


 |
 |
 |
 |
|
 |
 |
 |
 |
|
 |
||||
How to Prevent Peri-Implantitis?
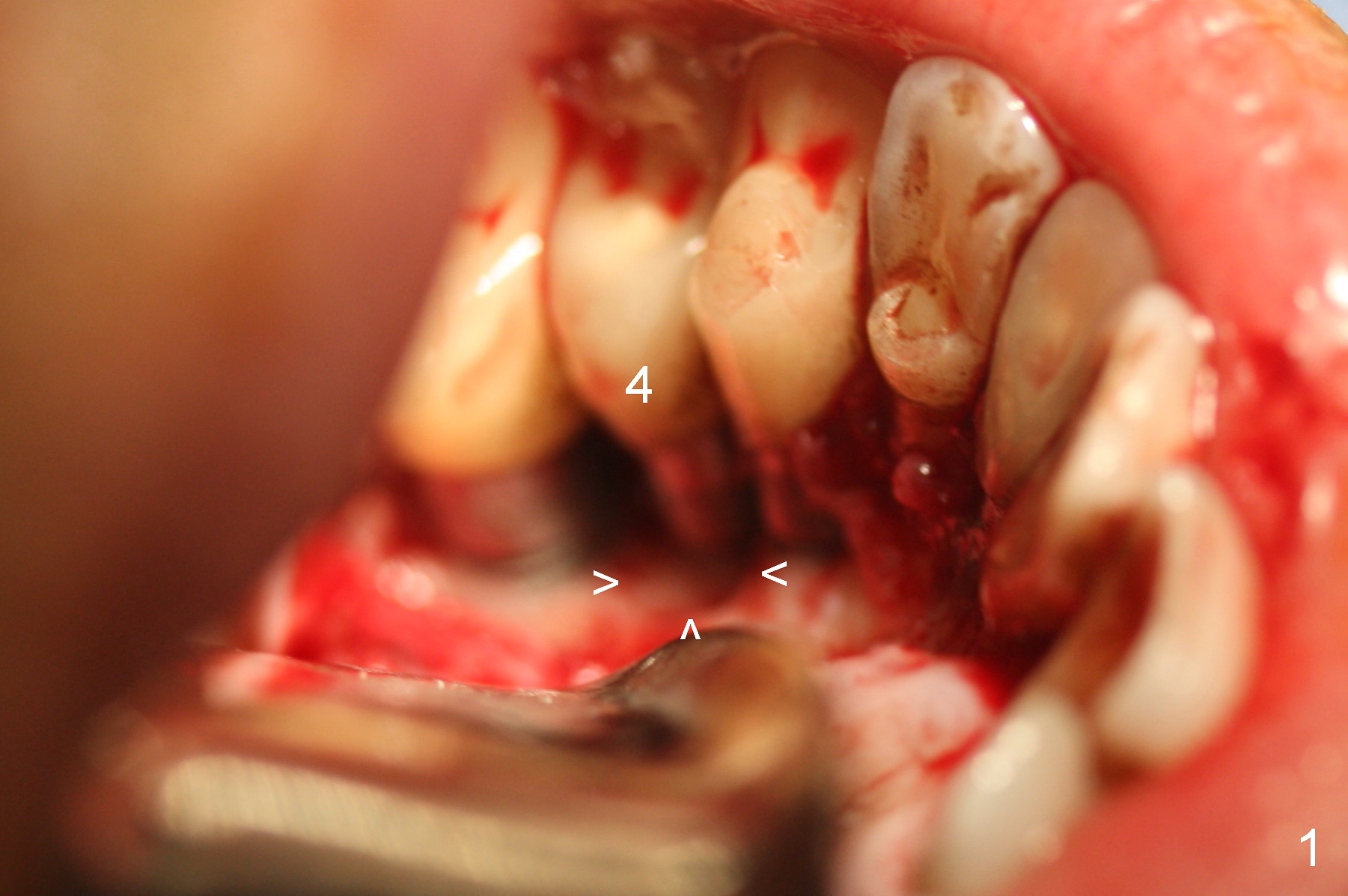
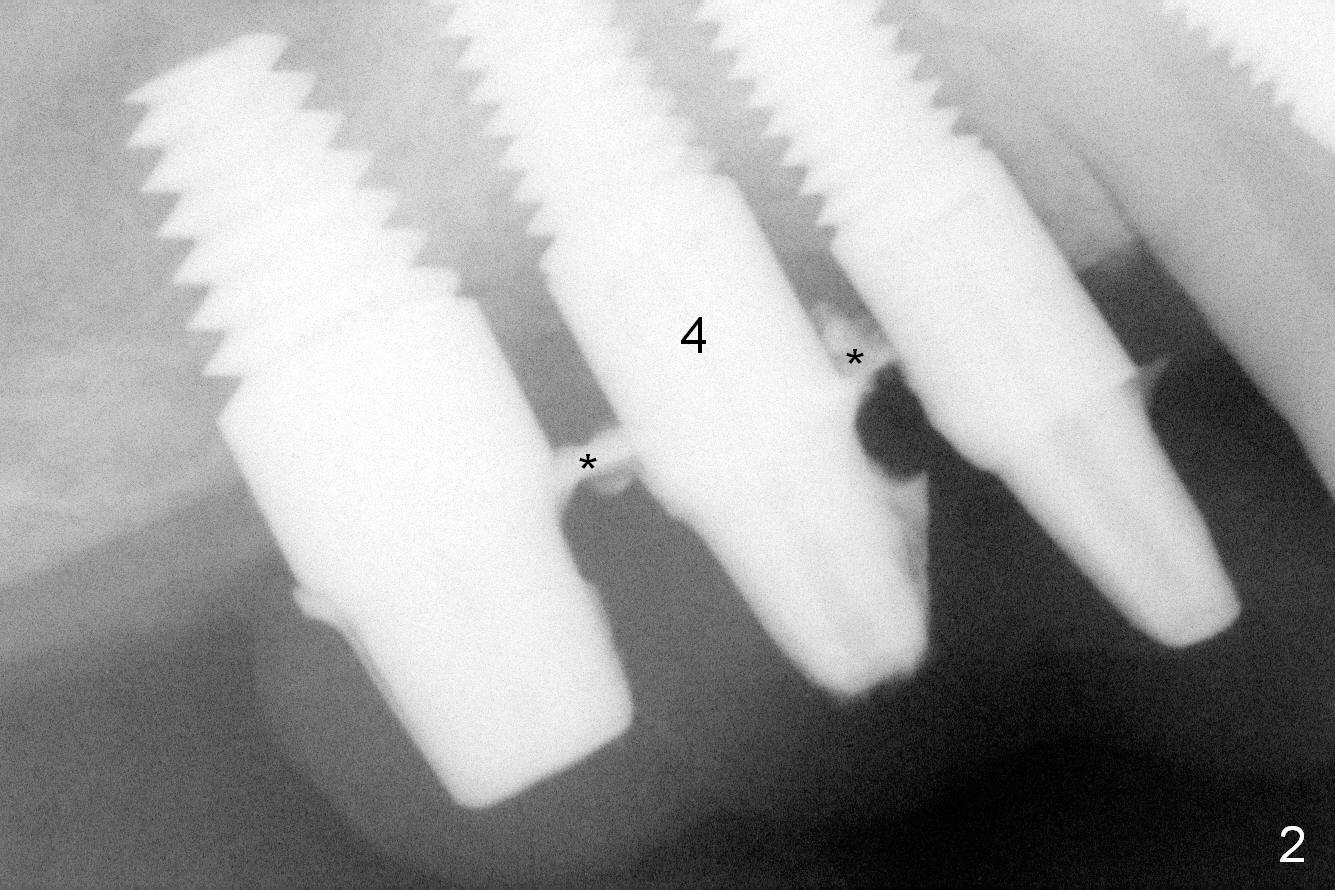
