



 |
 |
 |
 |
 |
|
 |
 |
 |
 |
 |
 |
 |
 |
 |
|||
There is a Solution to Every Challenge
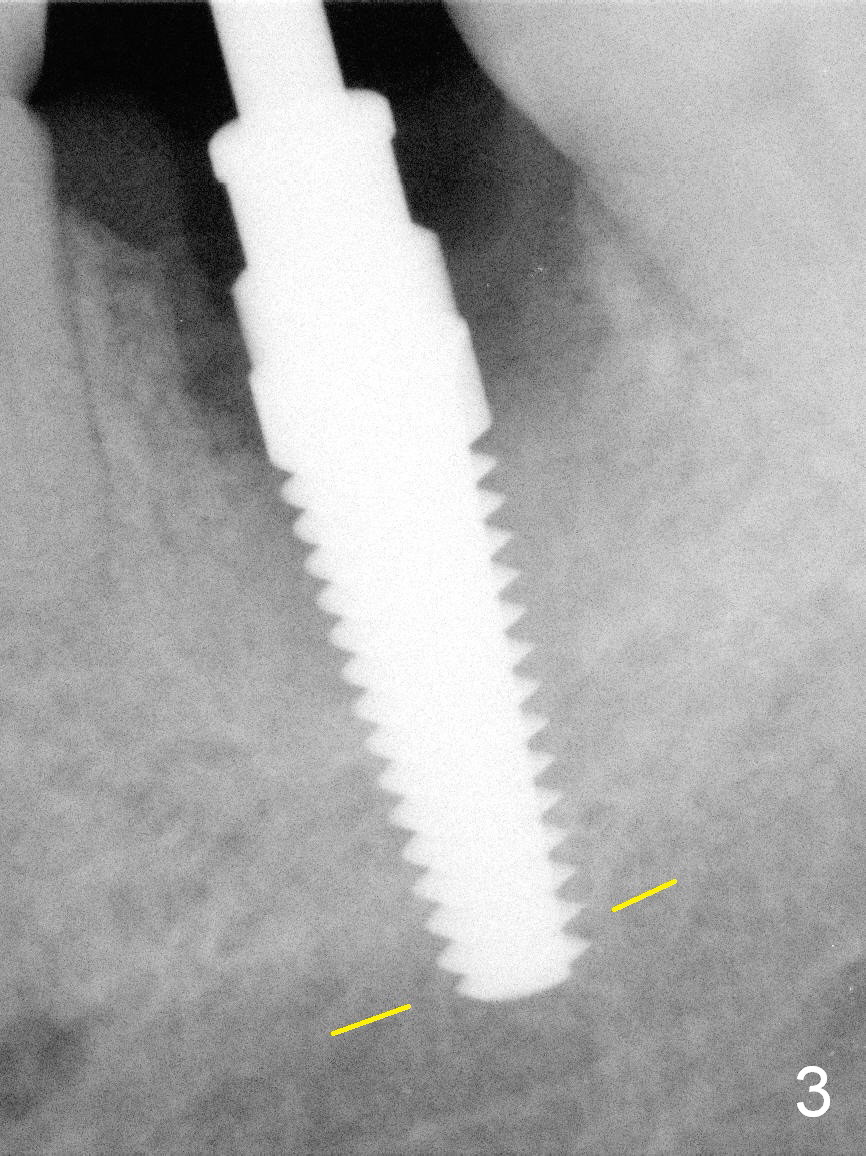
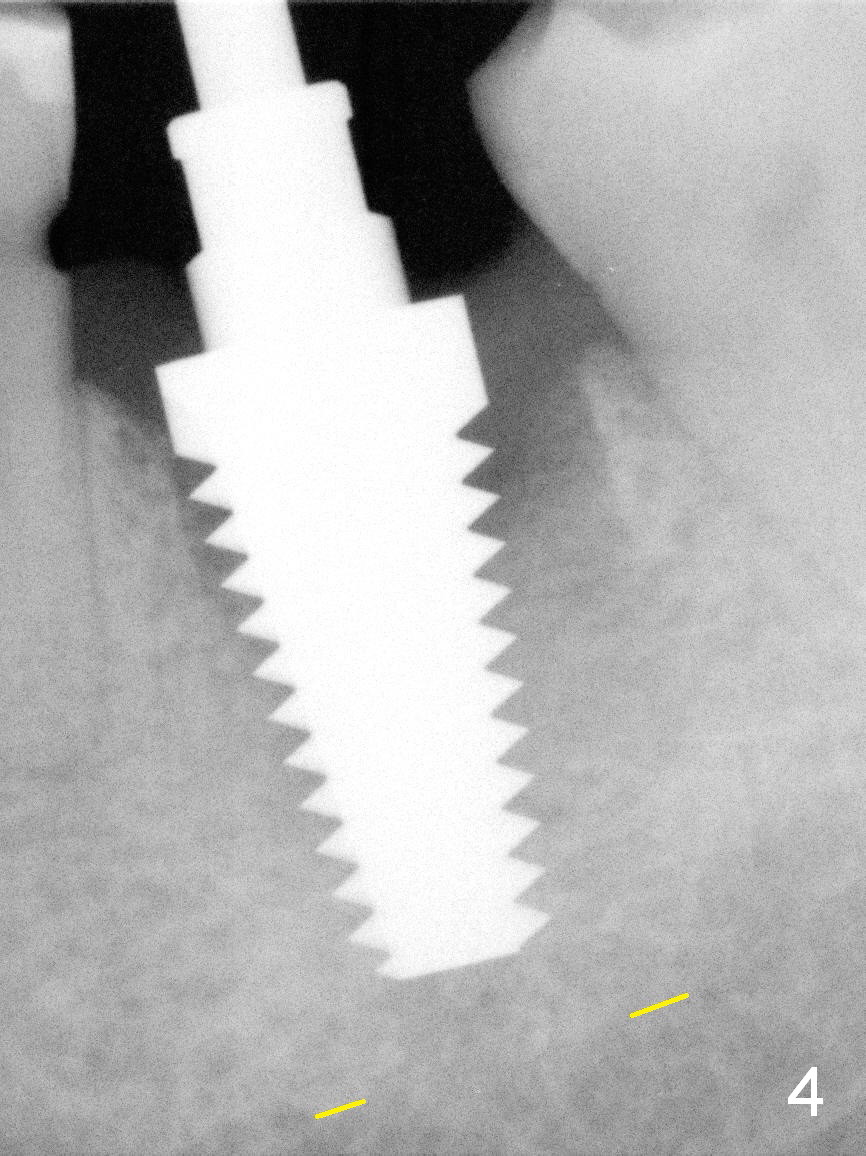
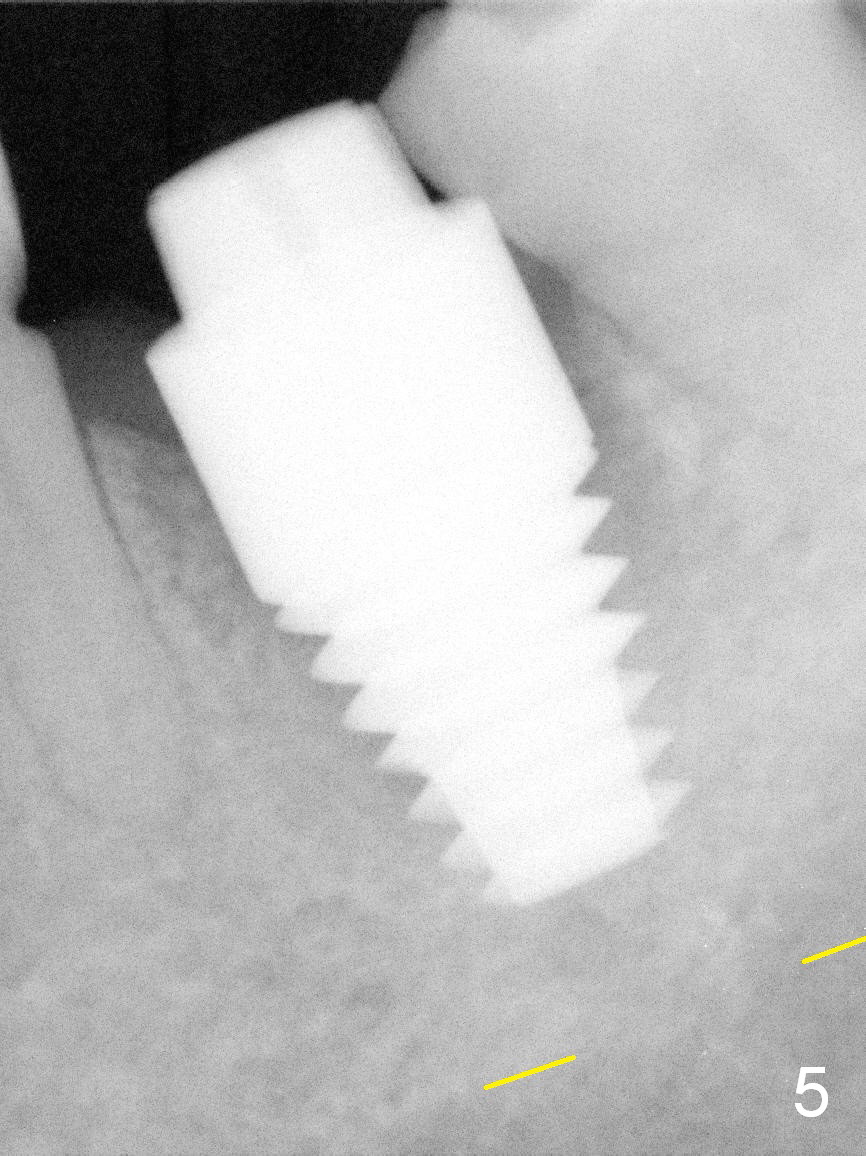
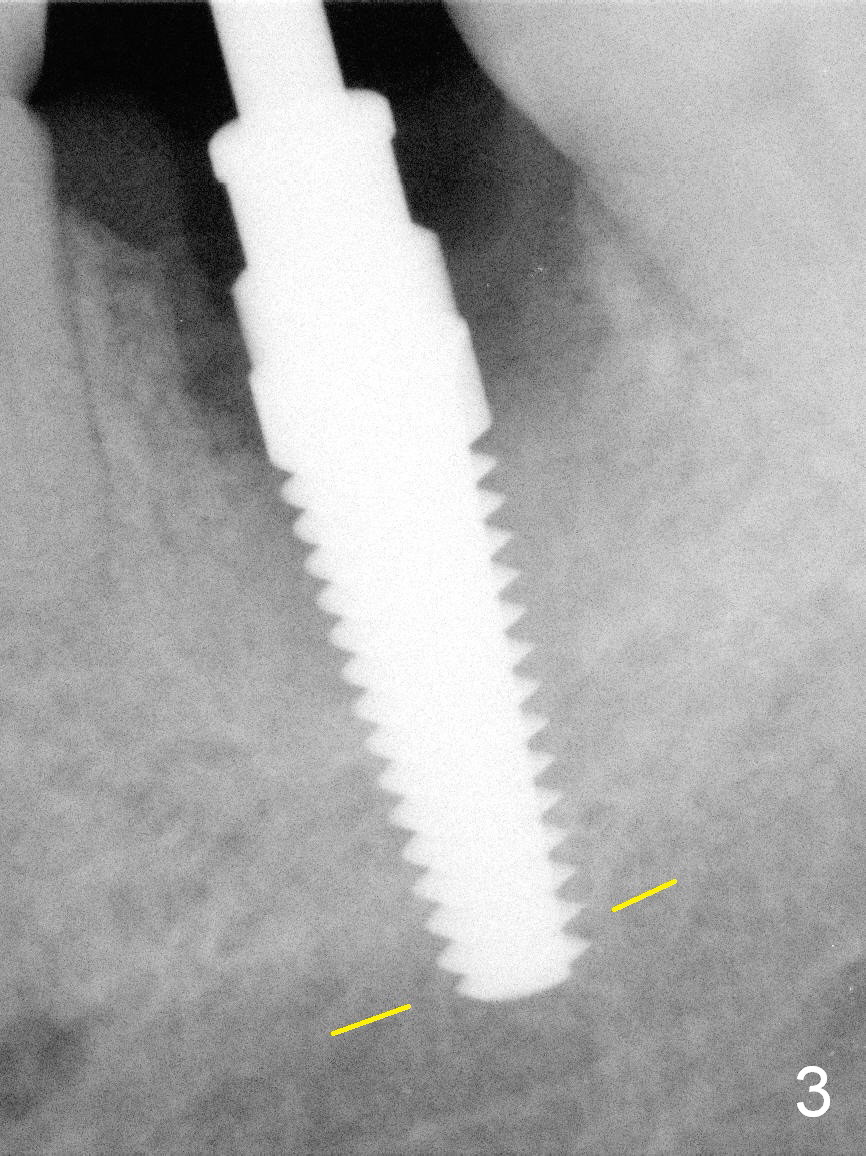
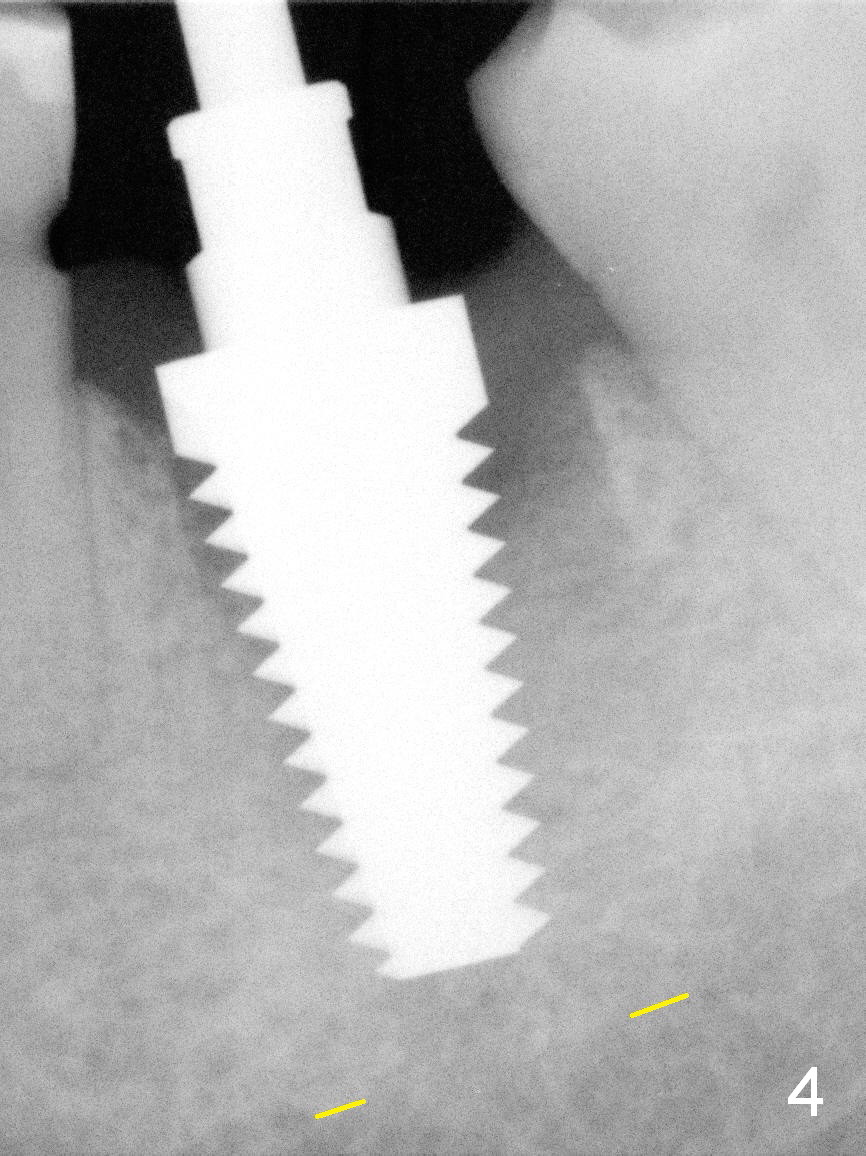
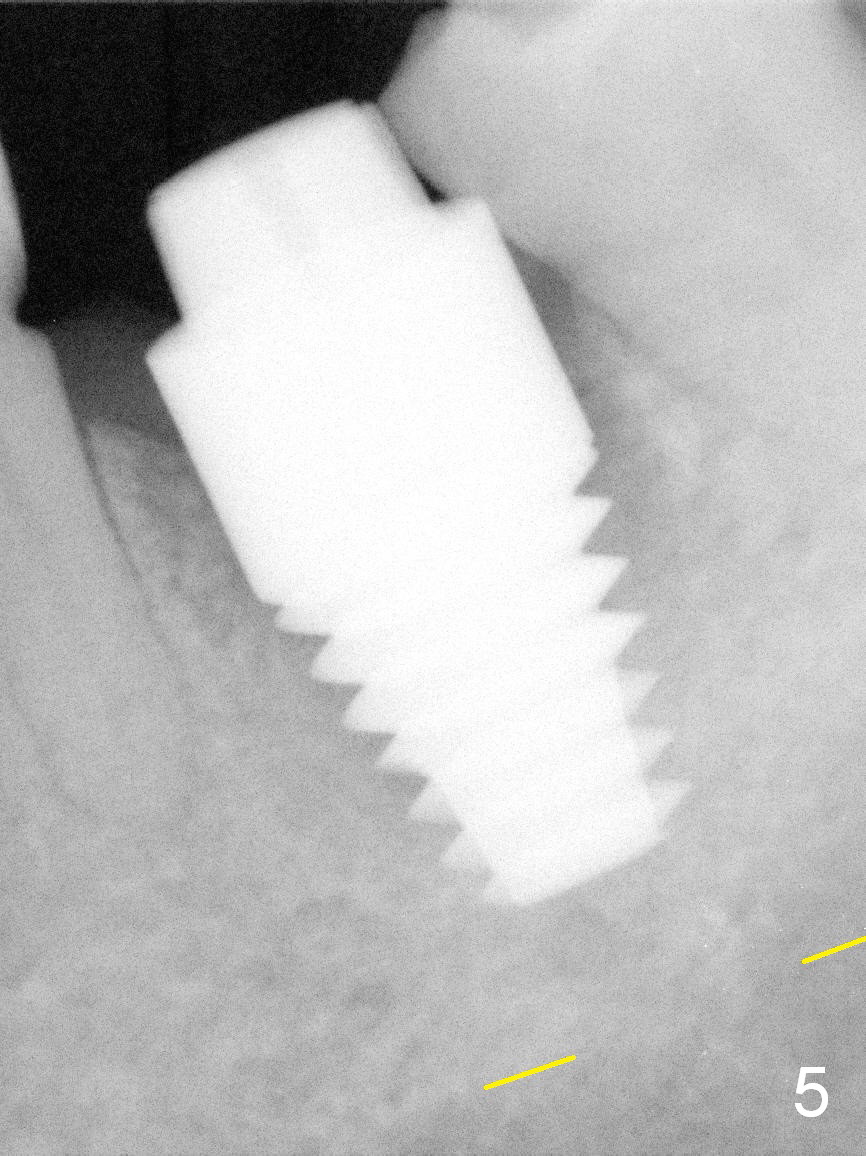
The patient reports that she has to keep the tooth #19 clean with Chlorhexidine to control the infection. When the tooth is extracted, the distal root is found to have been fractured with a large single socket (Fig.1). Furthermore, the socket is almost cylindrical apicocoronally (Fig.2). Common wisdom dictates obtaining apical new bone for primary stability. Due to the extensive lesion and the short statue and small mouth of the patient, the osteotomy turns out to extremely difficult: being too short initially (Fig.2), probably too long in the middle of the procedure (Fig.3) and having to be adjusted (Fig.4-6). Fortunately there is no paresthesia.
