

 |
 |
 |
|
 |
 |
 |
 |
 |
 |
 |
|
 |
 |
 |
|
 |
 |
||
Three Potential Sites for Upper Molar Immediate Implant
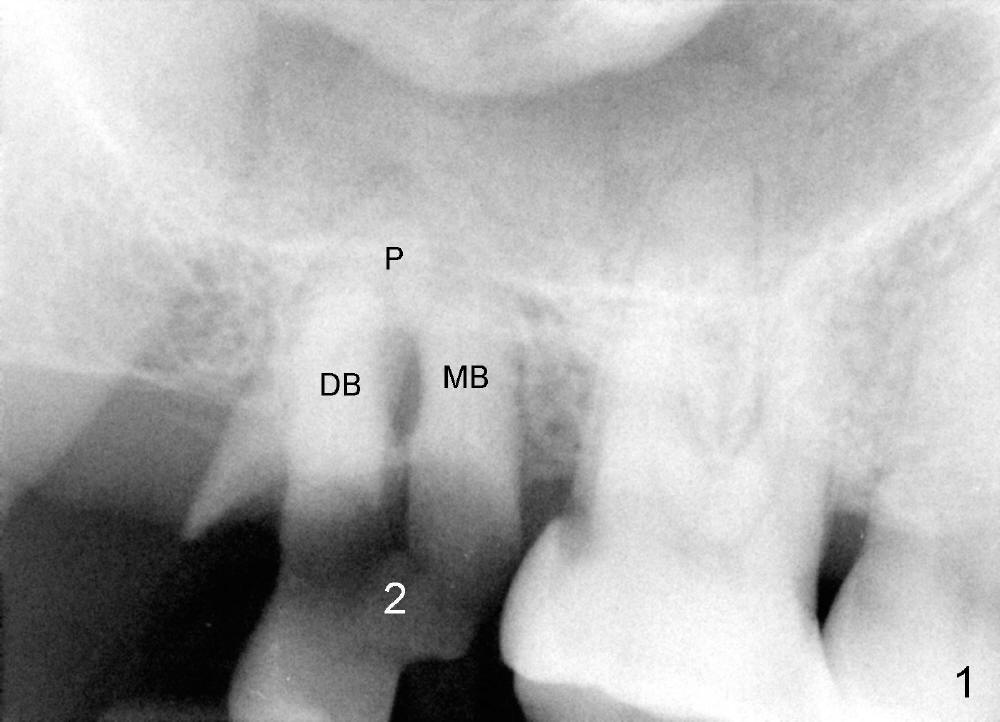
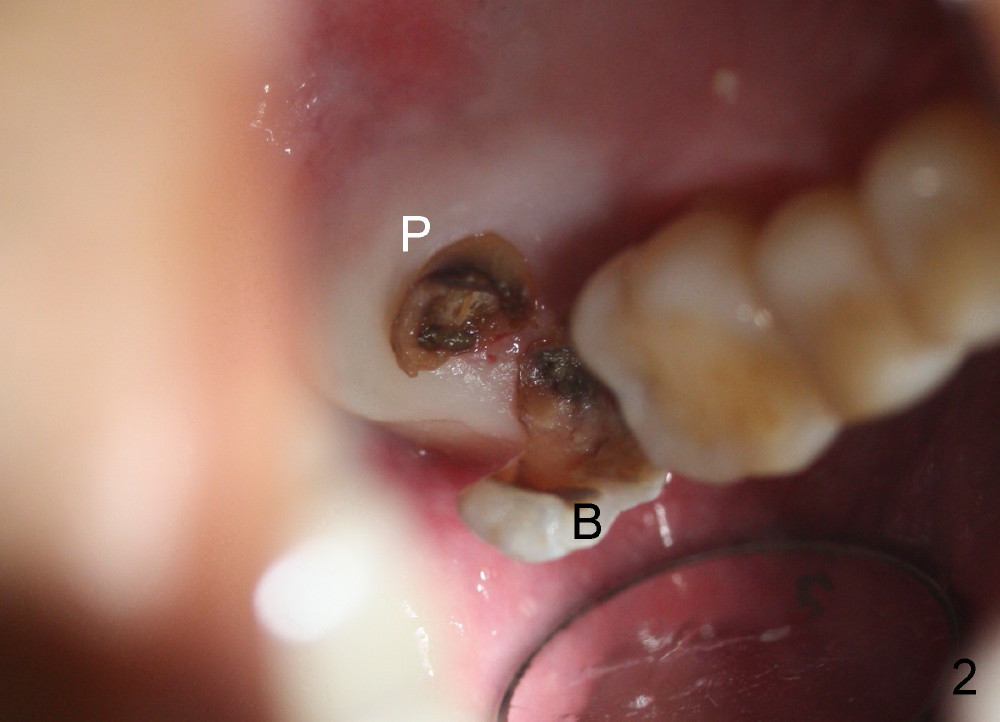
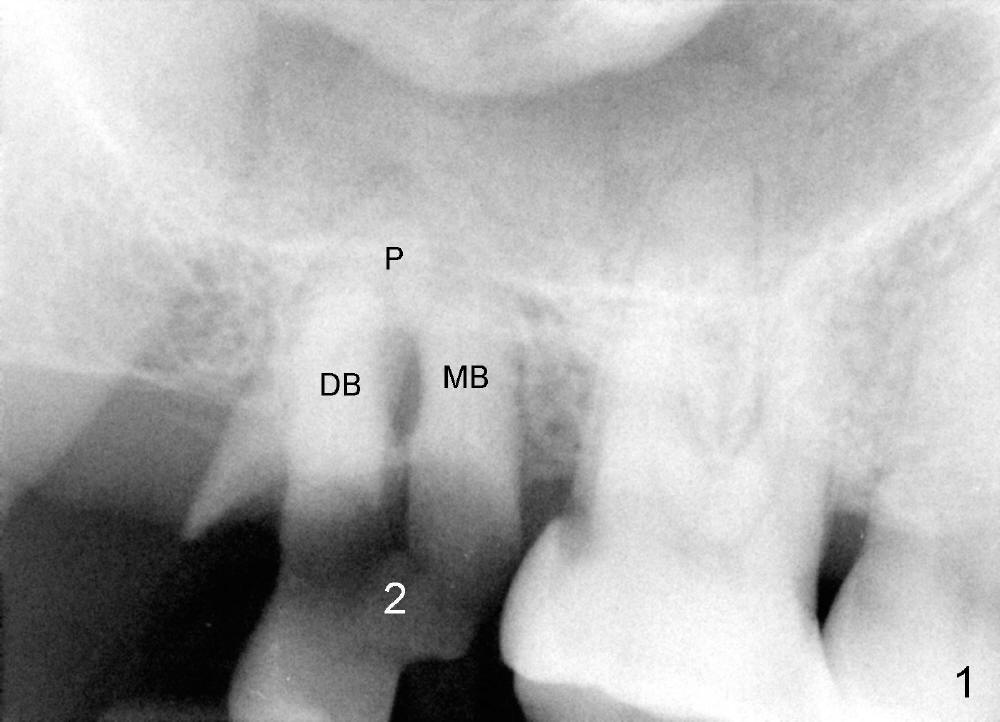
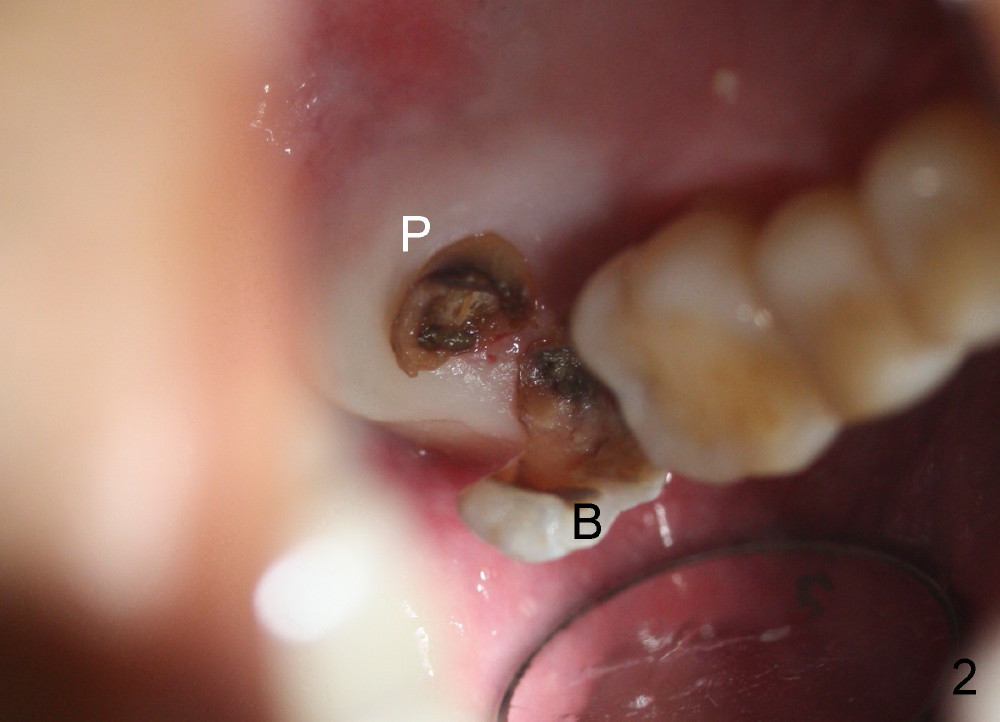
Immediately preop PA and photo confirm that the upper right 2nd molar is nonsalvageable (Fig.1,2). After extraction, it appears that there are 3 potential sites for immediate implant.
