



 |
 |
 |
 |
 |
 |
 |
 |
Reversal of Paresthesia
Four days postop, the patient returns to clinic with chief complaint "tingling of the bottom right teeth". Exam reveals paresthesia (Fig.1). After removal of perio dressing, the infection has disappeared (Fig.2 *). Without local anesthesia, the implant is reversed for 3 times with minimal discomfort when torque wrench is set at 60 Ncm. As expected, the patient apparently feels that the paresthesia decreases. Then the torque wrench is set at 50 Ncm; the implant is turned 2 more times. The implant is apparently stable (Fig.3). The patient is discharged with postop instruction: continuing oral Amoxicillin and Medrol Dose Pak.
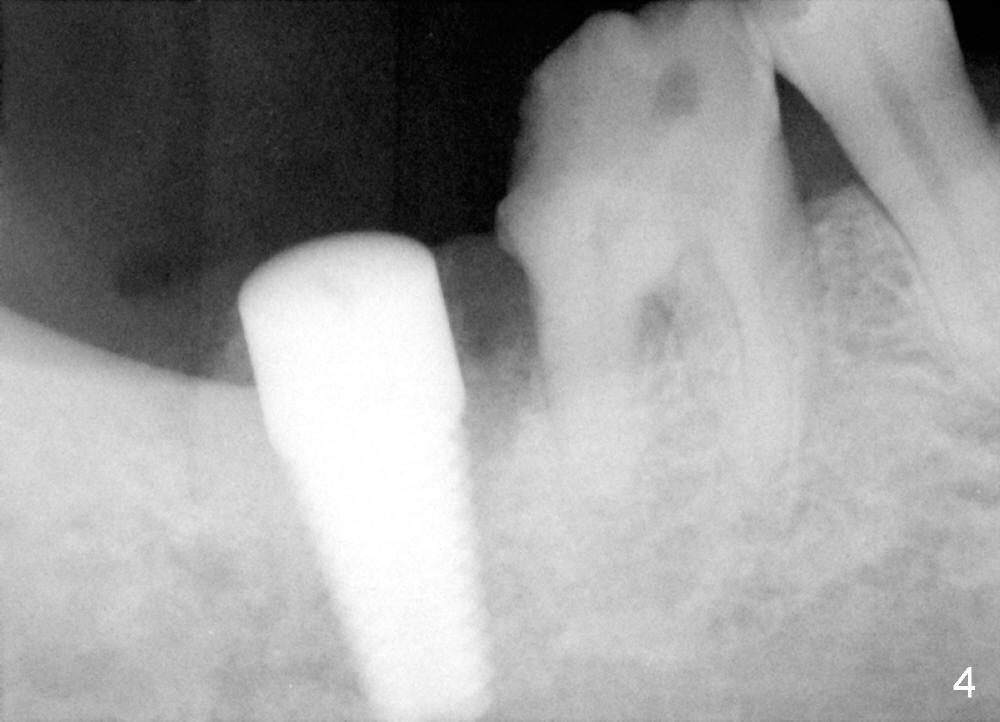
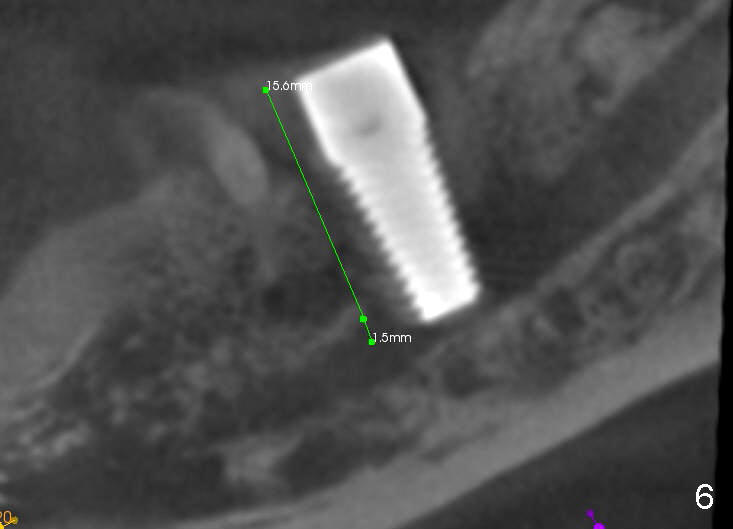
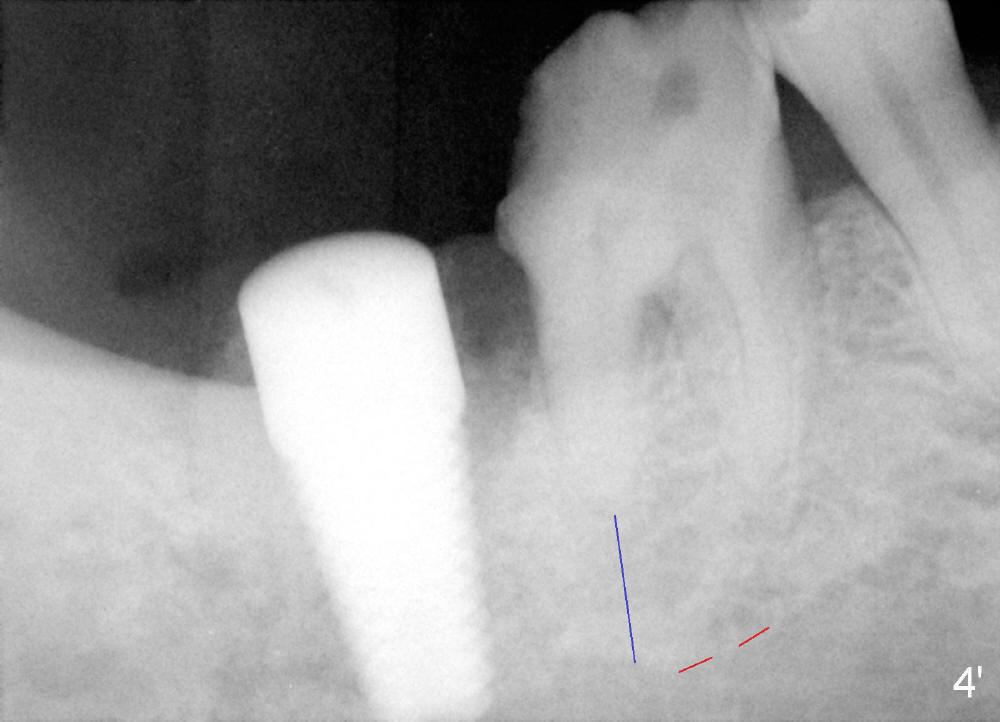
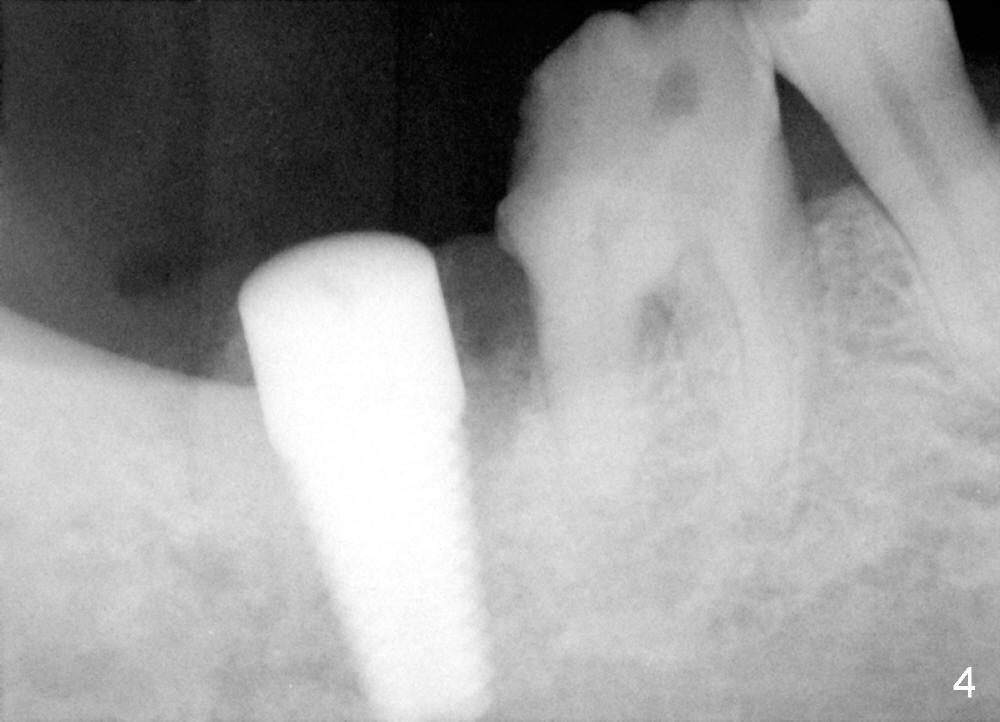
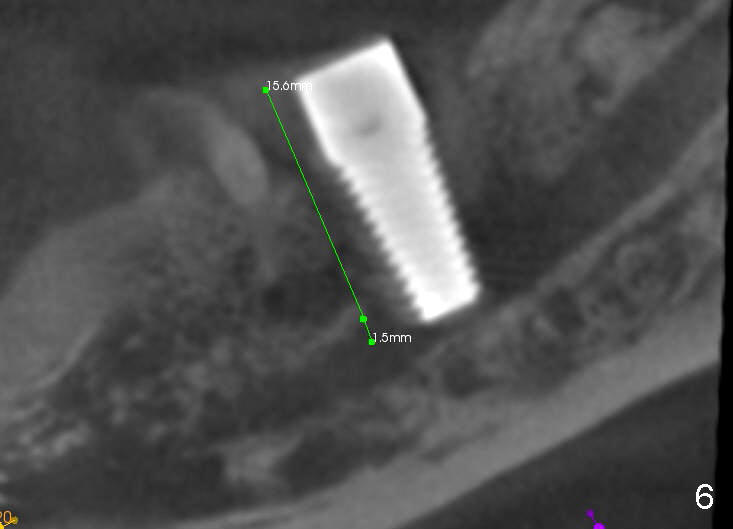
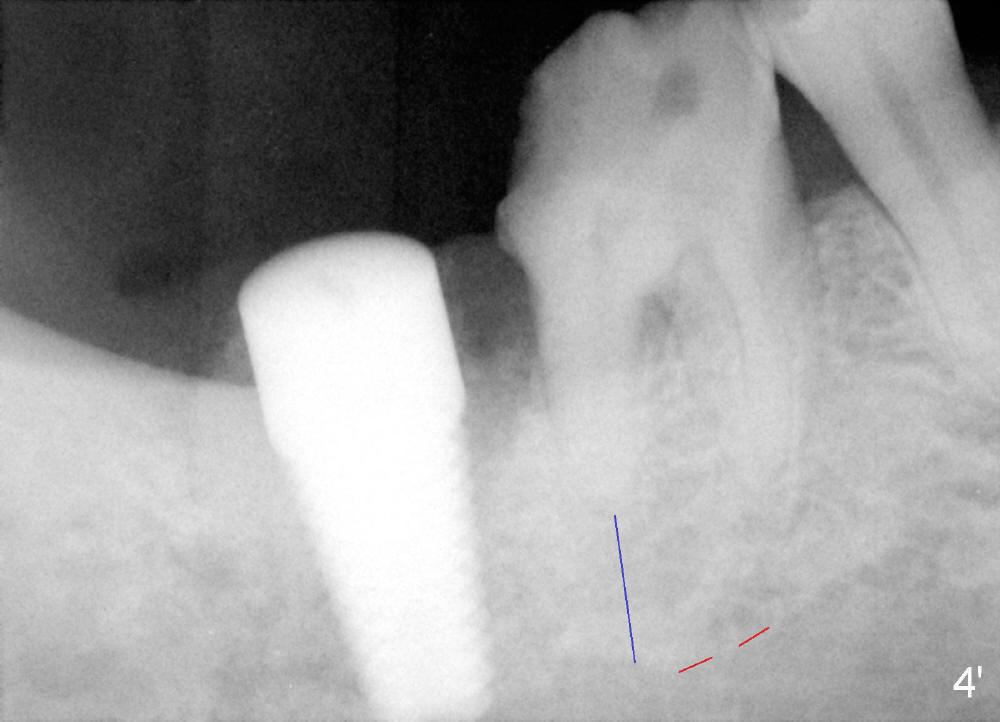
