




 |
 |
 |
 |
 |
 |
 |
 |
 |
 |
||
Mesh and Bone Graft
Two one piece implants (3x17 mm) were placed at the site of #23 and 26 with flapless approach 12 months ago. The implant at #26 was found to be placed too buccally intraop. Suggestion was made to the patient to remove the malpositioned implant immediately and placed at the site #25. The patient was so nervous that she declined the offer. These two implants healed apparently normally and restored 4-5 months later (3-unit bridge).
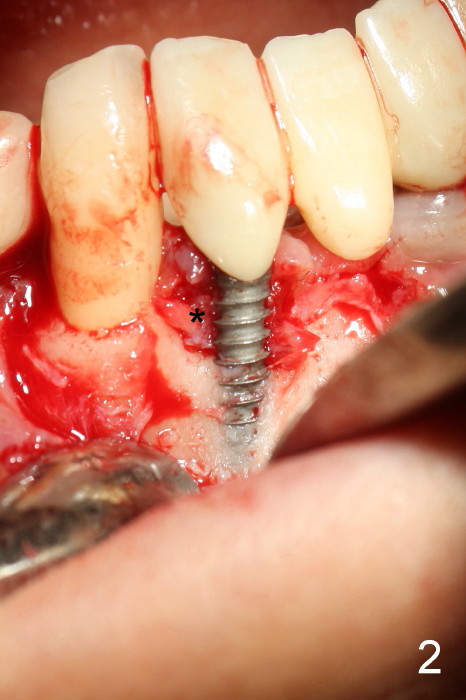
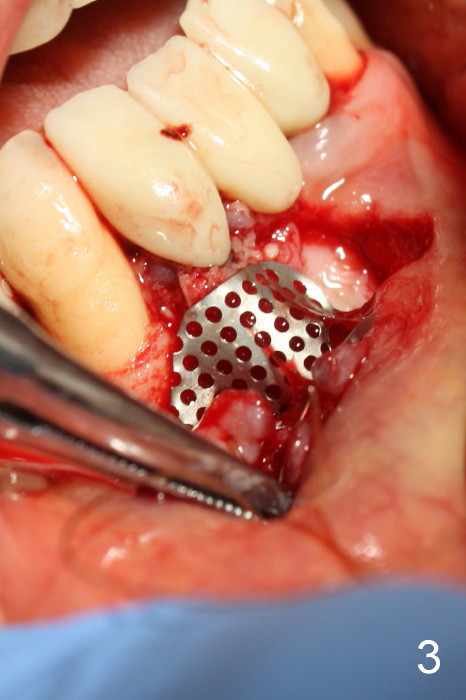
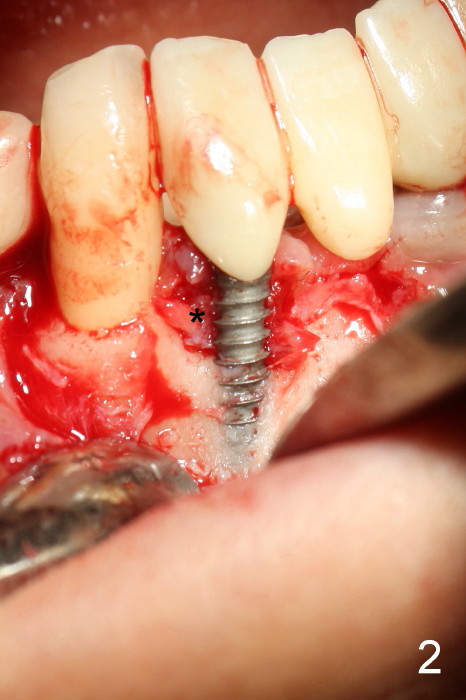
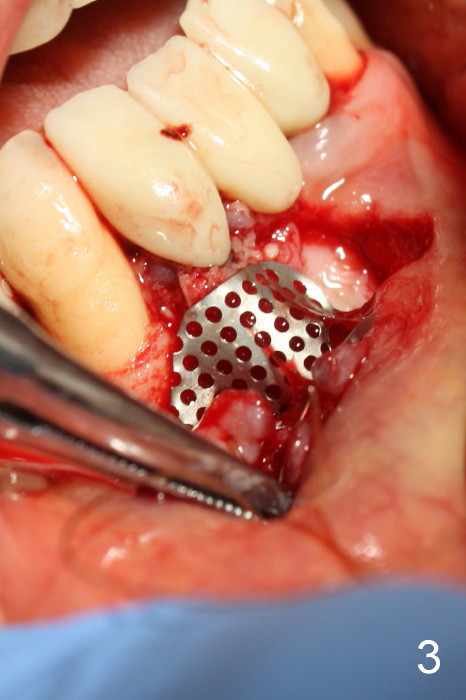
The patient has had chronic pain and swelling associated with the implant at the site of #26 (Fig.1). The extent of implant thread exposure is shown in Fig.2 after flap reflection; inflammatory granulation tissue is present around the most coronal threads (*, one year post cementation). Following debridement and Clindamycin soaking, allograft is placed around the exposed threads; a titanium mesh is used to contain the graft (Fig.3). The flap is closed with tension in spite of the periosteum being underscored. The patient develops moderate to severe ecchymosis postop.