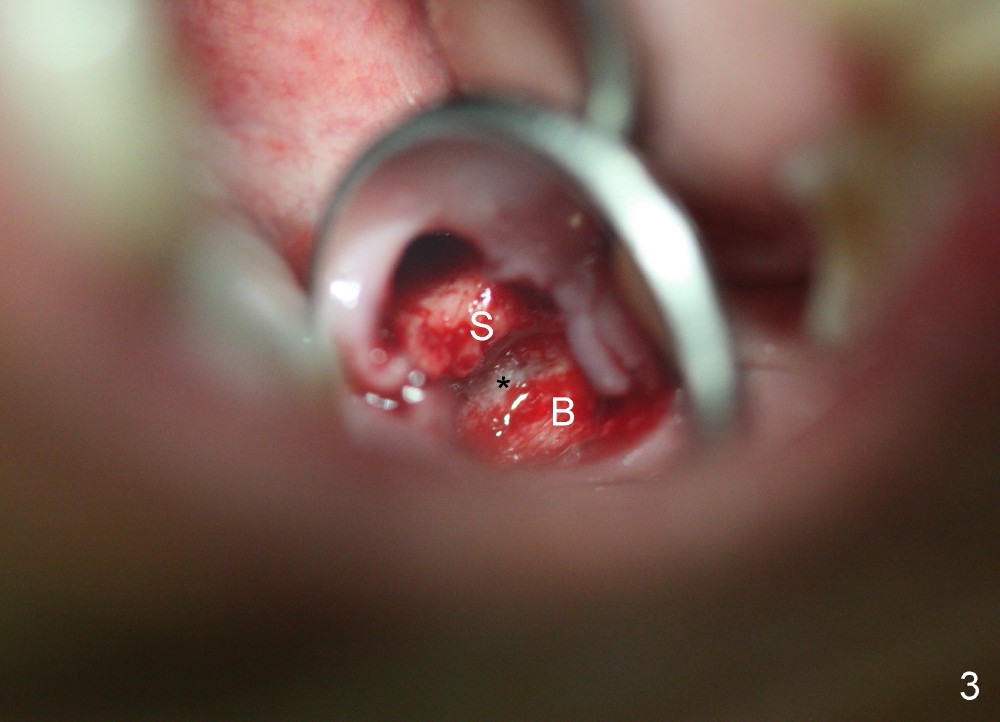
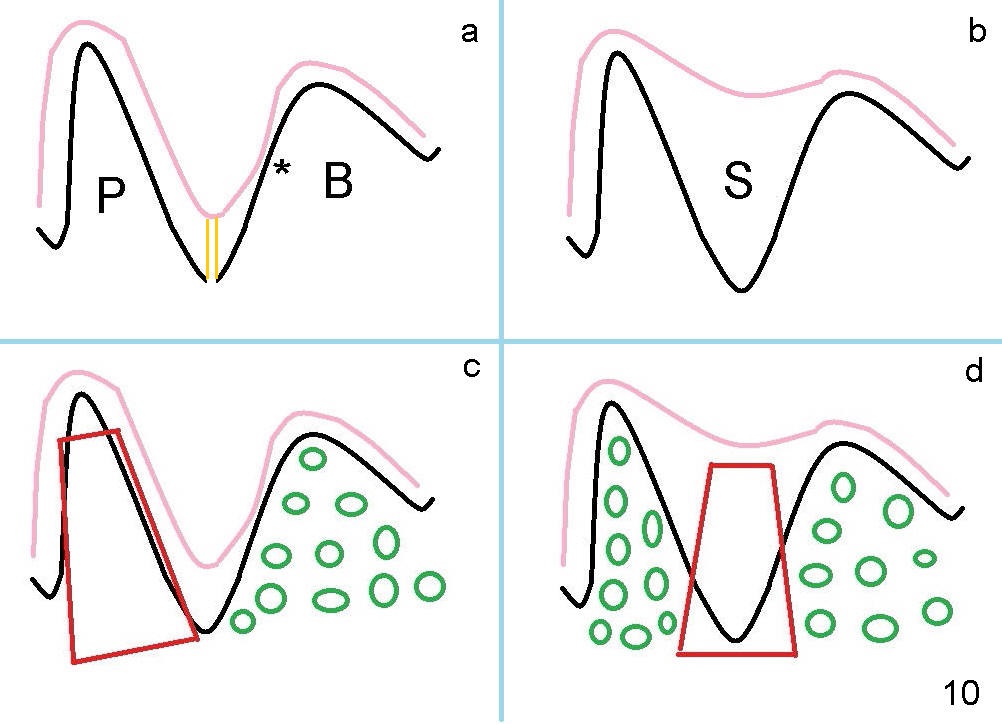
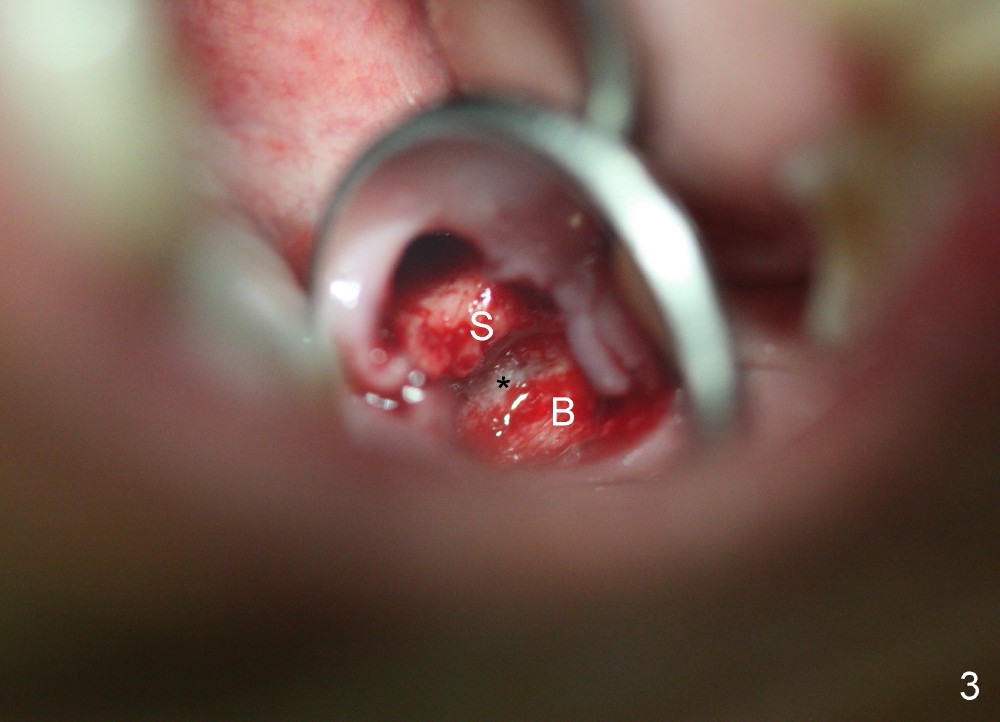
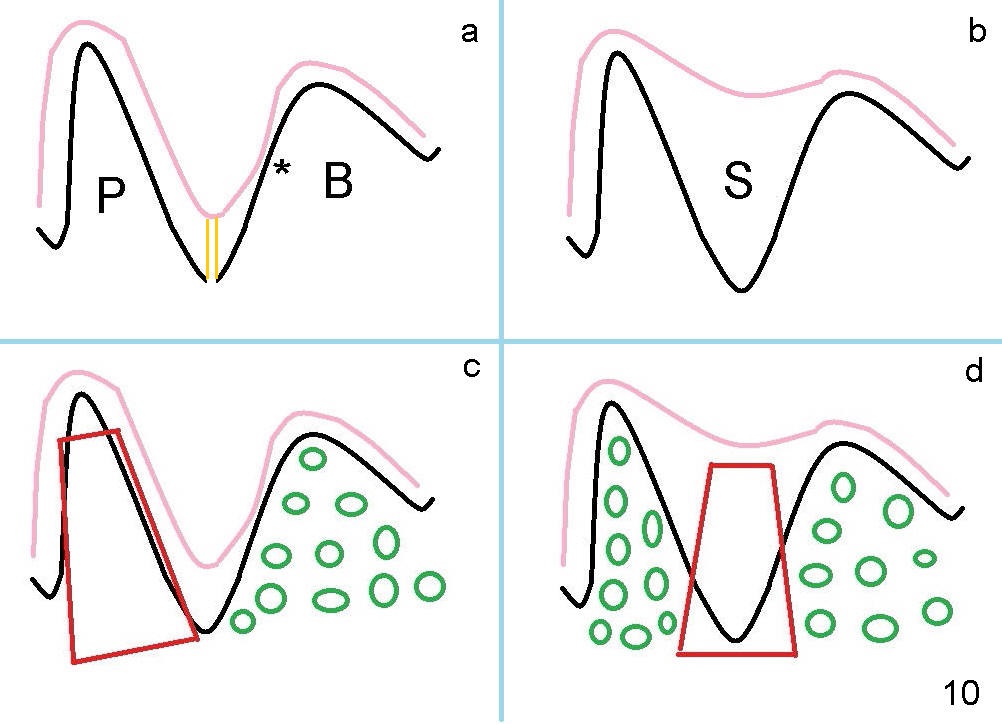
The buccal socket (Fig.3 B) is large and shallow (difficult to achieve primary stability of implant); the palatal wall of the buccal socket is apparently thin (greyish *). The most critical is that the buccal plate of the buccal socket is low (Fig.10a).
