
 |
 |
 |
|
 |
 |
 |
 |
 |
 |
||
Bone Graft For Periimplantitis
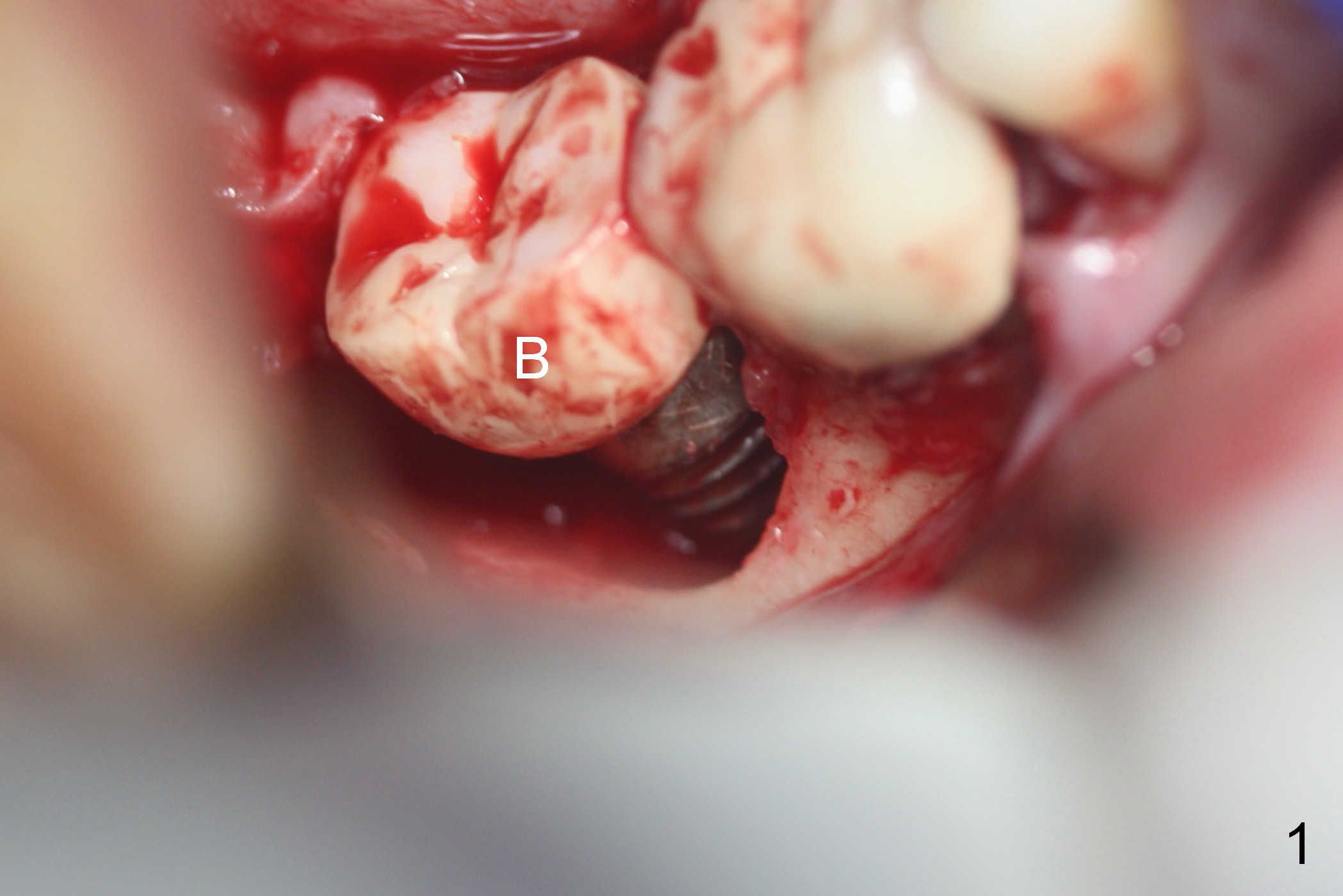
