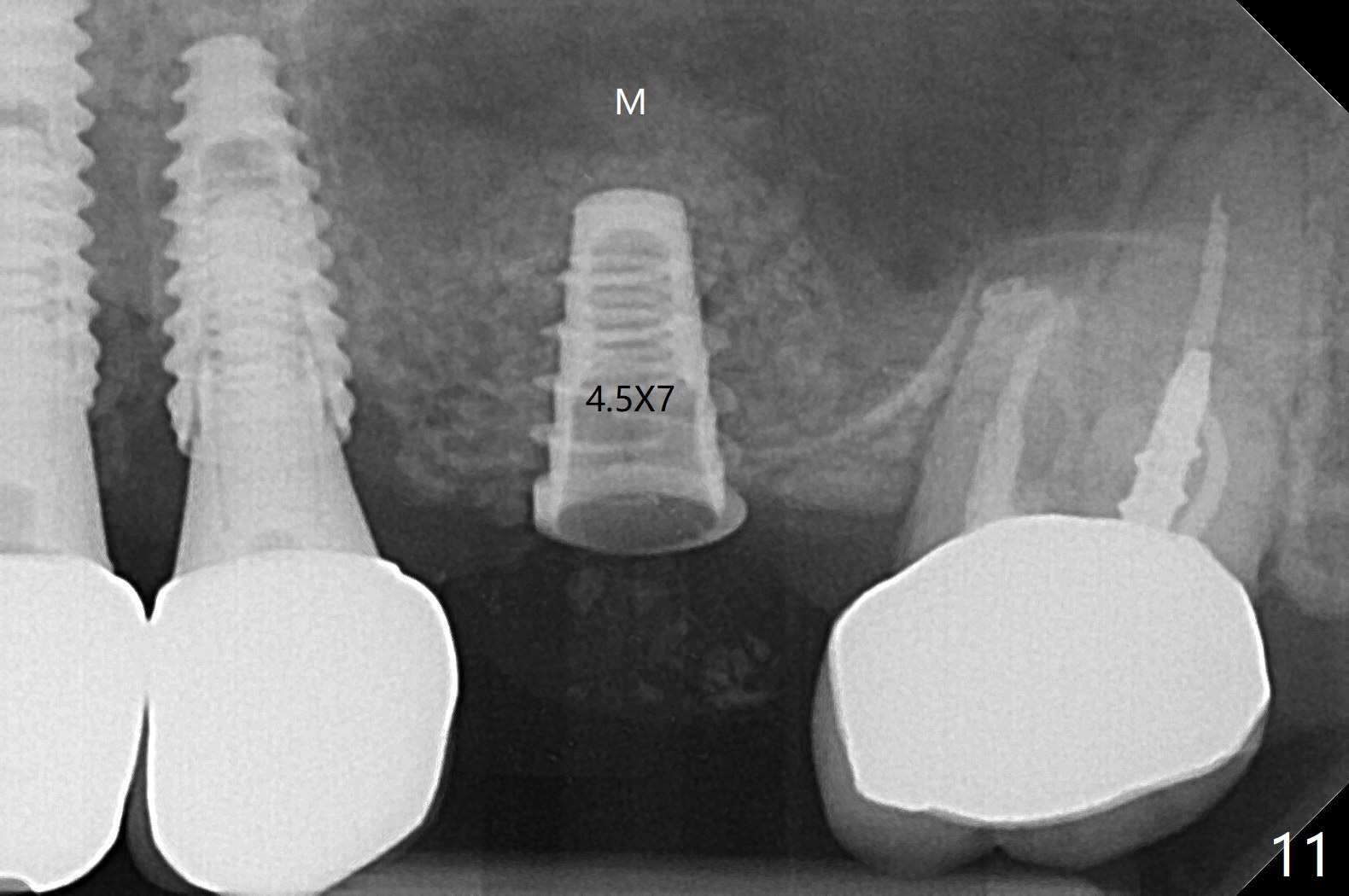
A 68-year-old timid woman is considering implant at #14 twenty months post cementation of #13 and 14 crown (Fig.1). Because of the narrow buccopalatal width (Fig.2 CT coronal section, B: buccal), a 4 mm implant (blue line) seems to be appropriate for the site (Fig.1). After crestal incision and flap reflection, a diamond round bur is used to thin the sinus floor until the bluish membrane is barely visible. An osteotome (Magic Sinus Lifter) is used for penetration. Water lift will be conducted if necessary, considering the already thickened sinus membrane (Fig.3 (CT sagittal section) M). Insert the first PRF membrane, followed by bone graft (not too sticky) repeatedly. Use sensor 1 to confirm lift degree. Try a 4x7 mm dummy FC to test stability. Place a definitive one (probably Magicore) if indicated. Use a second PRF membrane before closure of the wound. After nearly 15 month consideration (including coronovirus), the patient decides to get it done. With incision (Fig.4) and Marking Drill (Fig.5, the sinus membrane barely visible in the middle of the osteotomy (dimple, Fig.6 (black triangle)), the sinus floor does not break upon Magic Sinus Lifter). Later the patient complains of discomfort with tapping. In fact Magic Drill (similar to trephine bur, Fig.7) is used to break into the sinus without membrane perforation (Fig.8). Remember the thick membrane (Fig.2,3). In fact the fractured fragment is attached to the membrane (Fig.9 red lines, green sticky fracture). A small curette is used to further separate the membrane from the bony wall (Fig.10) before insertion of a small piece of PRF and sticky bone. When a 4.5x7 mm dummy implant is incompletely placed with stability (<10 Ncm), the membrane is stretched over the bone graft (Fig.11 M). After removal of the dummy, the major remaining piece of PRF (from 9 cc vial) and more allograft are placed before inserting a definitive implant (same size) with 15 Ncm; still the used to be thick membrane remains intact and stretched (Fig.12 M). The implant is equicrestal buccal, while slightly supracrestal palatal. To prevent implant dislodgement into the sinus and bone graft, a final abutment is placed (Fig.12). The wound is closed with 4-0 PGA, perio glue and perio dressing. The latter dislodges 3 days postop. The wound seems to be healing. No dressing is reapplied.
Return to
Trajectory
No Deviation
第一磨牙即种
101
Xin Wei, DDS, PhD, MS 1st edition
02/03/2020, last revision
05/16/2021