What is the solution? Quit implant placement and socket preservation? The patient is apprehensive and works out of state. She returns for surgery during Memorial holidays. It has taken 5 years to place her first implant after extraction.
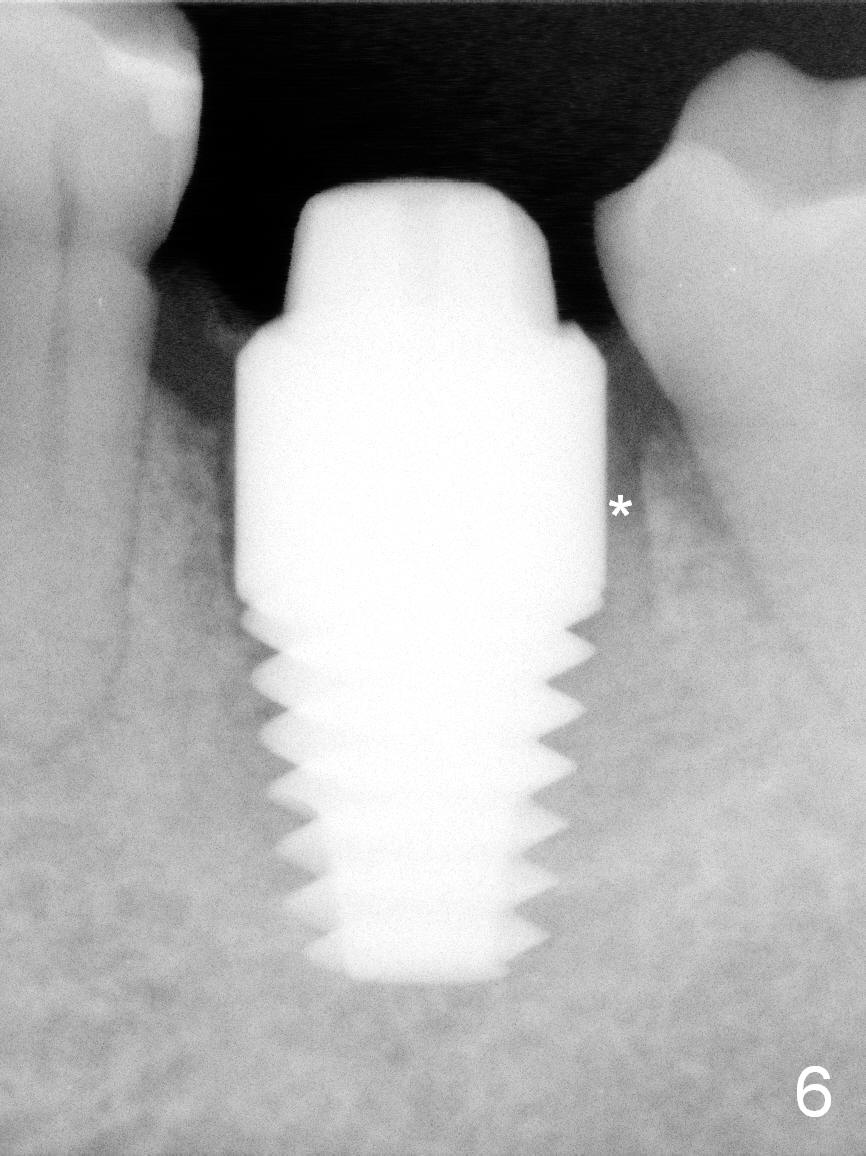
Prior to the afternoon implant case, No Drill approach is decided: the implant will occupy the whole length of the socket. However in surgery, it is almost impossible. The apical granulation tissue is too sensitive to be curetted or it is presumed to be close to the Inferior Alveolar Nerve. A large, but short tapered implant is used with primary stability. That is the Implant is Shorter than Socket! No new bone is required for primary stability.