The septum is narrow buccopalatally (Fig.3 S). It is difficult to make initial drill penetration at the top of the septum. It appears that the septal bone height is limited (Fig.10a). Preop PA shows that the sinus floor is lower than the root apices (Fig.1). This is a typical sign of sinus floor ditching in between the apieces.
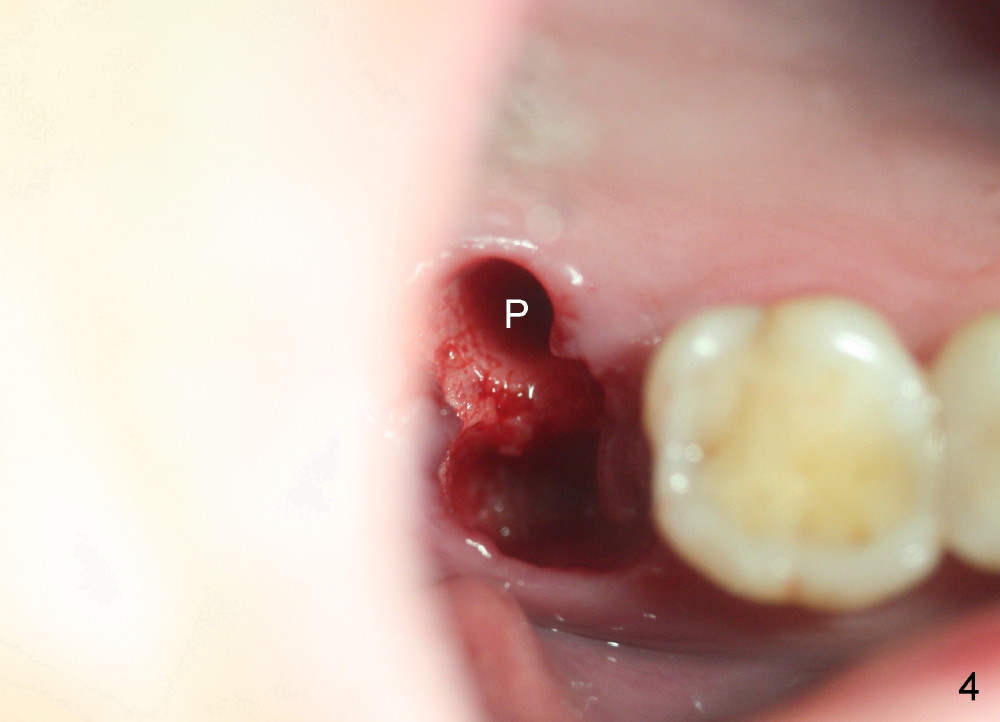
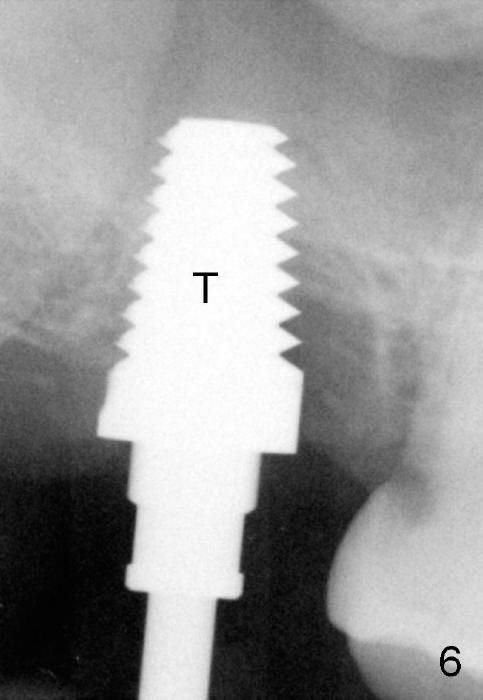
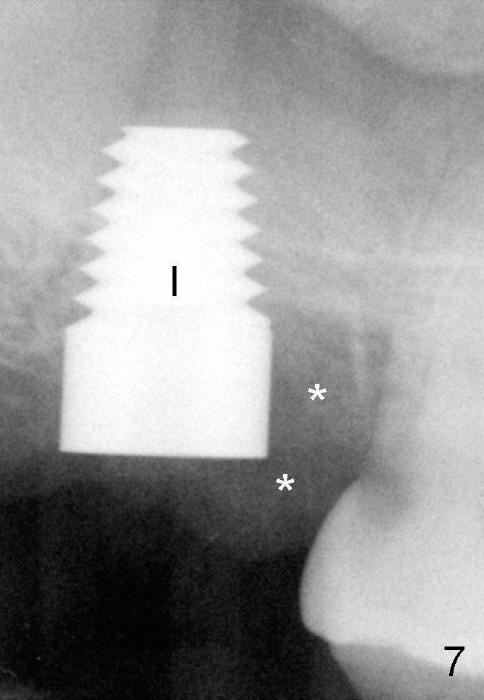
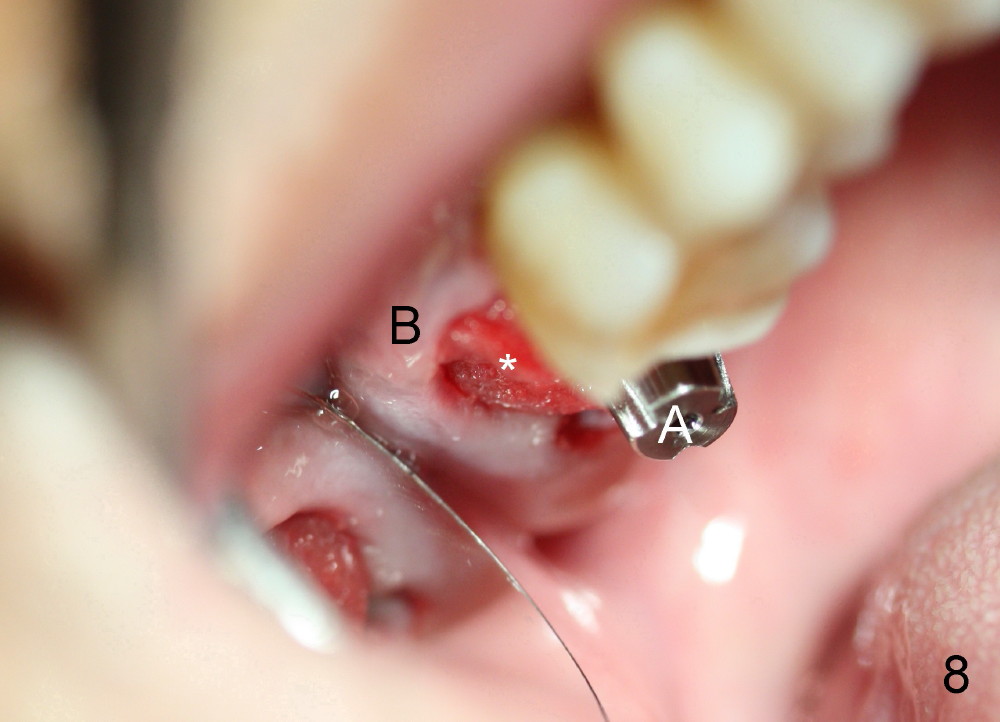
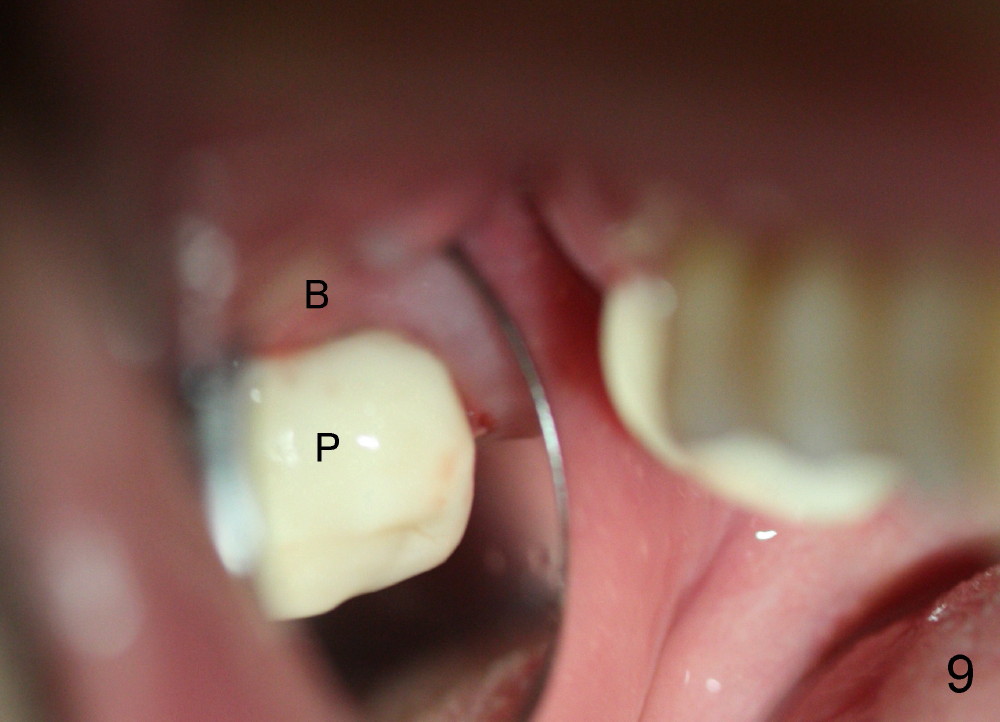
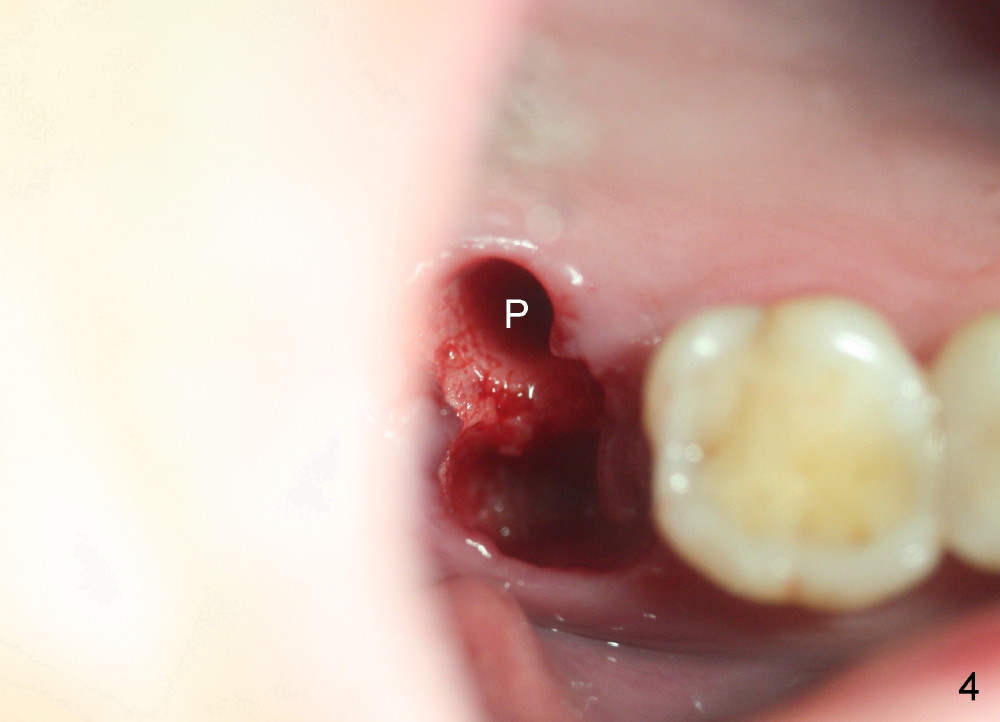
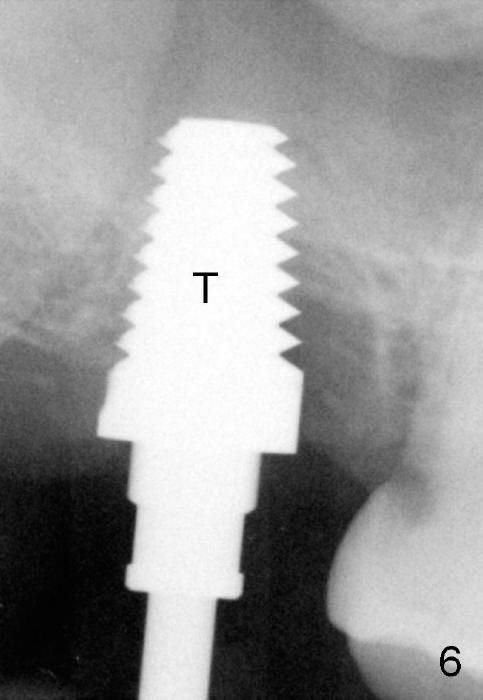
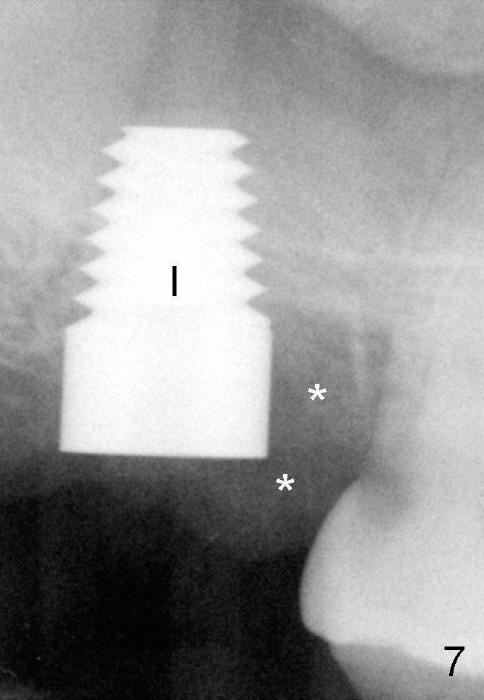
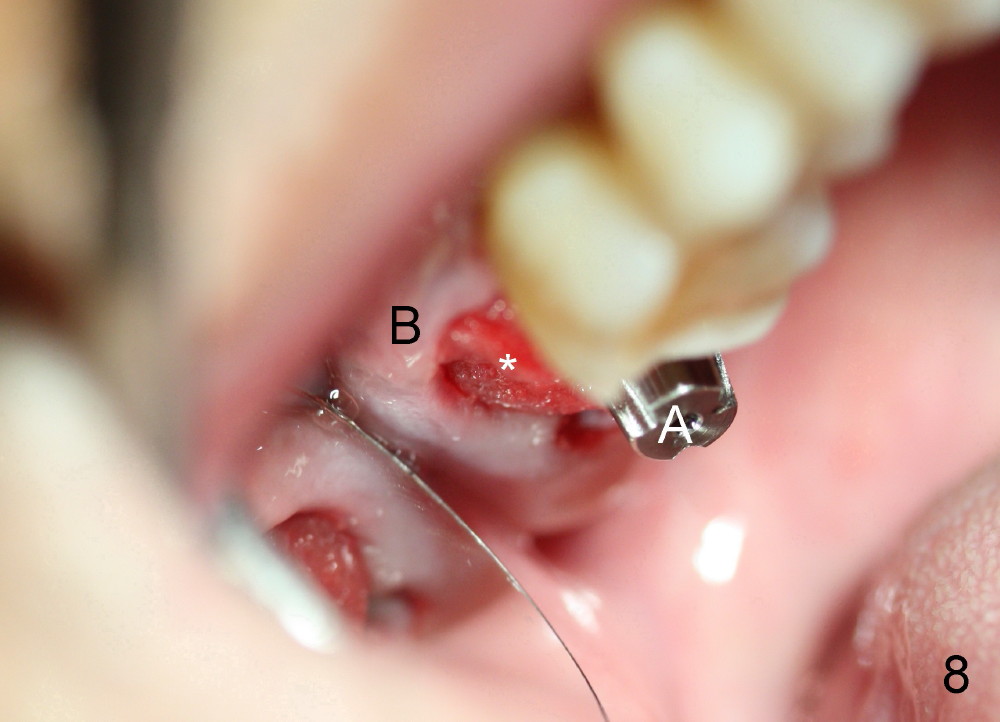
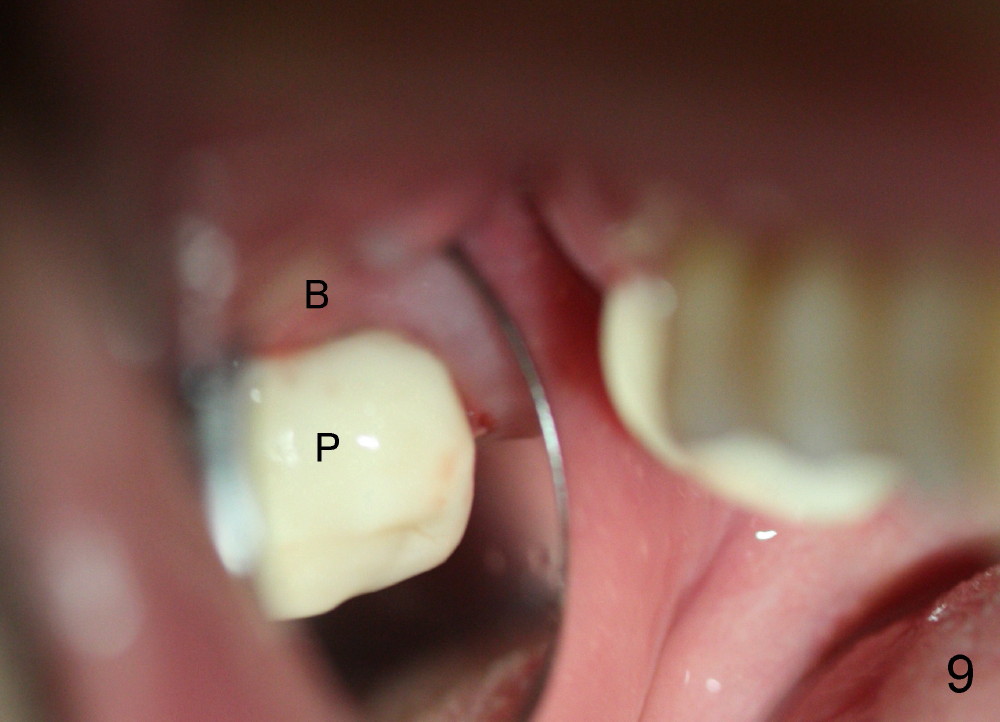
