





 |
 |
 |
 |
|
 |
 |
 |
||
 |
 |
 |
||
 |
 |
 |
||
 |
 |
 |
 |
 |
Angled 1-Piece Implant for Deep Bite
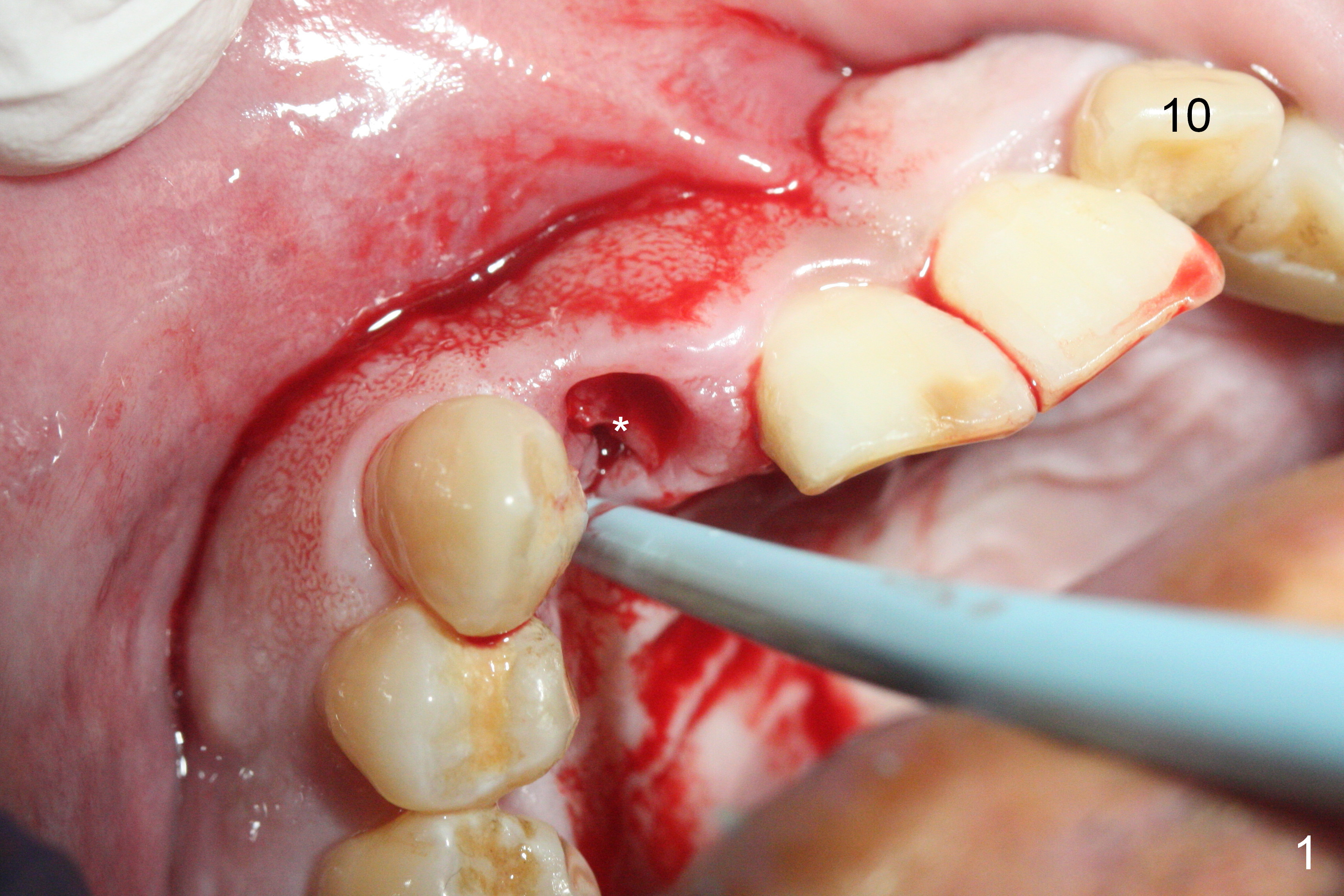
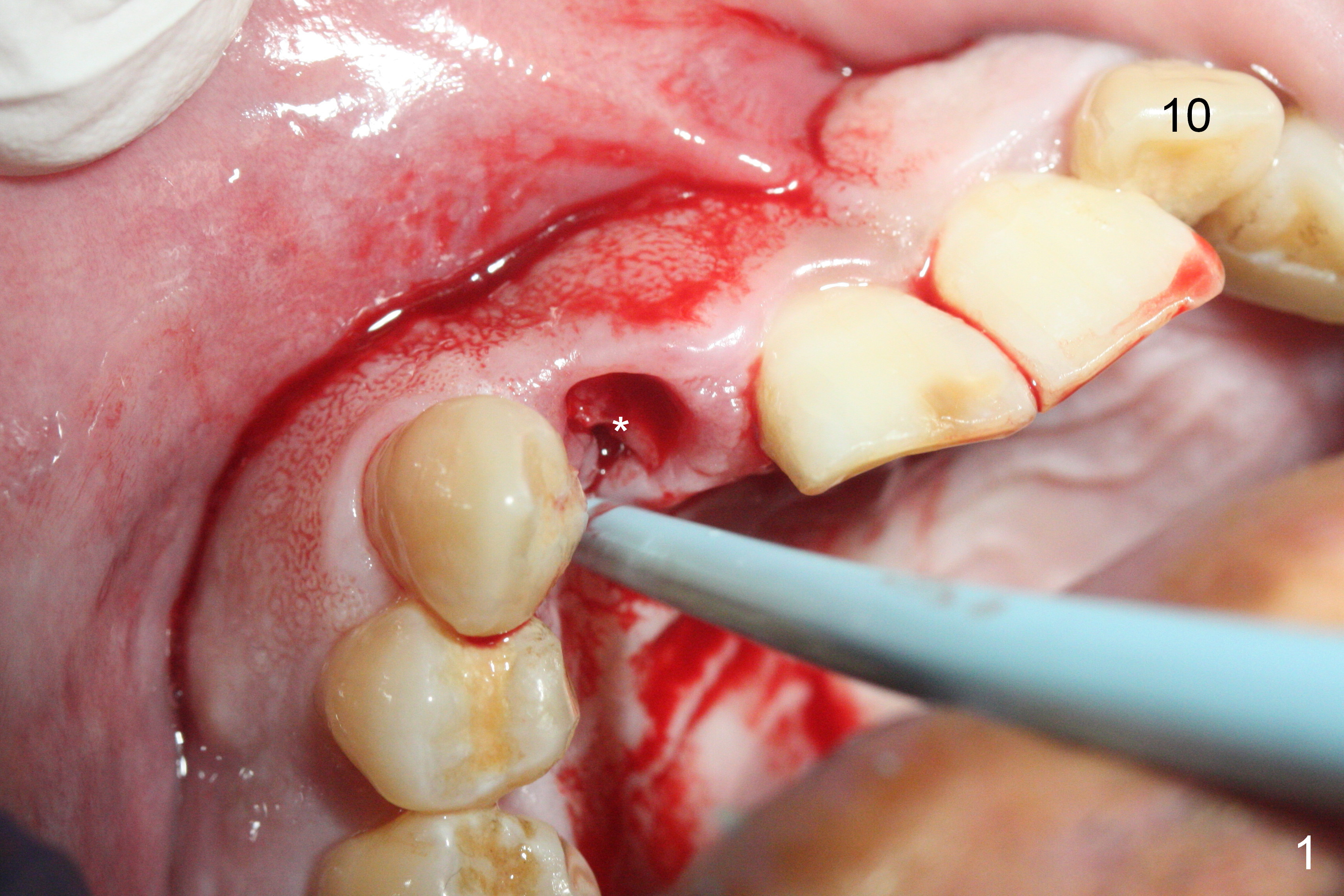
Access to the fractured root is limited after the crown is removed (Fig.1 *). Note the buccally-positioned tooth #10. After explanation the patient accepts in advance the possibility of the similar or same position of the restoration at #7.