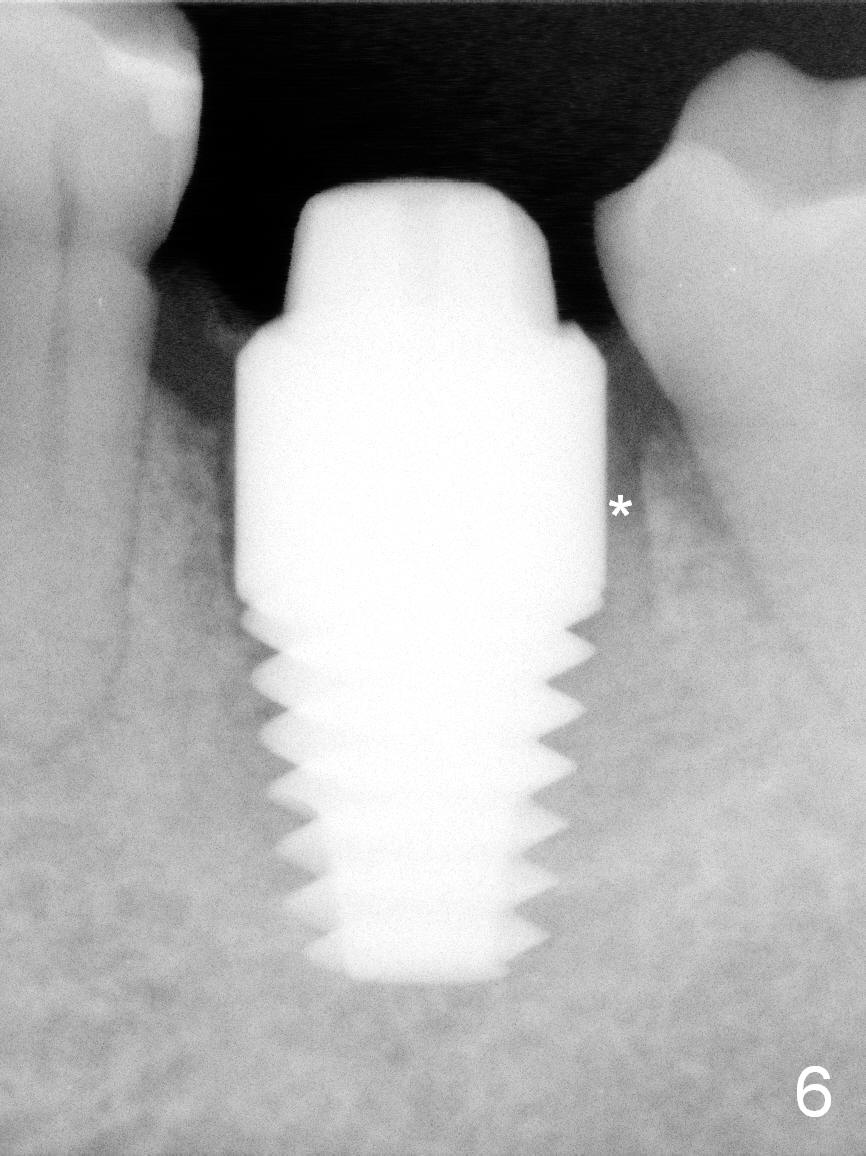
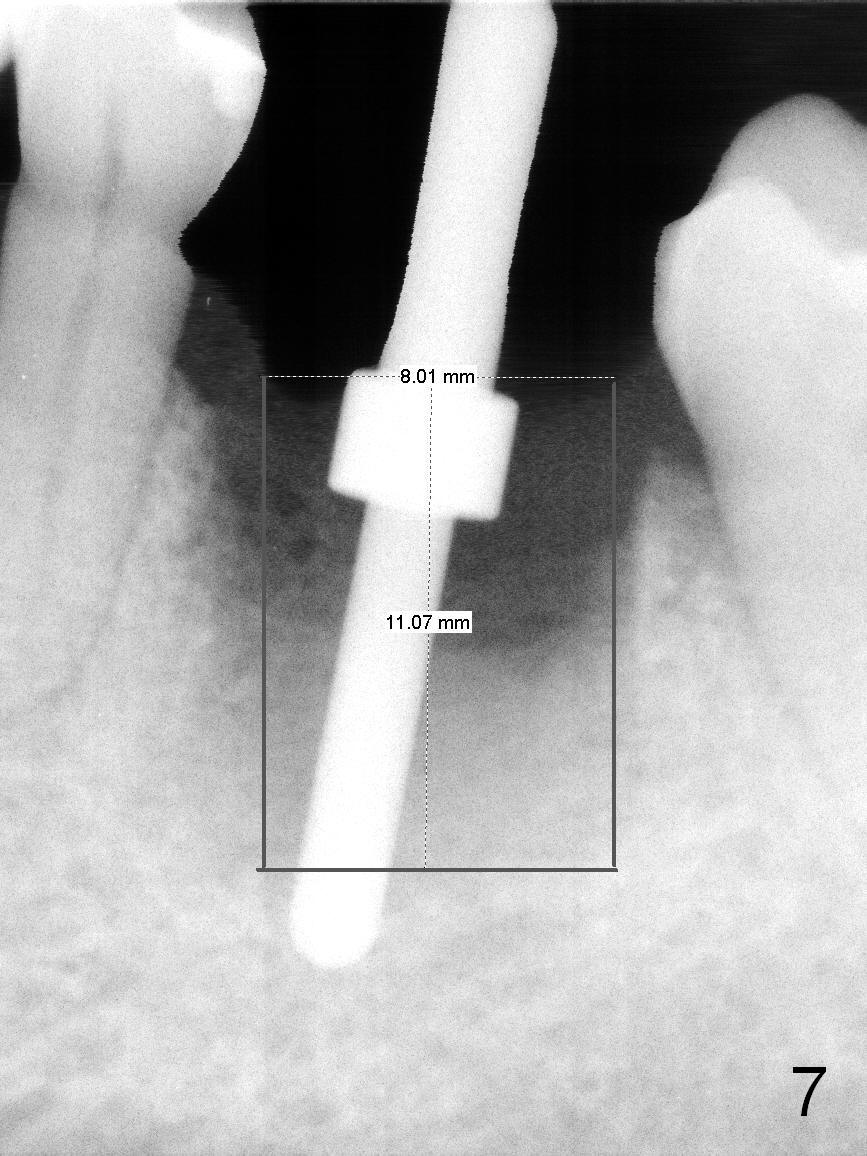
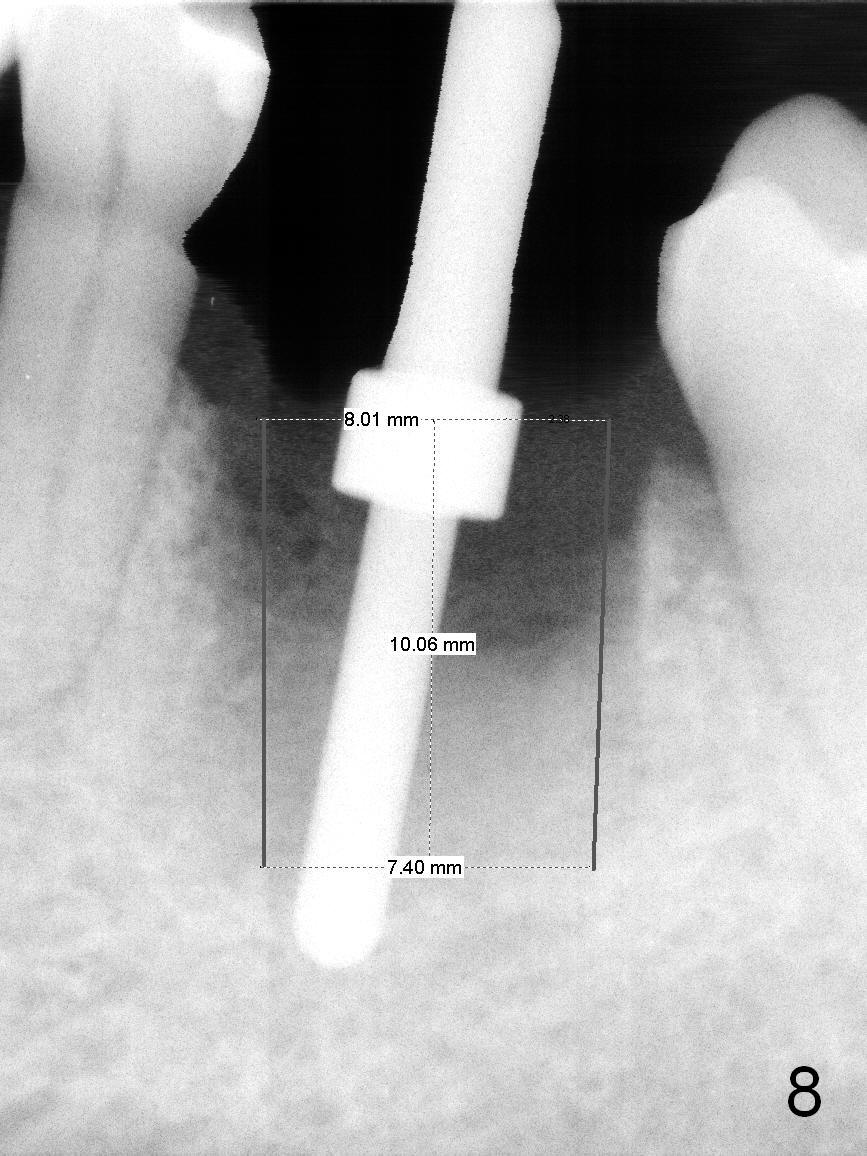
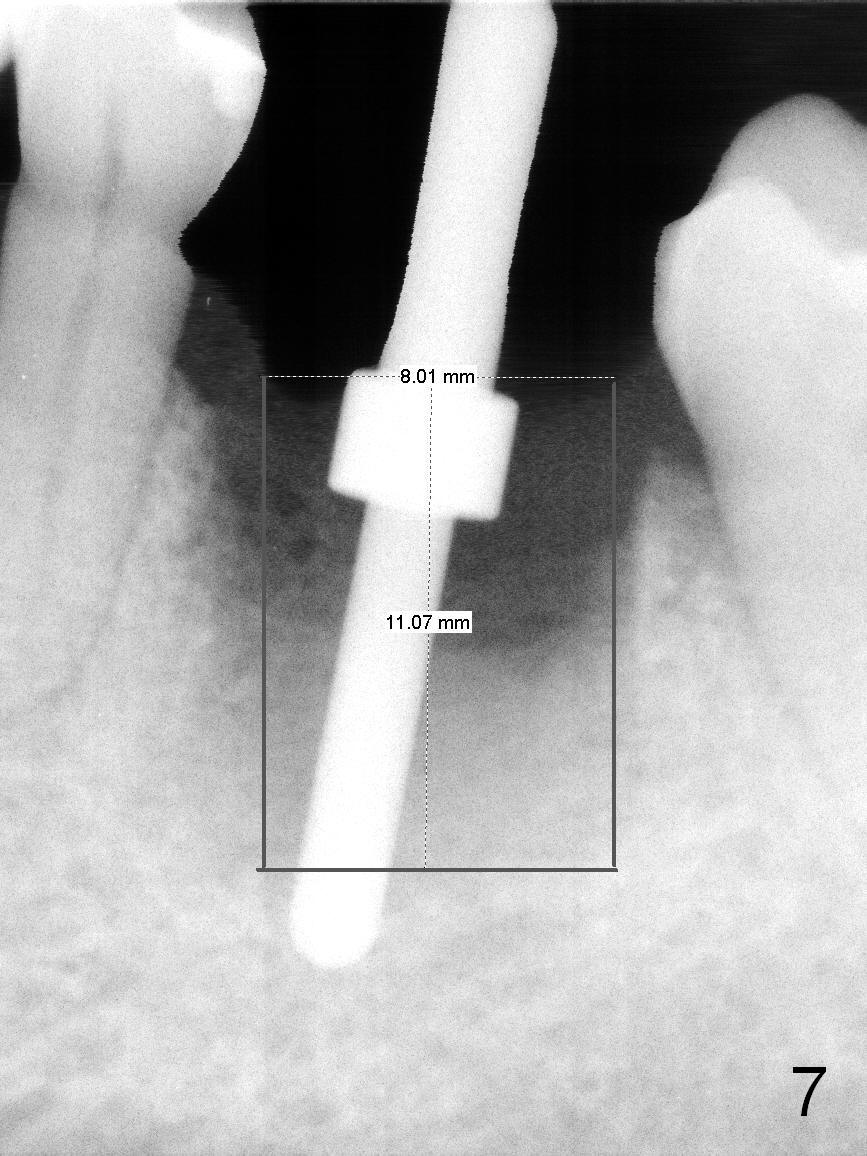
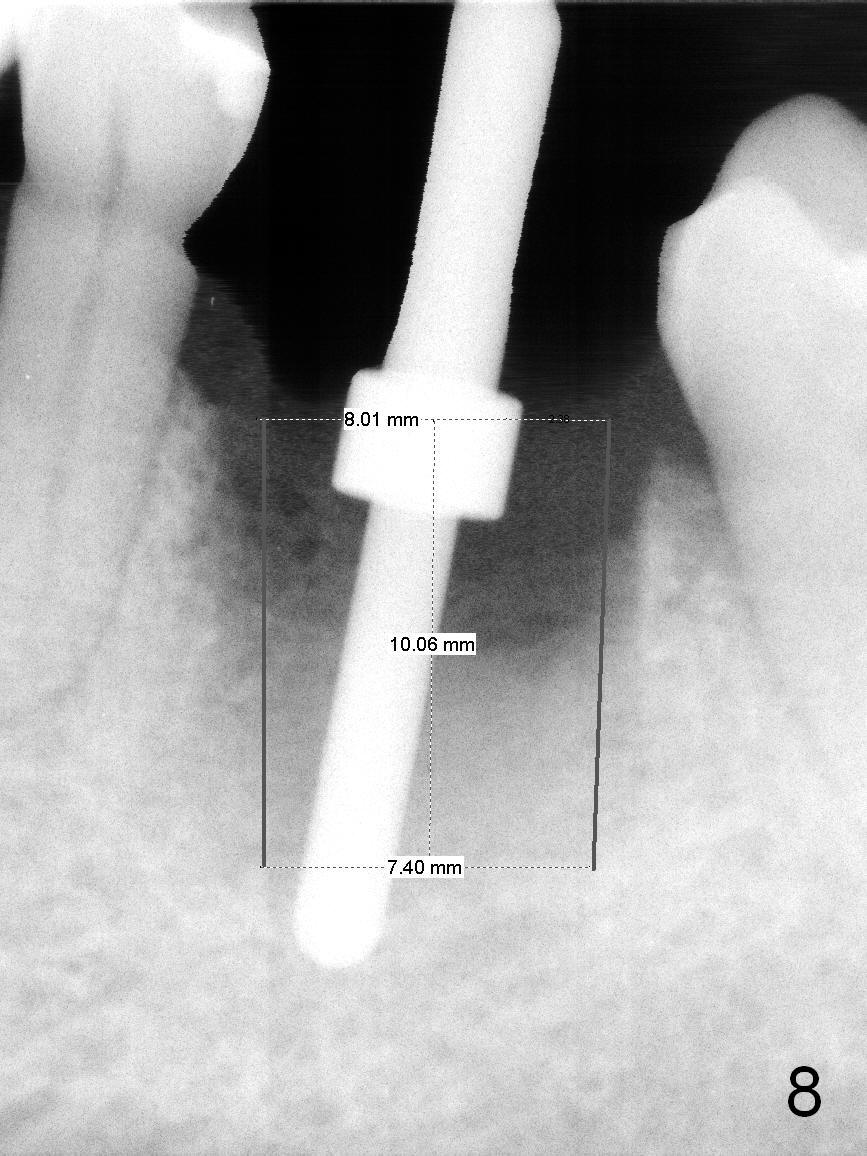
For safety, this case should have had a large cylindrical (Fig.7) or the least tapered (Fig.8) implant placed to occupy the cylindrical socket. The precaution to be taken for