

 |
 |
||
 |
 |
 |
 |
How to Debride Infected Socket Close to Inferior Alveolar Nerve
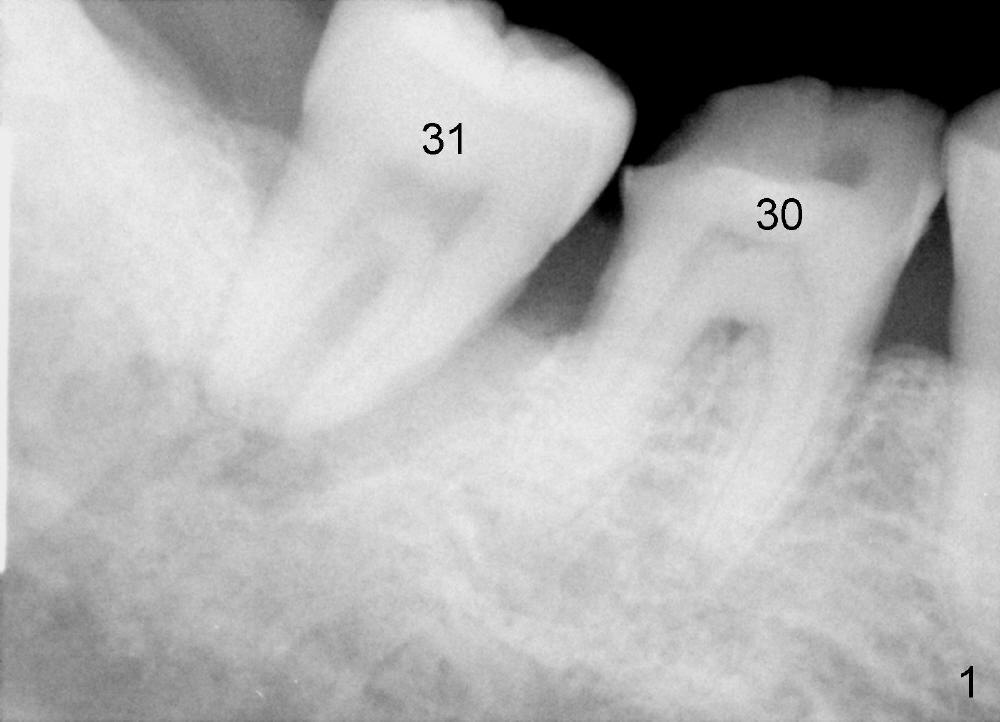
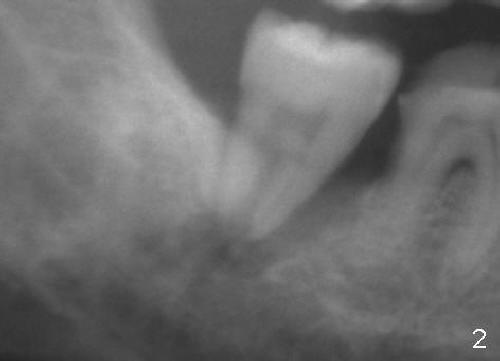
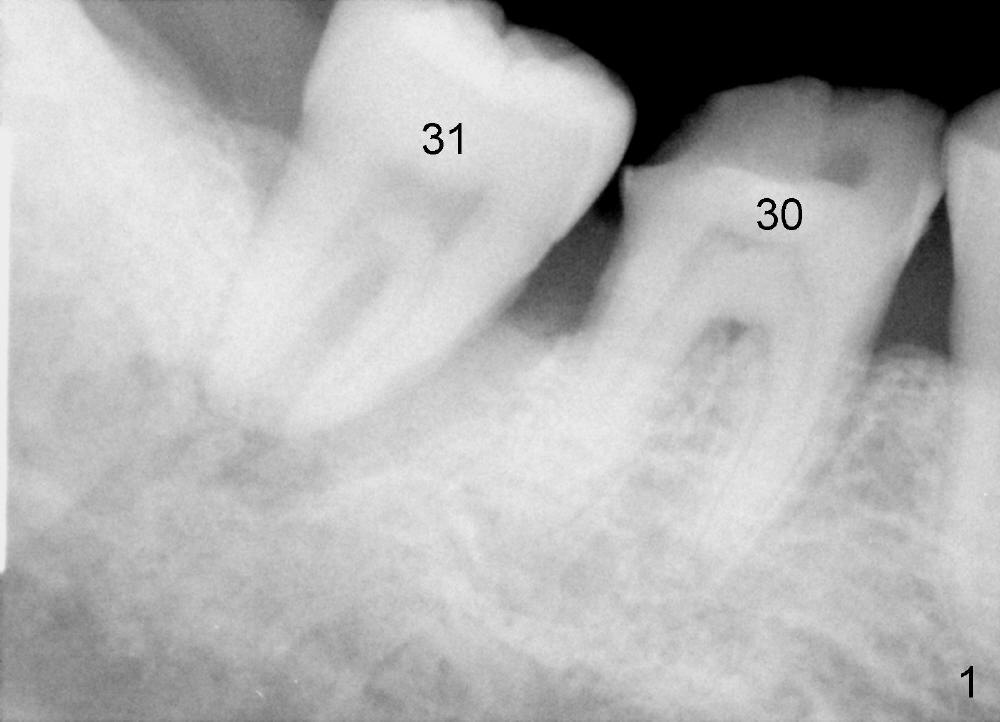
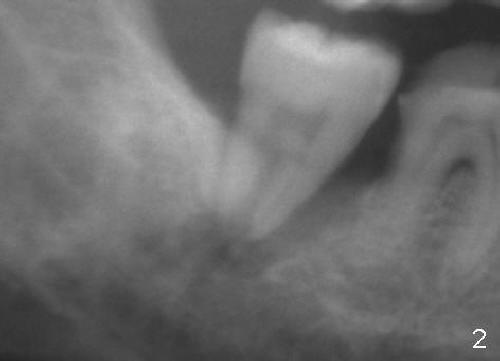
A 44-year-old man has had infection at the site of #31 for 6 months with history of chronic periodontits and possible traumatic occlusion (as suggested by severe wear of the tooth #30 in Fig.1). Fig.2 is an image from a panoramic film. Fig.3 (from Fig.1) shows that the large periapical radiolucency (red dashed line) extends apically toward the upper border of the inferior alveolar canal (yellow dashed line).
How to debride the socket without damaging to the nerve? First, infiltration anesthesia is administered with 4% Articaine with 1:100,000 Epinephrine. Intraligamnetal injection should not be used as the first line of action, since it may anesthetize the nerve if the upper border of the inferior alveolar canal has been perforated by the infection. Second, carefully approach and debride the apical portion of the socket once the tooth is extracted. If the access is limited, the distal wall of the socket will be trimmed, as shown by Fig.4 black dashed line.