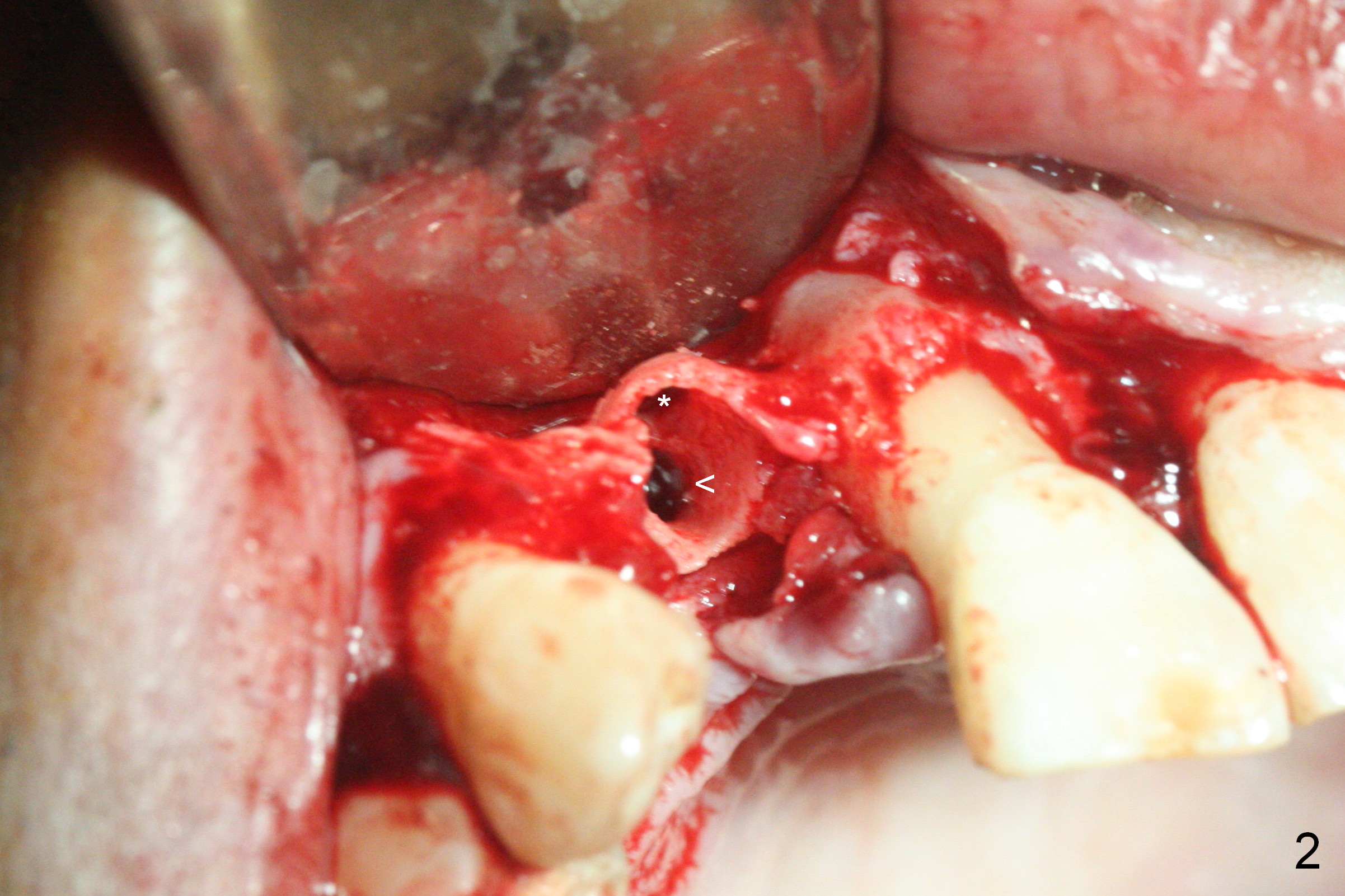
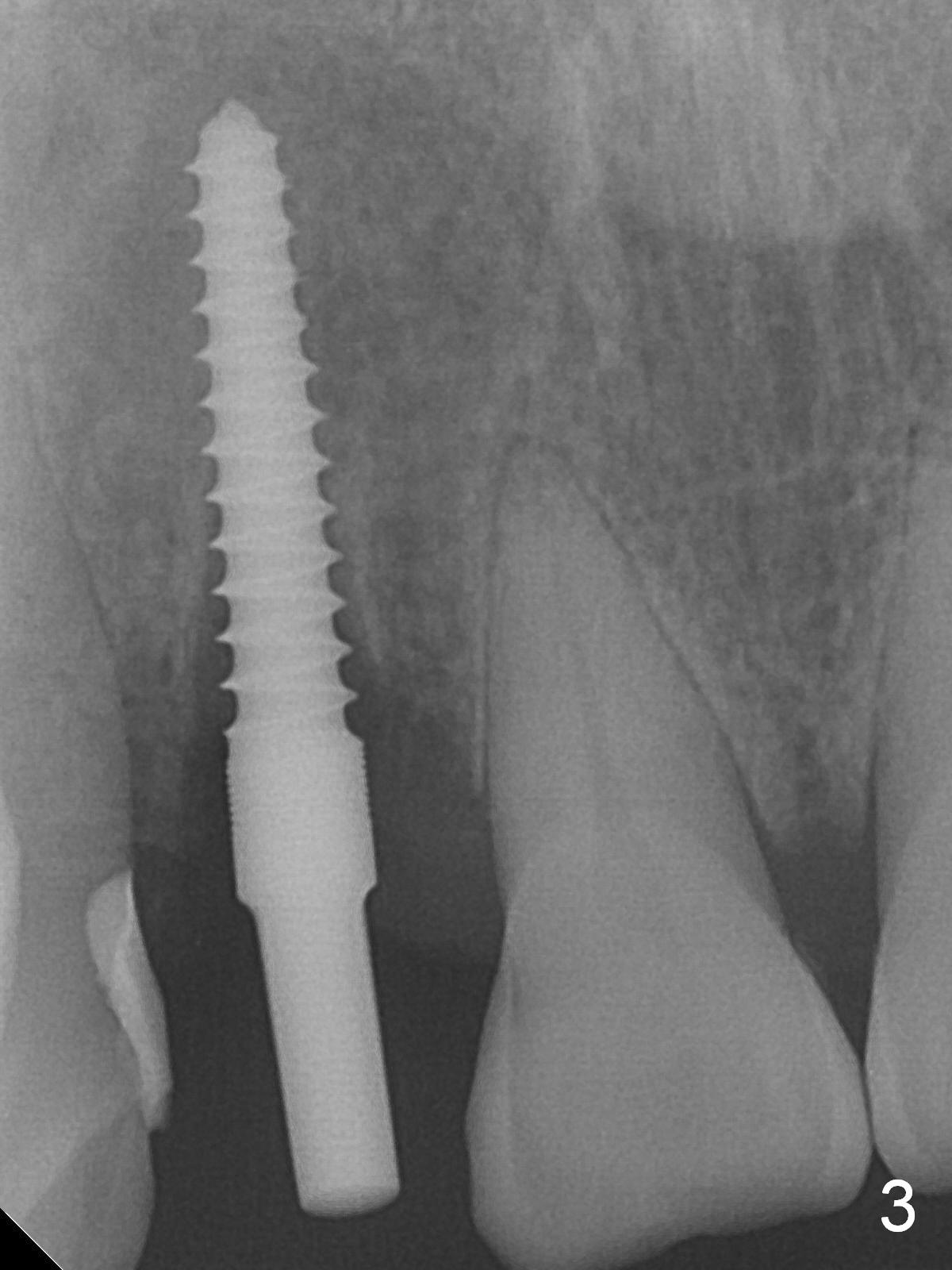
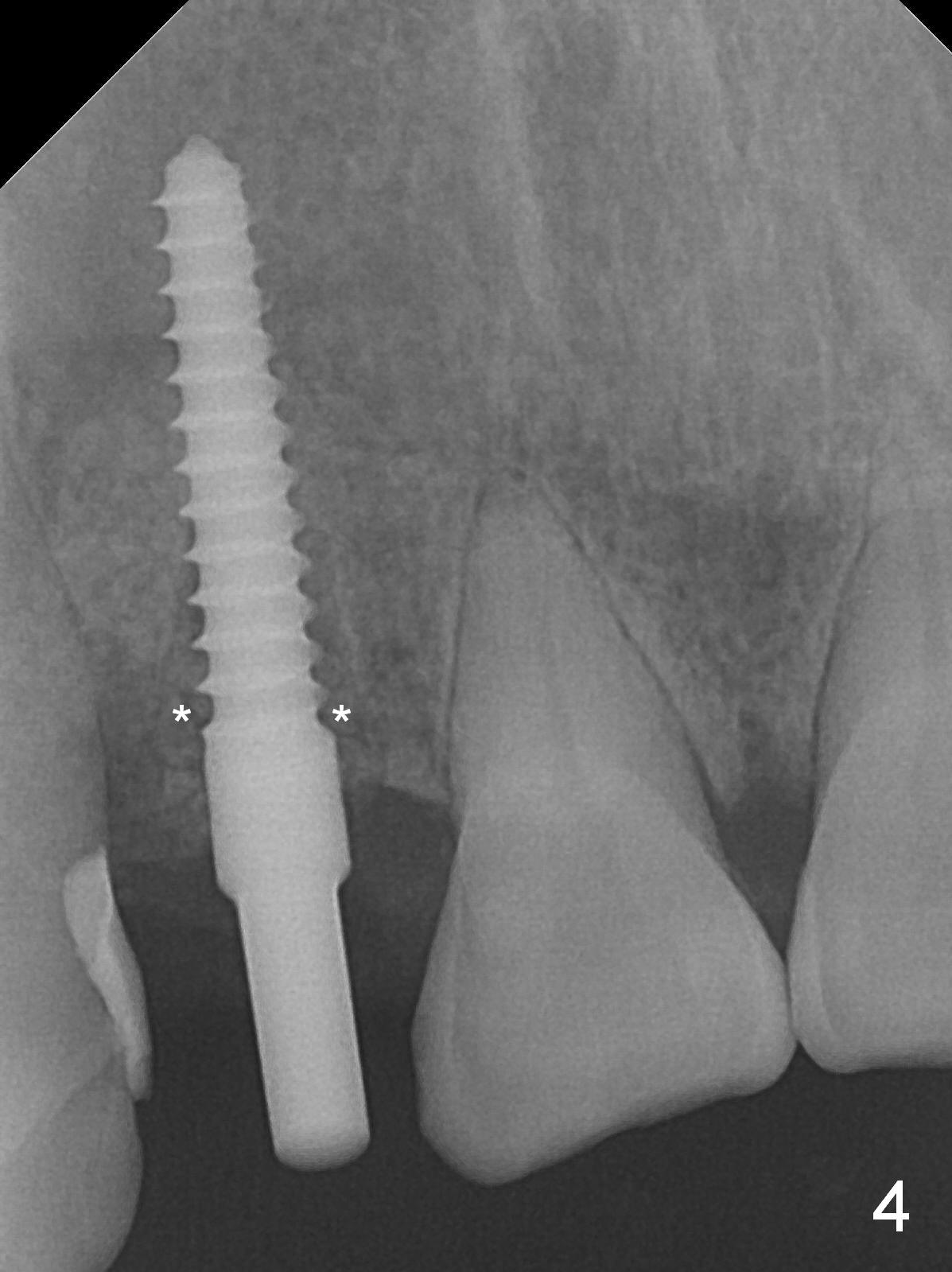
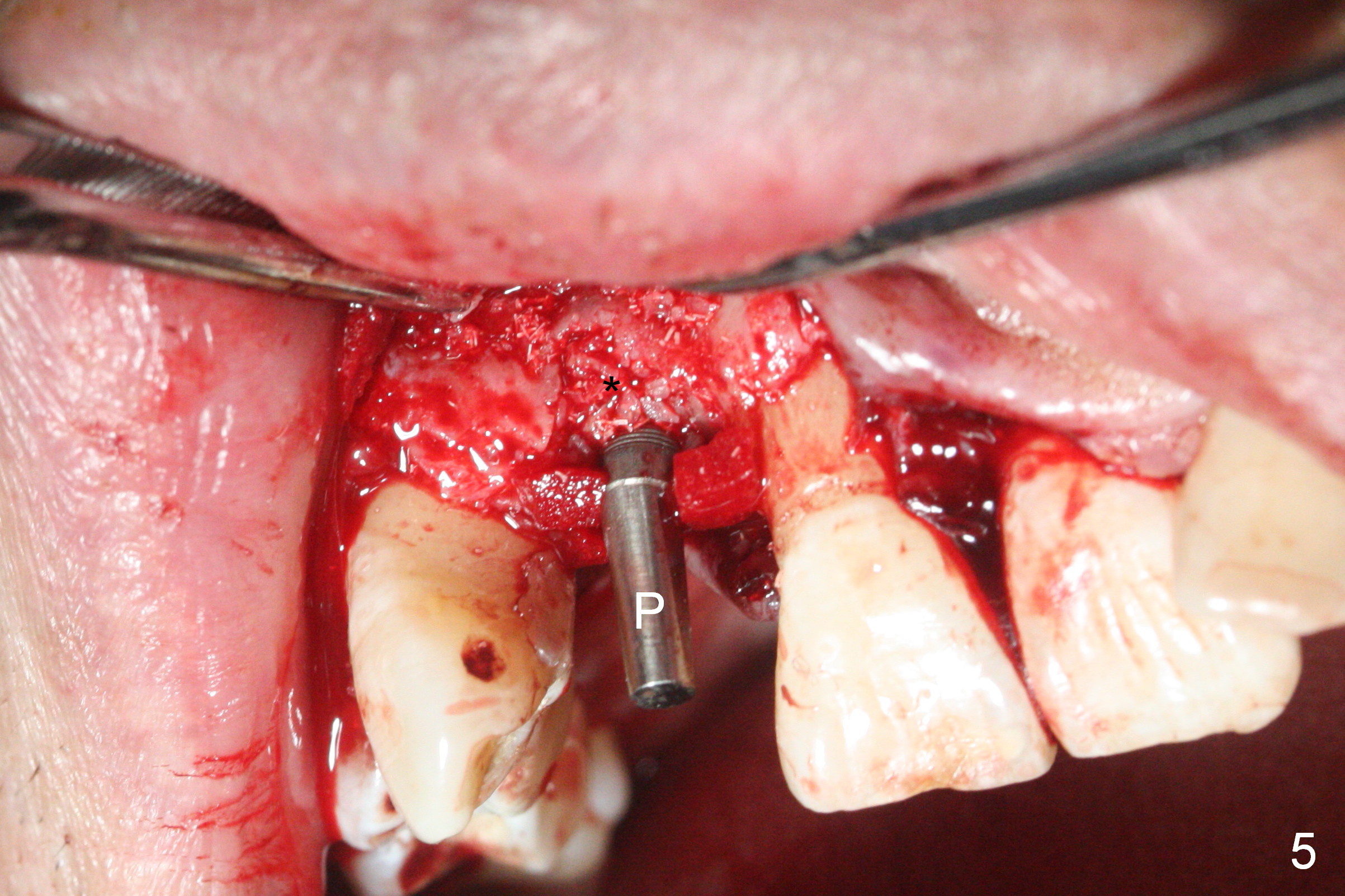
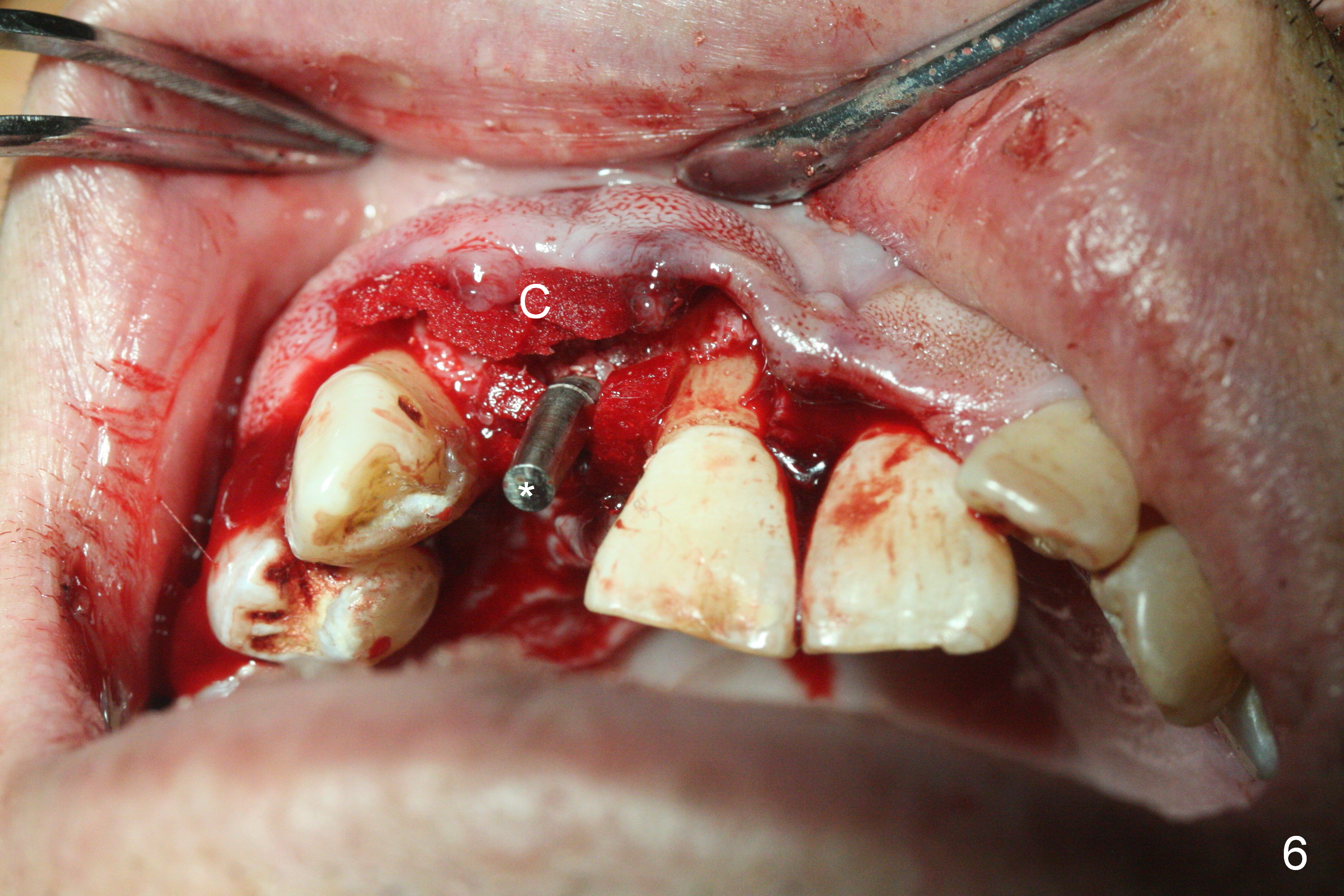
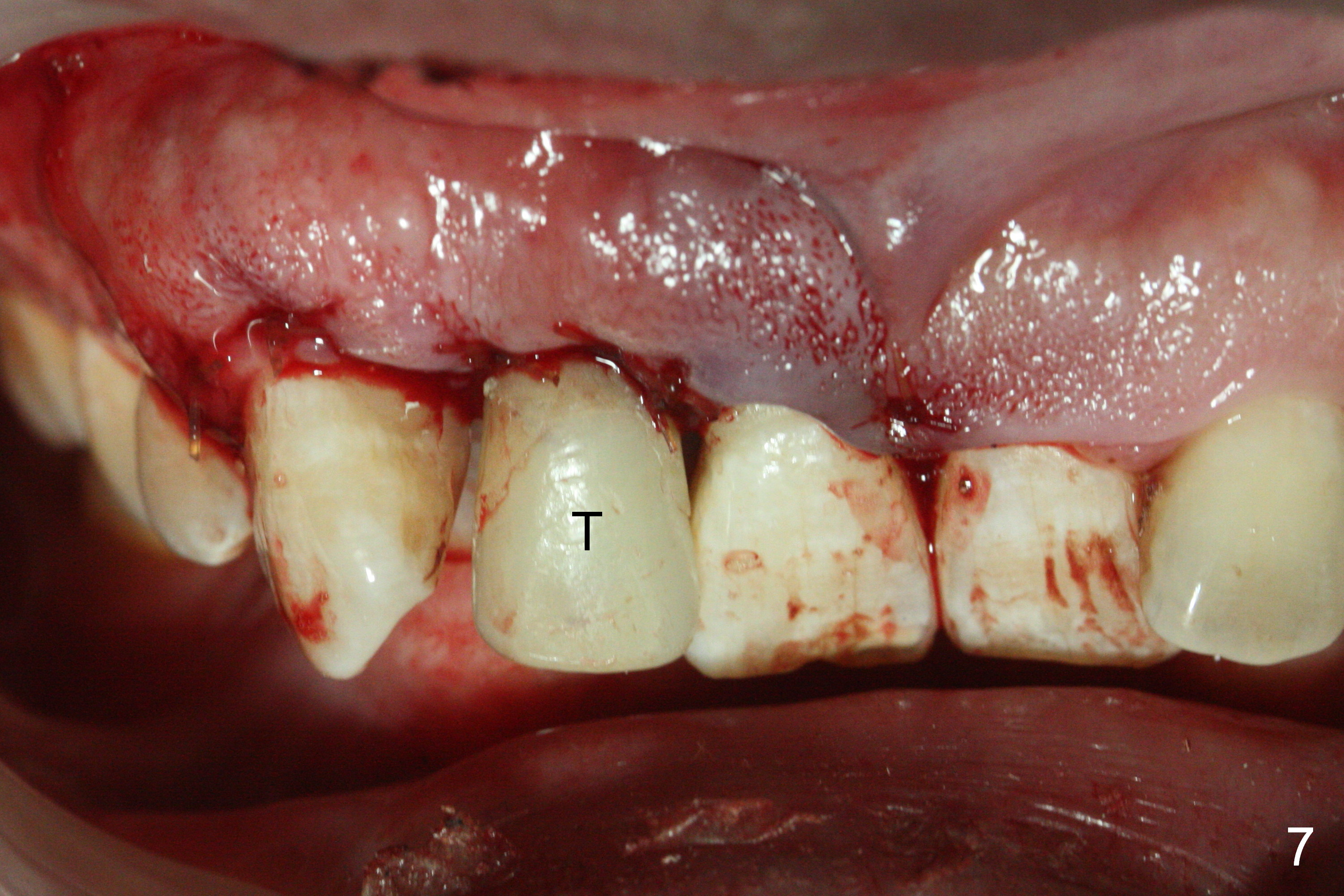
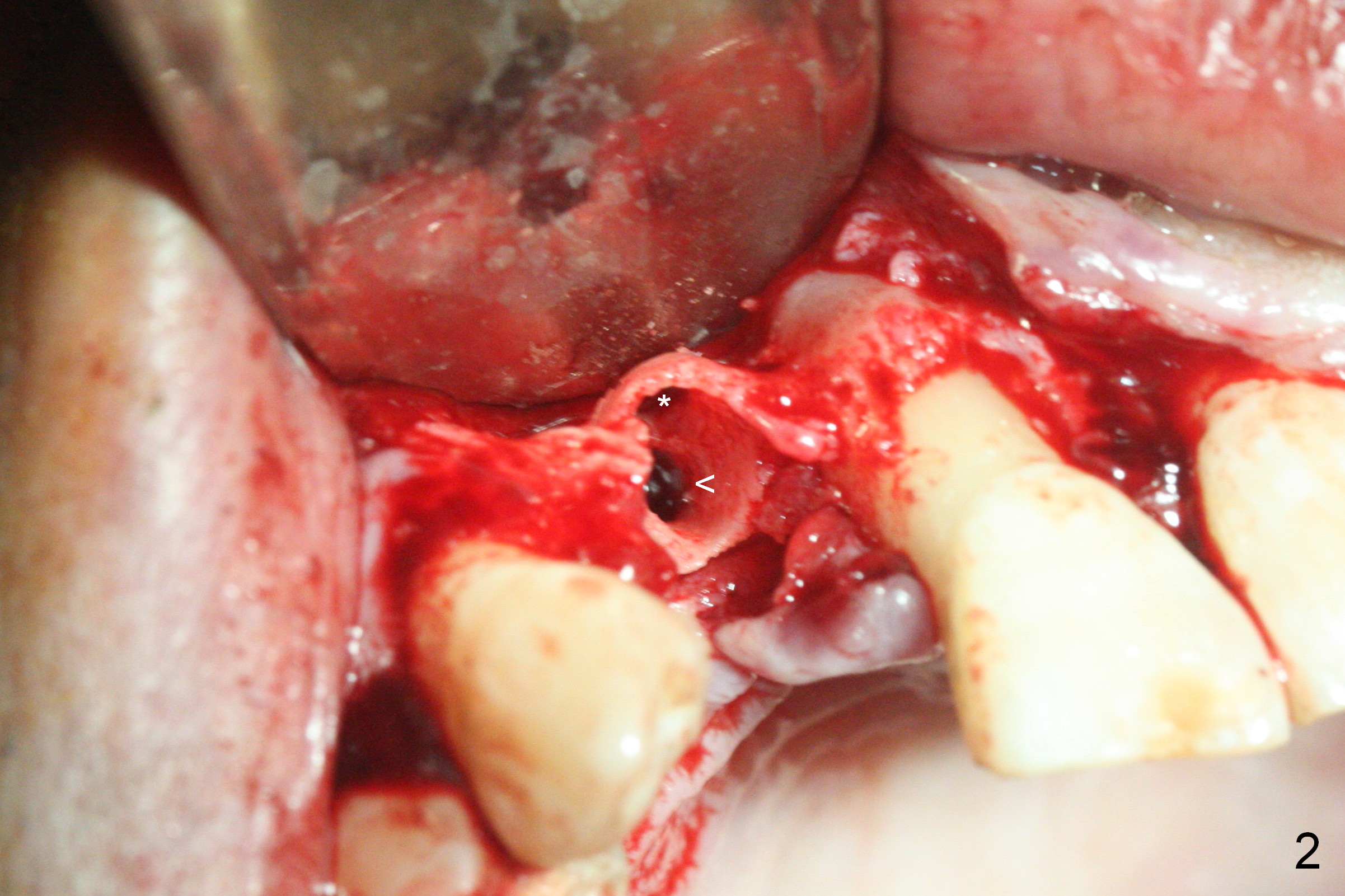
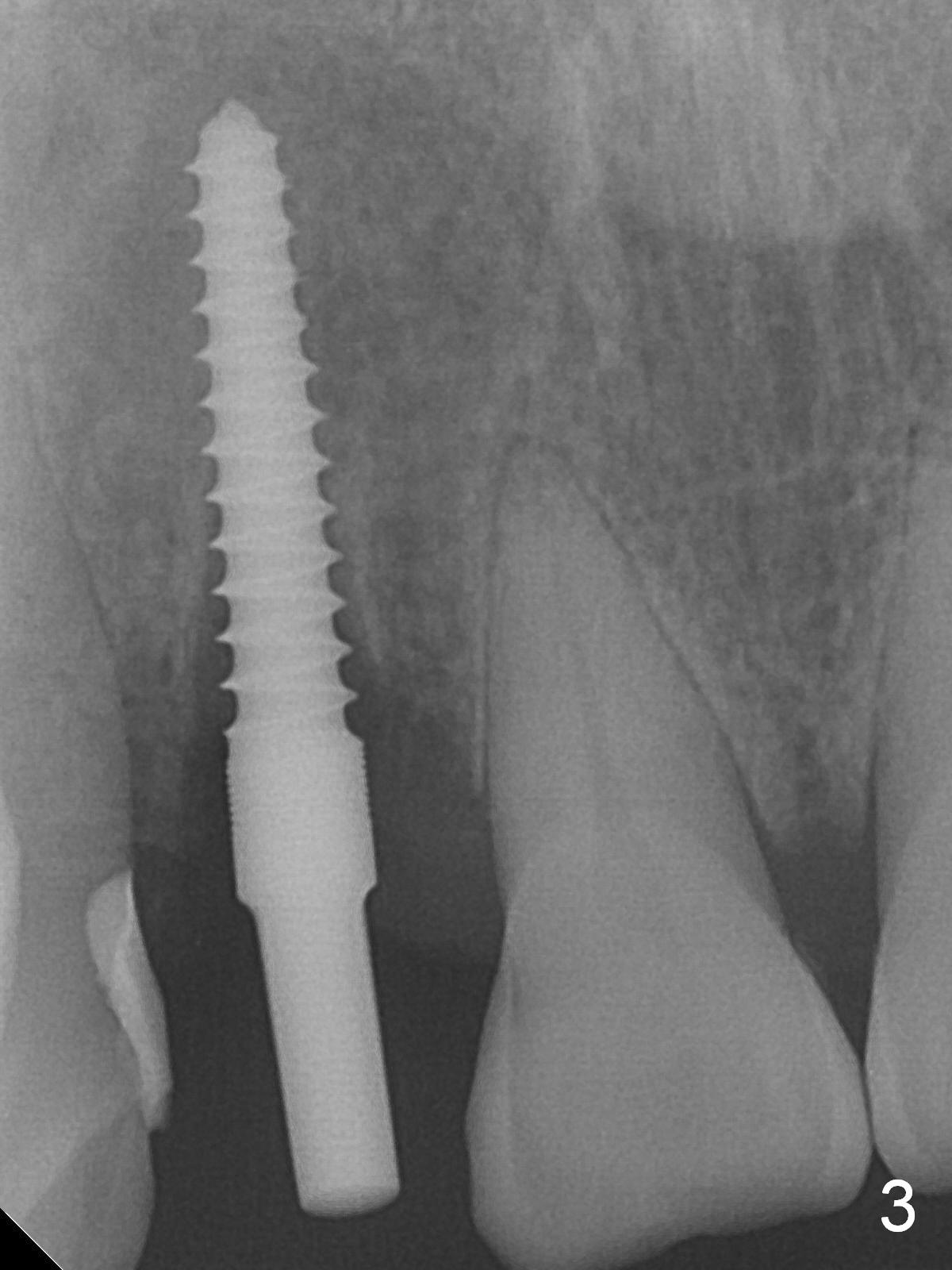
