

 |
 |
 |
 |
 |
 |
 |
 |
  |
Unintentional Sinus Lift M
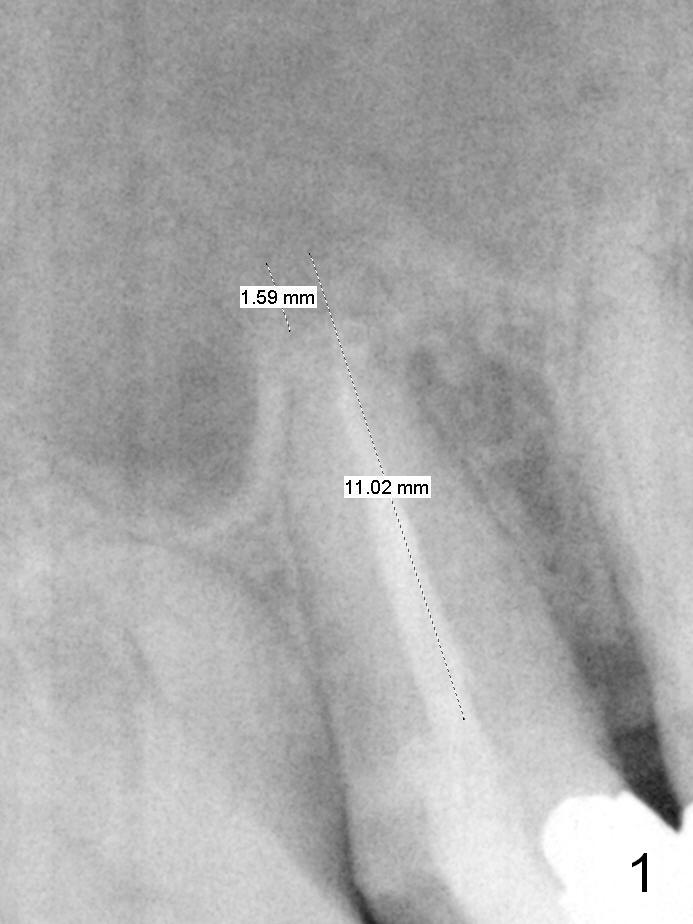
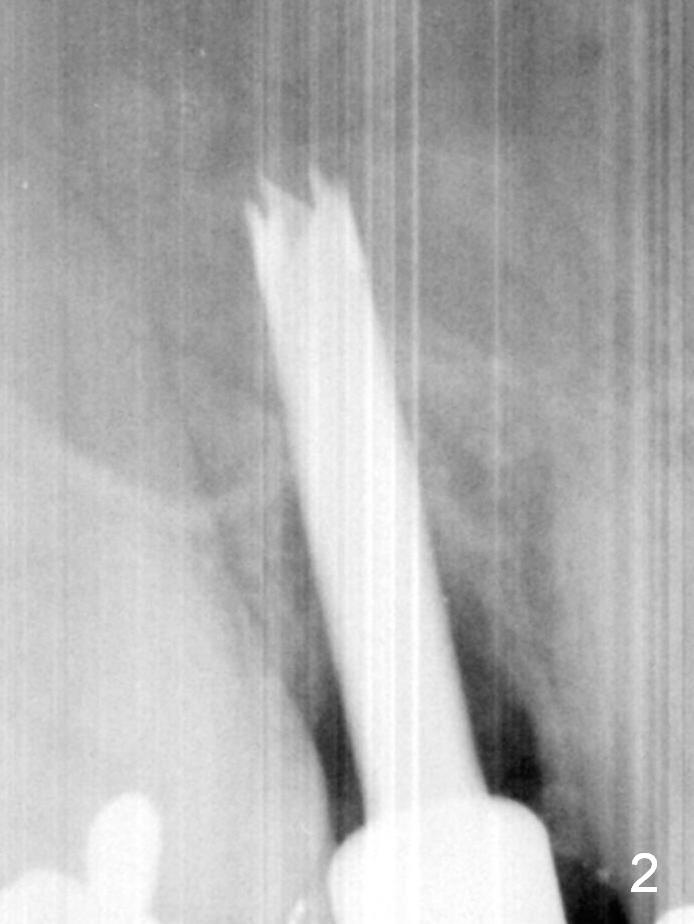
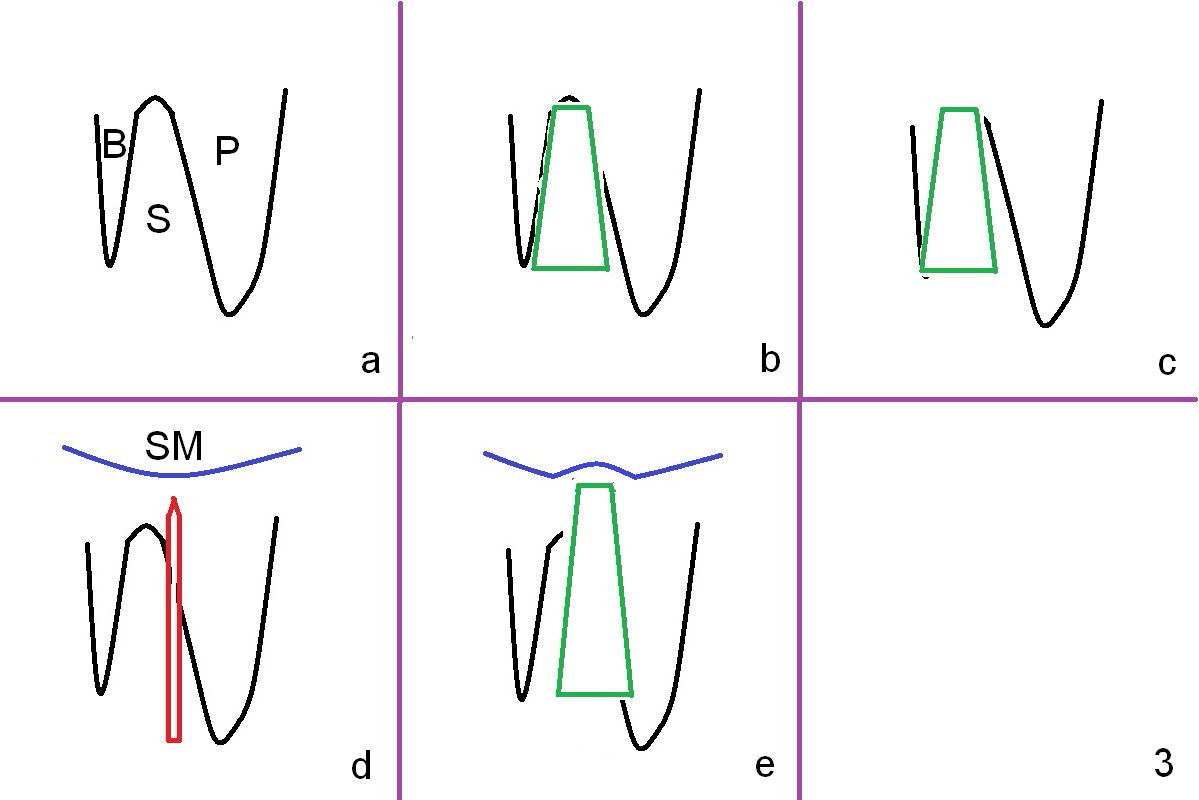
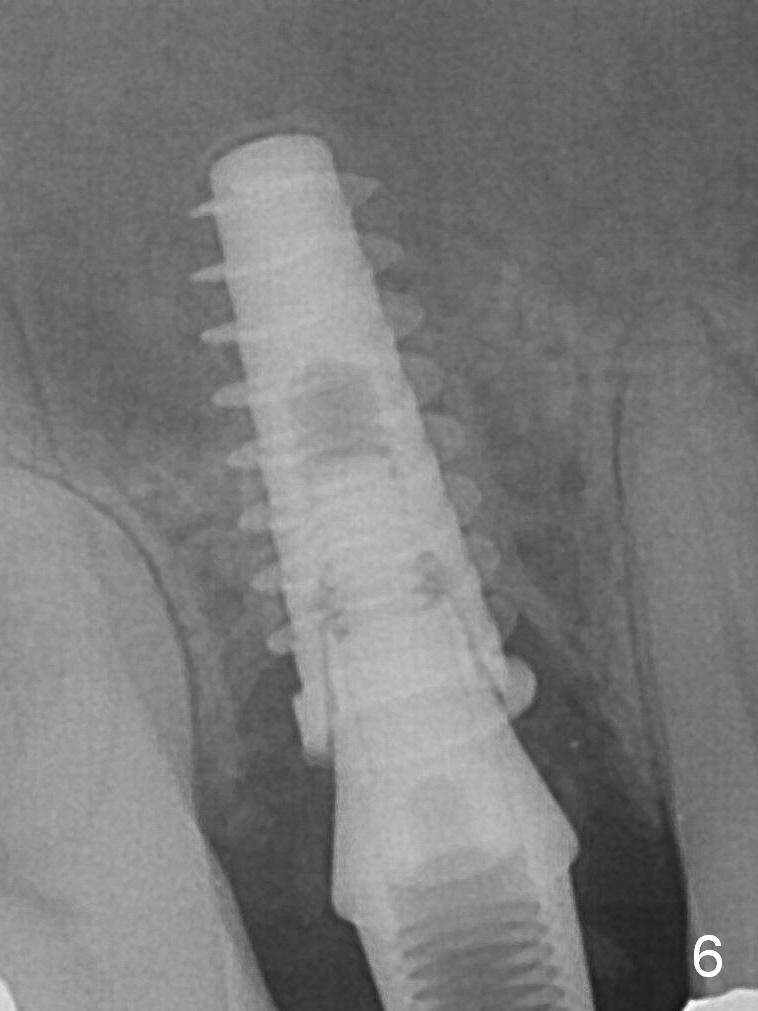
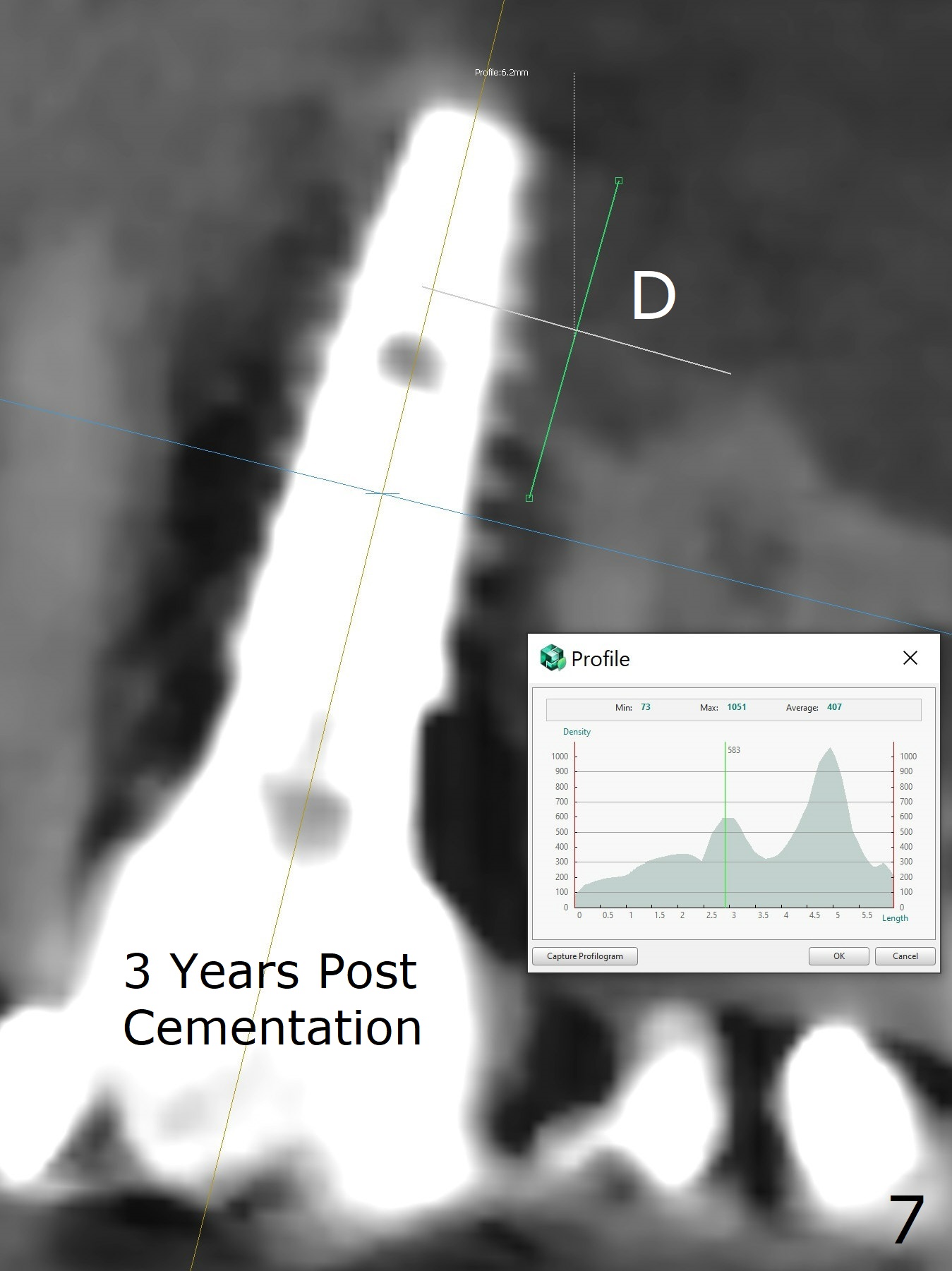
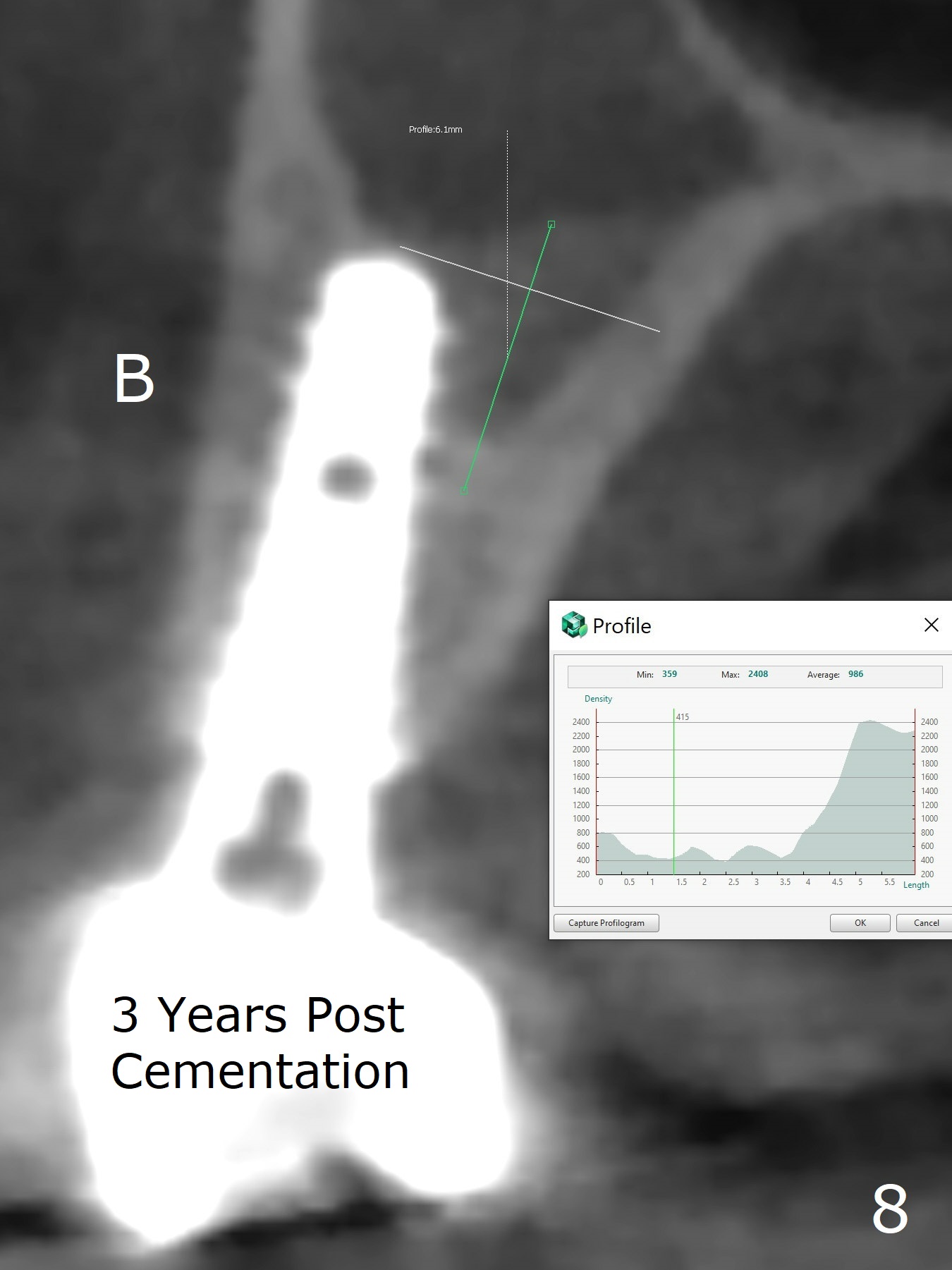
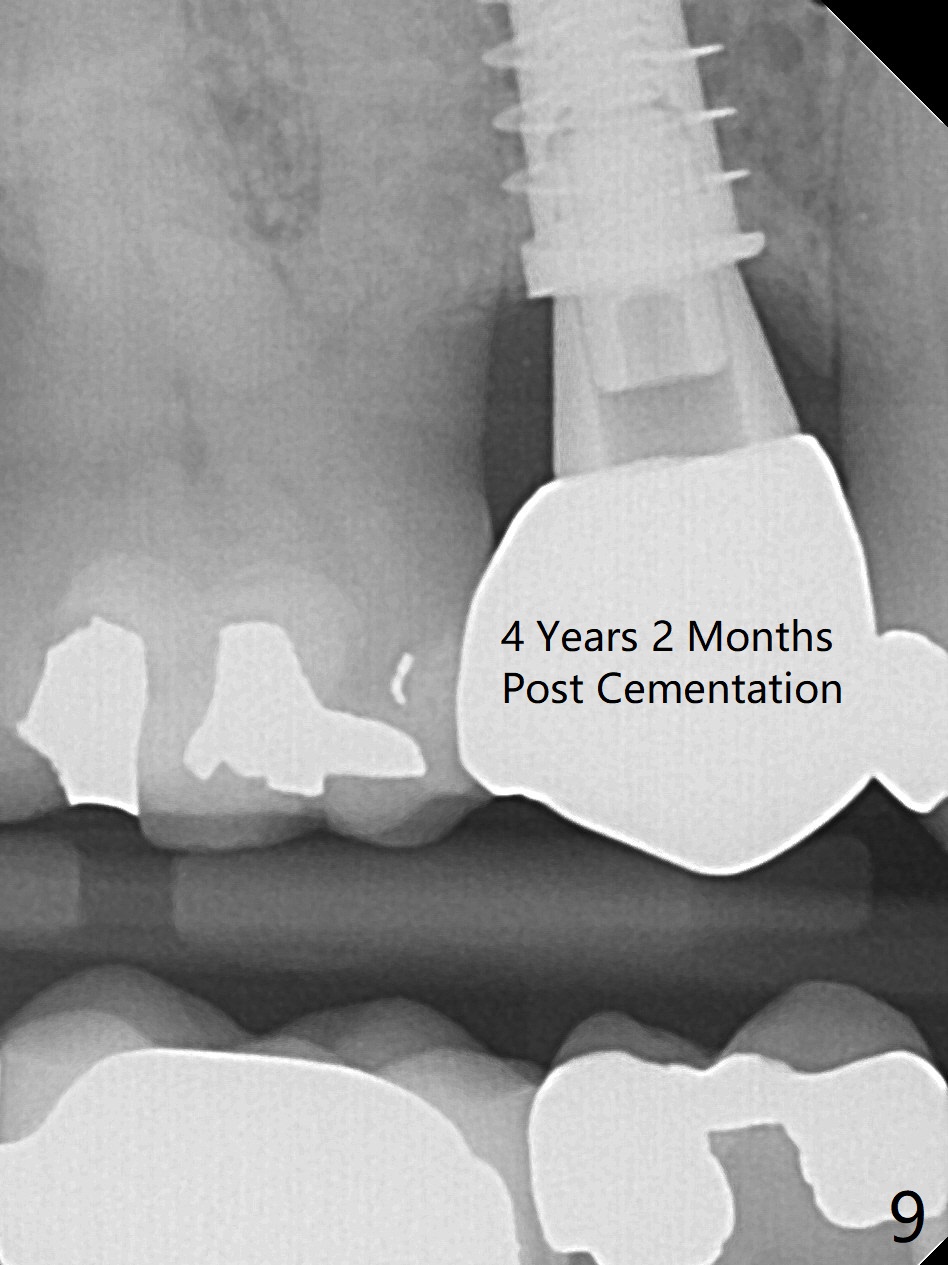