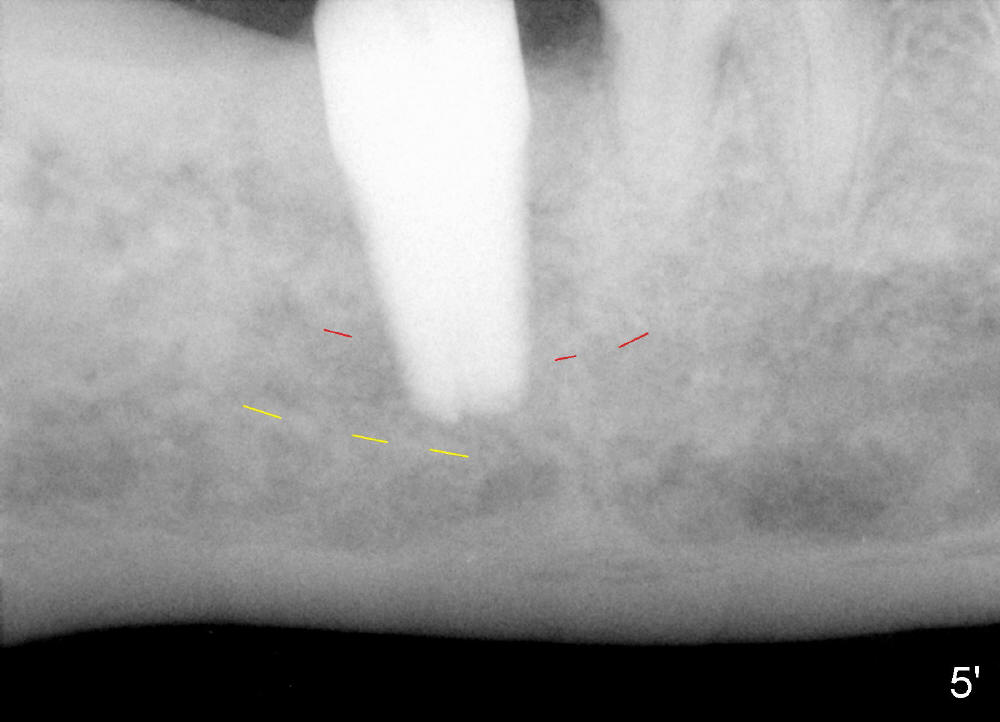
The patient returns 2 days later with the same sign and symptoms. Two PAs are taken without definitive information (Fig.4,5). CBCT is taken the following day (Fig.6). Under local anesthesia, the implant is backed up. It loses stability. A 8x14 mm tap is tried in without binding. Allograft is placed and collagen plug is used.
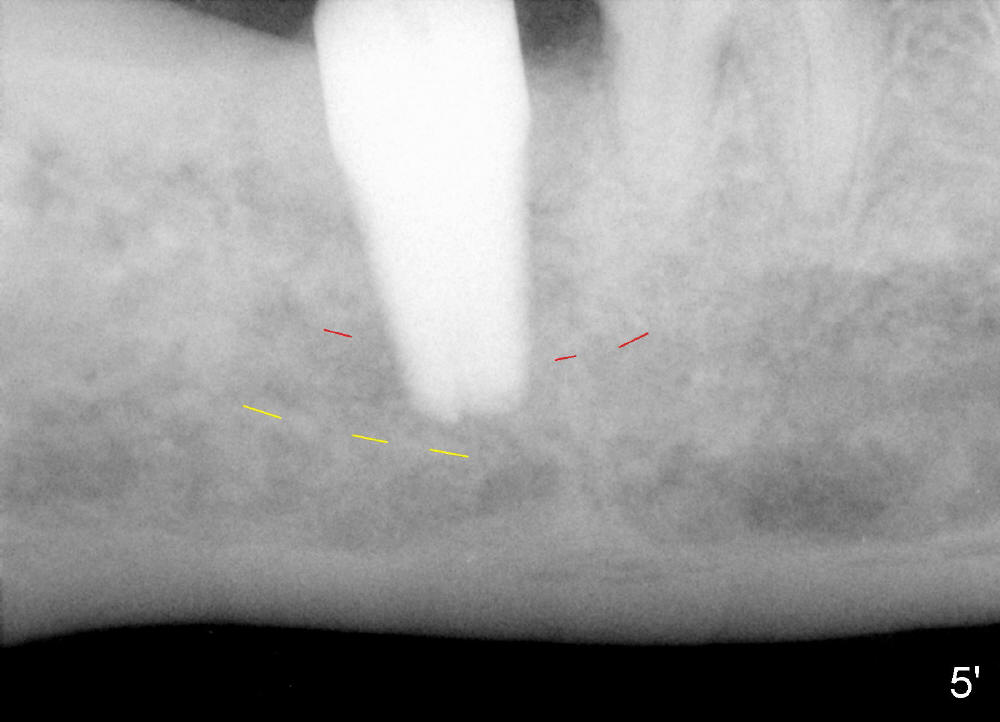
From this case, it appears that the upper border of the inferior alveolar canal may be ambiguous from regular X-ray (Fig.4',5' red lines). In this situation, CBCT should be taken. The 2nd line of defense is pain encountered in osteotomy. Do not administer block anesthesia. Osteotomy depth should be controlled tightly, not too far away from the apices of the 1st molar (Fig.4' blue line), another anatomic landmark.
Return to Lower Molar Immediate Implant
Xin Wei, DDS, PhD, MS 1st edition 09/20/2014, last revision 09/28/2014