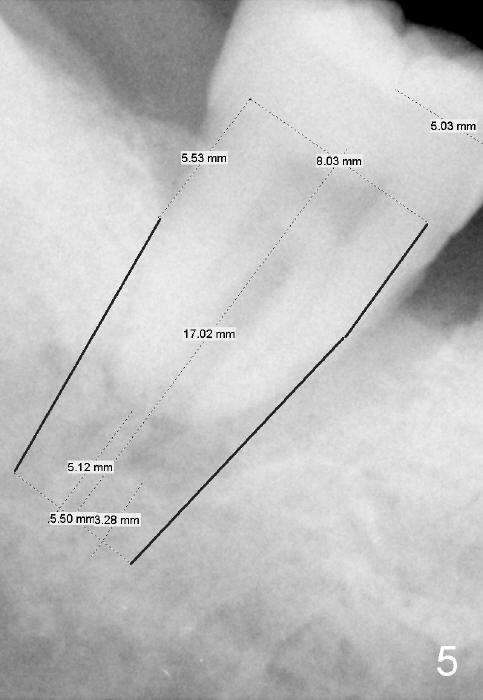
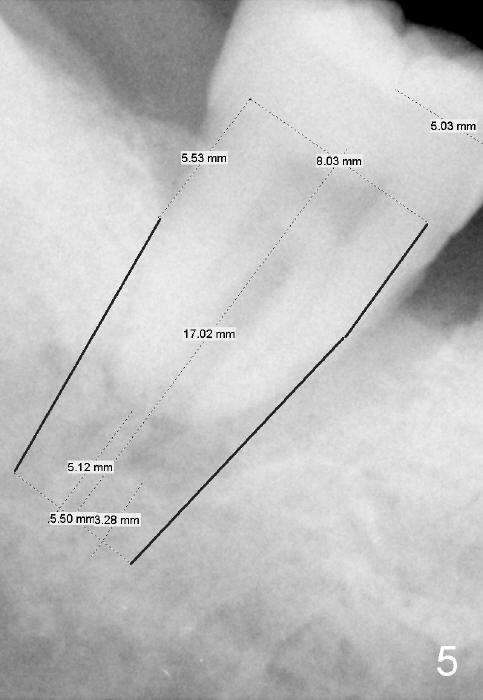
If there is any doubt about the depth of the socket as related to the nerve, take PA with or without a drill or paralleling pin.
Do not over debride the socket. Use gauze for pressure hemostasis. If there is risk of injury to the nerve, close the socket with collagen plug with or without bone graft.
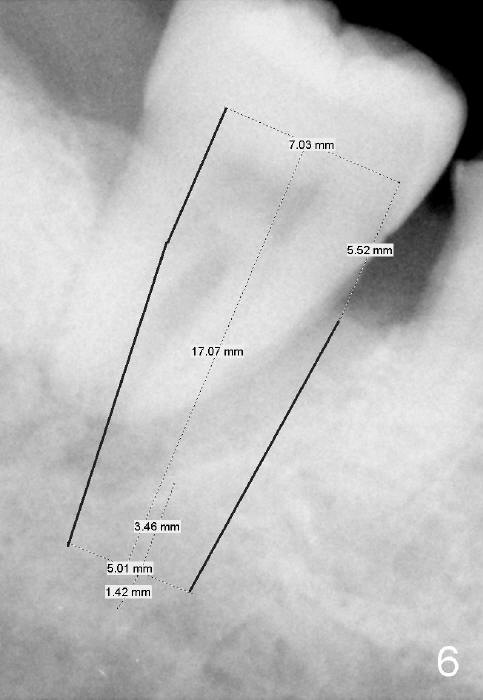
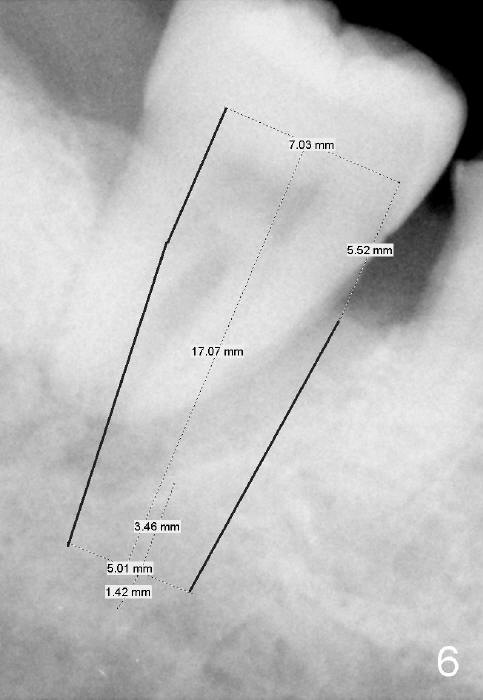
If the socket is thoroughly debrided, start osteotomy in the mesial slope of the socket (Fig.6 vs. 5). Depth is approximately 3 mm. Find a reliable landmark for the depth, gingival margin or alveolar crest. Surgery is finished as planned.
Return to Lower Molar Immediate Implant
Xin Wei, DDS, PhD, MS 1st edition 09/15/2014, last revision 09/16/2014