
 |
 |
 |
 |
 |
 |
Short Tatum Implant (Part 1)
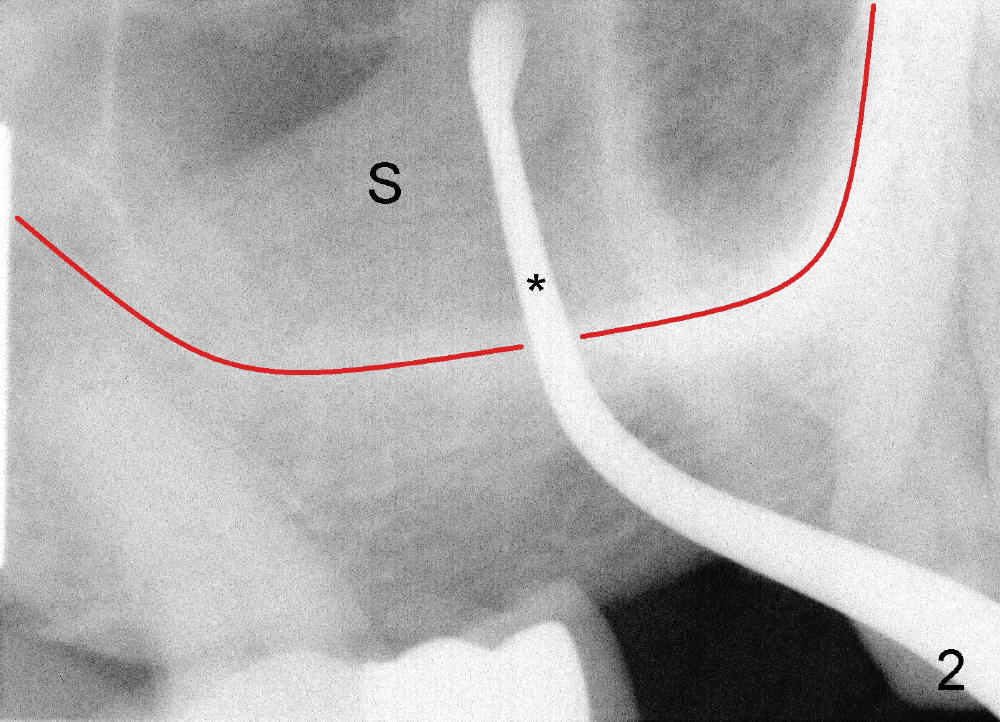
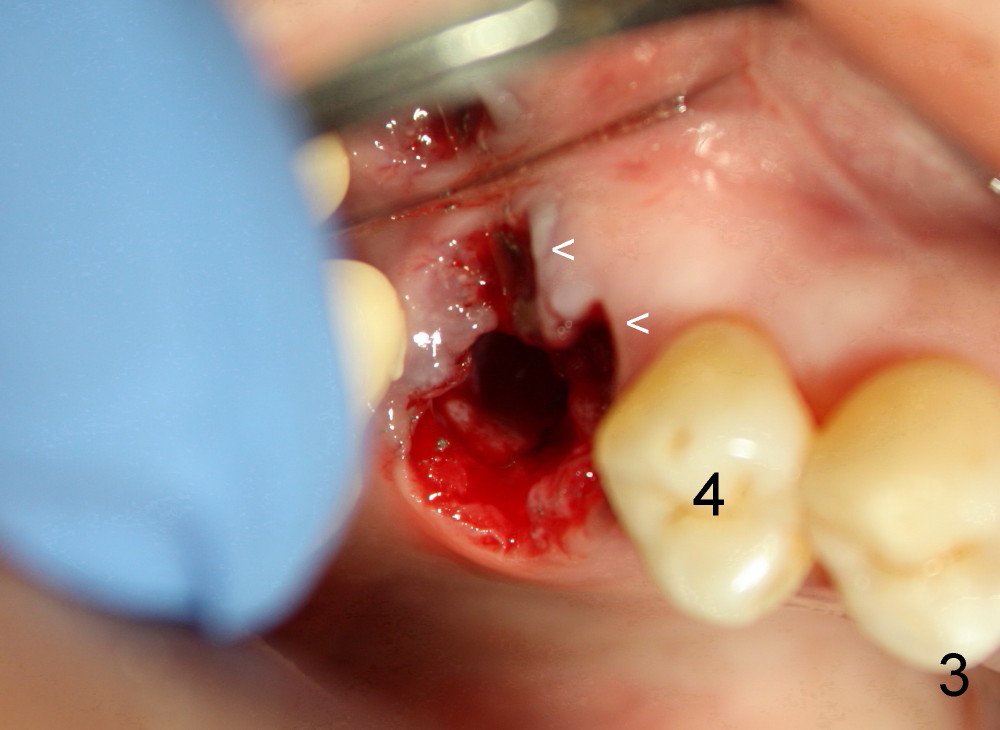
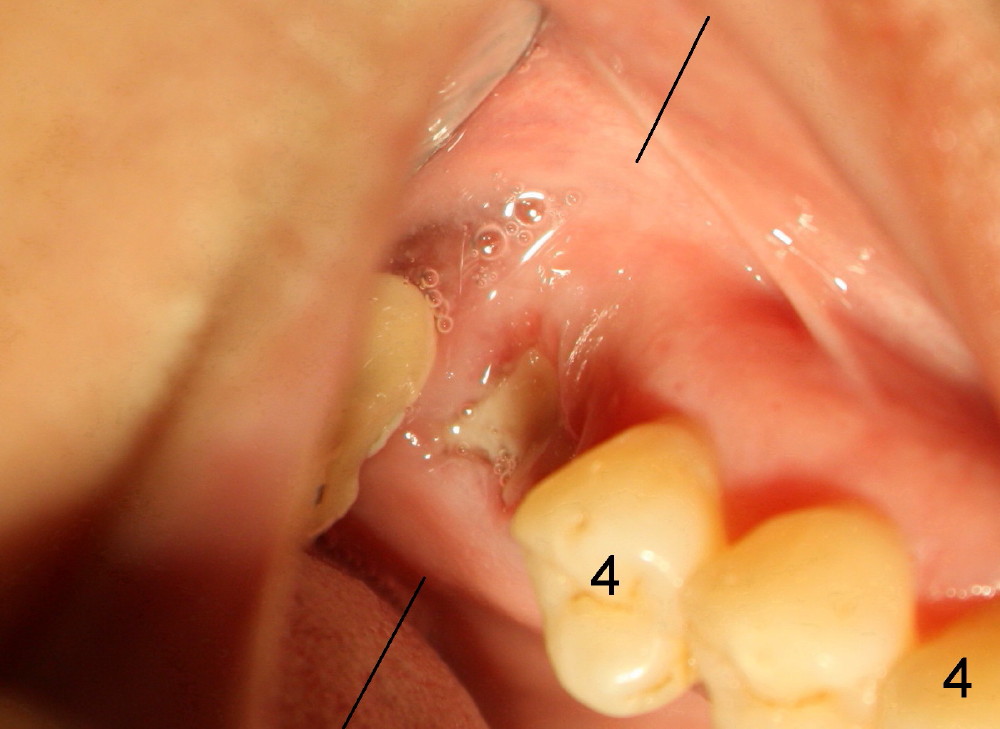
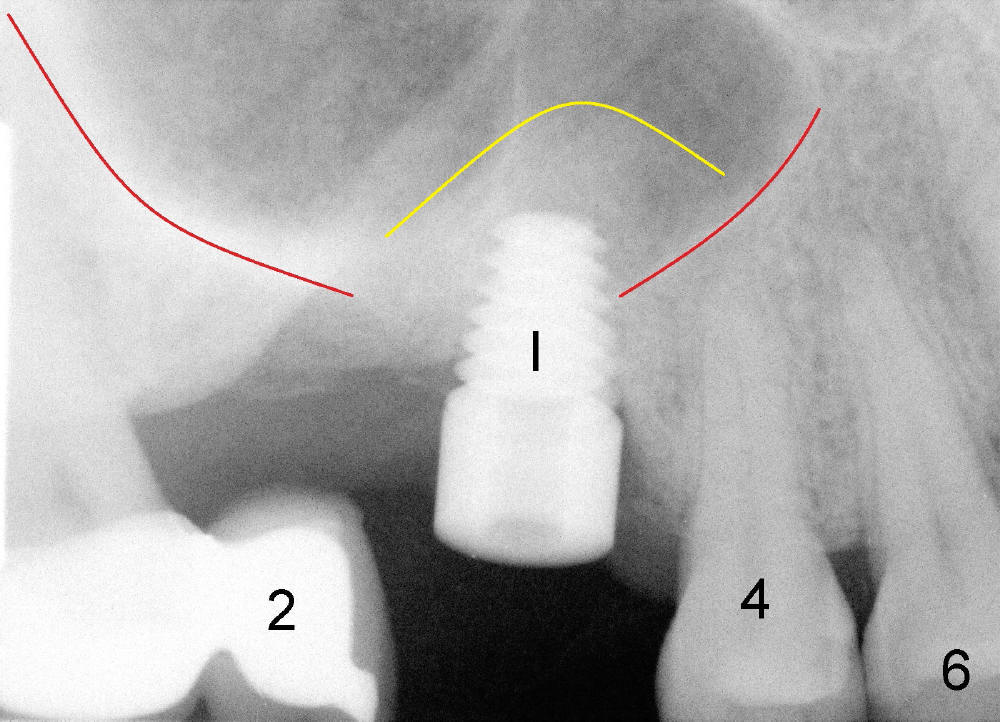
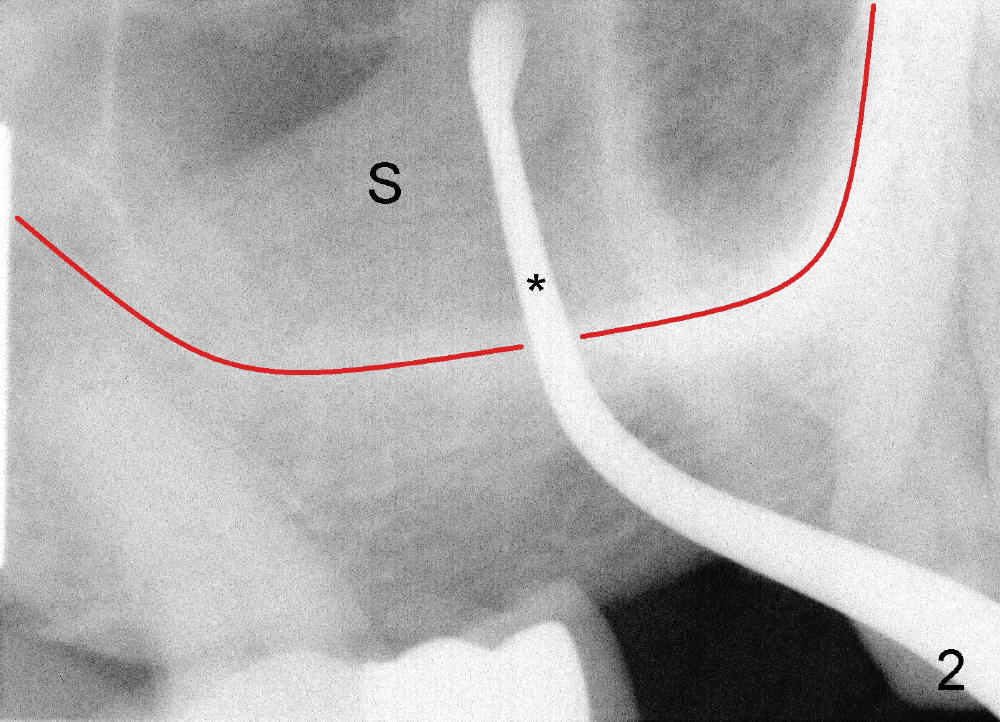
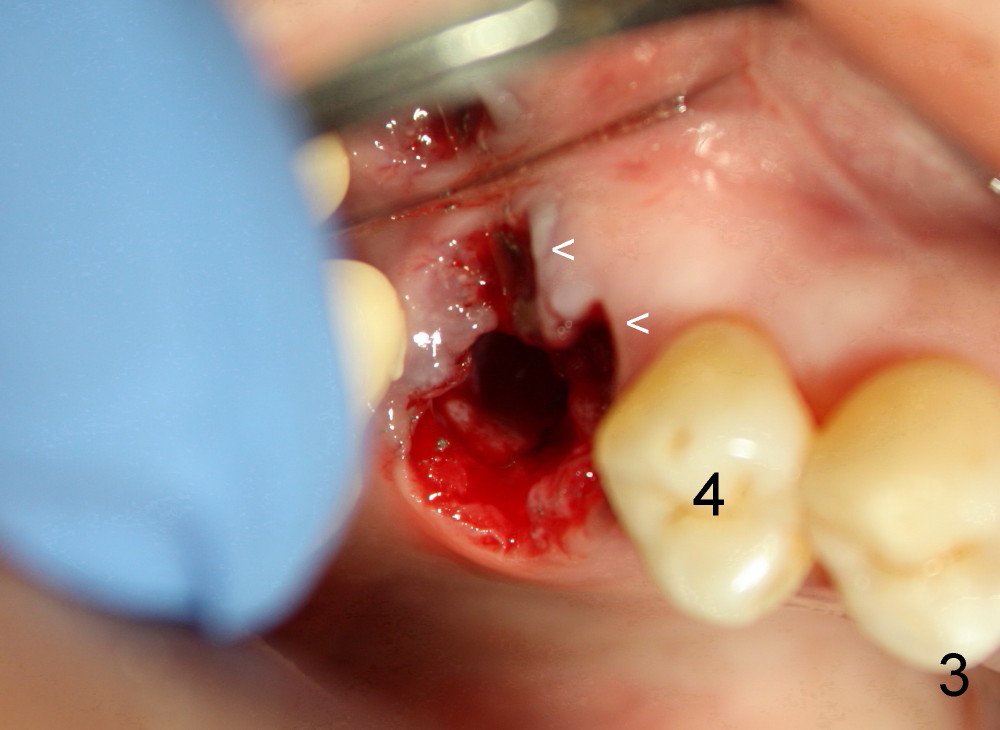