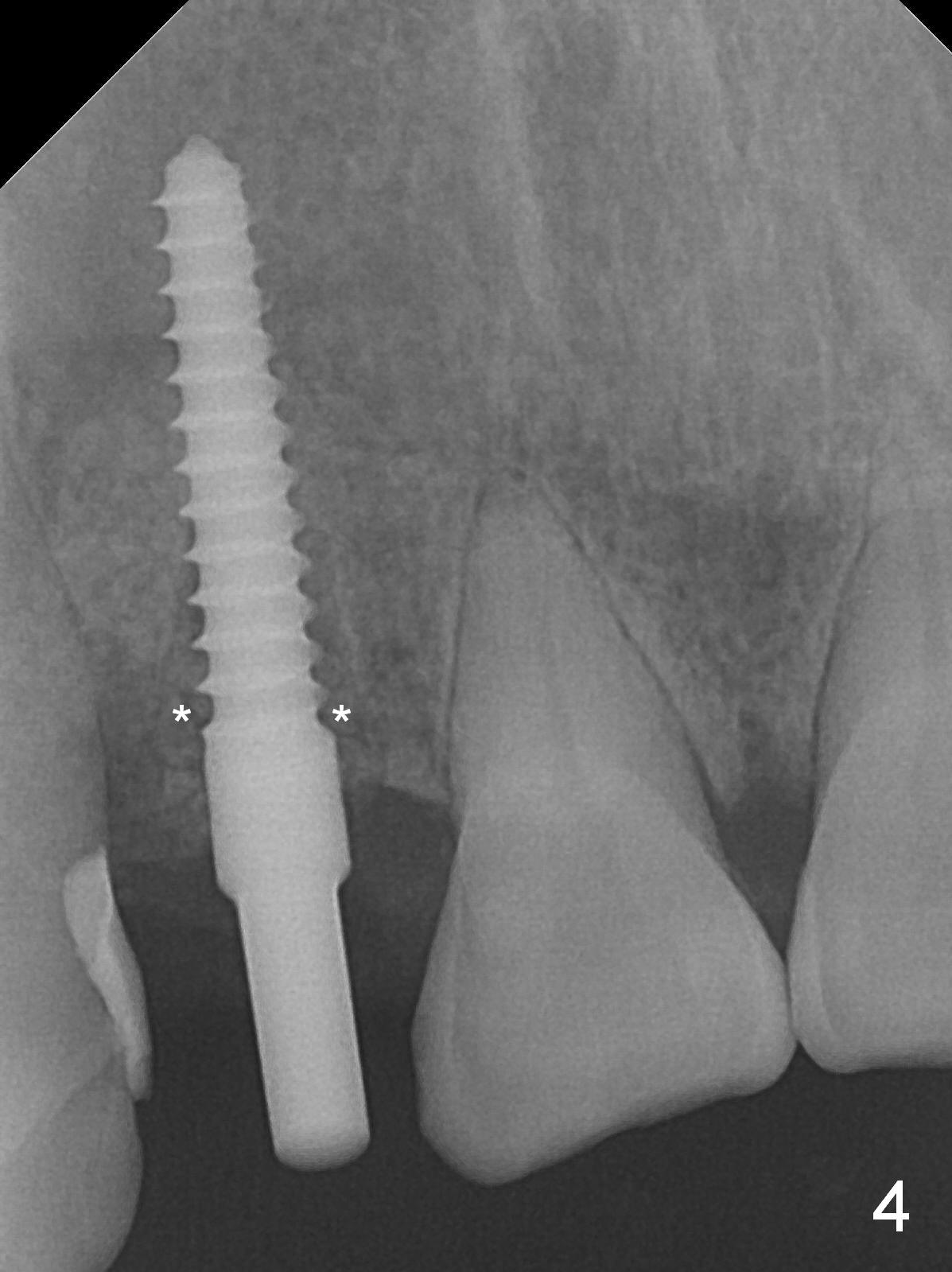
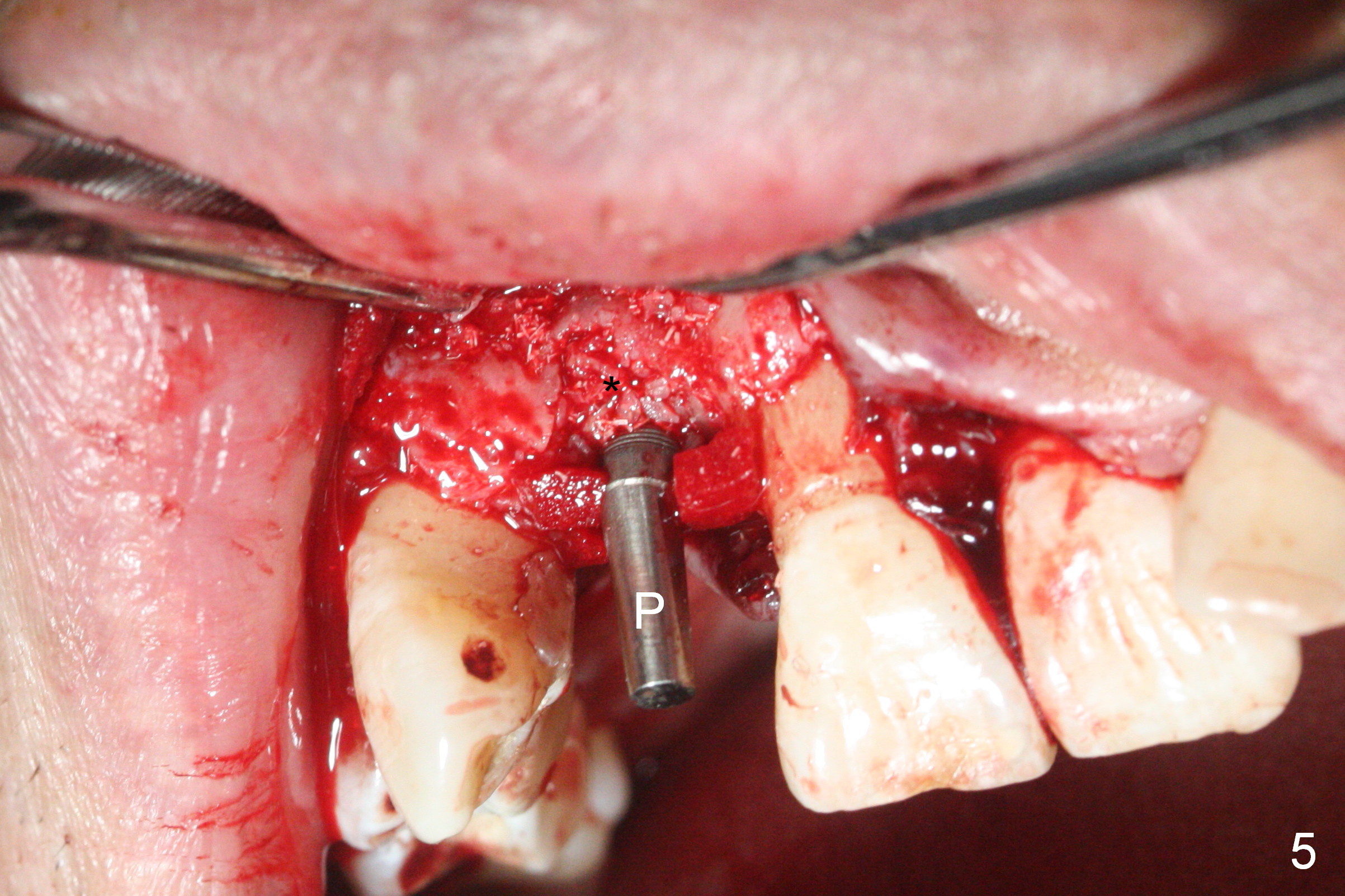
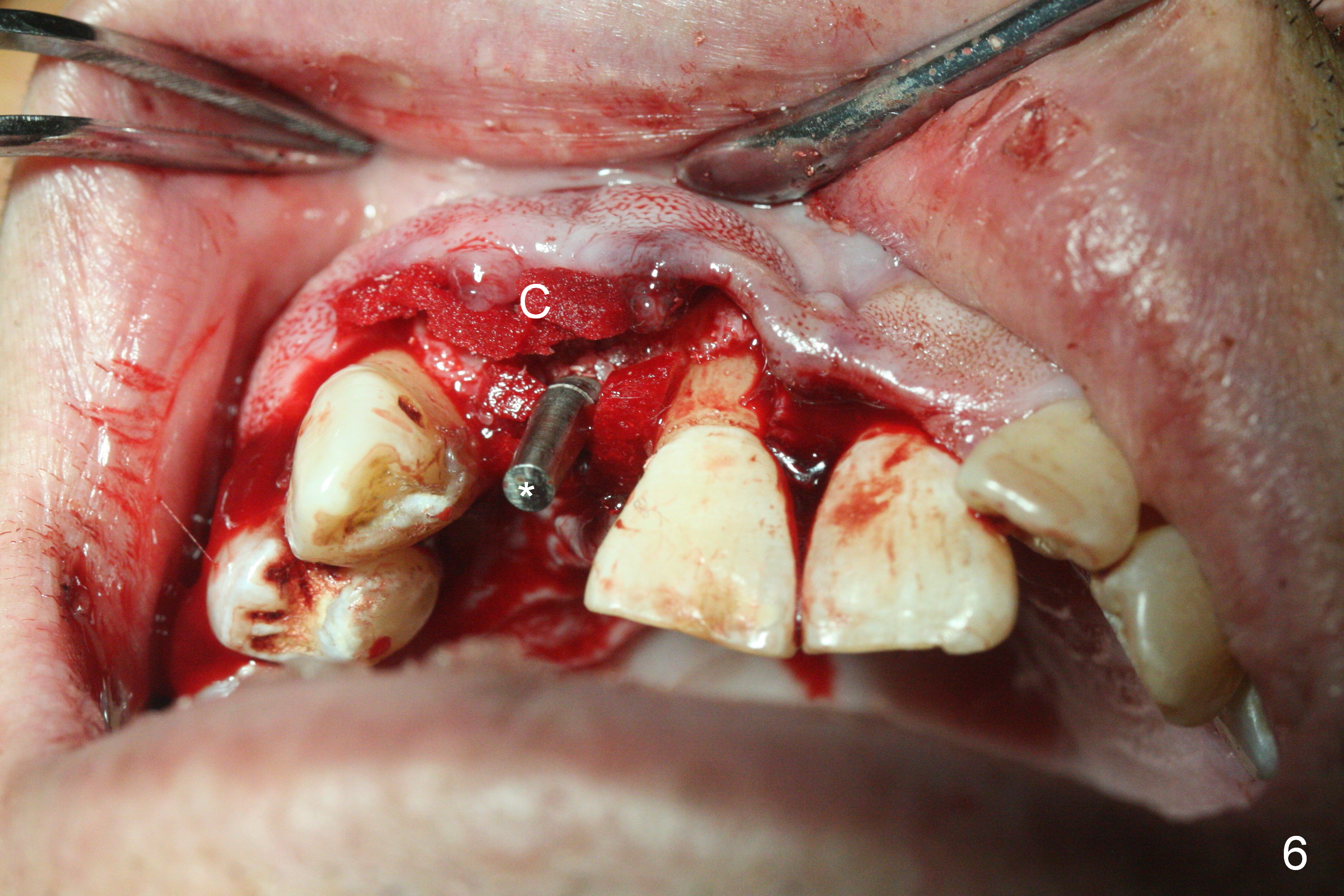
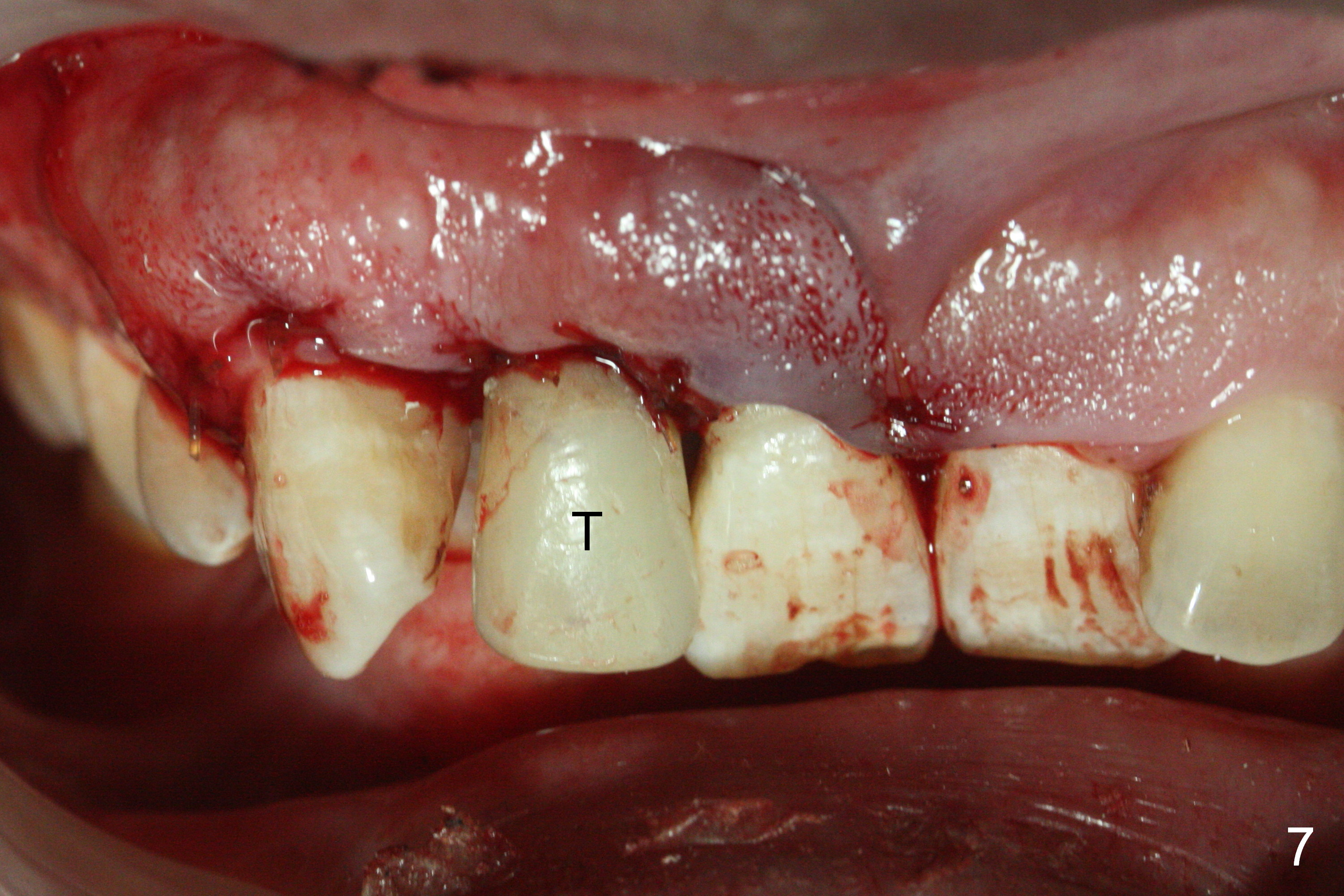
When the flaps are raised, the buccal plate is found to be perforated (Fig.2 *); osteotomy is being established in the narrow palatal wall (<). When a 3x17 mm (tissue-level) 15 ° 1-piece implant is placed (Fig.3,5 P), the incisal end