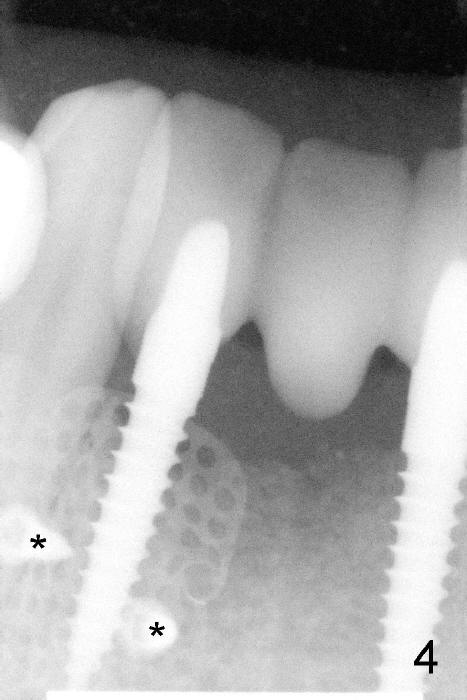
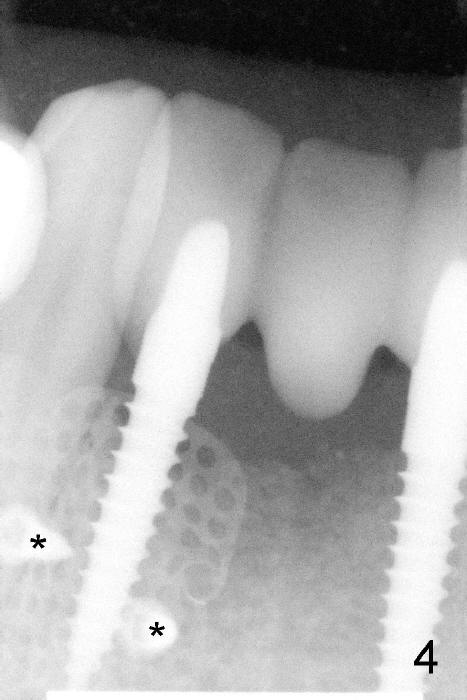
The coronal portion of the mesh is exposed with loss of bone graft granules. It appears that the mesh has lost its function. It is planned to be removed. PA is taken 16 days post placement of the mesh (Fig.4).