By contrast the palatal socket is deep and relatively small (Fig.4 P), easy to insert taps without drills. When a 7x11 mm tap is placed (Fig.5 T), the coronal end is more or less near the lingual cusps (functional cusps). Although the 7x14 mm tap (Fig.6 T) and a 7x11 mm implant (Fig.7 I) look poking into the maxillary sinus, they are in fact within the palatal socket (Fig.10c). Allograft and Osteogen are placed in the buccal socket (Fig.7 *), followed by collagen dressing (Fig.8 *). A 5x5 mm abutment is placed (Fig.8 A). An immediate provisional (Fig.9 P) is cemented to keep the graft and collagen dressing in place.
If the sinus floor (Fig.10b: pink line) is flat over the septum, there is enough bone height in the septum to support an implant (Fig.10d: red line). It is easier to restore. Bone graft (green circles) is placed in the buccal and palatal sockets.
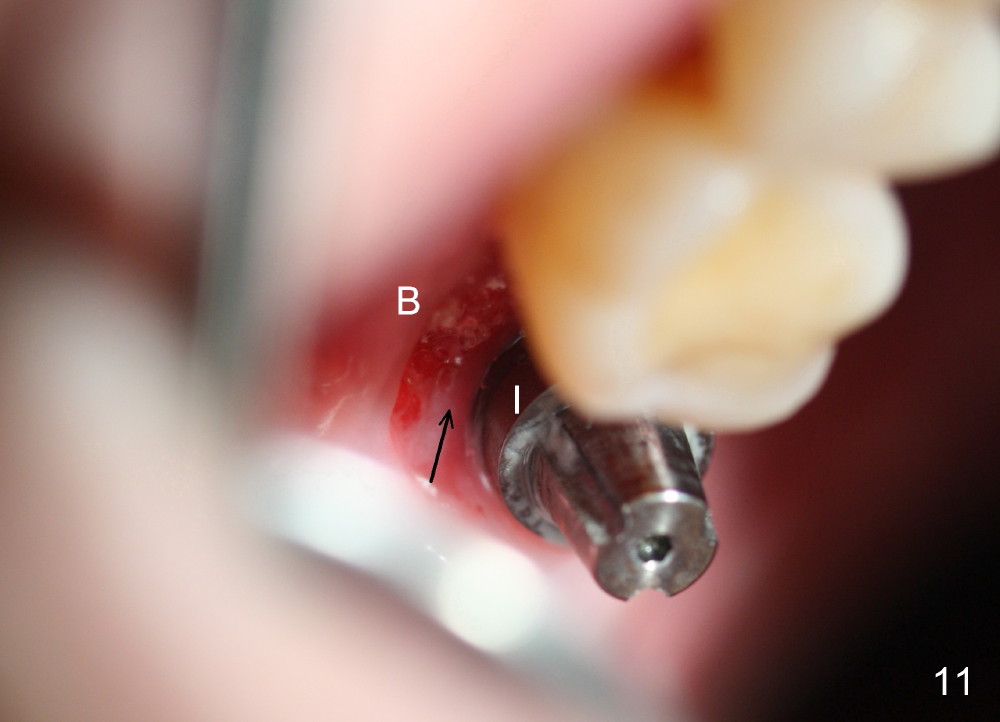
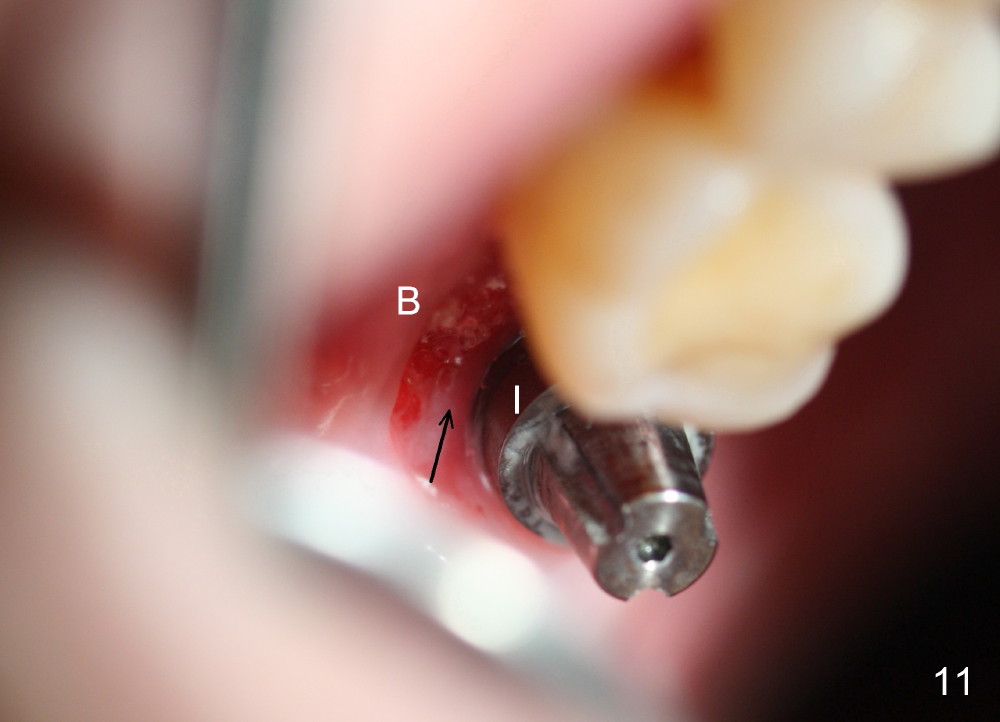
The patient returns to clinic 1 month postop, because of loosening of the provisional. The buccal socket appears to have epithelium (Fig.11 B); the keratinized gingiva has apparently moved (arrow) to cover the buccal surface of the implant (I). The long abutment, which was used for retention of the immediate provisional as well as the graft and collagen dressing, has finished its mission. It is changed to a shorter one to accommodate the future occlusion. A second implant is planned to be placed at the site of #31.