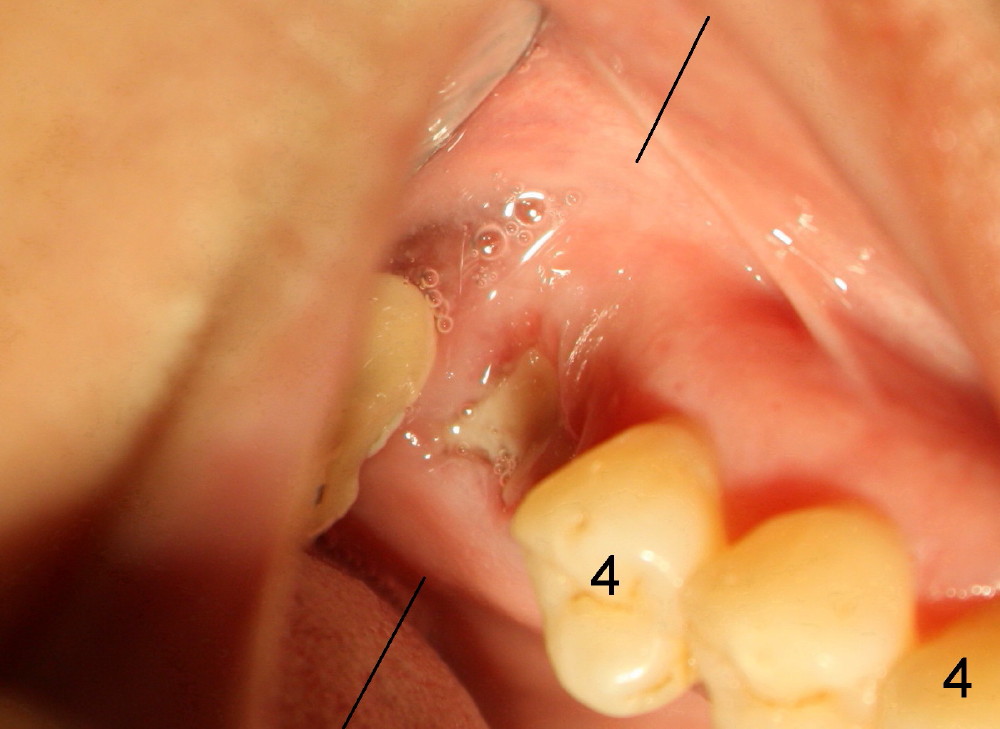
A fifty-four-year-old Chinese lady is a typical fearful patient. She has an atypical bridge to replace the tooth #2 (Fig.1). The anterior abutment, the tooth #3, is failing with severe bone loss. An immediate implant is planned after extraction considering her fear, not