




 |
 |
 |
|||
 |
 |
 |
 |
 |
 |
 |
 |
||||
Change Osteotomy Position with Lindamann Bur
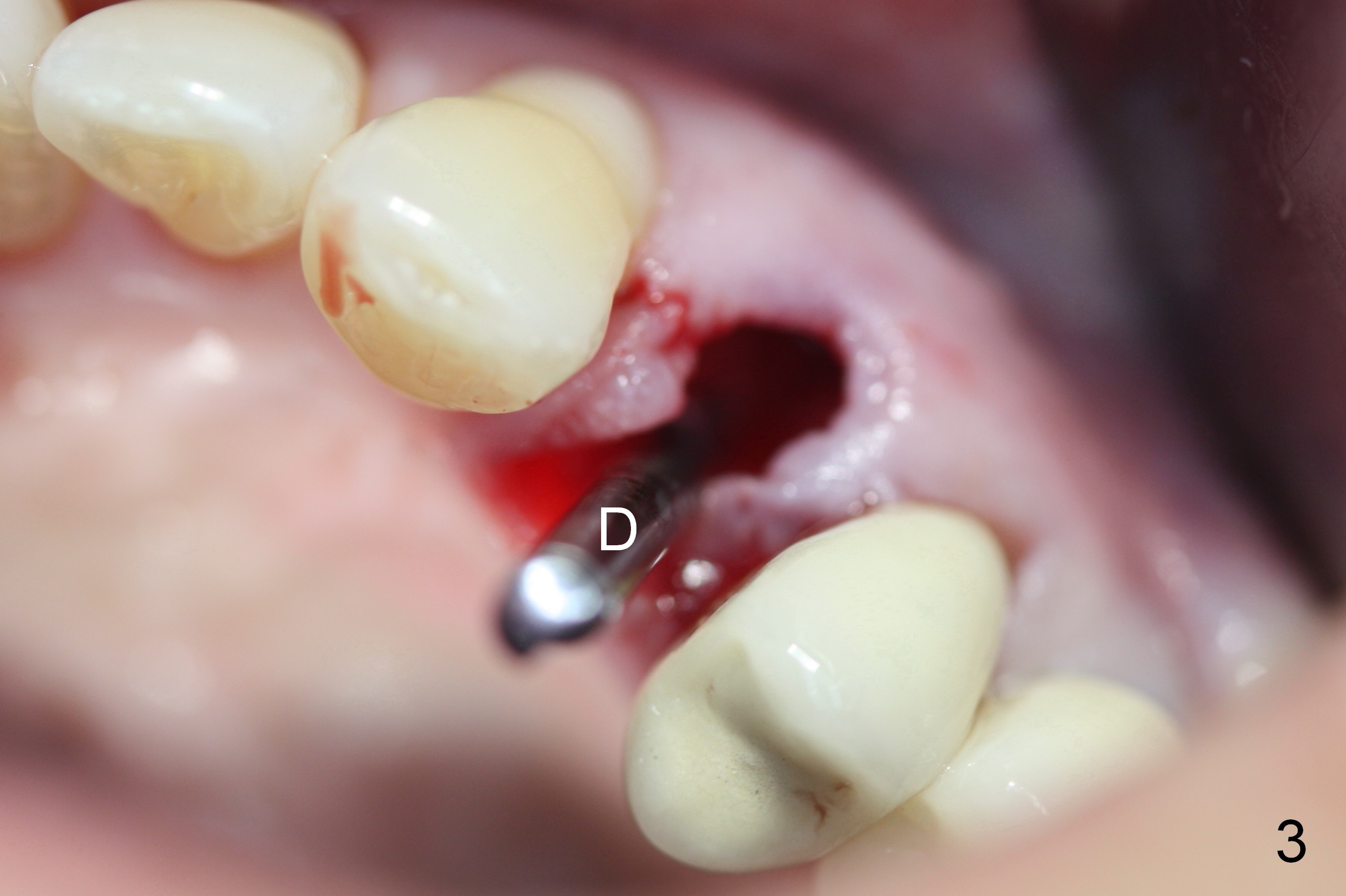
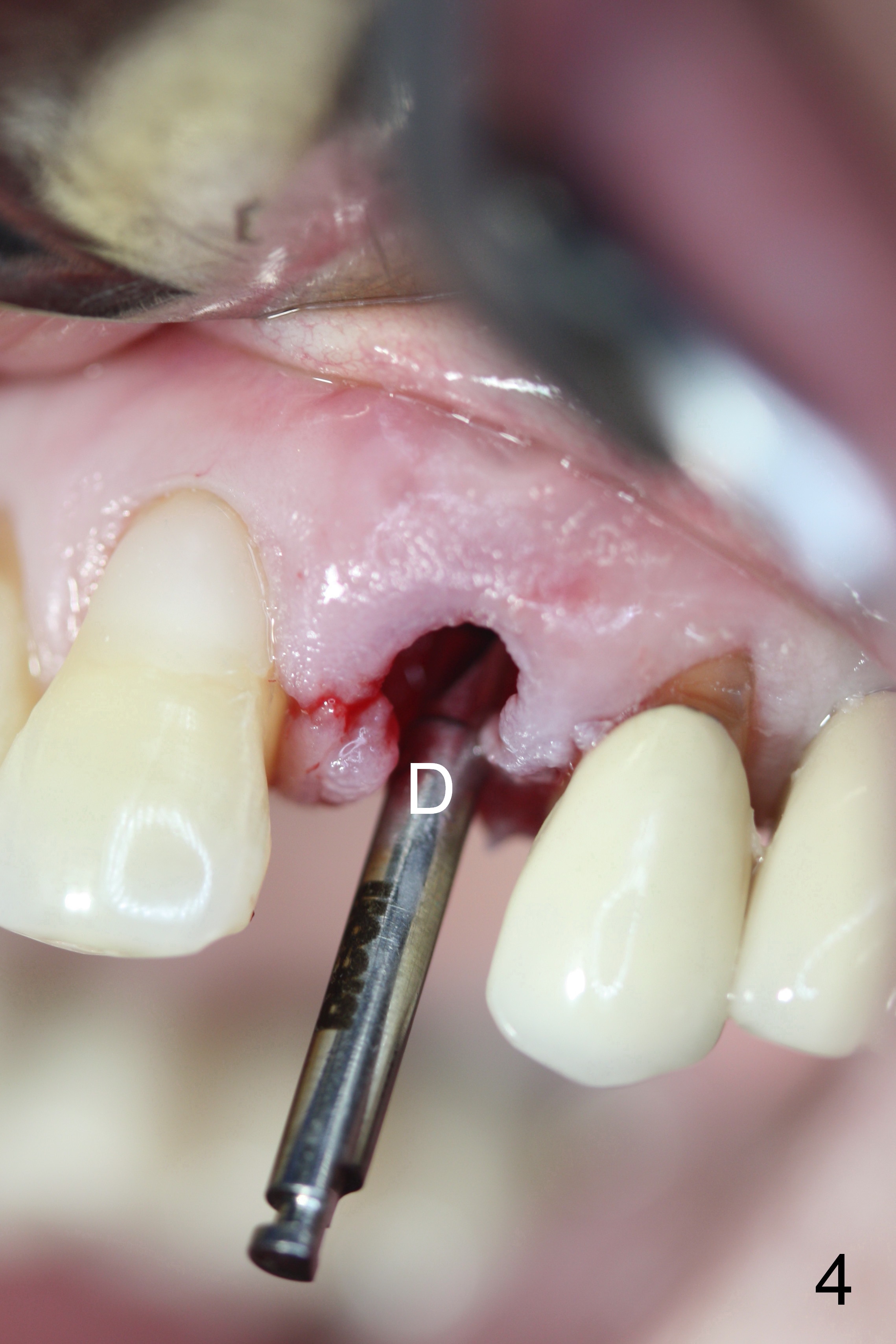
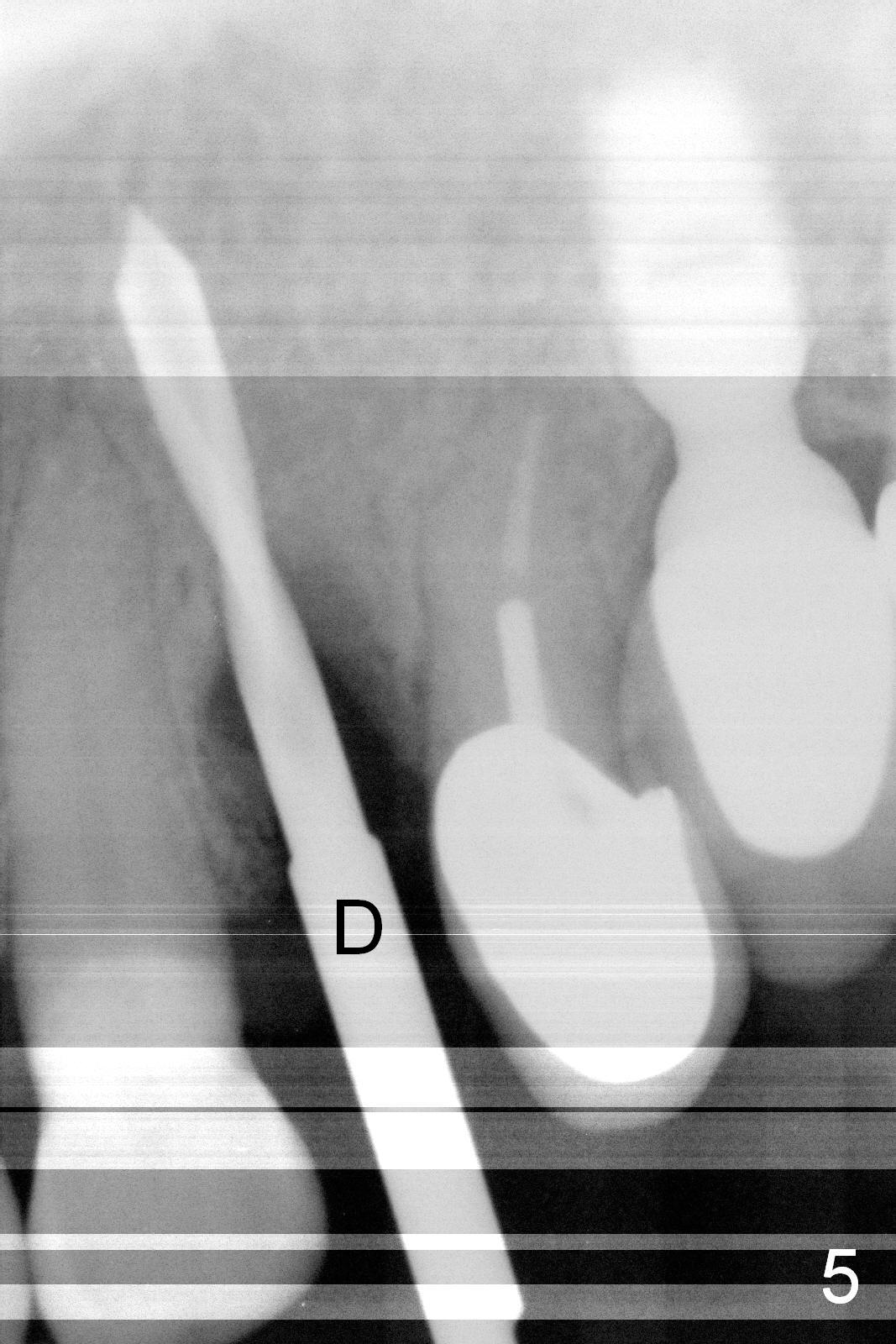
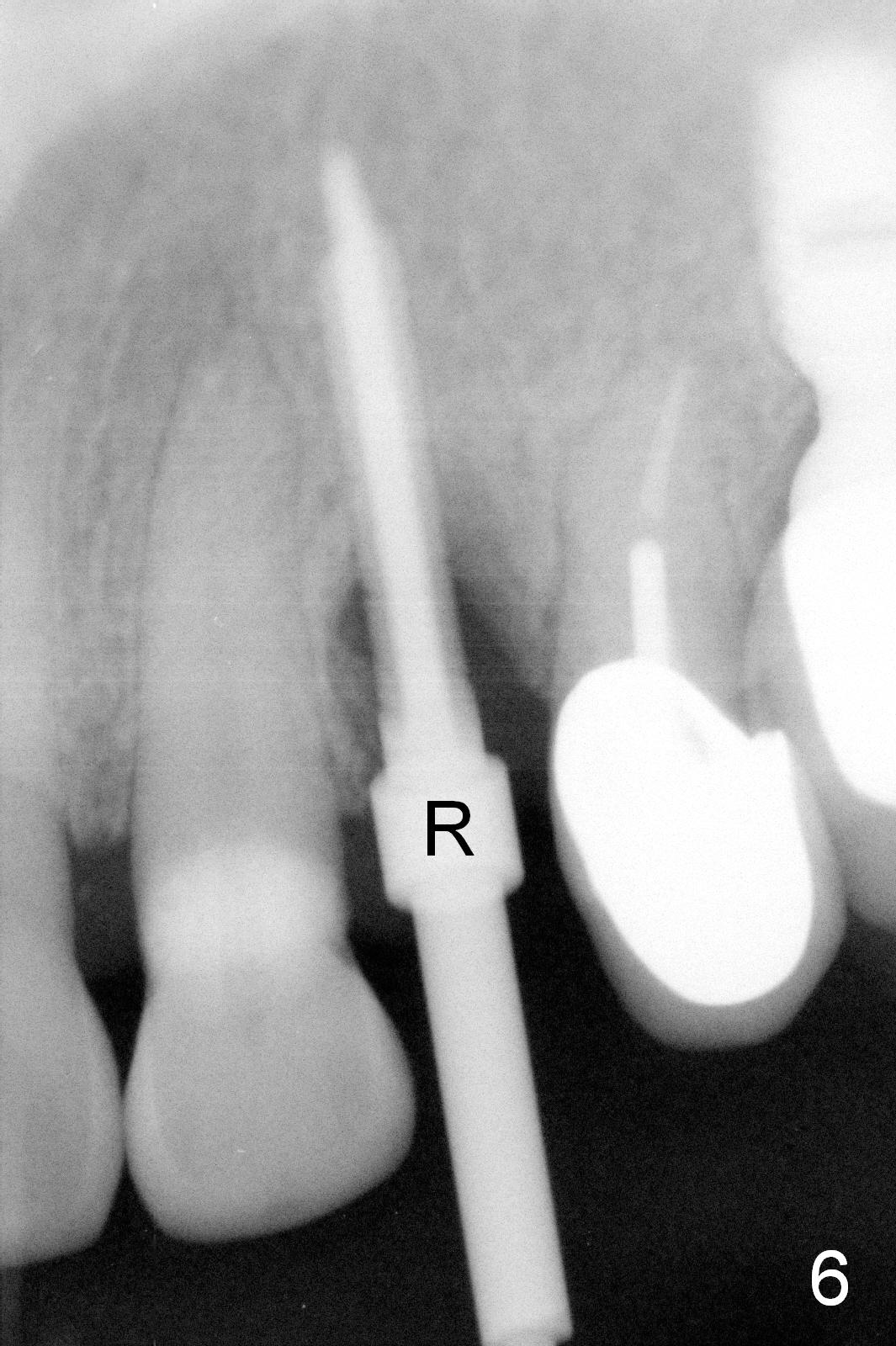