of the implant is between the incisal edge of the central incisors and that of the tooth #10 (Fig.6) so that the temporary crown (Fig.7 T) is slightly buccal with sufficient palatal clearance with the opposing dentition.
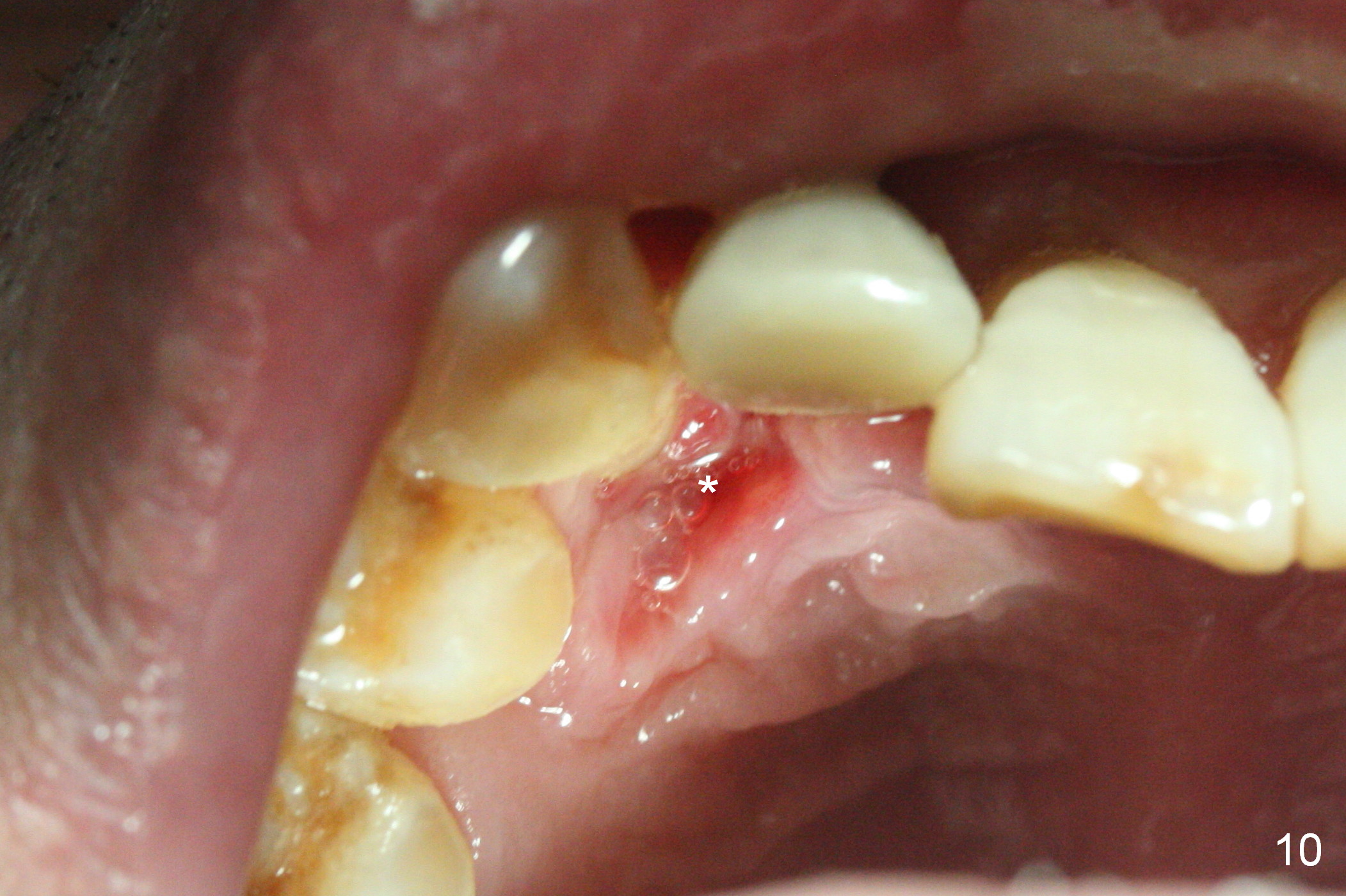
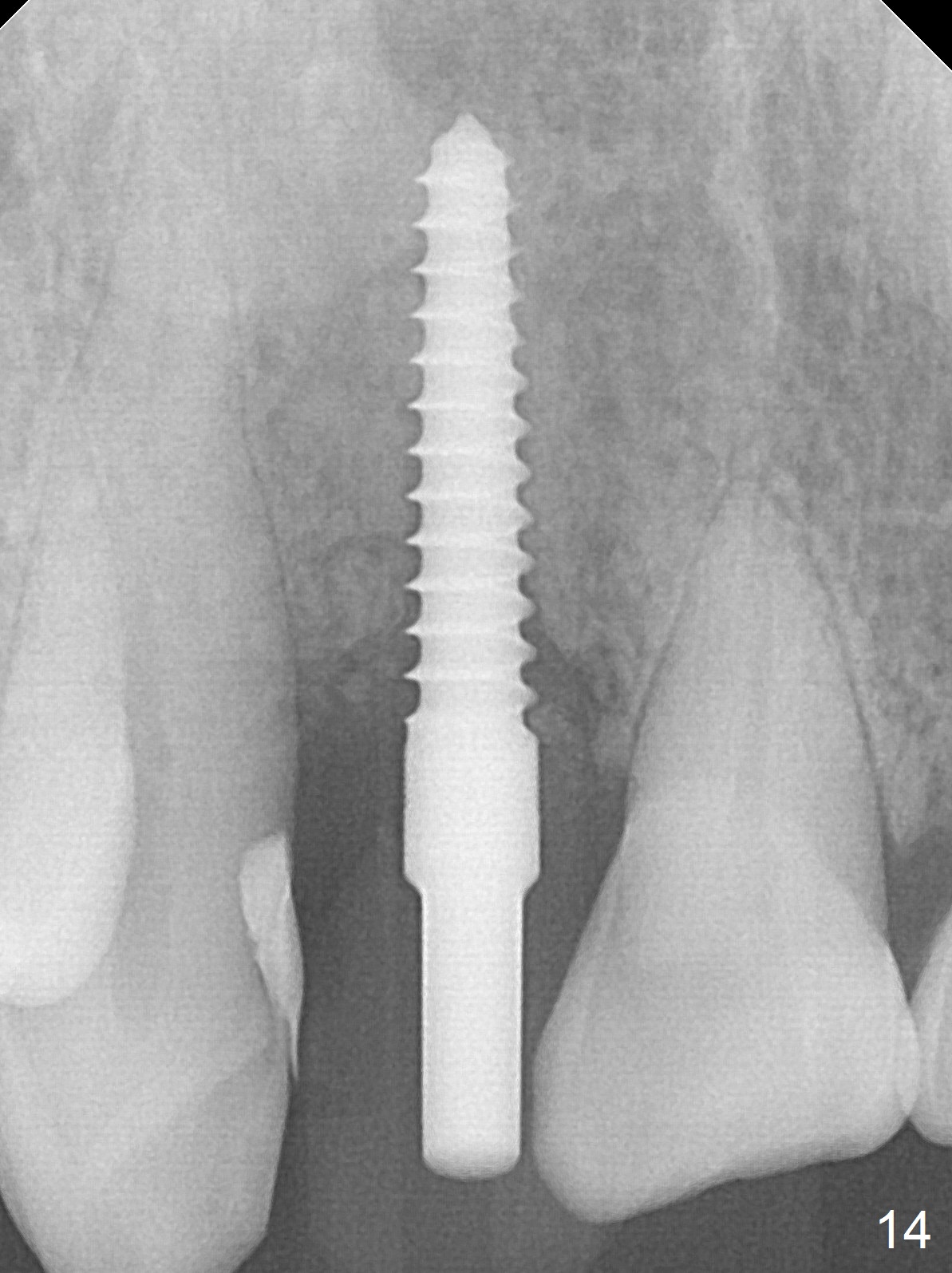
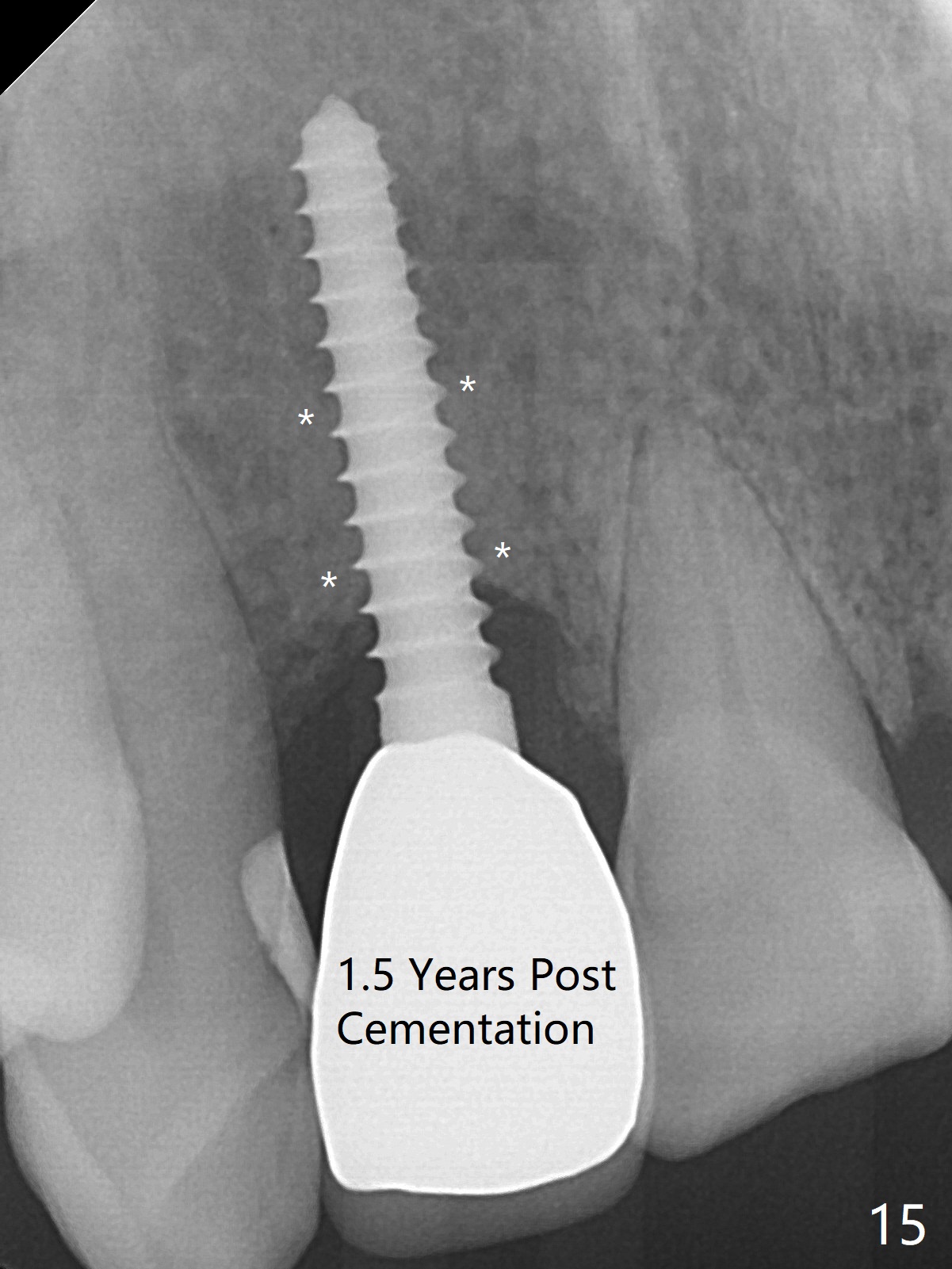
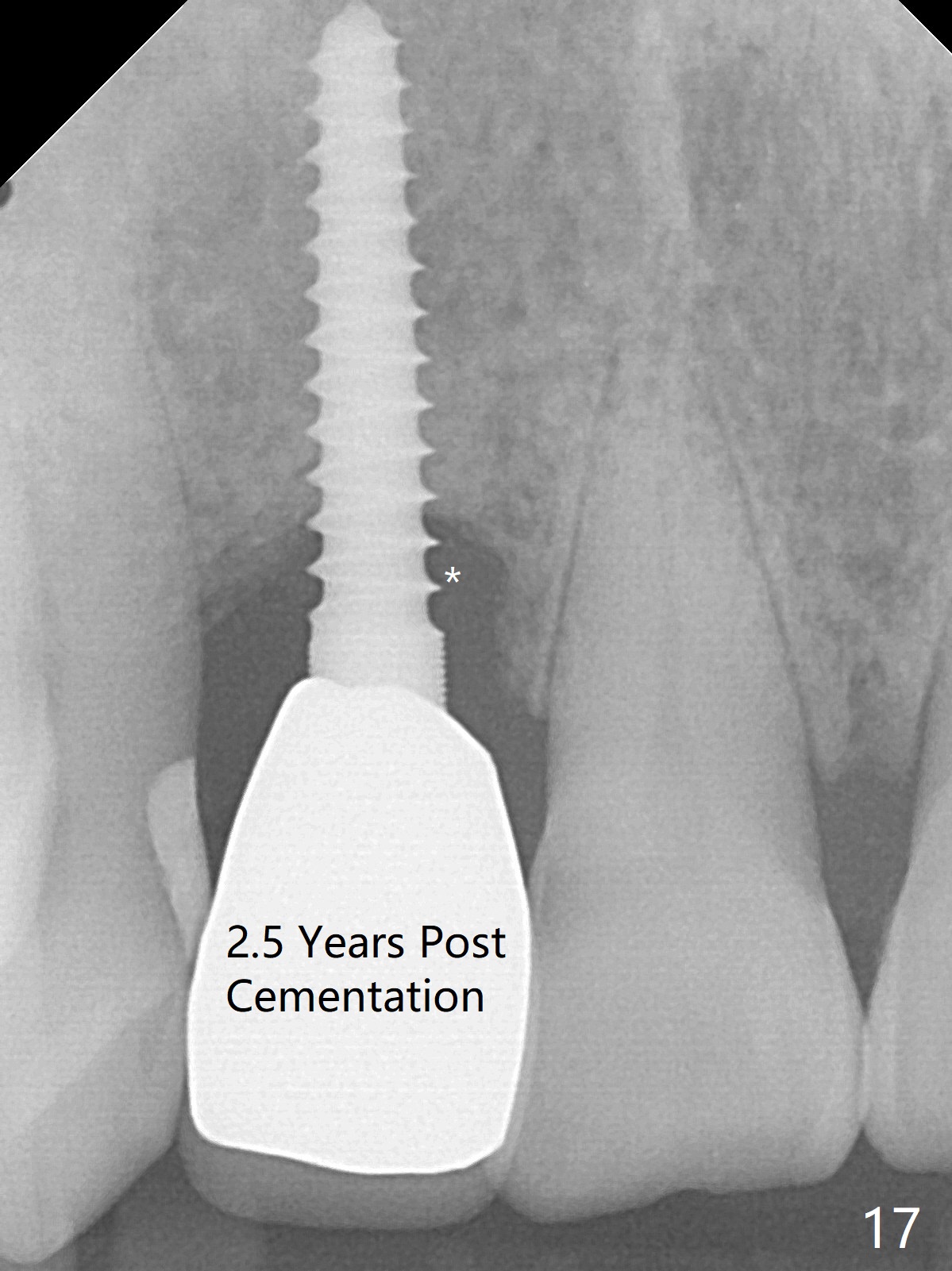