the large non-tapered implant is to protect the buccal plate while it is being placed. Lean the implant as lingual as possible. Bone graft if necessary.
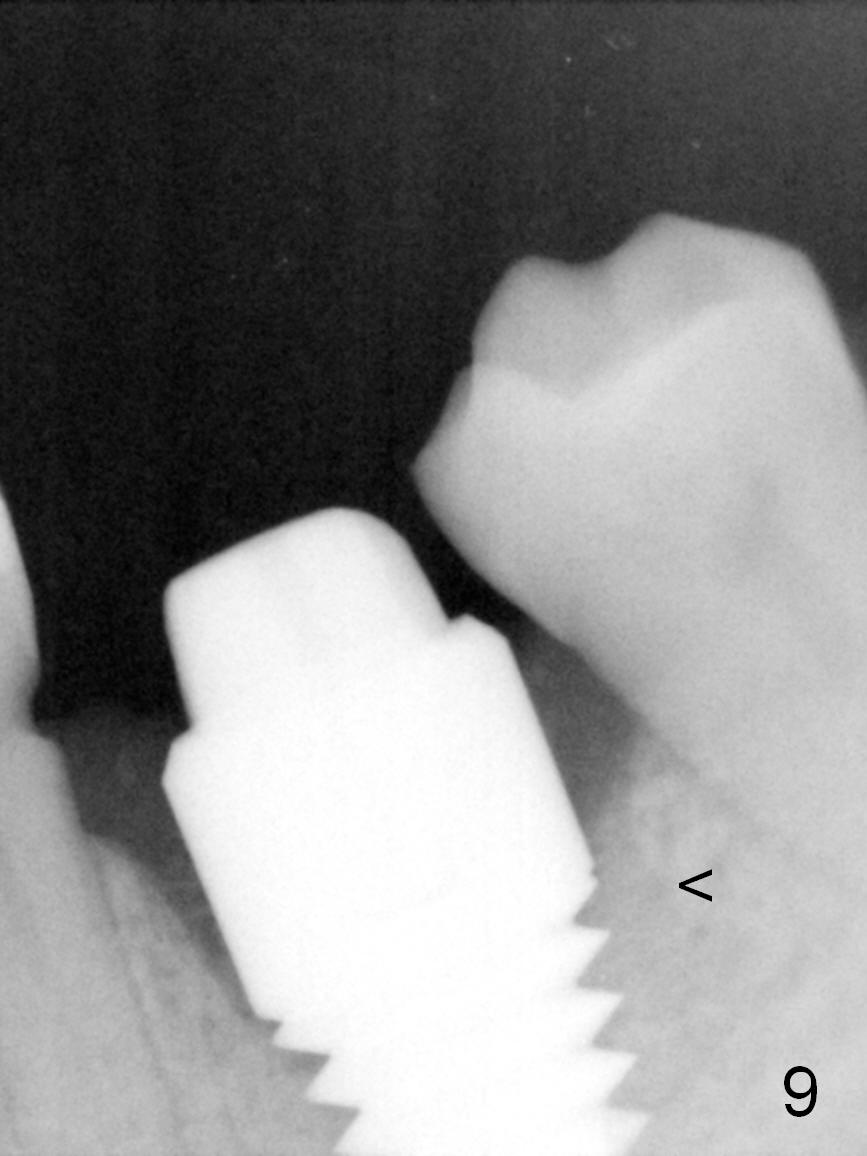
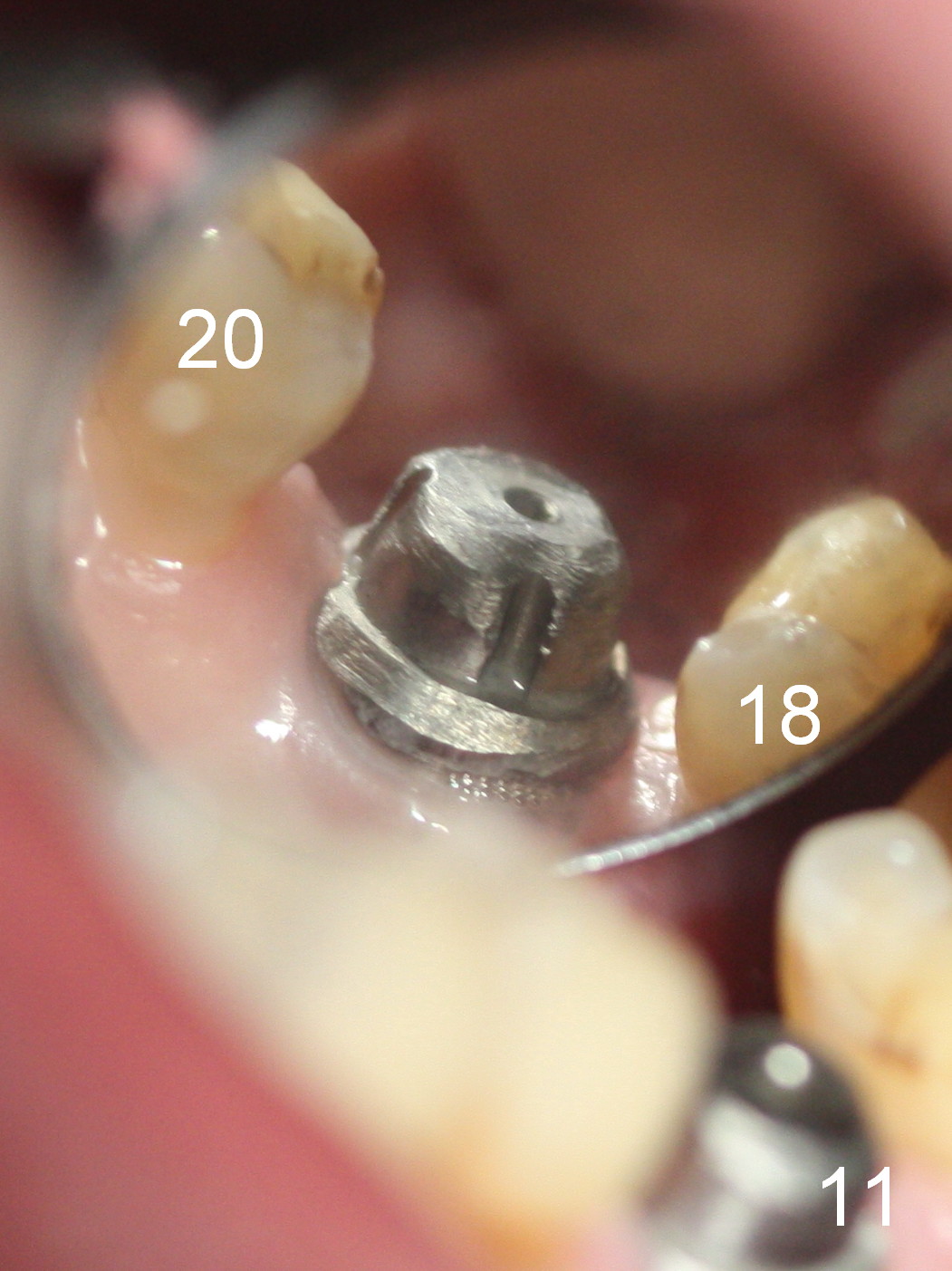
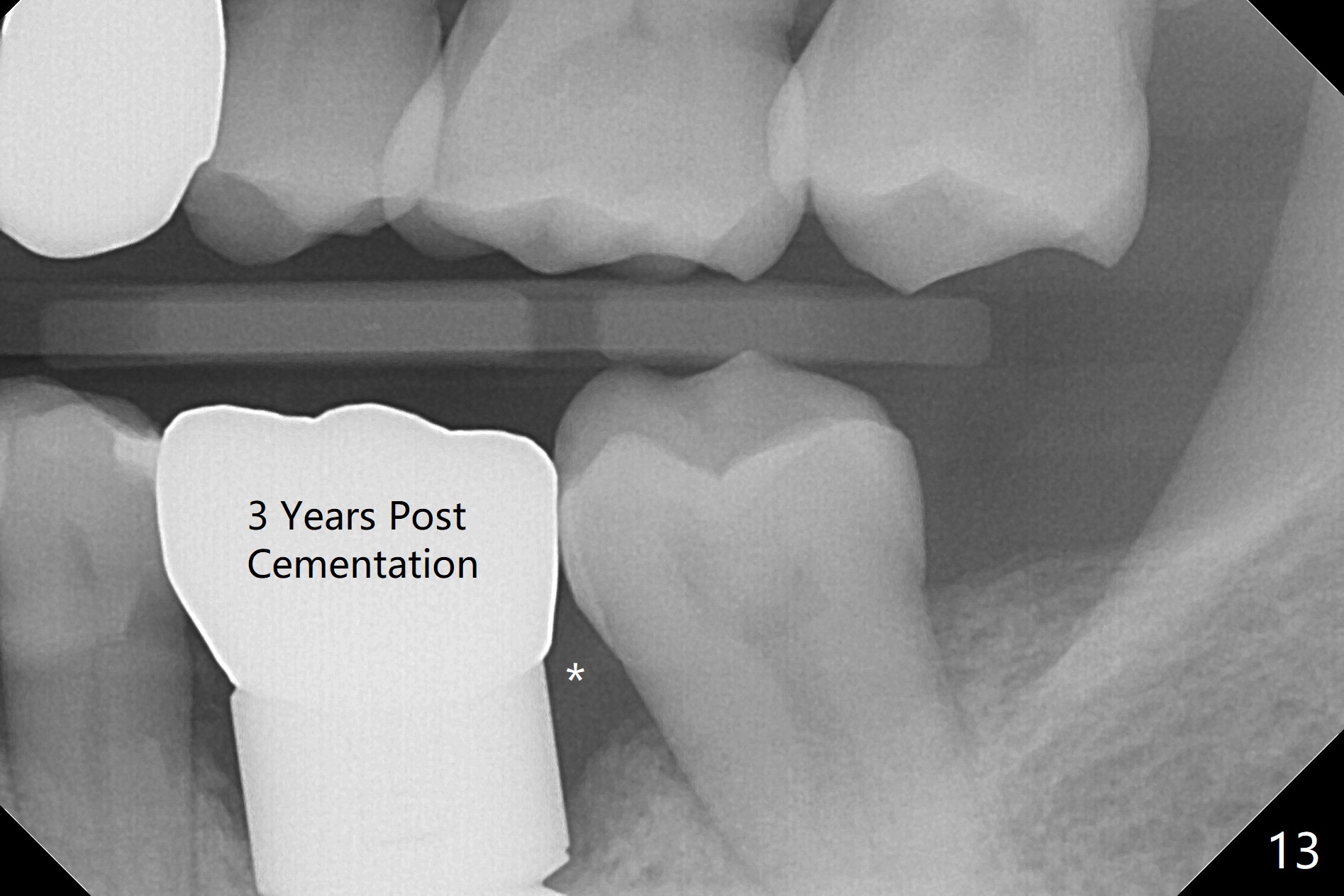
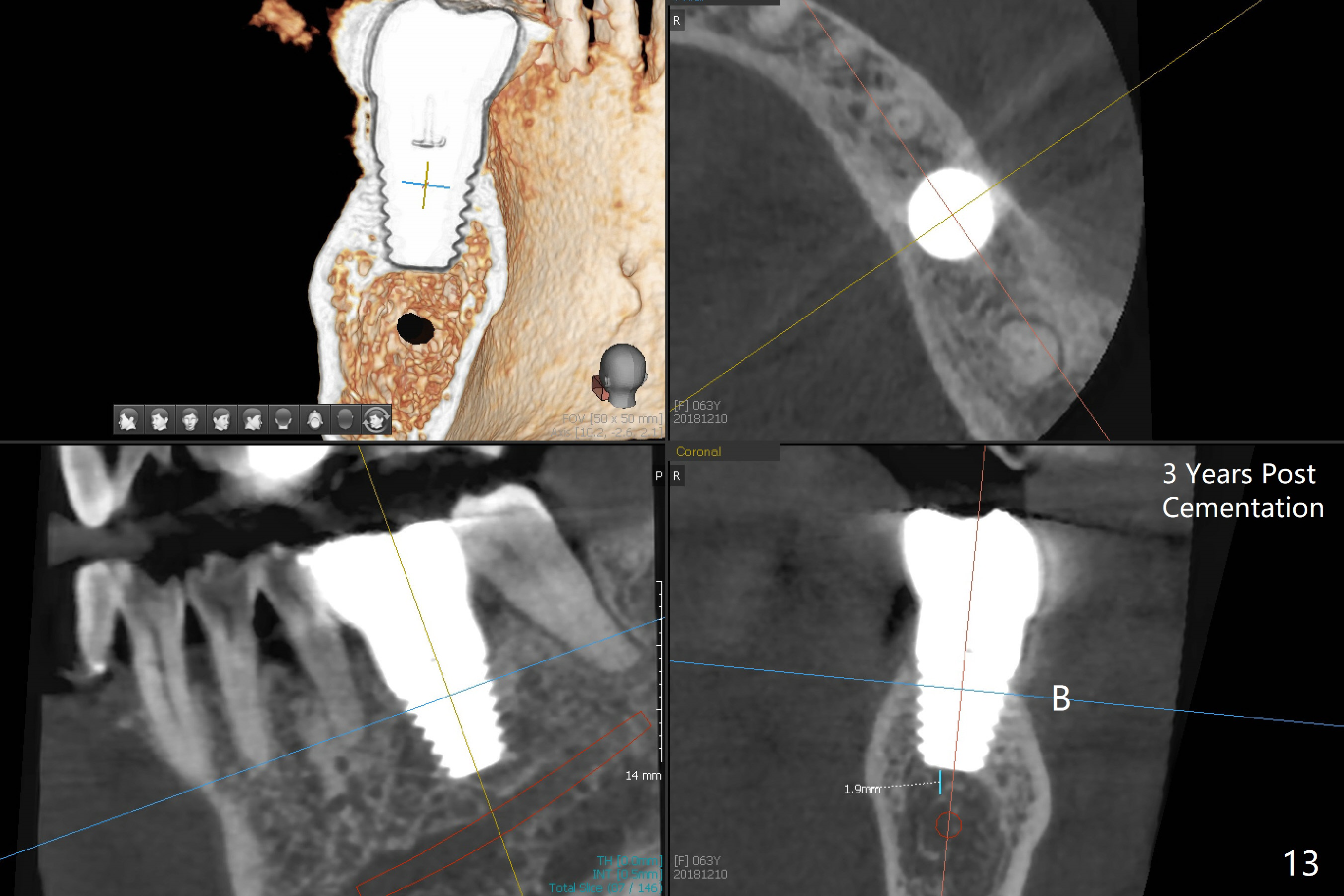
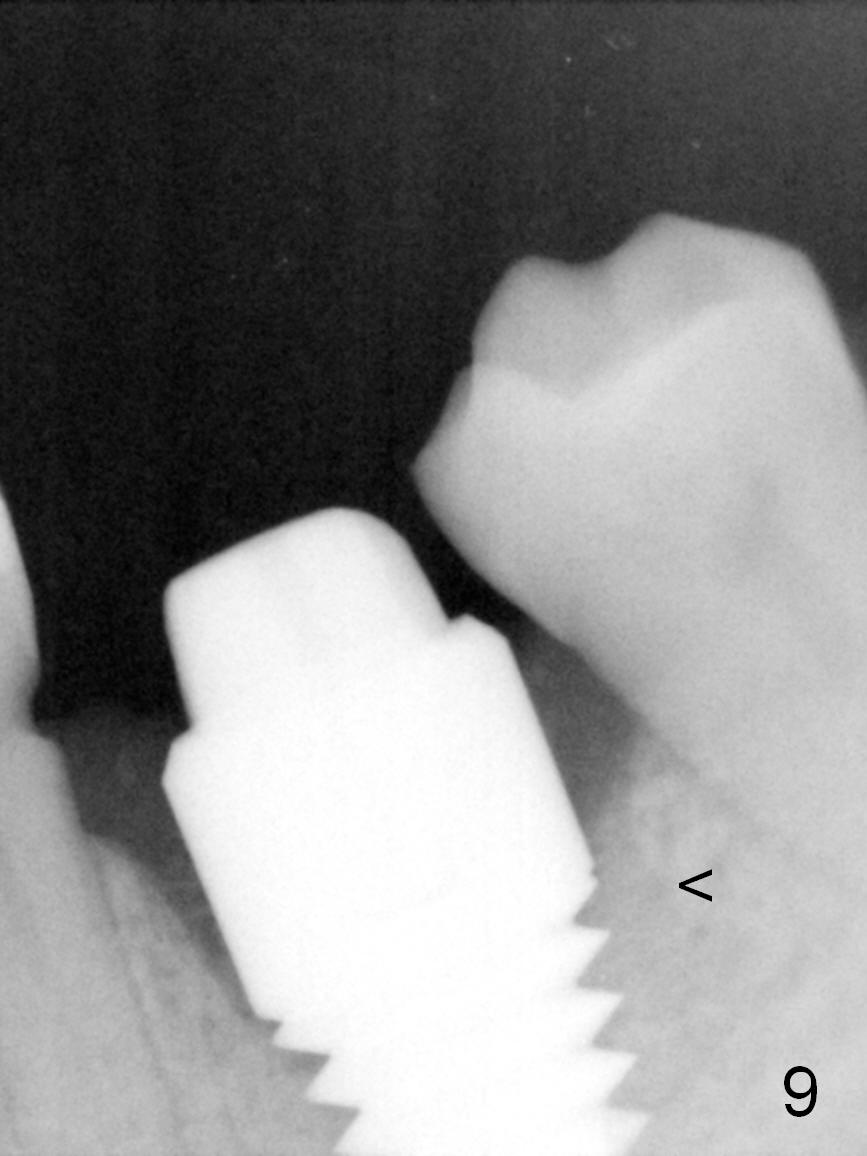