to mention sinus graft. After the extraction, the socket is found to communicate with the sinus (Fig.2 S; *: surgical curet). In addition, The red line represents the bottom of the sinus. In addition, there are large gingival defects involving buccal roots (Fig.3 <) . It appears that immediate implant placement is not indicated. In one week the wound was healing nicely (Fig.4).
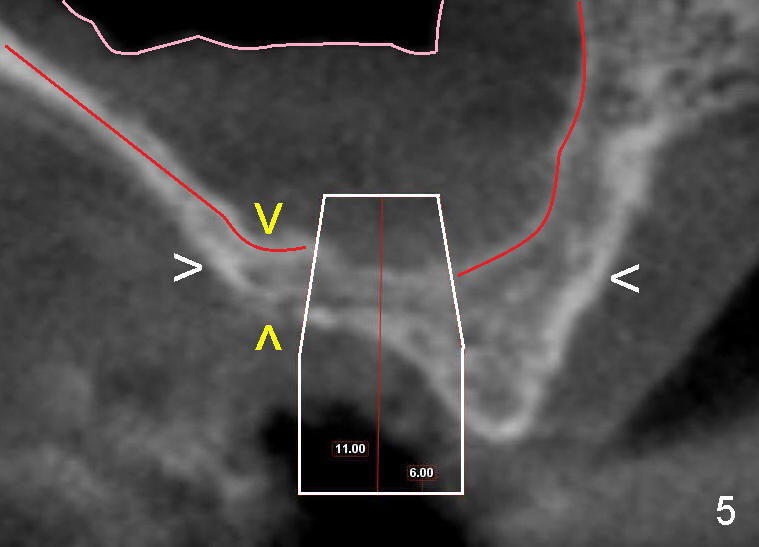
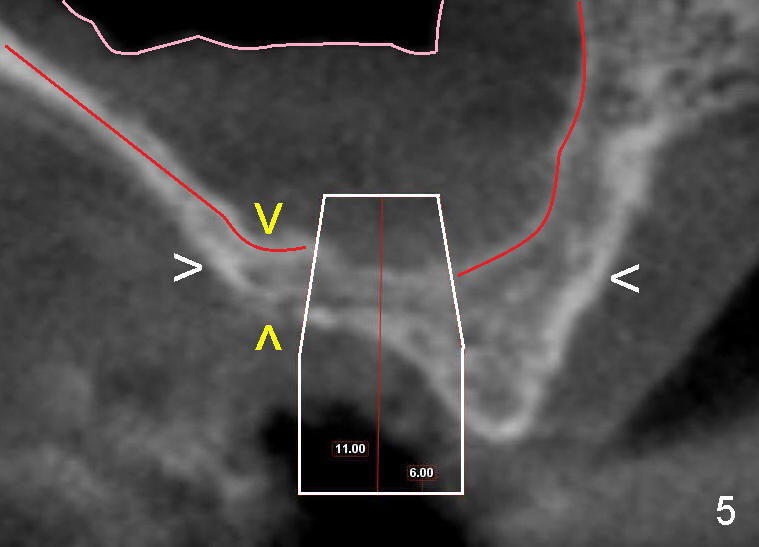
CT taken less than a week after extraction shows that the bone is wide (Fig.5 (cross section of the healing socket as indicated by lines in Fig.4) between white arrowheads), whereas the height is limited (between yellow >). A wide, but short implant is planned (as shown in Fig.5 white box: 6x11 mm). The top end of the implant is protruded into the sinus, but still within the sinus membrane (soft tissue, between pink and red outlines).