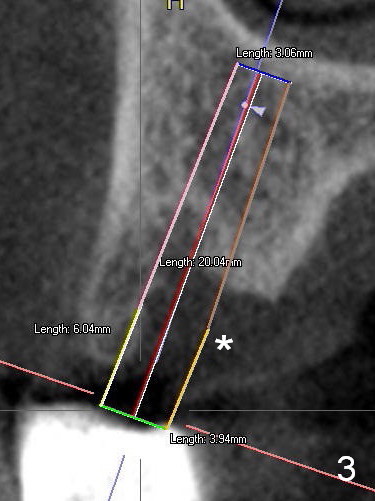
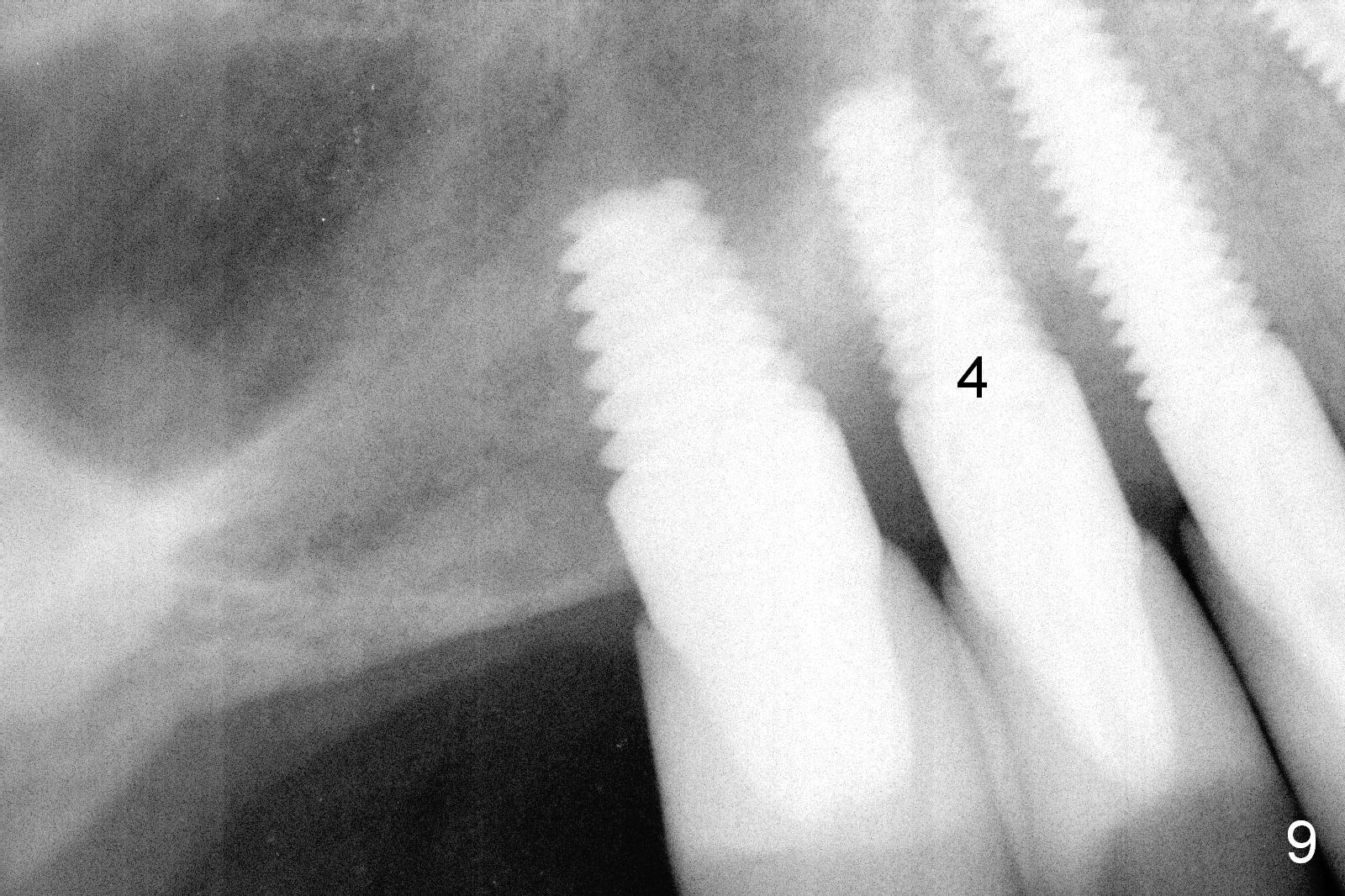
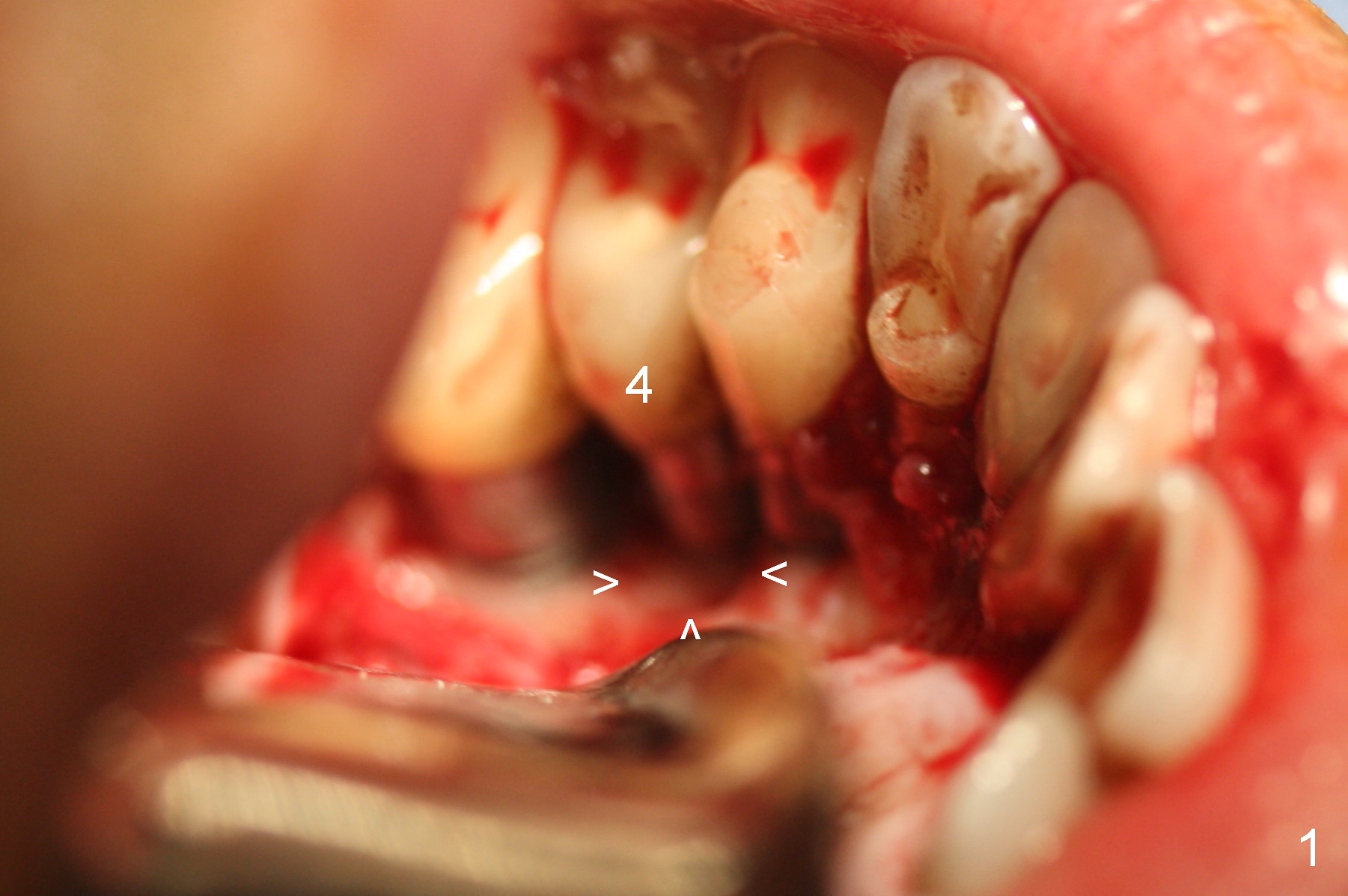
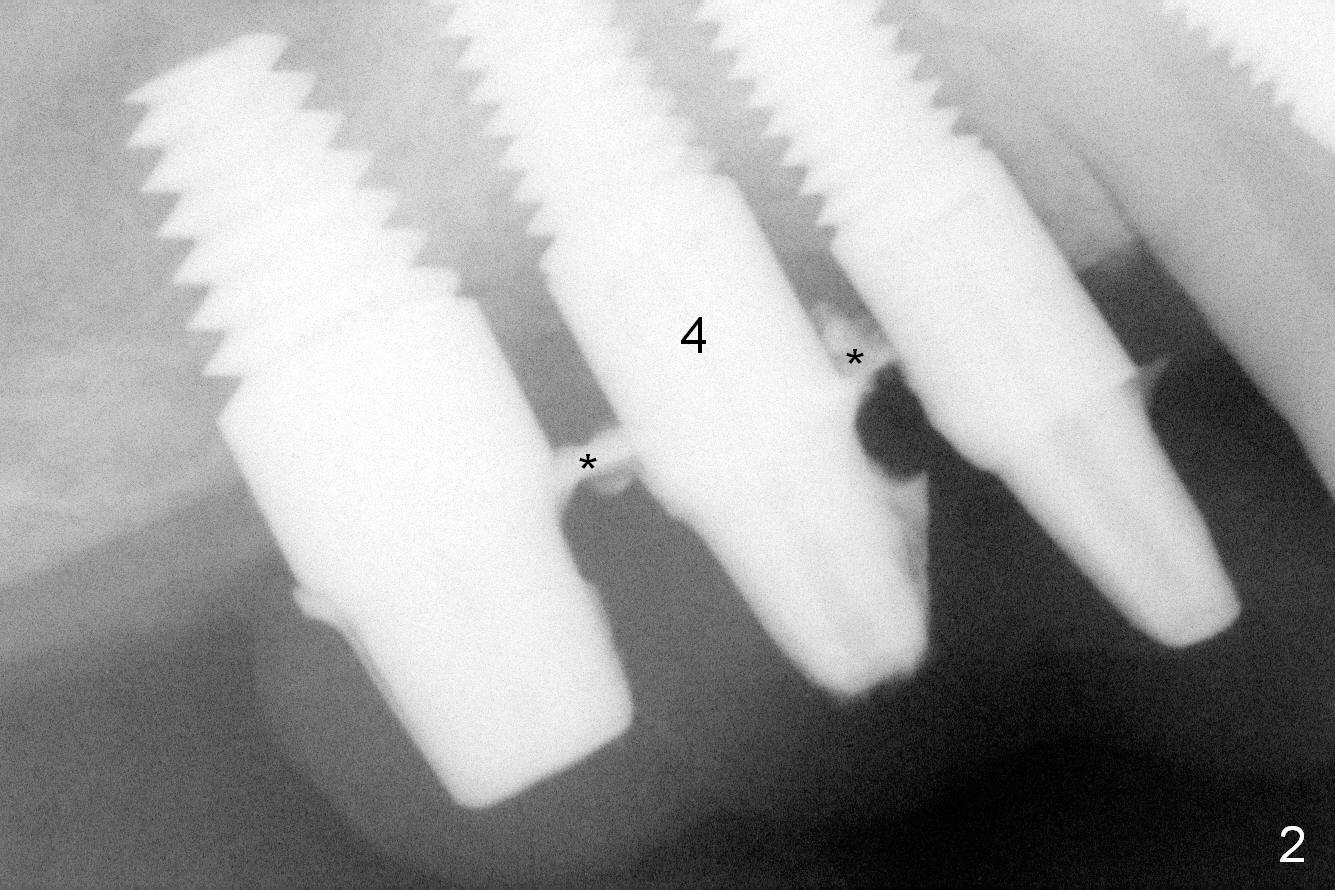
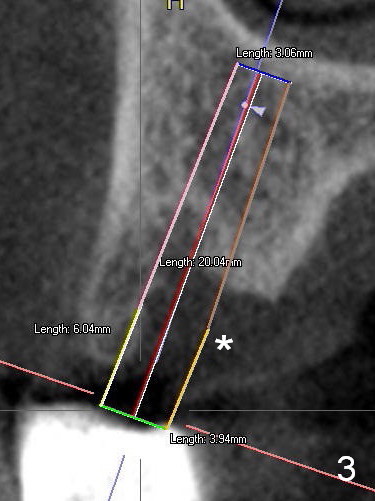
After reconfirmation of the deepest pocket between the implants at #3 and 4, a palatal sulcus incision is made with reflection of the flap. After granulation tissue curettage, a crater is found palatal to the implant at #4 (Fig.1 arrowheads), consistent with preop CT coronal section (Fig.3 *). Another complicating factor is excess temporary cement used for splinted provisional between #3 and 5 (Fig.2 *) between 0.5 and 4 months post #4 implant placement.