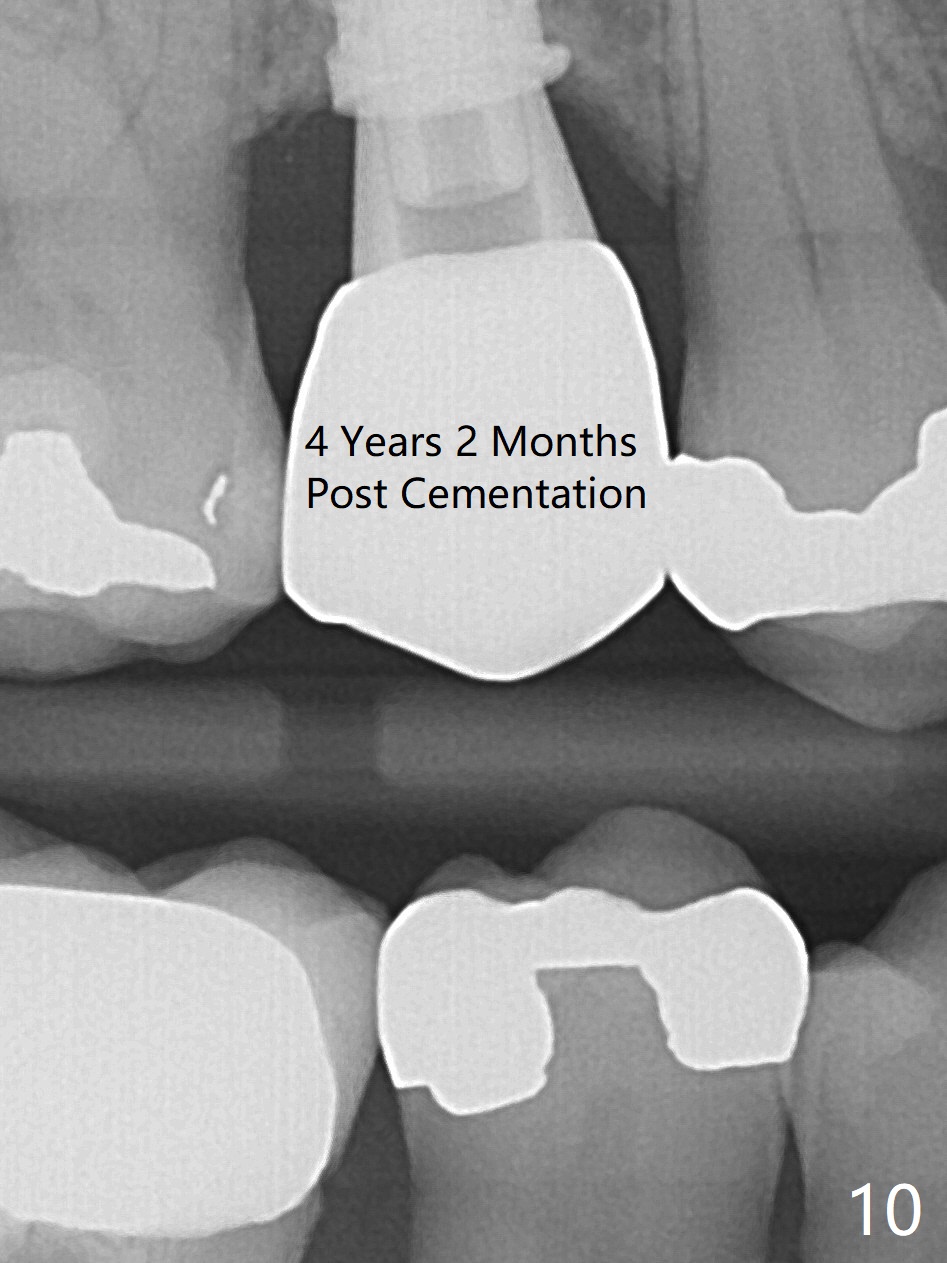
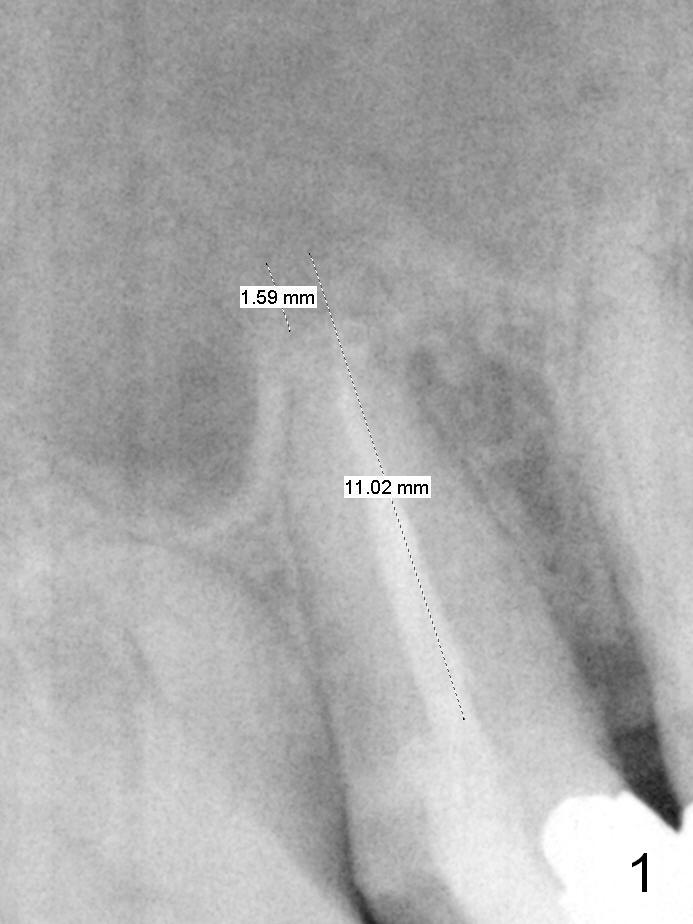
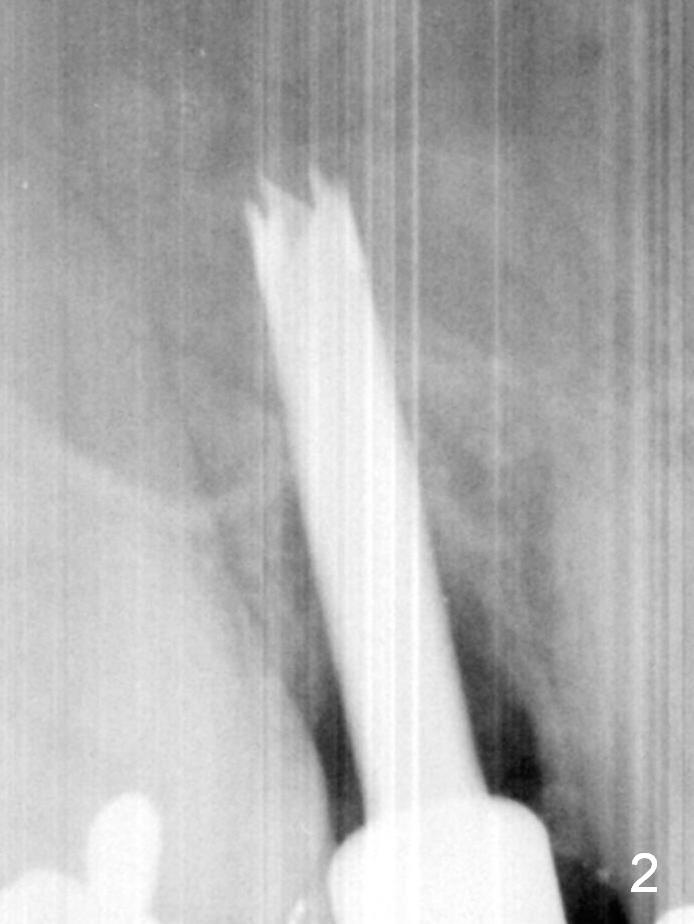
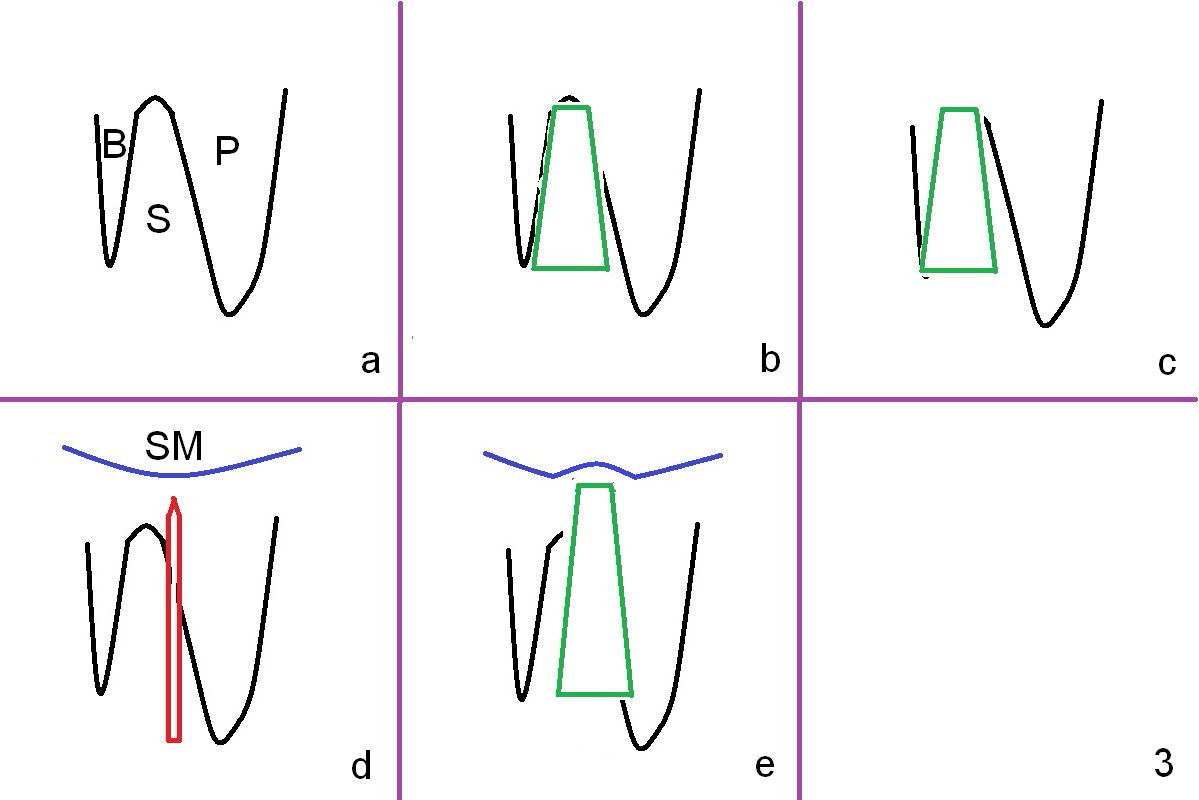
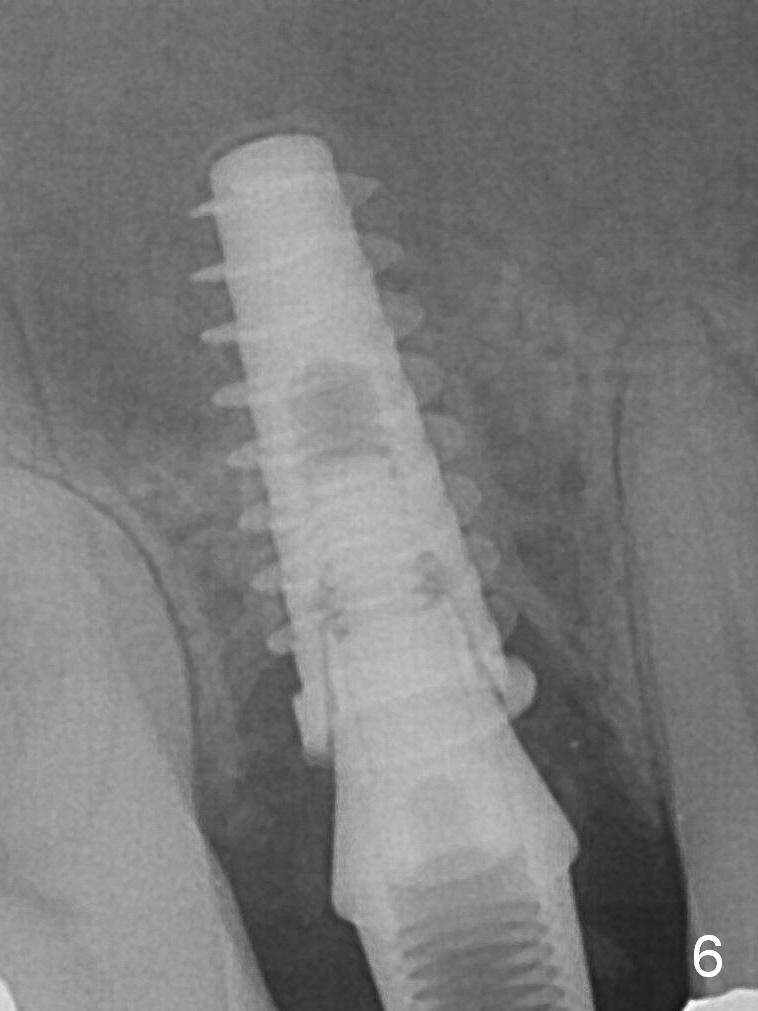
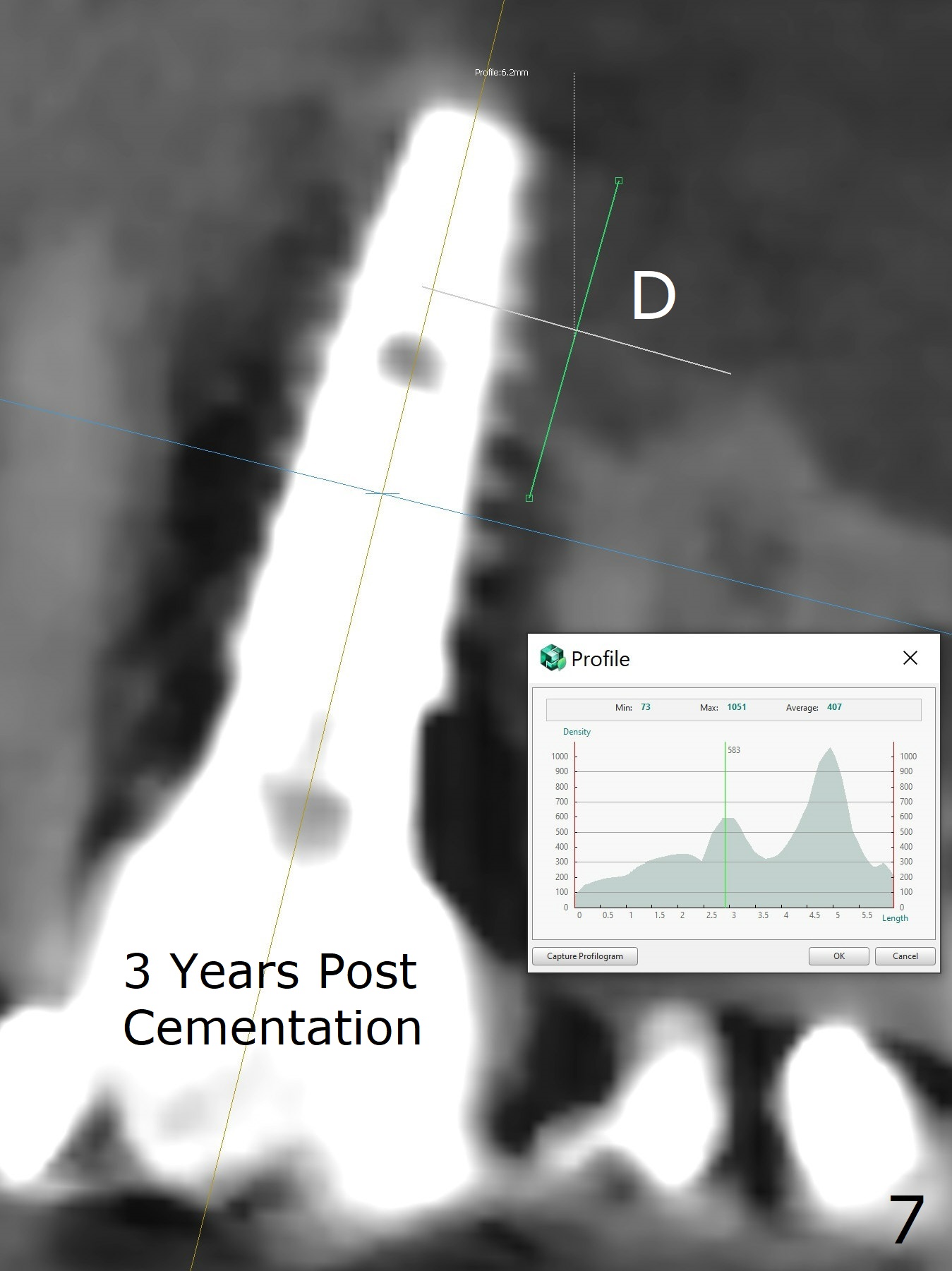
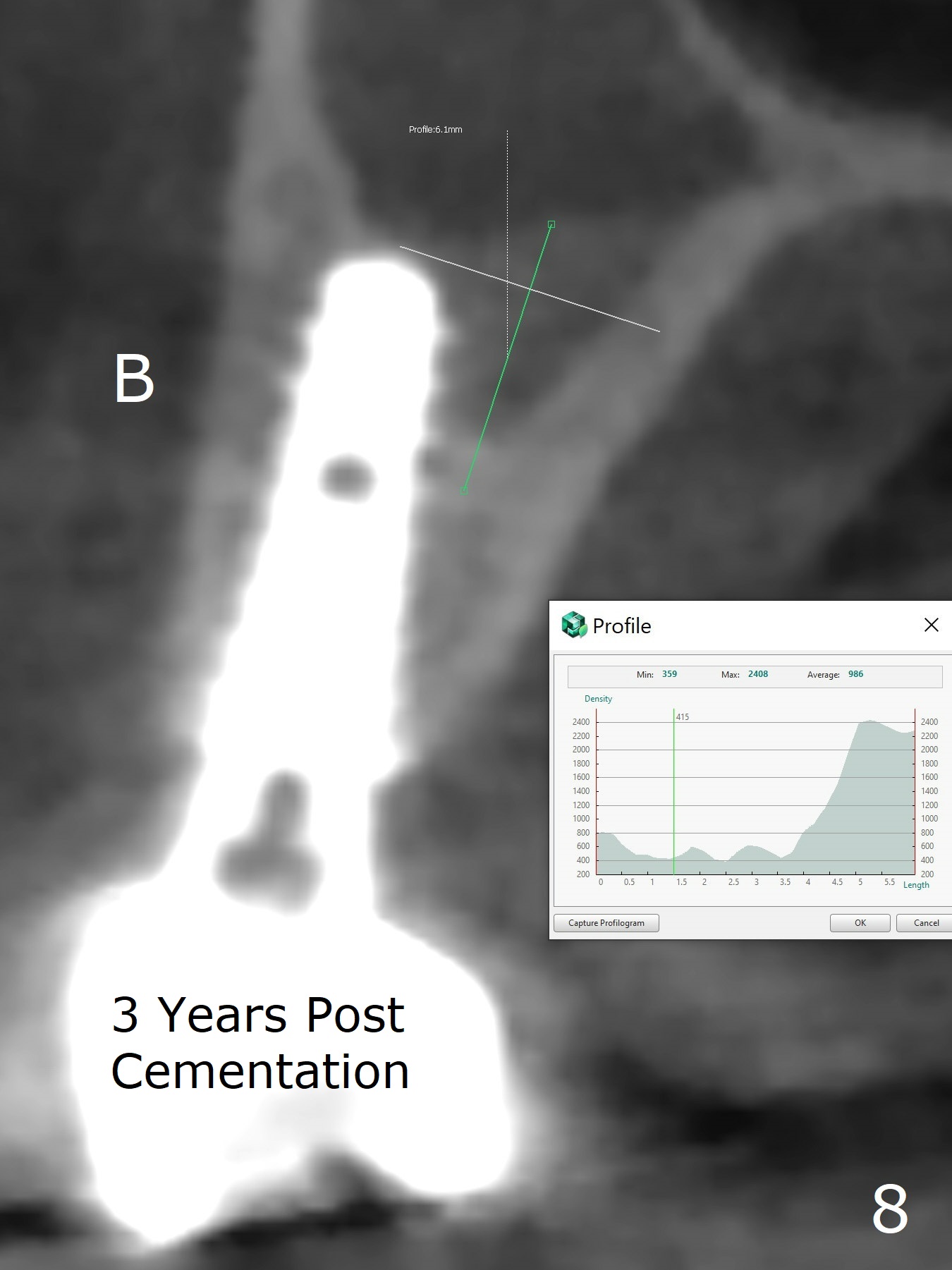
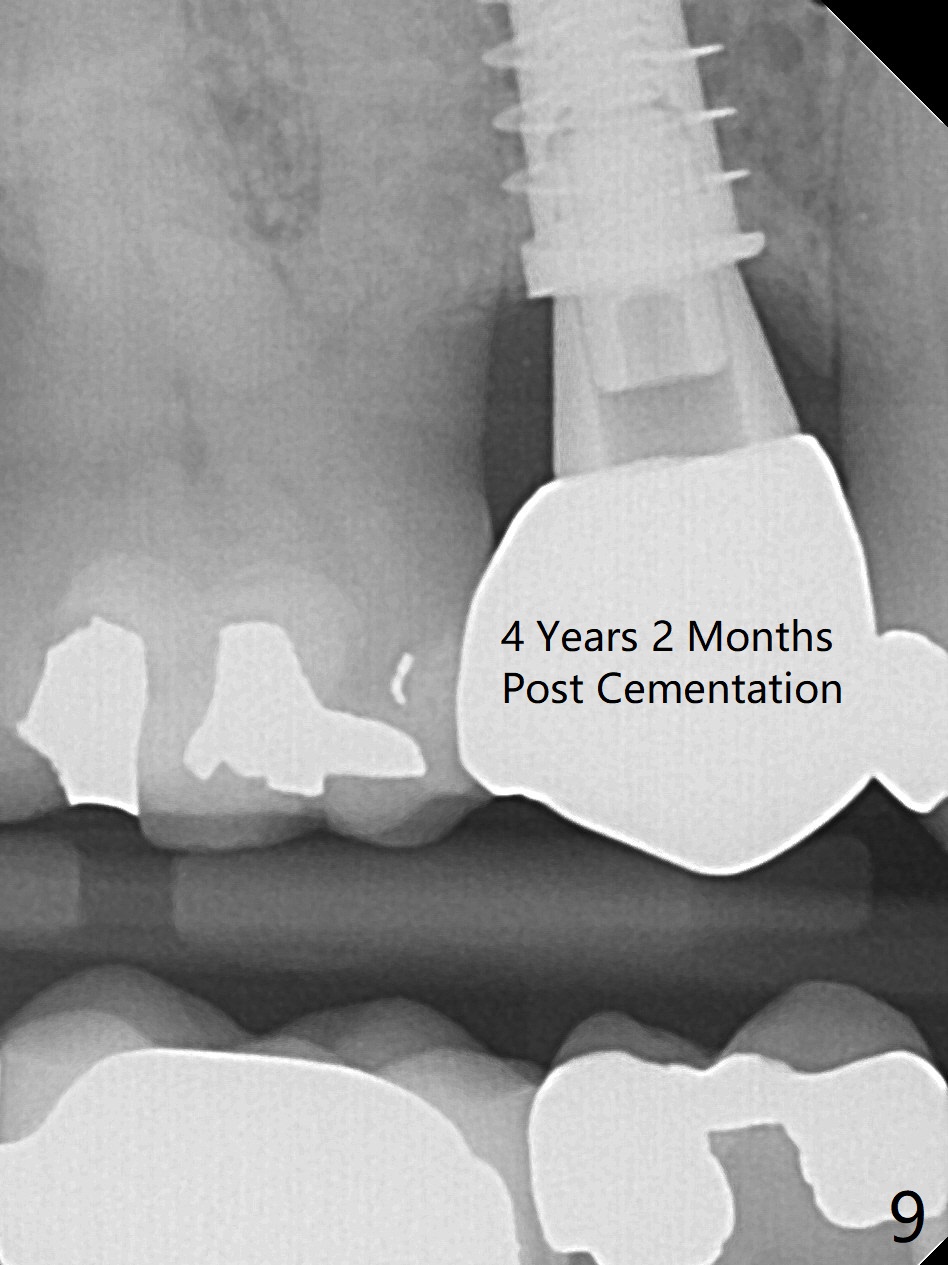