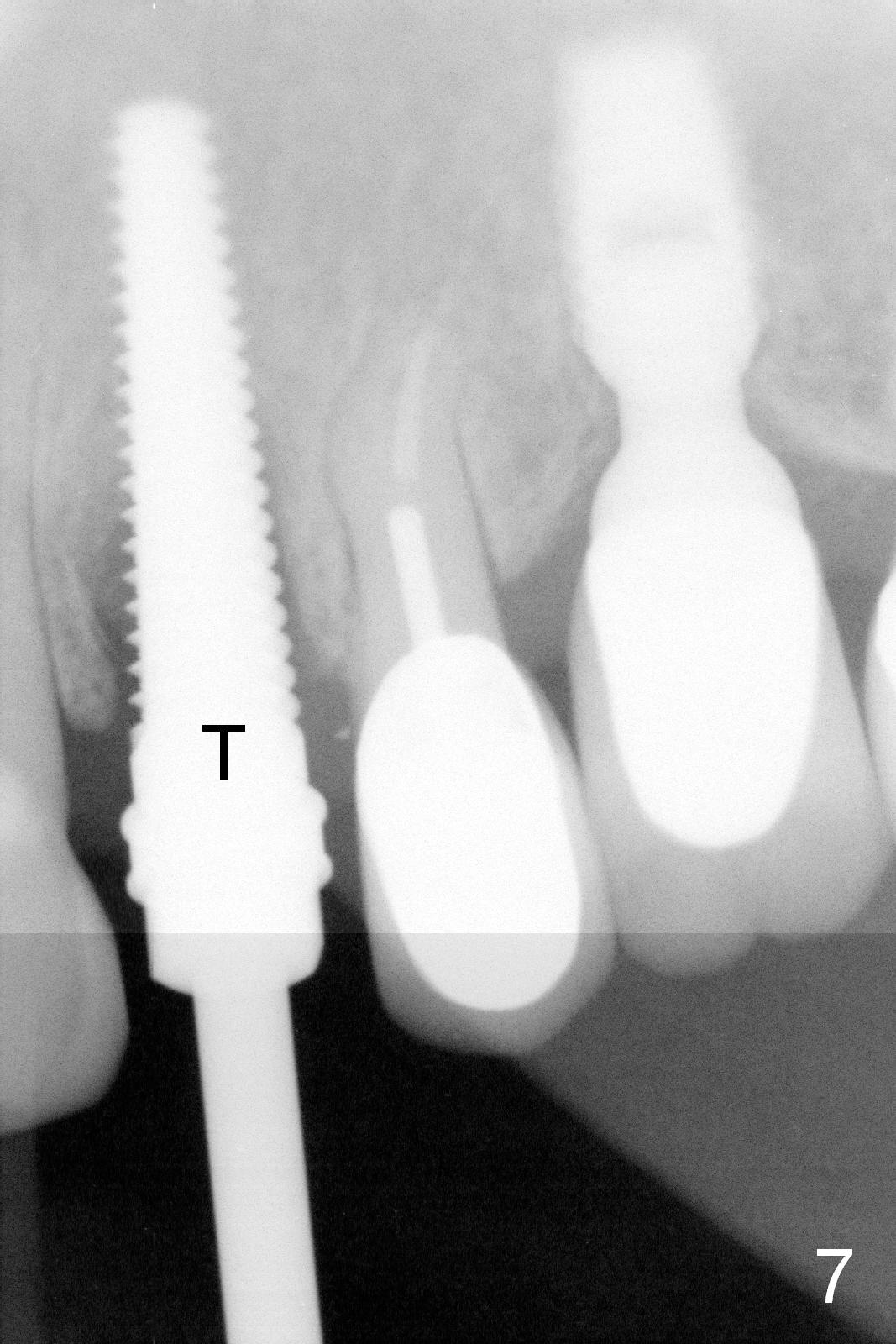
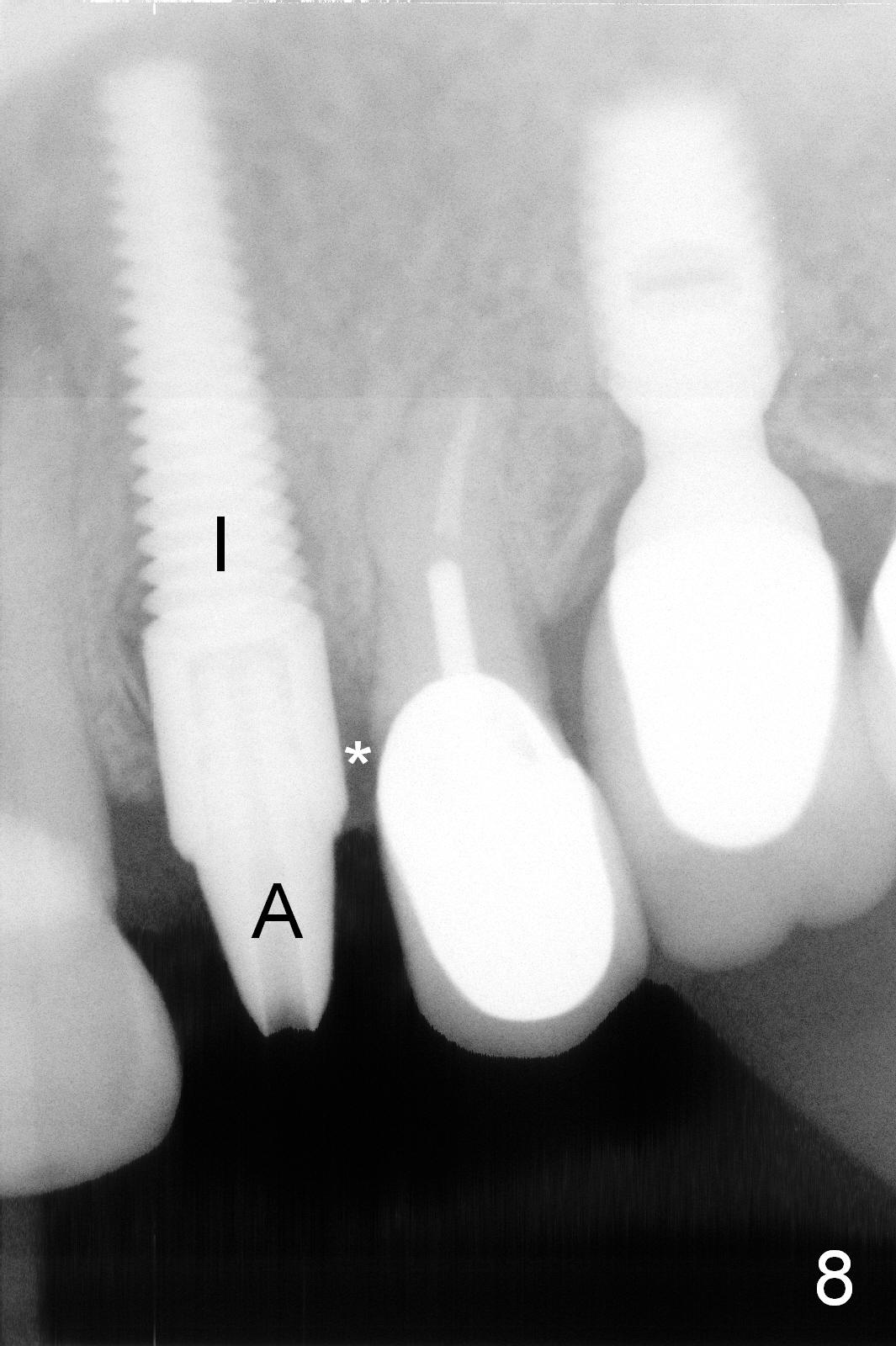
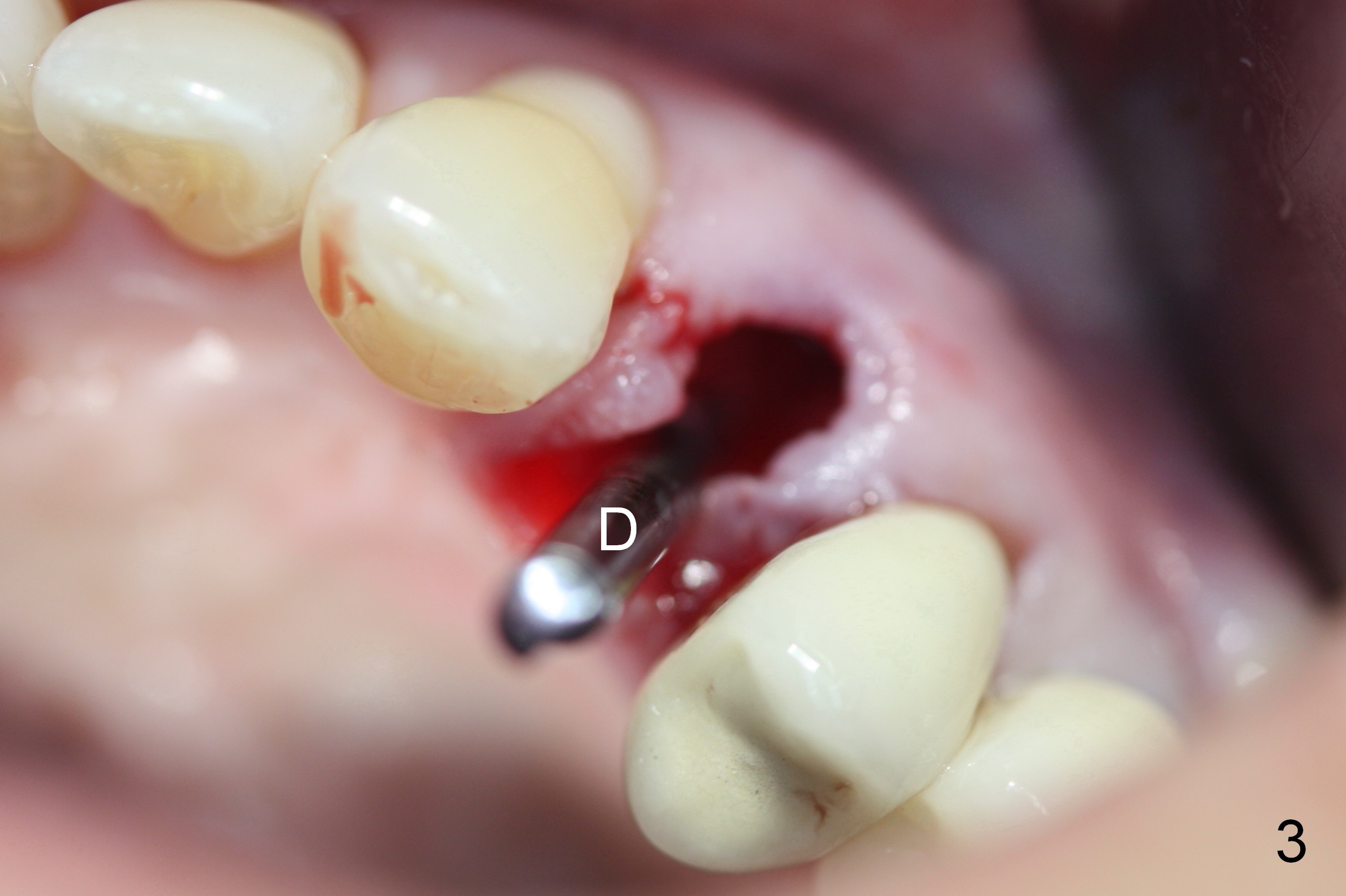
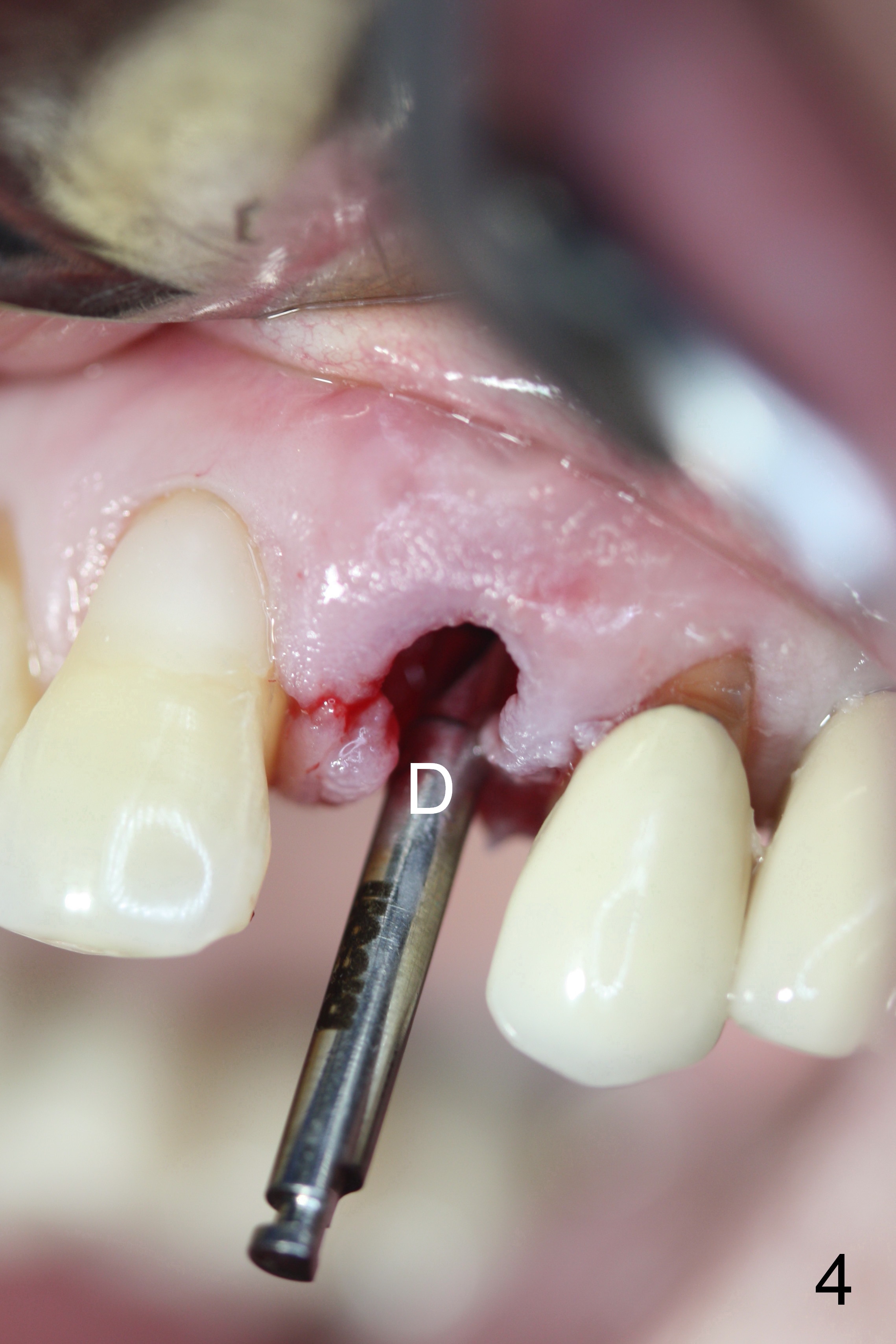
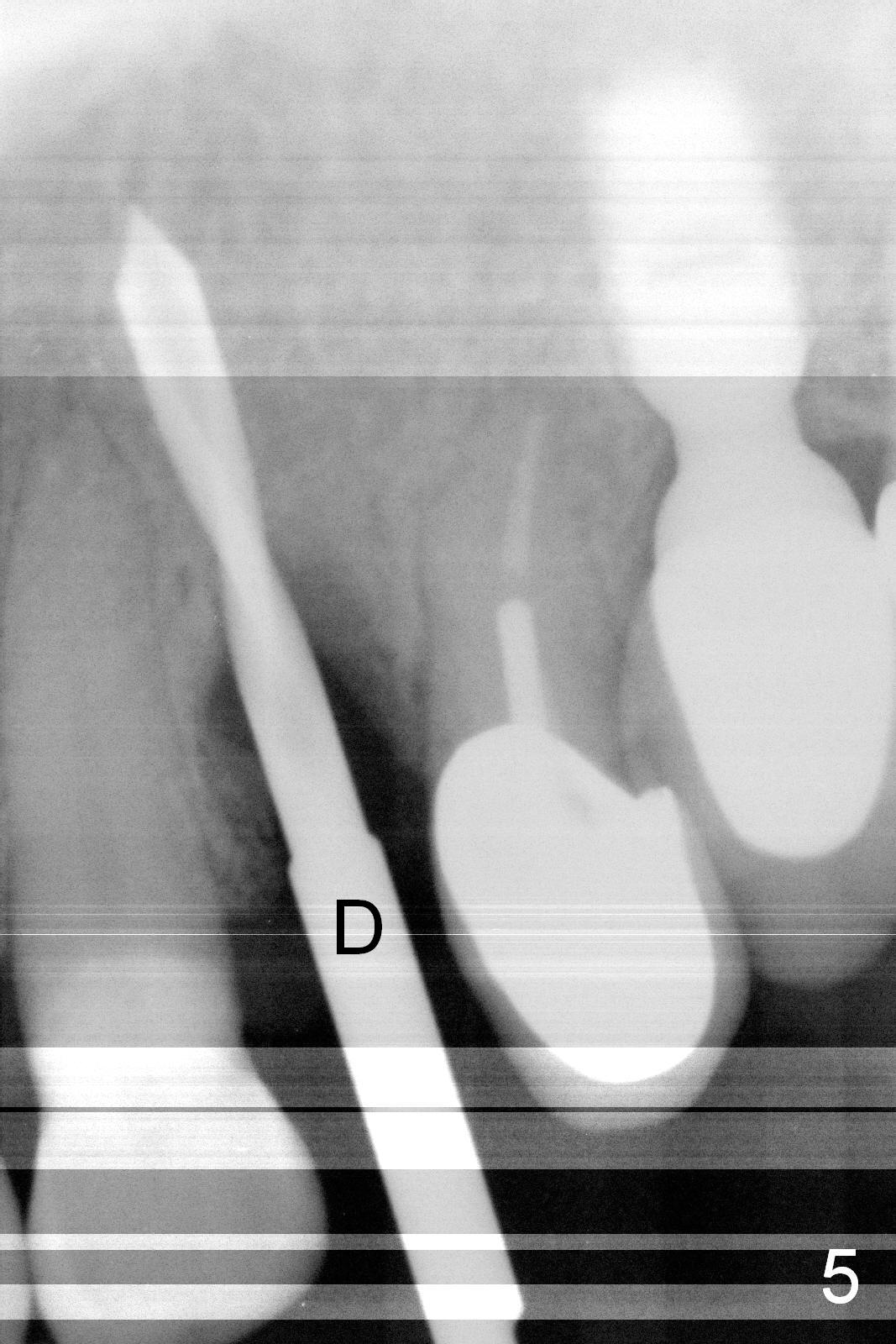
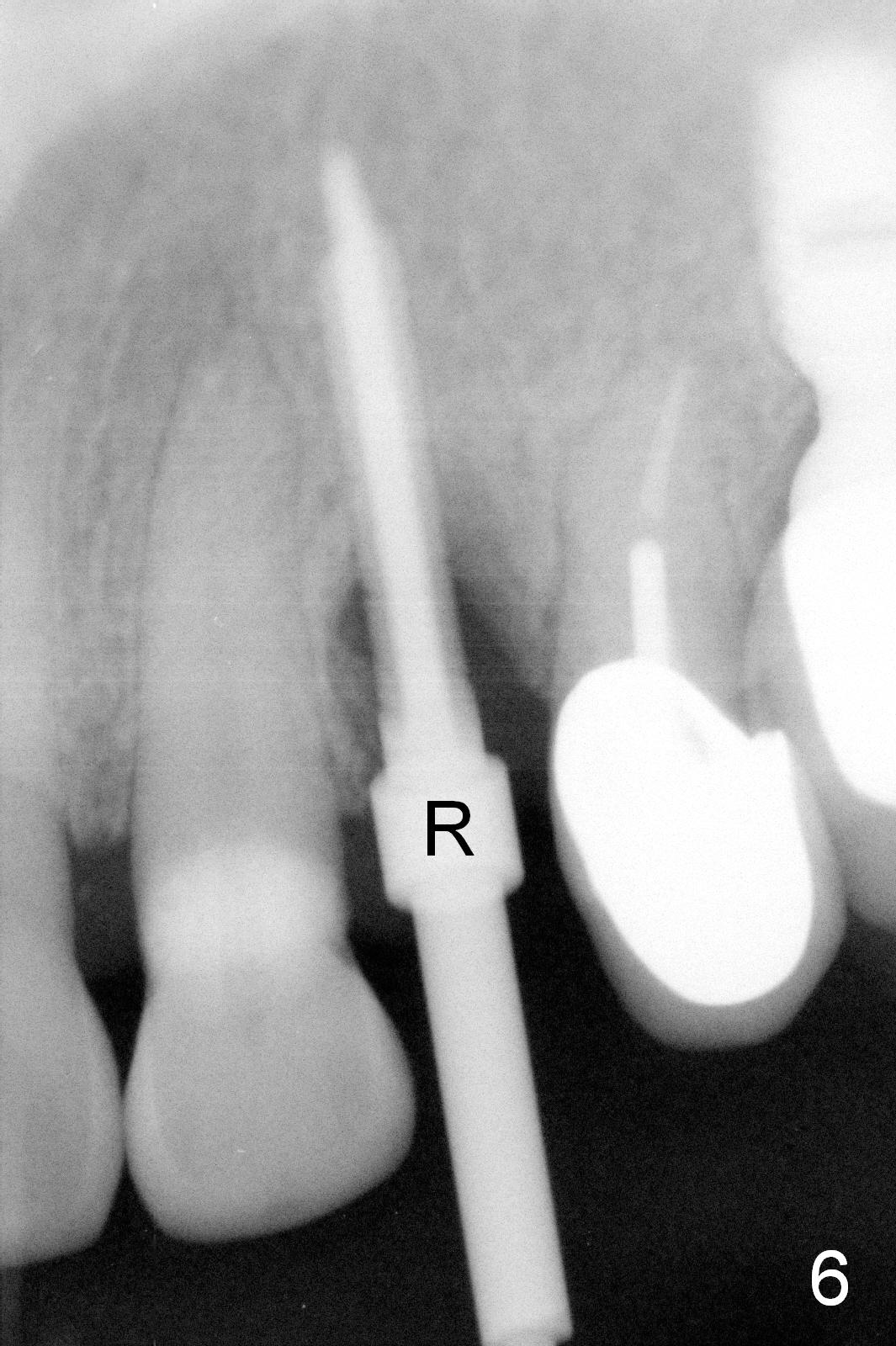
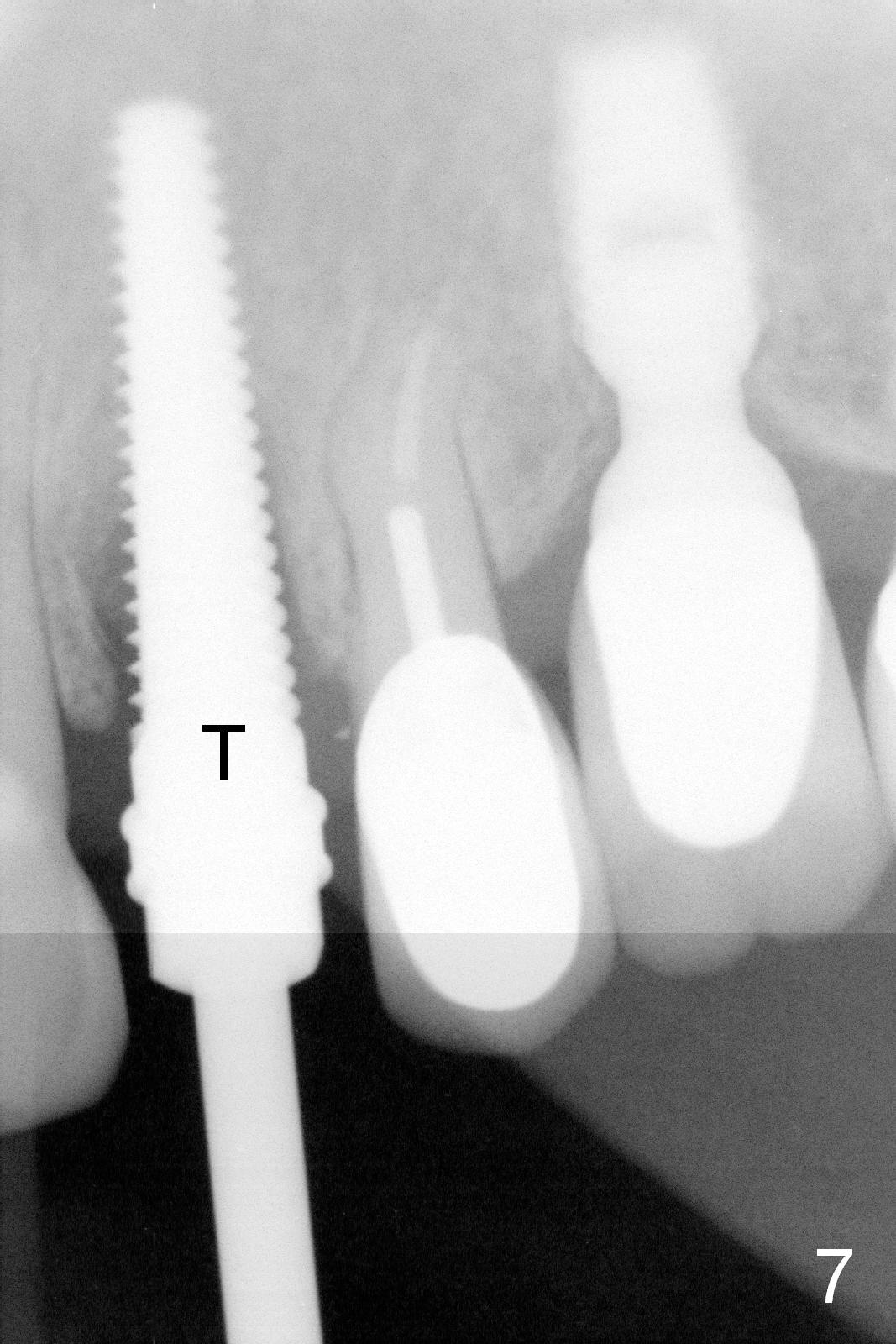