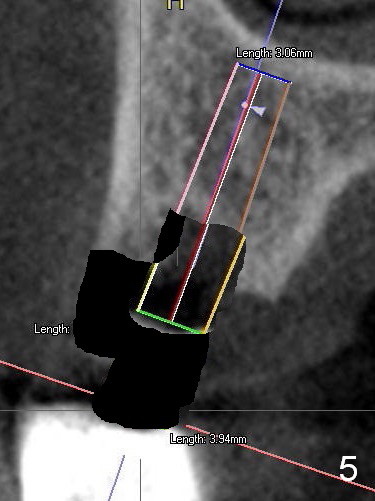
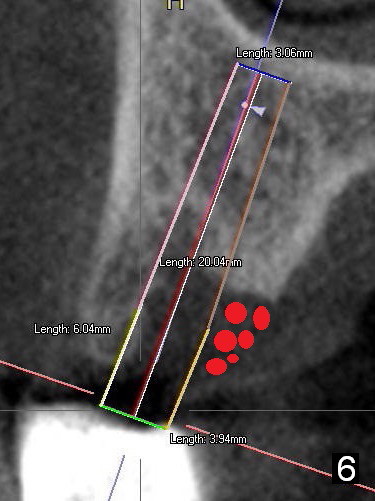
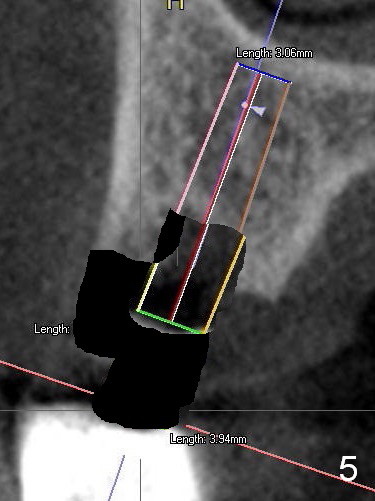
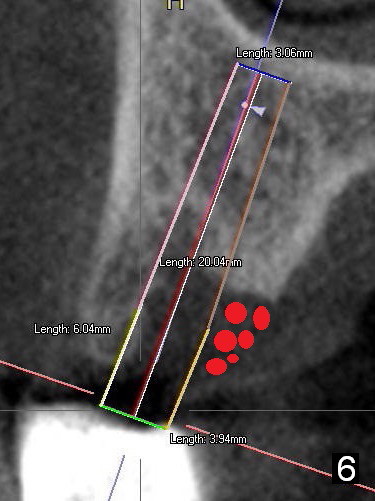
At the implant placement, either the buccal bone should have been removed (Fig.4 black area) and a shorter implant be placed (Fig.5). Or bone graft should have been placed palatal to the long implant (Fig.6 red circles).