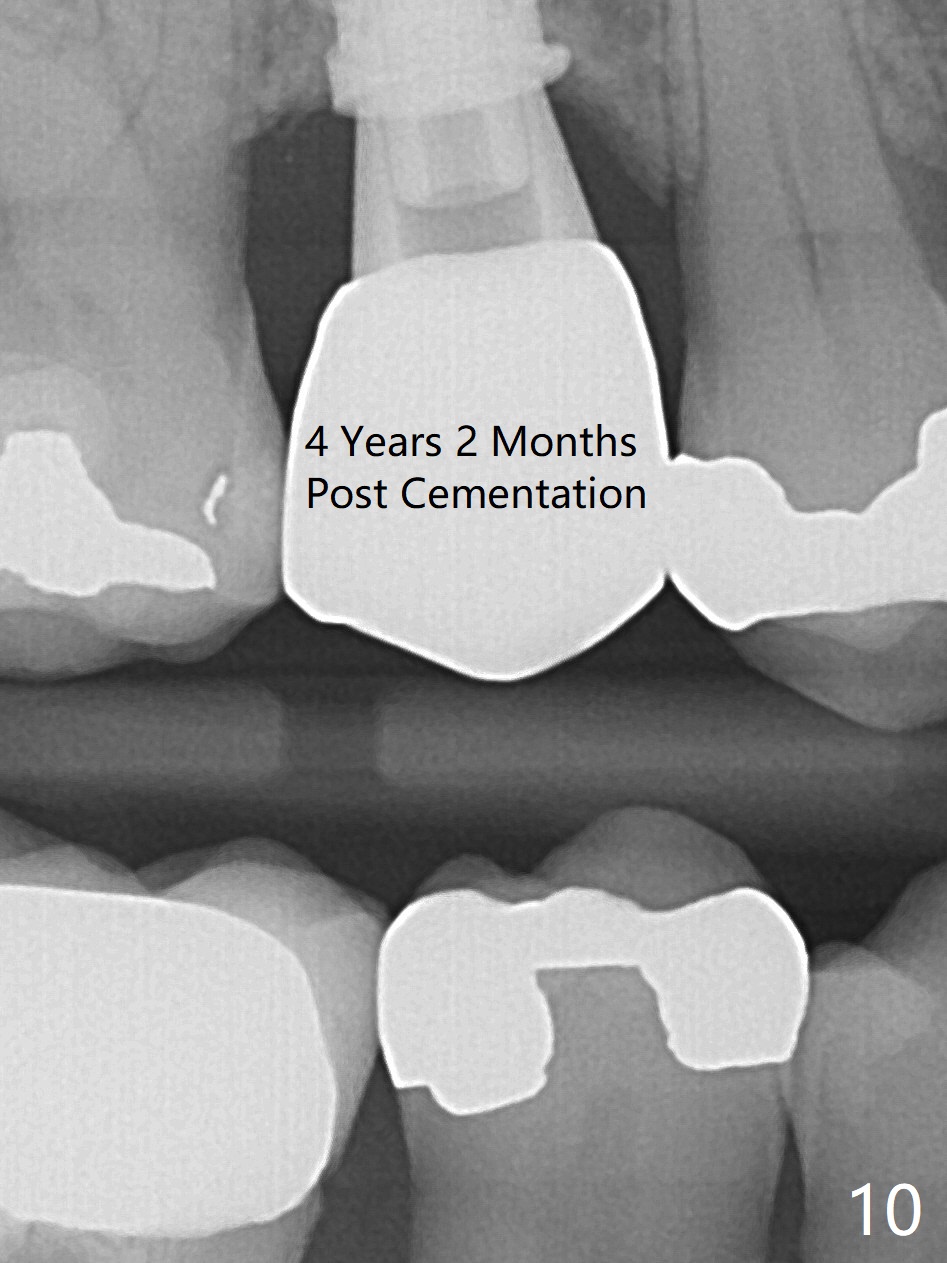
To prevent sinus lift related sinusitis, a shorter implant is going to be placed (Fig.1), approximately 2 mm beyond the apex. Following extraction, the buccal plate (Fig.3a (coronal section): B) is not only ~ 2 mm shorter than the palatal one (P), but also thinner. Since the bone density of the palatal plate is