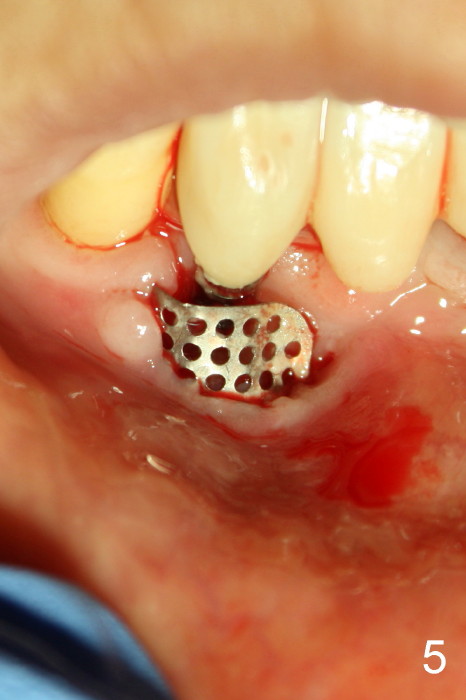
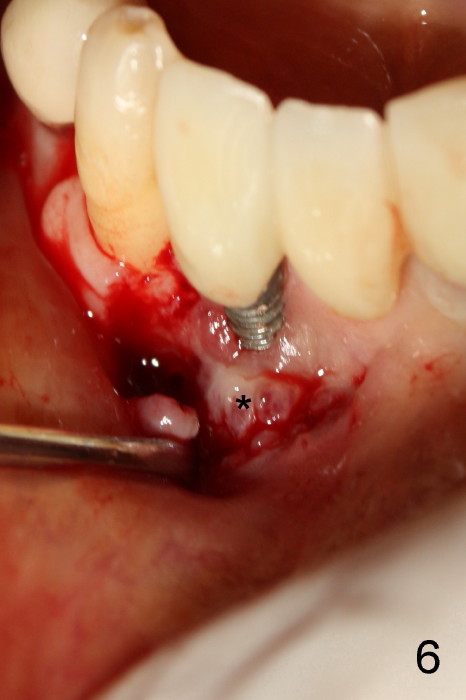
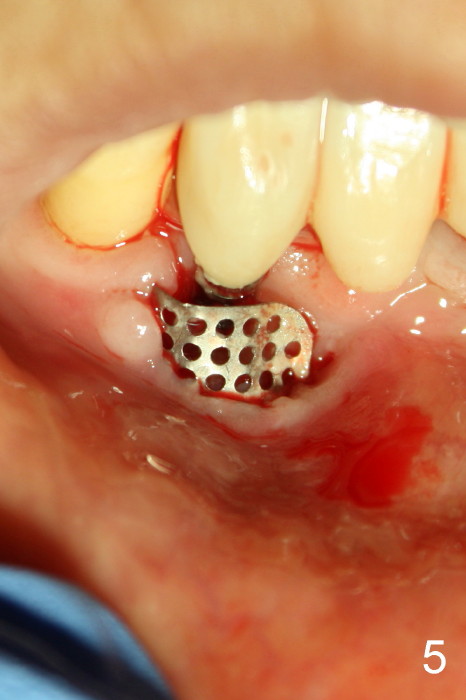
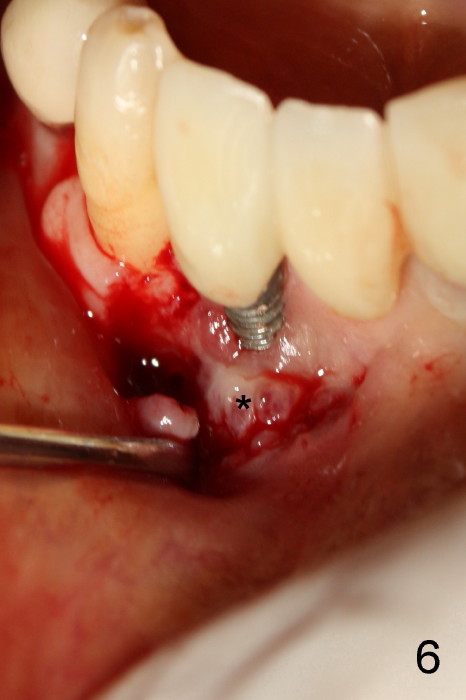
Fig.5 is taken following local anesthesia to show the exposed mesh, 22 days post placement. When the latter is removed, the exposed threads appear to be less (Fig.6, as compared to Fig.2). There is healthy granulation tissue growth apically (*). The patient is asymptomatic 1 month post mesh removal; there is no tenderness around exposed threads (Fig.7). Connective tissue graft is planned to cover the exposed threads through tunnel technique. Thread exposure appears less 3 months post mesh removal (Fig.8). There is infection when the region is not kept clean (Fig.9 (2.5 years post mesh removal)). The other 1-piece implant should have minor implant exposure (<). It appears that there is no thread exposure associated with the immediate implant at #28. Using smaller 1-piece implants (2.5 or 2.0 vs. 3 mm) with flap surgery should be able to prevent the complication. The 72-year-old phobic patient declines any further treatment. Two years later, she agrees to have treatment because of repeated infection (Fig.10). Impression has been taken for stent. After sectioning FPD and removing the infected implant (Tatum), a smaller implant will be placed in between the implants. If her vein is not too small, blood will be drawn for PRF.
How to avoid thread exposure? How to prevent mesh exposure?
Return to Instrument, Lower Incisor Immediate Implant, Armaments 1-Piece
Xin Wei, DDS, PhD, MS 1st edition 06/12/2014, last revision 12/26/2020