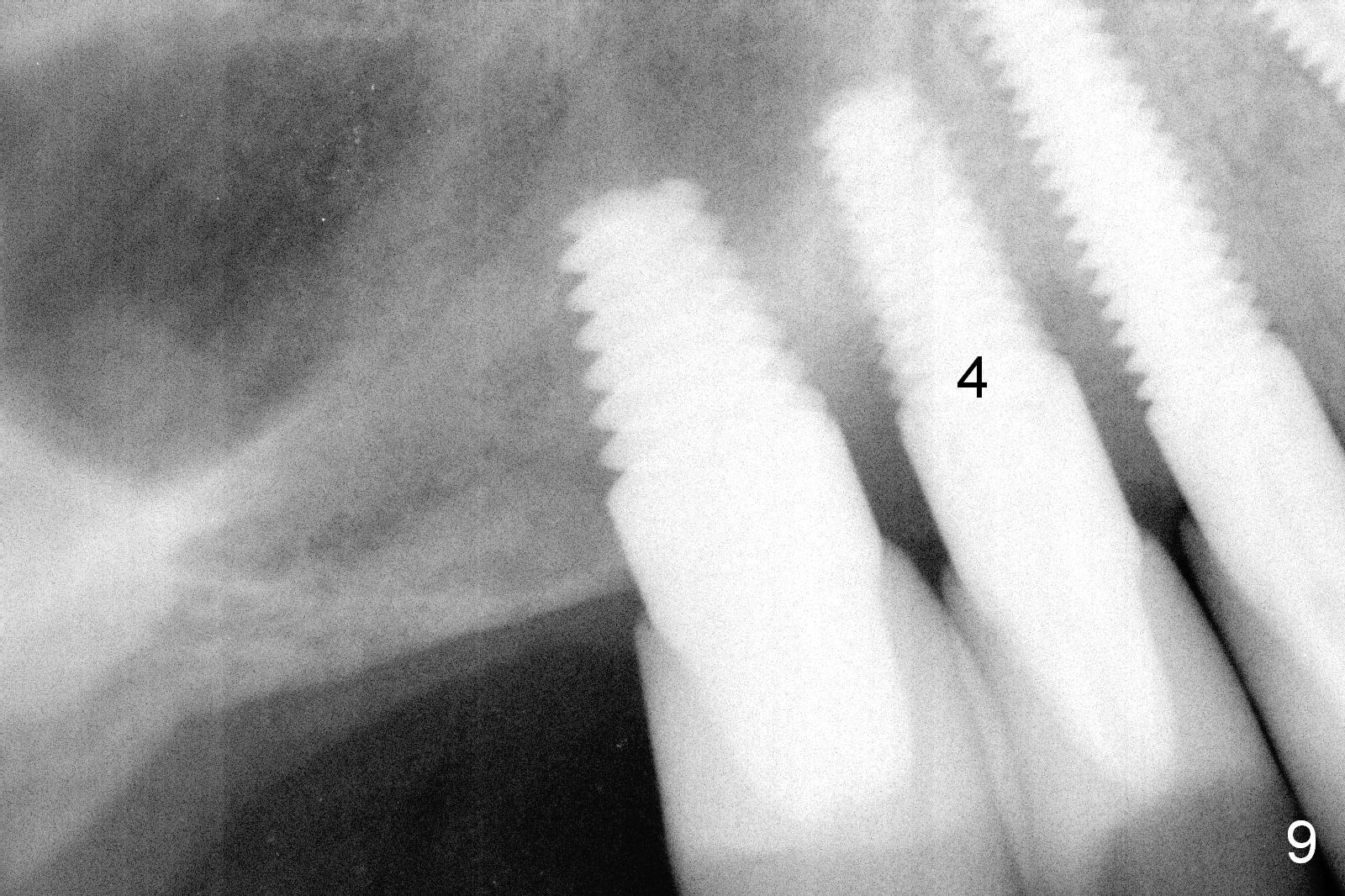
The patient returns for follow up 3 months postop. There is no gingival bleeding around the site of #4 palatally (Fig.7) or buccally (Fig.8). There is no further bone resorption (Fig.9).
Six months postop, periimplantitis relapses. Bone graft is re-done in 4 different manners. Envelop incisions are made both buccal and palatal (vs. palatal in the 1st try). Granulation tissue is found mainly interproximal. Autogenous bone (vs. allograft) is harvested from the buccal plate of the edentulous area of #1 and 2. Graft is mainly placed interproximal (vs. palatal). Last PRF membrane (vs. collagen membrane) is placed palatal, while collagen dressing is placed buccal. It would be better to dip the dressing in the PRF liquid lightly before application or inject the liquid after dressing application.
Return to
Peri-implantitis
Xin Wei, DDS, PhD, MS 1st edition 11/22/2015, last revision 05/31/2016