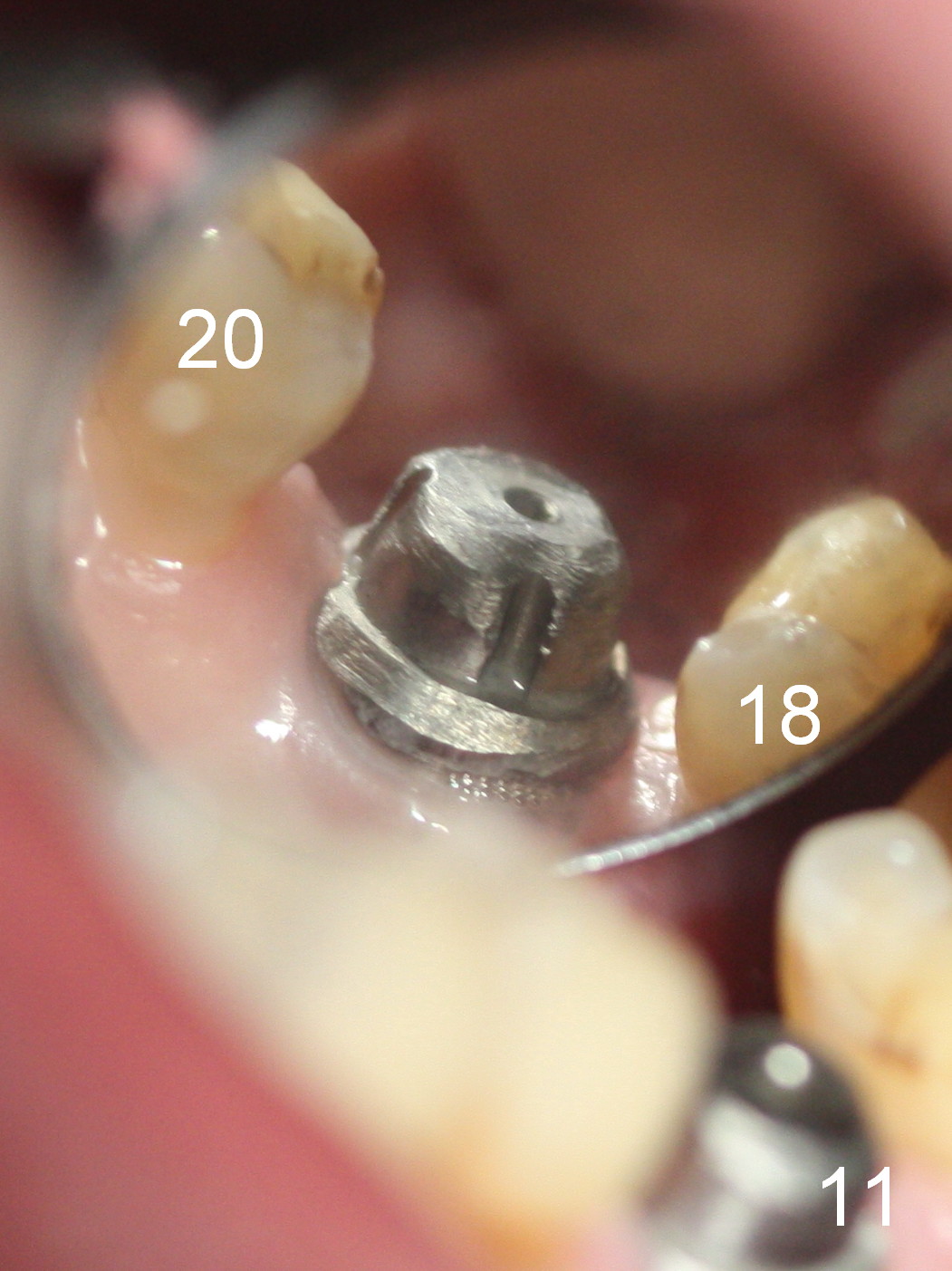
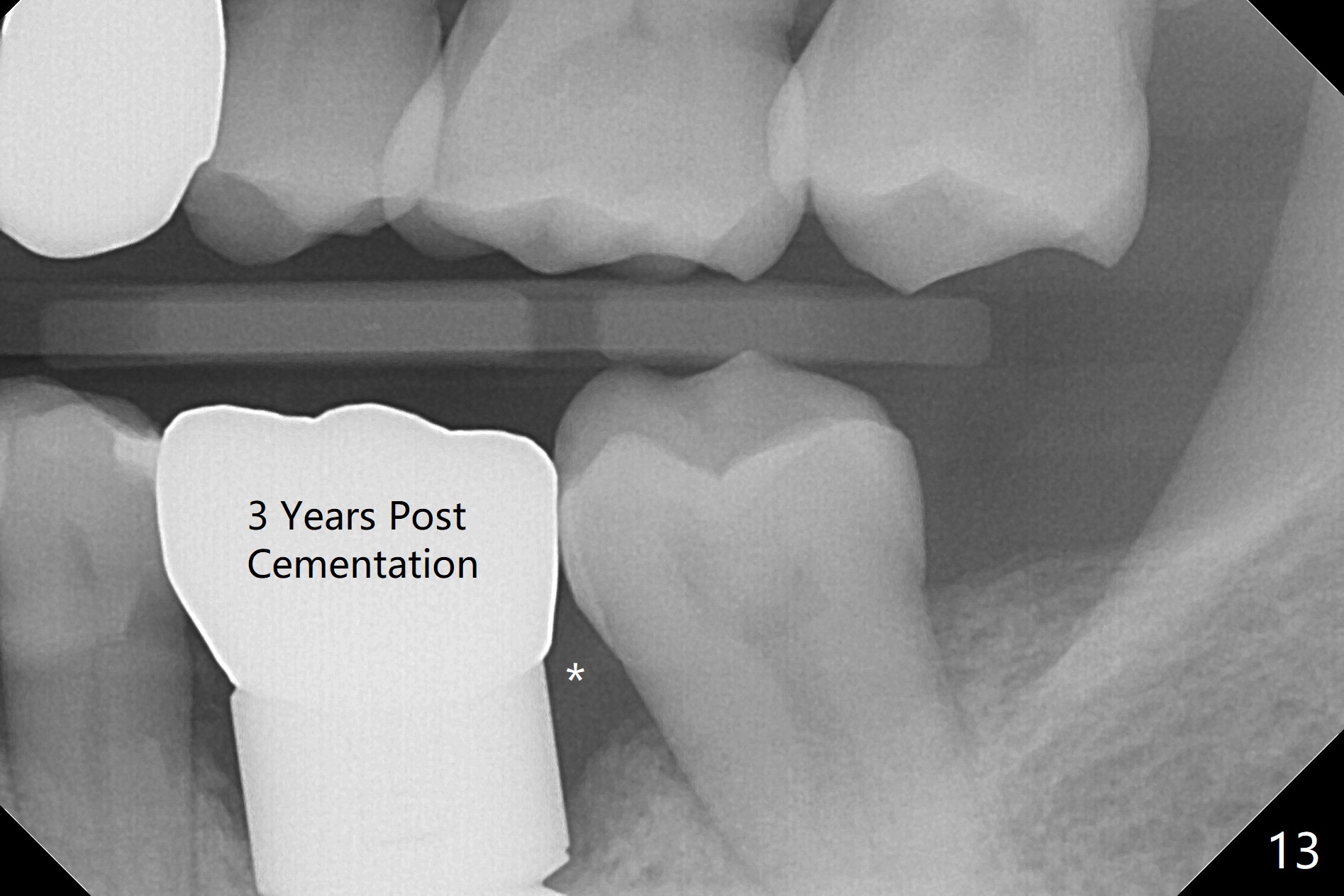
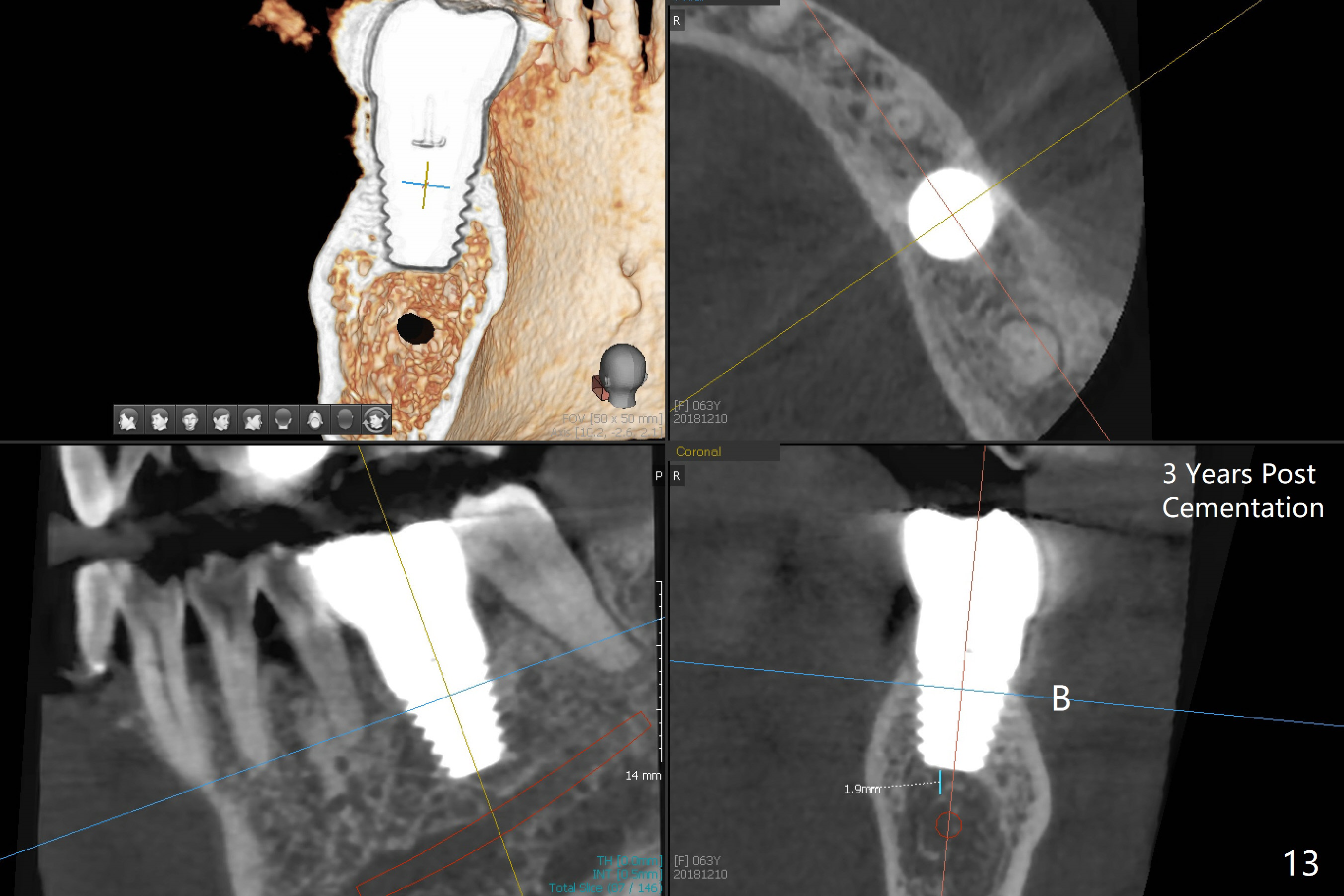
The distal gap appears to close 2.5 months postop (Fig.9 <). The buccal (Fig.10) and lingual (Fig.11) gingiva is healthy and keratinized (*). The implant is ready for restoration. The mesial margin is slightly subgingival (Fig.11). After prep, the margin is lower than what is shown in Fig.10.11. Trim a little bit of gingiva from the mesial papilla (in model). Take one more look at the model (Fig.12, 2.5 months postop) to appreciate the gingival cuff (*) due to the large implant (I). The patient complains of distal food impaction with infection ~ 1 week earlier. Although the contact is within normal limit, there is a large distal gingival embrasure (Fig.13 *). Clinical exam reveals tenderness over the buccal gingiva, although there is not much buccal thread exposure (Fig.14 B). Water pik is recommended. The existing crown will be removed for provisional with deeper distal margin and good contour.
Return to Lower Molar Immediate Implant, Technicians Xin Wei, DDS, PhD, MS 1st edition 05/21/2015, last revision 12/11/2018