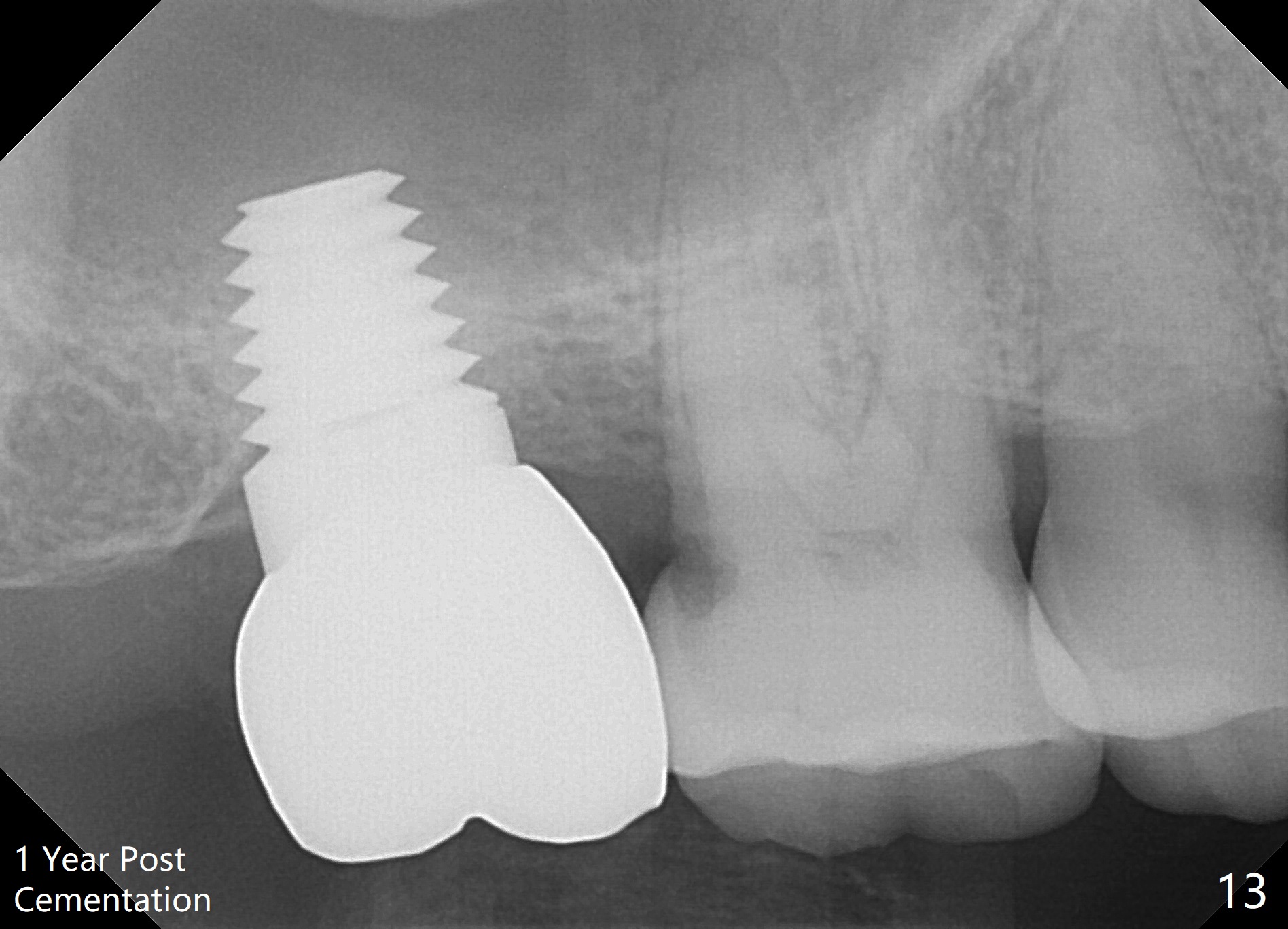
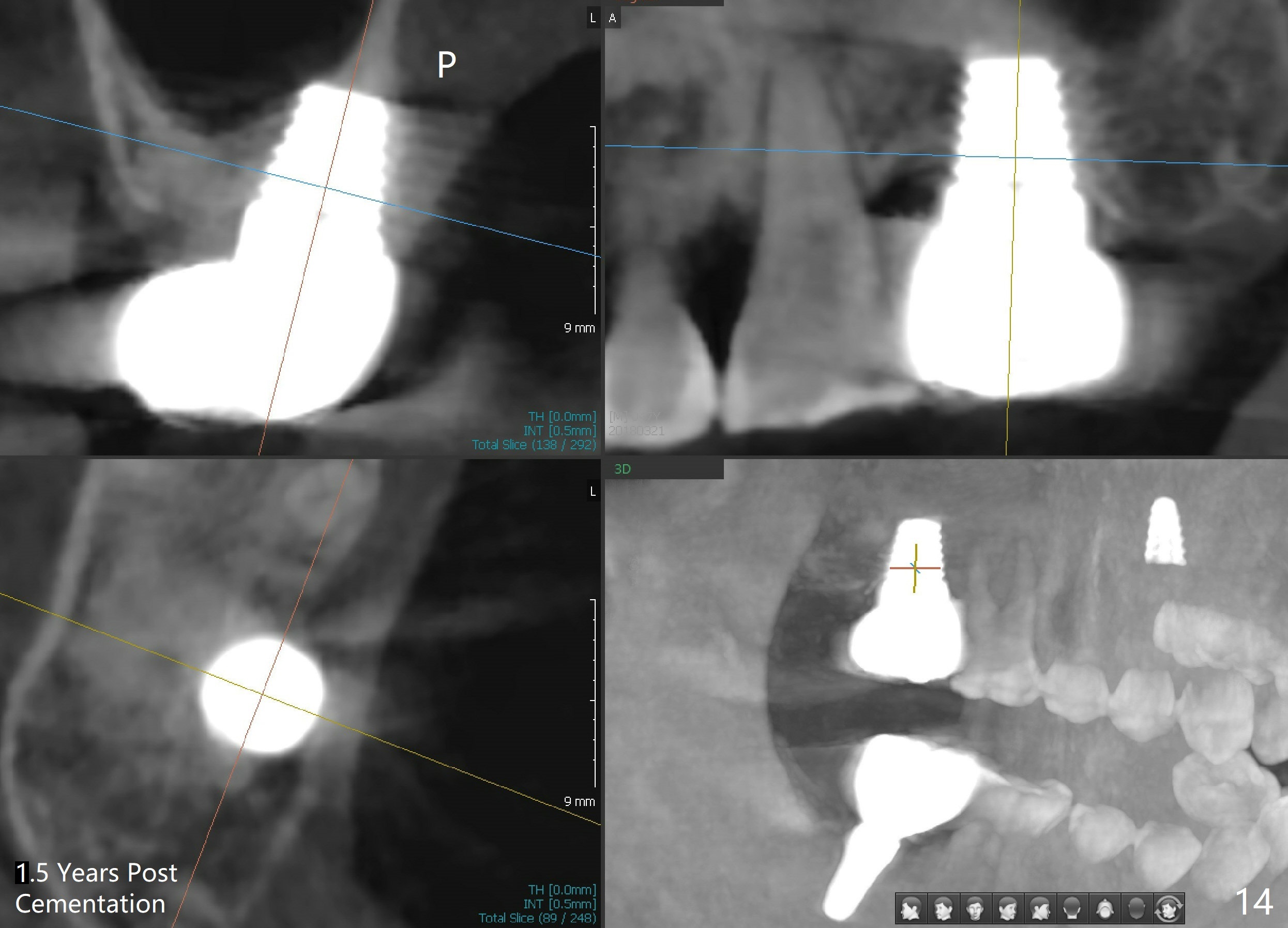
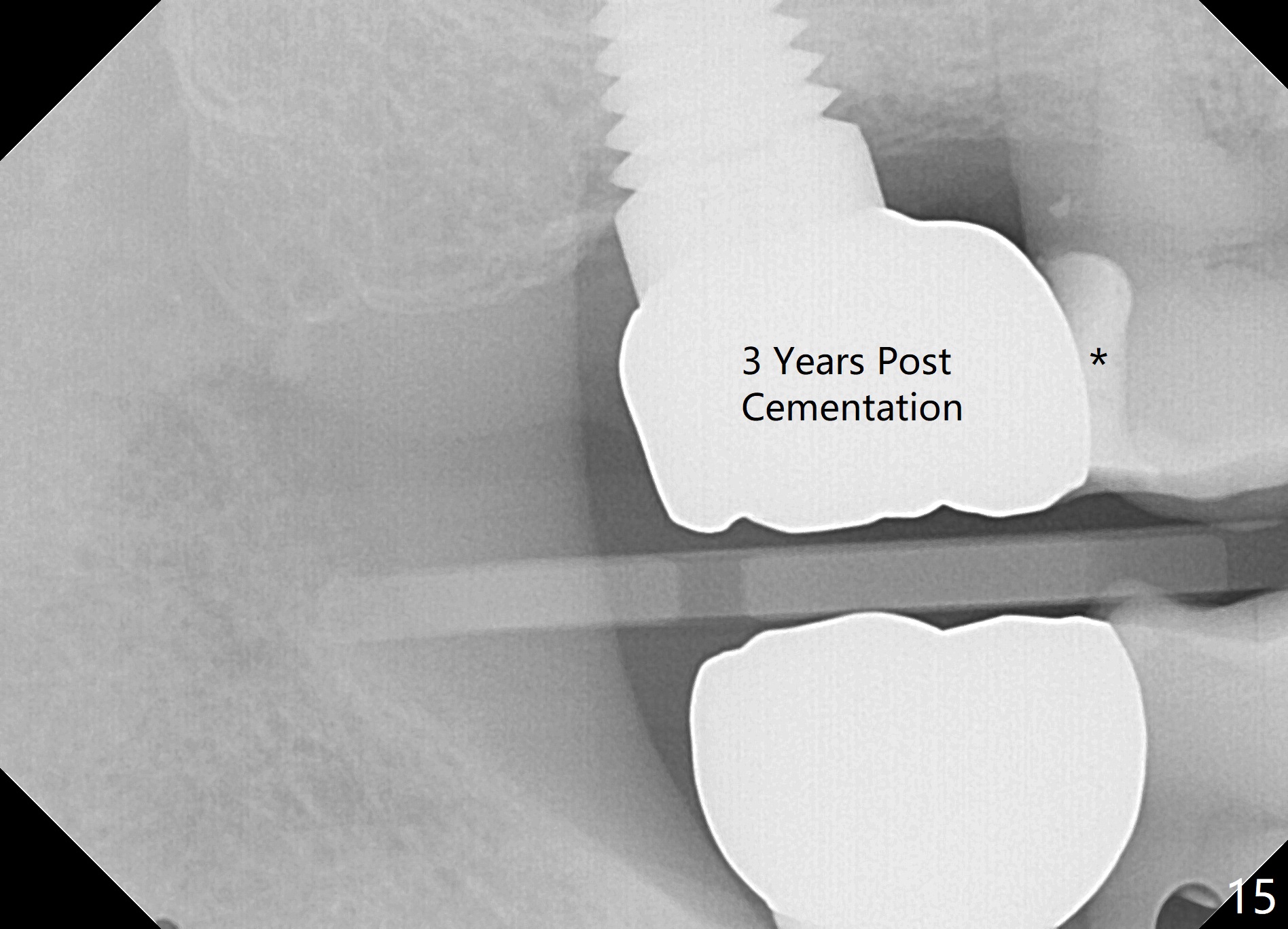
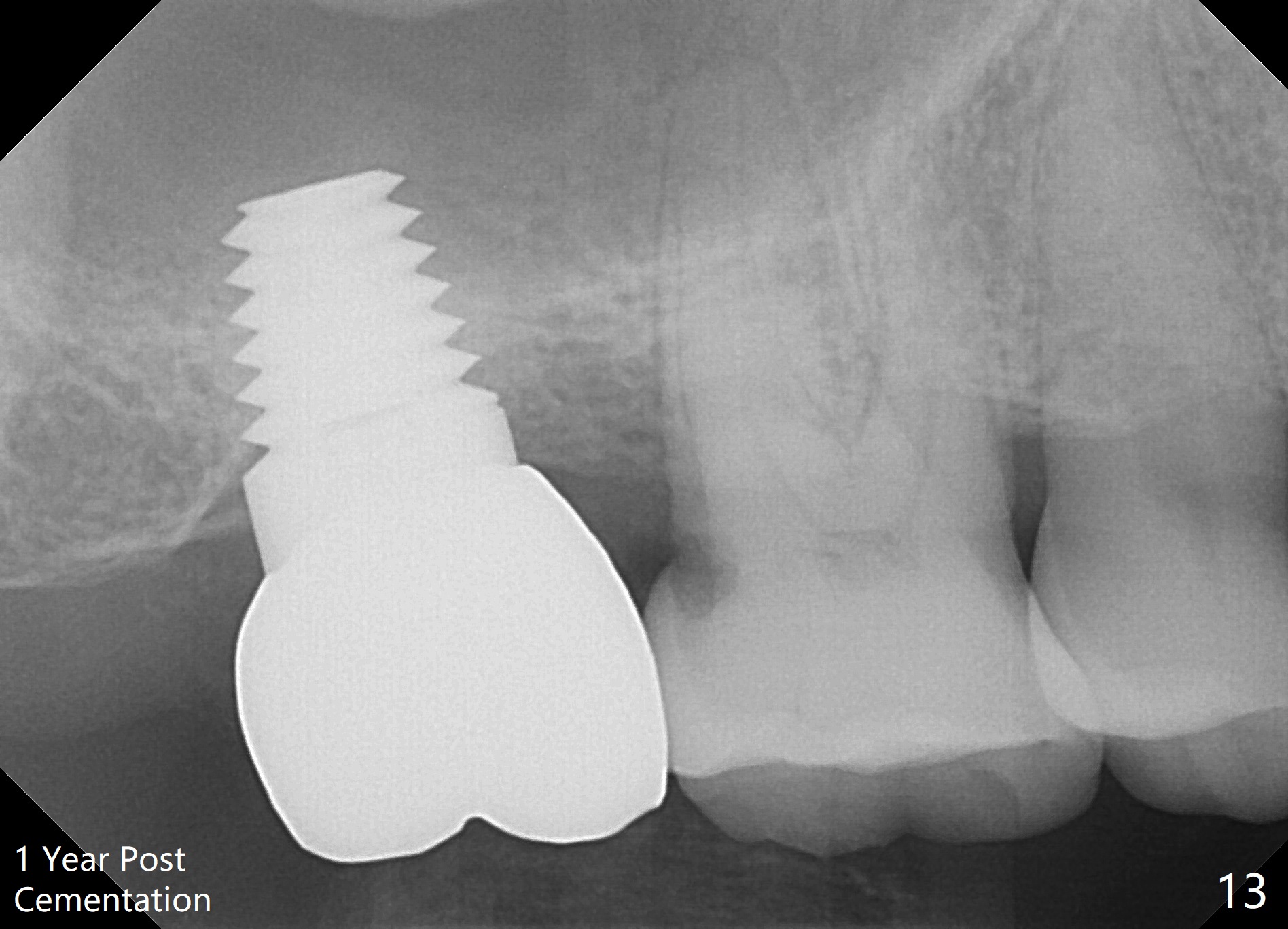
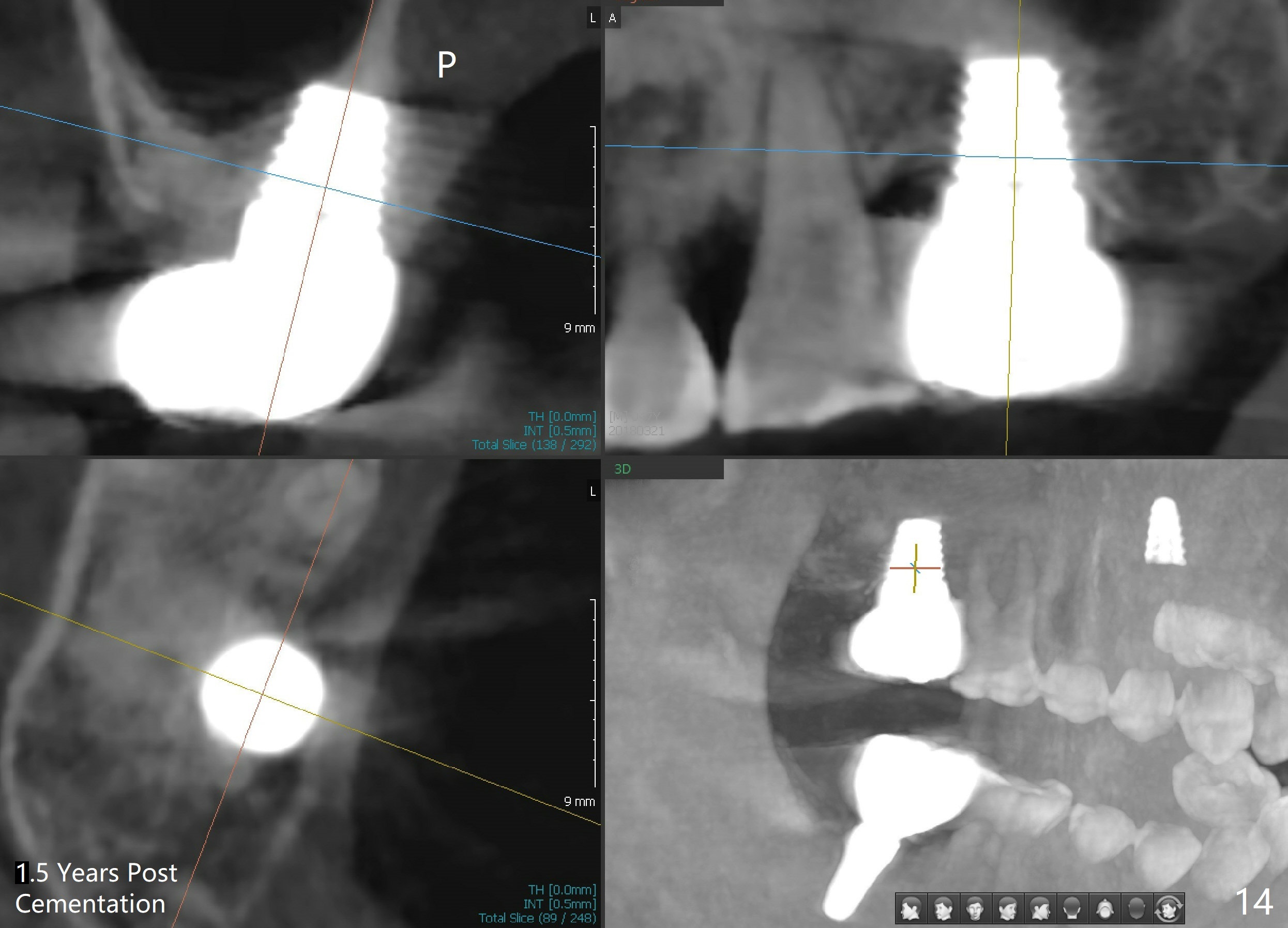
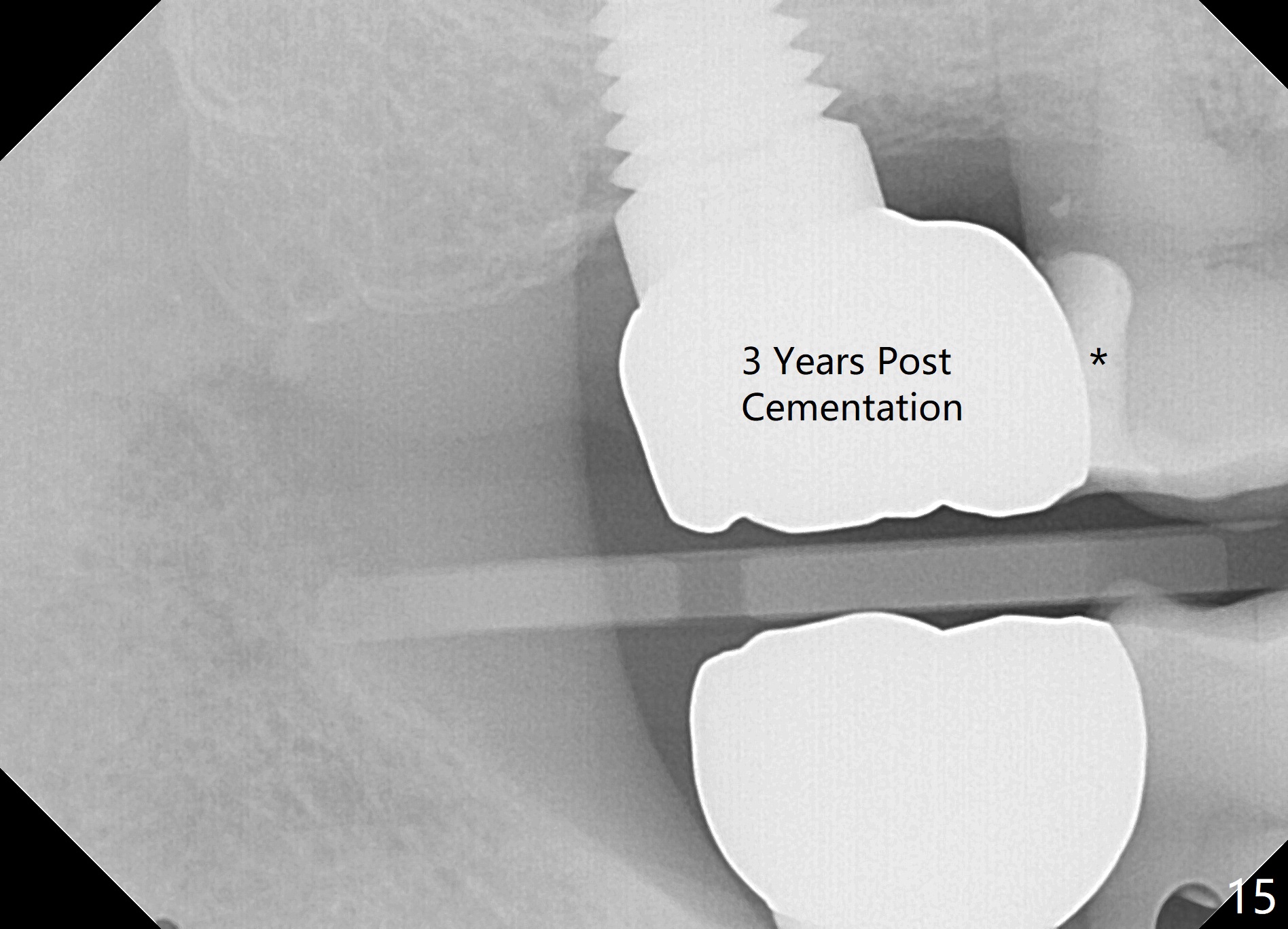
The patient returns for final restoration 22 months postop (Fig.12). Implant threads are embedded in the bone. Panoramic X-ray is taken after removal of perforated provisional and abutment. The implant remains asymptomatic 1 year post cementation (Fig.13) in spite of the fact that there appears to be no palatal plate (Fig.14 (1.5 years post cementation)). It is probably related to the thick palatal (P) gingiva. Periimplantitis develops 3 years post cementation and immediately post #15 implant 2nd removal. The implant is found to be palatal when #3 DO composite is placed (Fig.15). Oral hygiene appears to be difficult to maintain in spite of use of water pik. His diabetes is under control with Insulin.
Return to
Upper Molar Immediate Implant
Systemic Diseases, #15,
31
Xin Wei, DDS, PhD, MS 1st edition 12/05/2014, last revision 12/05/2020