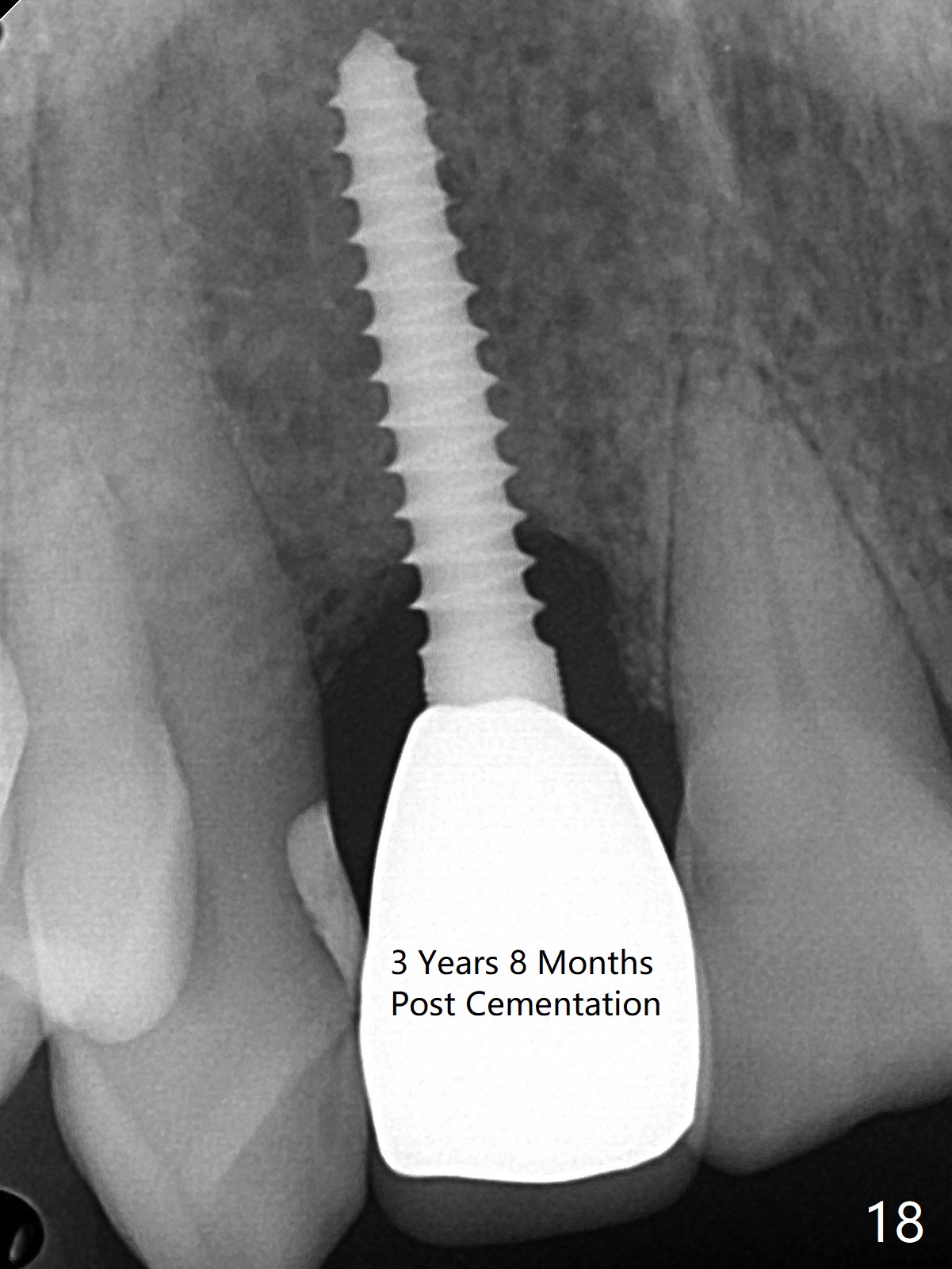
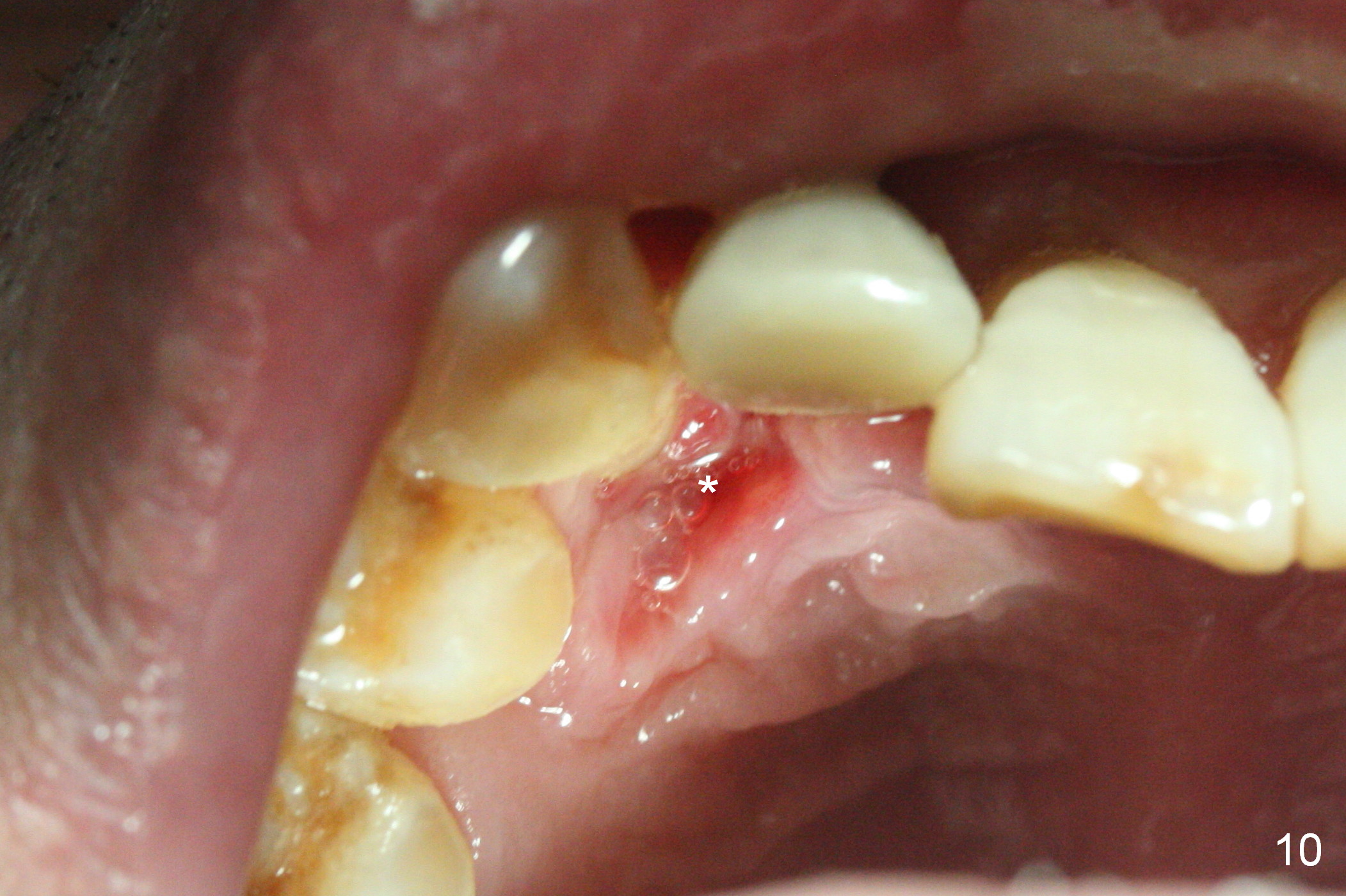
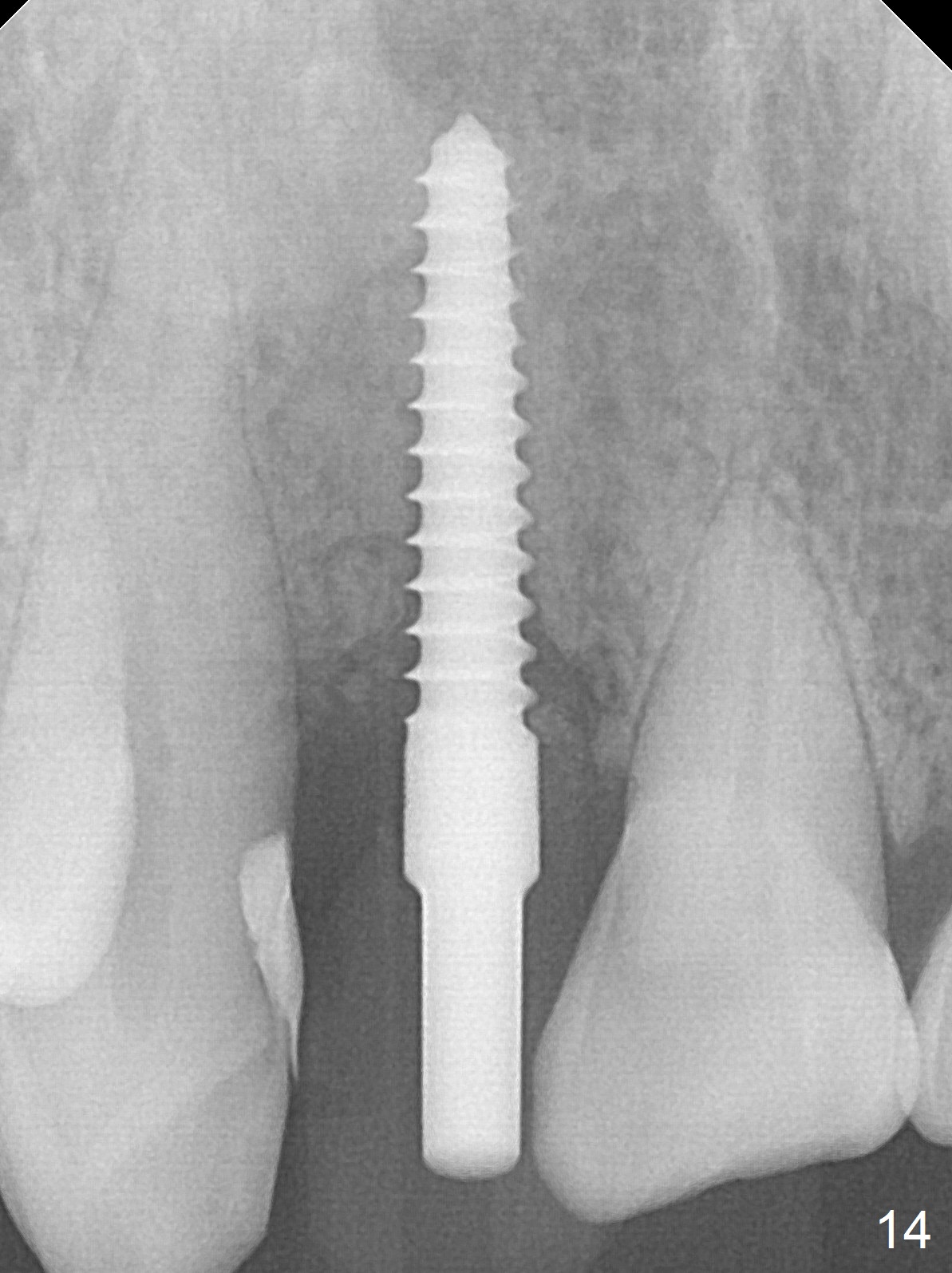
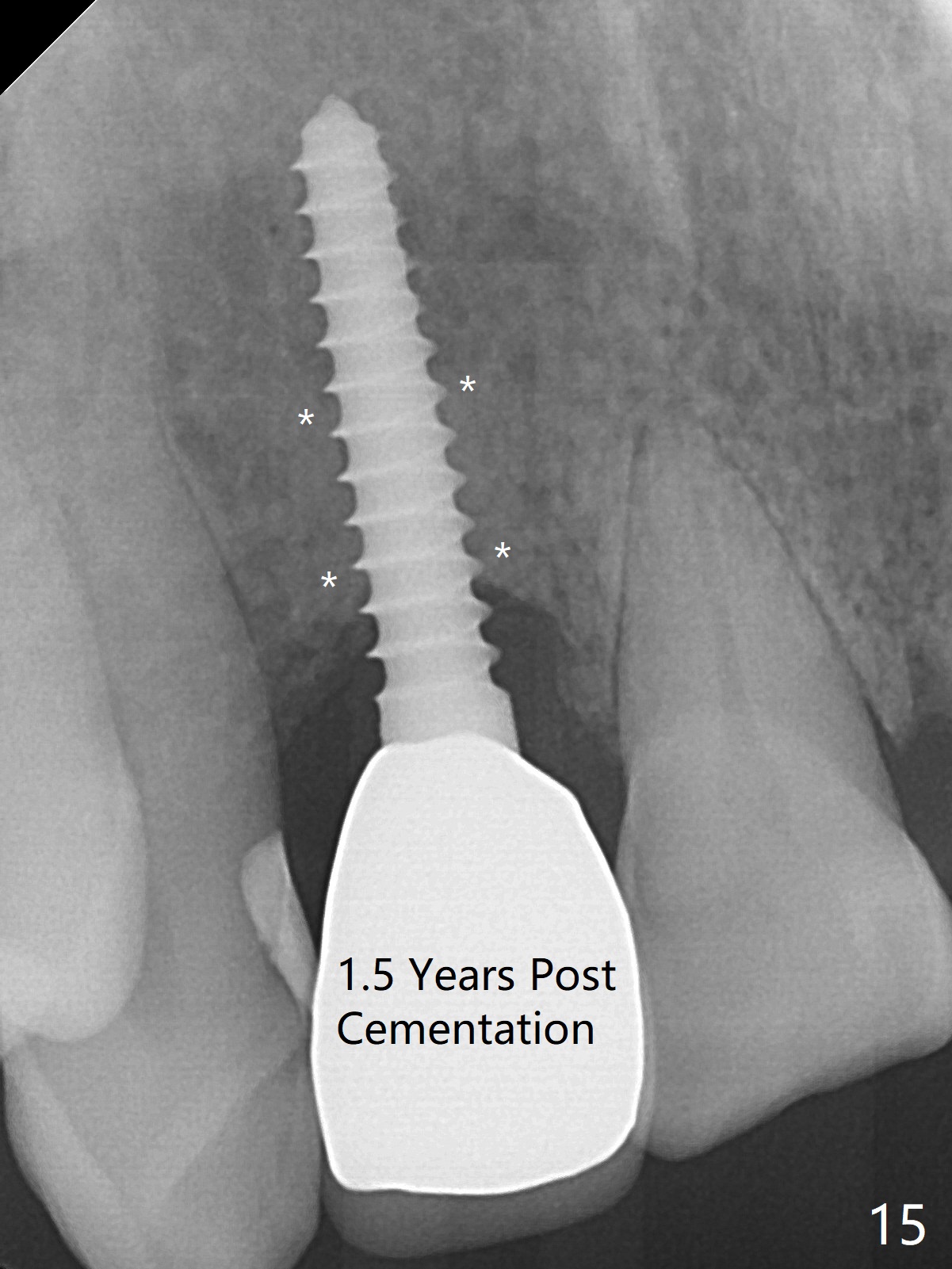
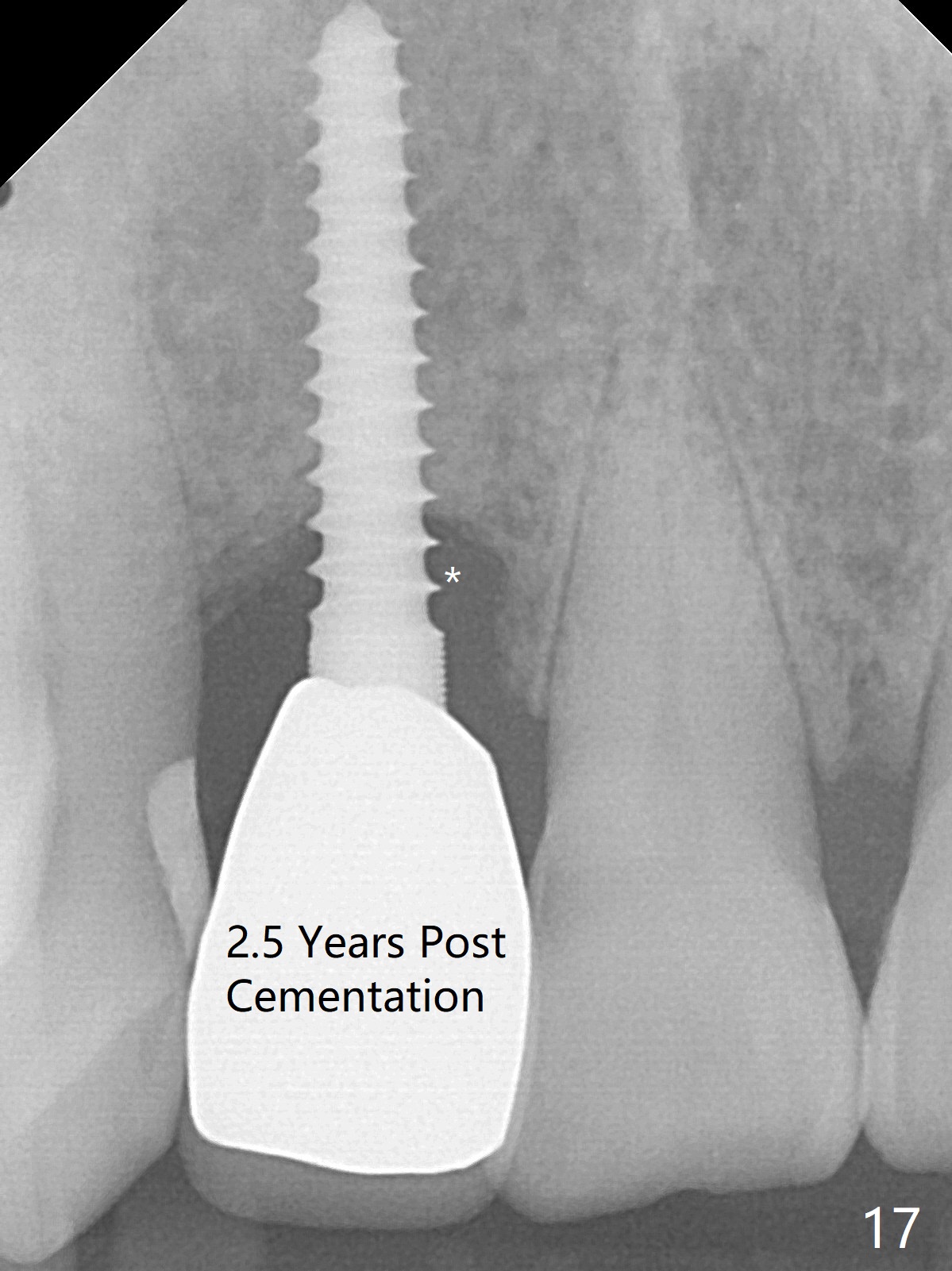
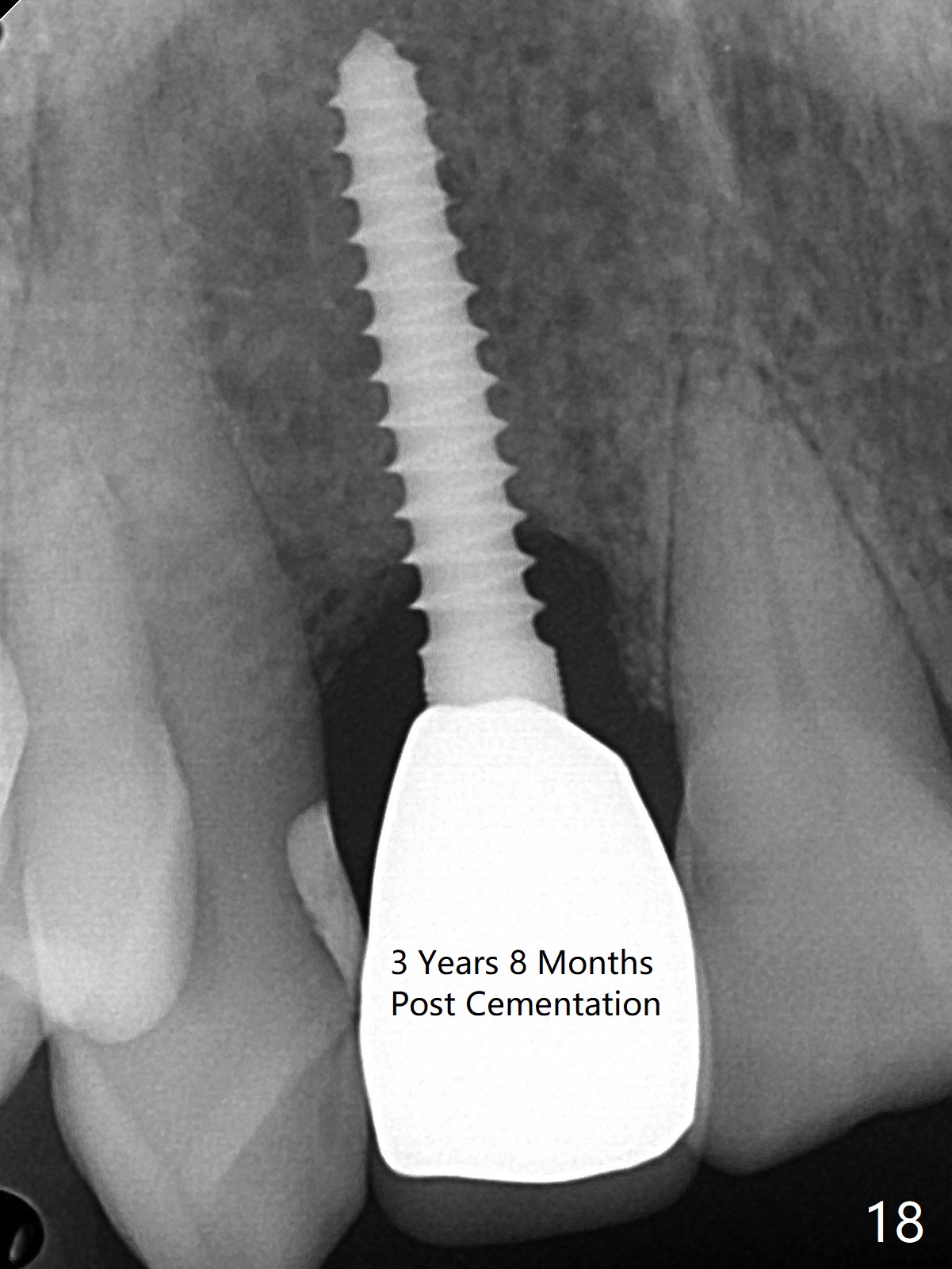
Sixteen days postop, the patient is doing fine, although the labial fistula has not disappeared (Fig.8 <). The detached distolabial papilla is healing (Fig.9 *) with mild bone graft exposure (^). The lacerated distopalatal papilla is also healing (Fig.10 *). These complications are related to flap surgery. The apical portion of the socket appears to have reduced 4 months postop (Fig.14). When the definitive restoration is delivered 5 months postop, there is gingival recession, including the distal of #8 (Fig.11 arrows, which is expected to improve over time) due to flap surgery. The labial plate collapse is minimal (Fig.12 *), while the palatal laceration (Fig.10) has healed (Fig.13). When the patient returns 1.5 years post cementation, there is increased bone density next to the coronal portion of the implant, equivalent to the bone graft (Fig.15 *). The fistula is absent (Fig.16). The crestal bone loss remains 2.5 years post cementation (Fig.17 *), although there is no sign of periimplantitis (magnification). Oral hygiene is poor. There is no change in the soft (gingival recession; data not shown) or hard tissues 3 years 8 months post cementation (Fig.18).
Return to
Upper
Incisor Immediate Implant,
IBS
Xin Wei, DDS, PhD, MS 1st edition 01/26/2017, last revision 03/22/2021