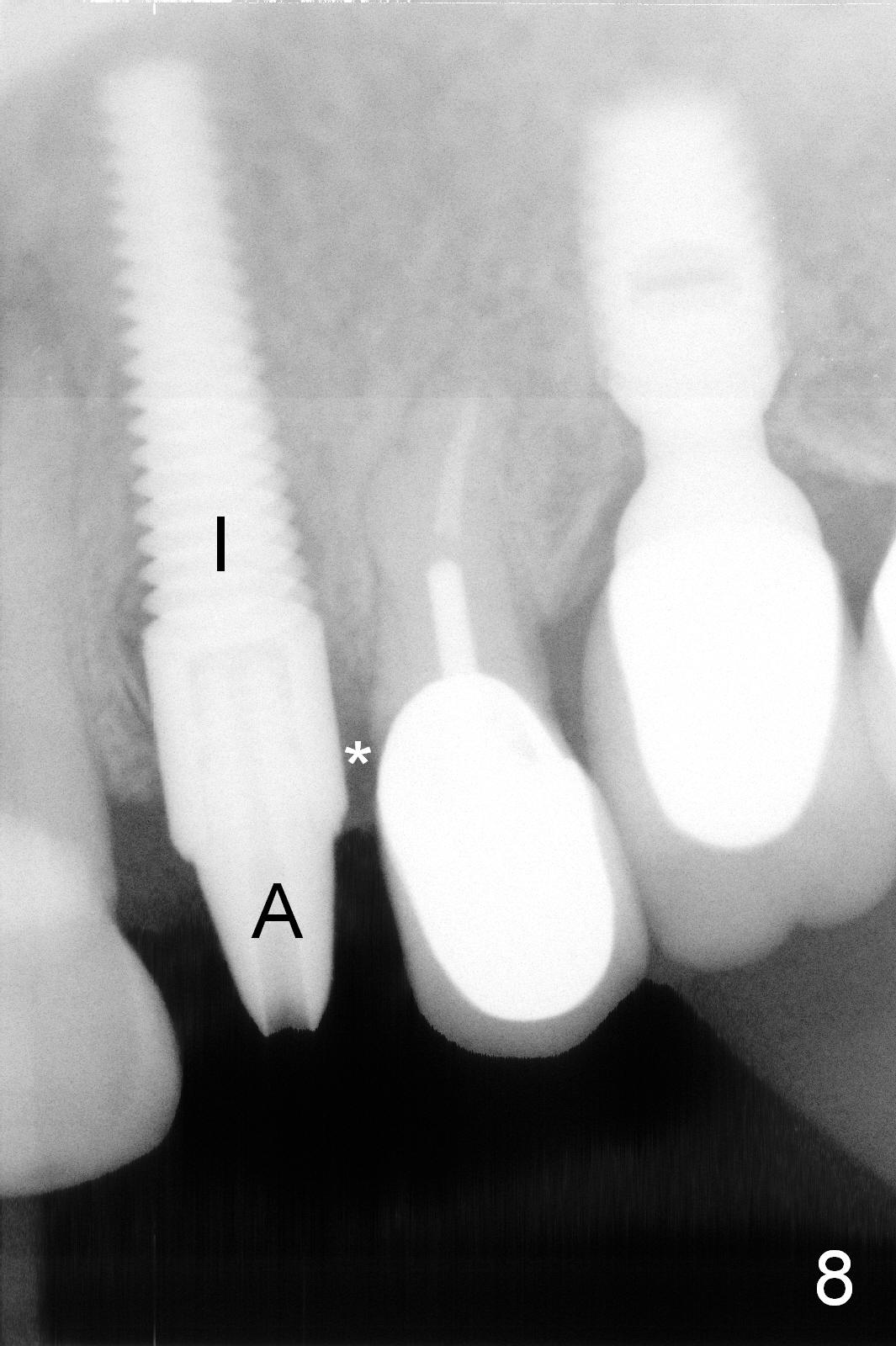
Root fracture is evident clinically (Fig.1 arrowheads). When the root is extracted, the apical buccal plate is perforated (Fig.2, a curette against the buccal socket wall). After thorough debridement of granulation tissue from the