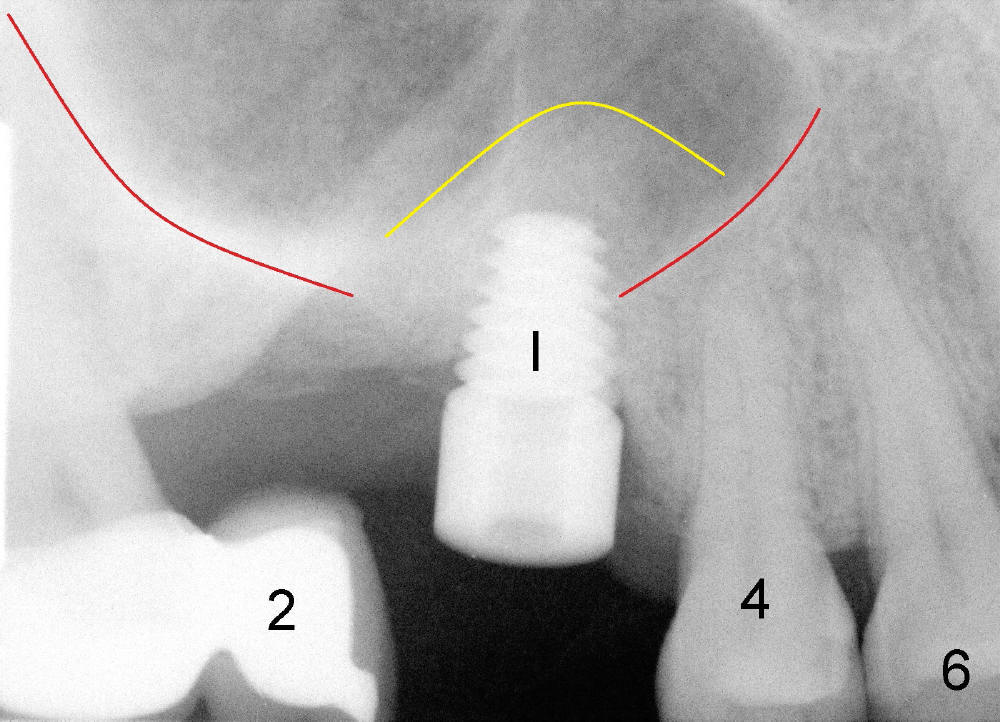
One month after extraction, an implant is placed (Fig.6: I, as planned: 6x11mm, >60 Ncm). In fact with bone expansion (osteotomes and tapered taps (no drill)) and placement of the implant, bone is pushed upward into the sinus (yellow outline as compared to original sinus floor (red outline)). In fact, a small area is found to be continuous with the sinus. It appears that bone graft through sinus lift is not appropriate. But I have to place the implant, because this fearful patient would not allow me to do the same surgery for a second itme.
How is she doing after implant surgery? She feels a little pain when numbness wears off. But next morning she feels fine. There is no nasal bleeding either after extraction or implant placement. There has been two months since implant placement. No sign of infection or discomfort is noticed.
Return to Professionals
Xin Wei, DDS, PhD, MS 1st edition 04/20/2013, last revision 04/21/2013