higher, without osteotomy an implant is less likely placed in the middle of the socket (S (Fig.1); Fig.3b) than buccal (Fig.3c). Therefore drills are used to form osteotomy in the apical 1/3 of the palatal slope (Fig.3d (red arrow); SM: sinus membrane). When 3.3 mm Magic Drill (MD) is in place (Fig.2), the distal surface of the sinus septum is perforated without air leakage. Demineralized allograft (.0125-.085) is placed for sinus lift (Fig.4 *) prior to placement of 4.5x11 mm implant with ~ 30 Ncm. The implant is slightly buccal to the ideal position indicated in Fig.3e (curved blue line: sinus lift). A 4.5x4(2) mm pair abutment is placed for an immediate provisional to hold mineralized allograft in the remaining socket gaps (Fig.4 arrowheads, .5-1.5 mm). A 9 mm implant may avoid sinus floor perforation on the distal slope of the 2nd premolar. The osteotomy should have been established initially as mesial as possible. In fact the patient has nasal hemorrhage while sneezing for the first 2 days postop. Although he complains of pain buccal to the implant, the gingiva appears to heal 7 days postop (Fig.5). The distobuccal papilla appears to be displaced somewhat. Raising mucoperiosteal flap is most likely associated with postop pain and esthetic compromise. The implant appears to have osteointegrated 5 months postop (Fig.6). A 4.5 mmx15° 3 mm cuff angled abutment is placed for final restoration. The distolingual portion of the implant is supported by the regenerated bone 3 years post cementation (Fig.7,8). There is no bone loss 4 years 2 months post cementation (Fig.9,10).
Return to
Upper Premolar Immediate
Implant,
IBS,
#18
19
Xin Wei, DDS, PhD, MS 1st edition 10/03/2016, last revision 05/06/2021