socket, osteotomy is initiated with a 2 mm pilot drill in the palatal wall (Fig.3, 20 mm deep, bone density felt apparently low), but the trajectory is off (Fig.4,5). Effort is exerted to change the trajectory with the same drill and a 2.5 mm reamer without effect (Fig.6: R, 20 mm deep). Then a Lindemann bur is used to move the osteotomy distally, followed by a 3.0 mm reamer, 3 mm less than the intended depth. When a 4.5x20 mm tap is inserted 17 mm deep, the trajectory appears to have been corrected (Fig.7 T). All of osteotomy steps mentioned above are under prep, leading to high insertion torque of a 4.5x20 mm tissue-level implant (Fig.8: I, >60 Ncm). A 3.5x5 mm abutment is placed immediately (A) for an immediate provisional. After placement of Osteo Tape (buccally) and allograft/Osteogen in the remaining socket (Fig.8,9 *), the provisional is cemented temporarily. The provisional stays in place for the next 5 months (Fig.10 *), while a peri-implant space is closing (Fig.10 <, as compared to Fig.8). There is no buccal plate collapse; the socket gap heals (Fig.11 *, compare to Fig.9 *). Fifteen months post cementation, the patient returns for follow up. Exam shows possible root fracture at #13.
Return to Upper Bicuspid Immediate Implant,
Posterior Immediate Provisional
Xin Wei, DDS, PhD, MS 1st edition 07/15/2015, last revision 07/08/2017