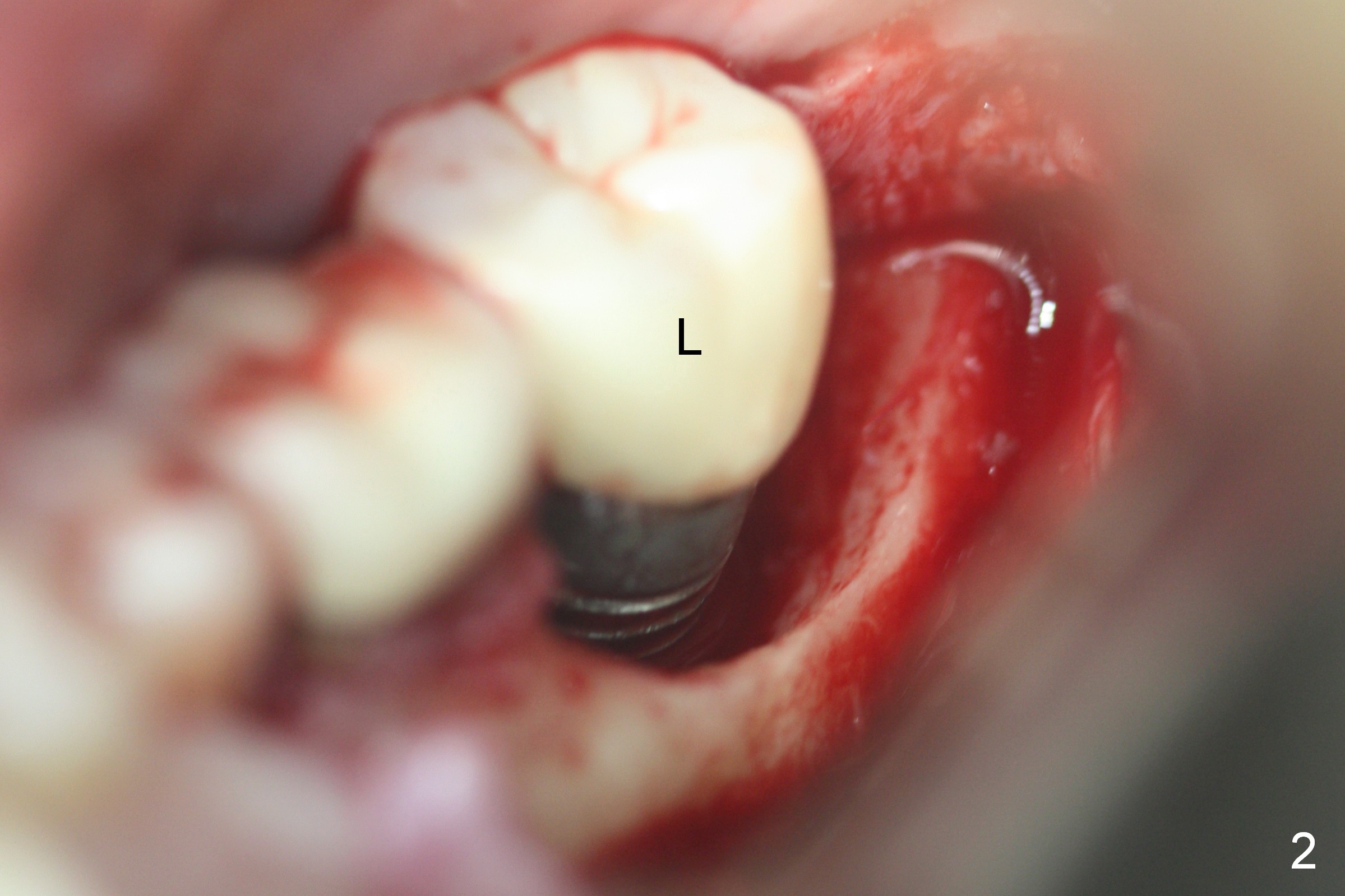
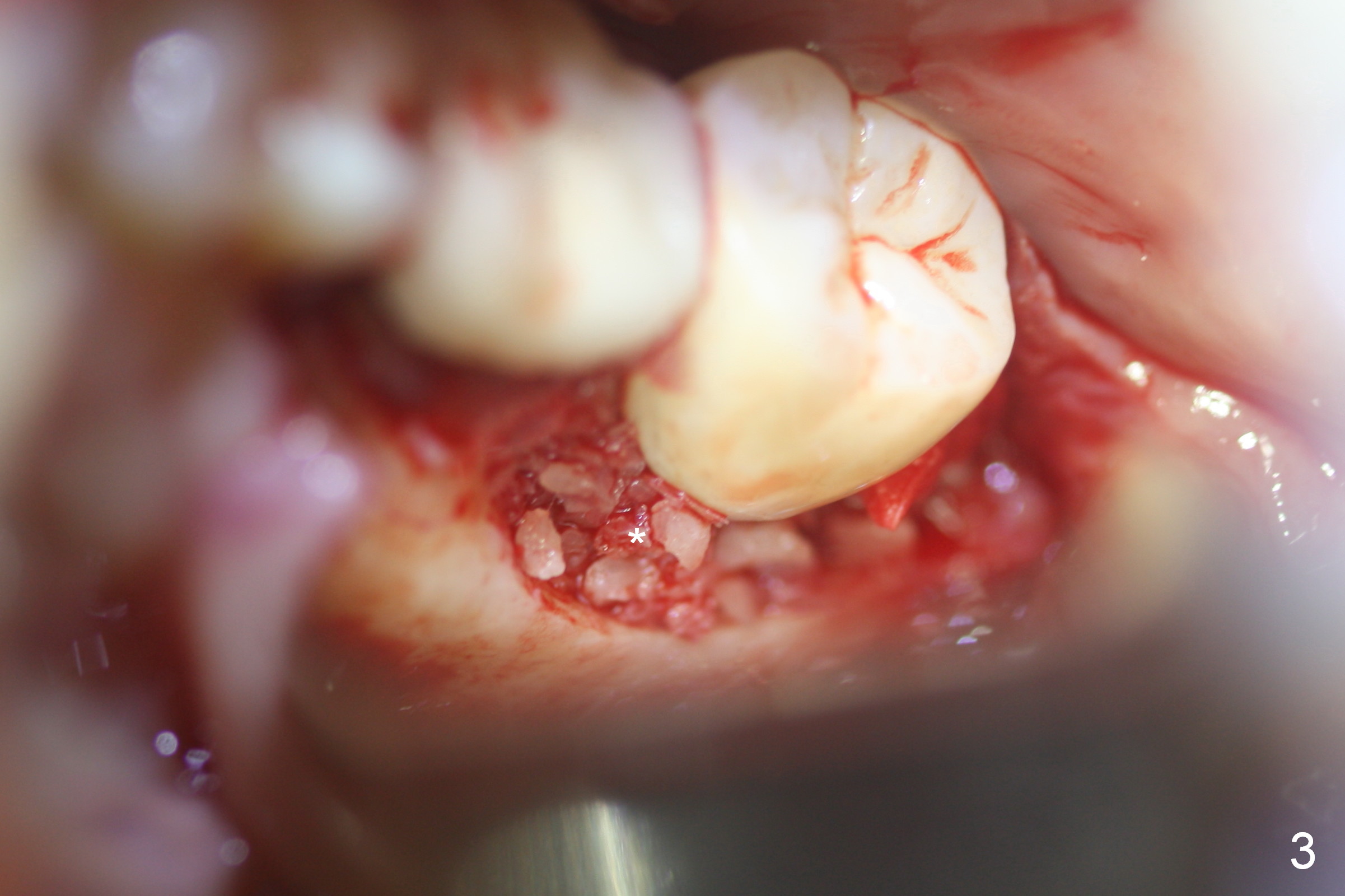
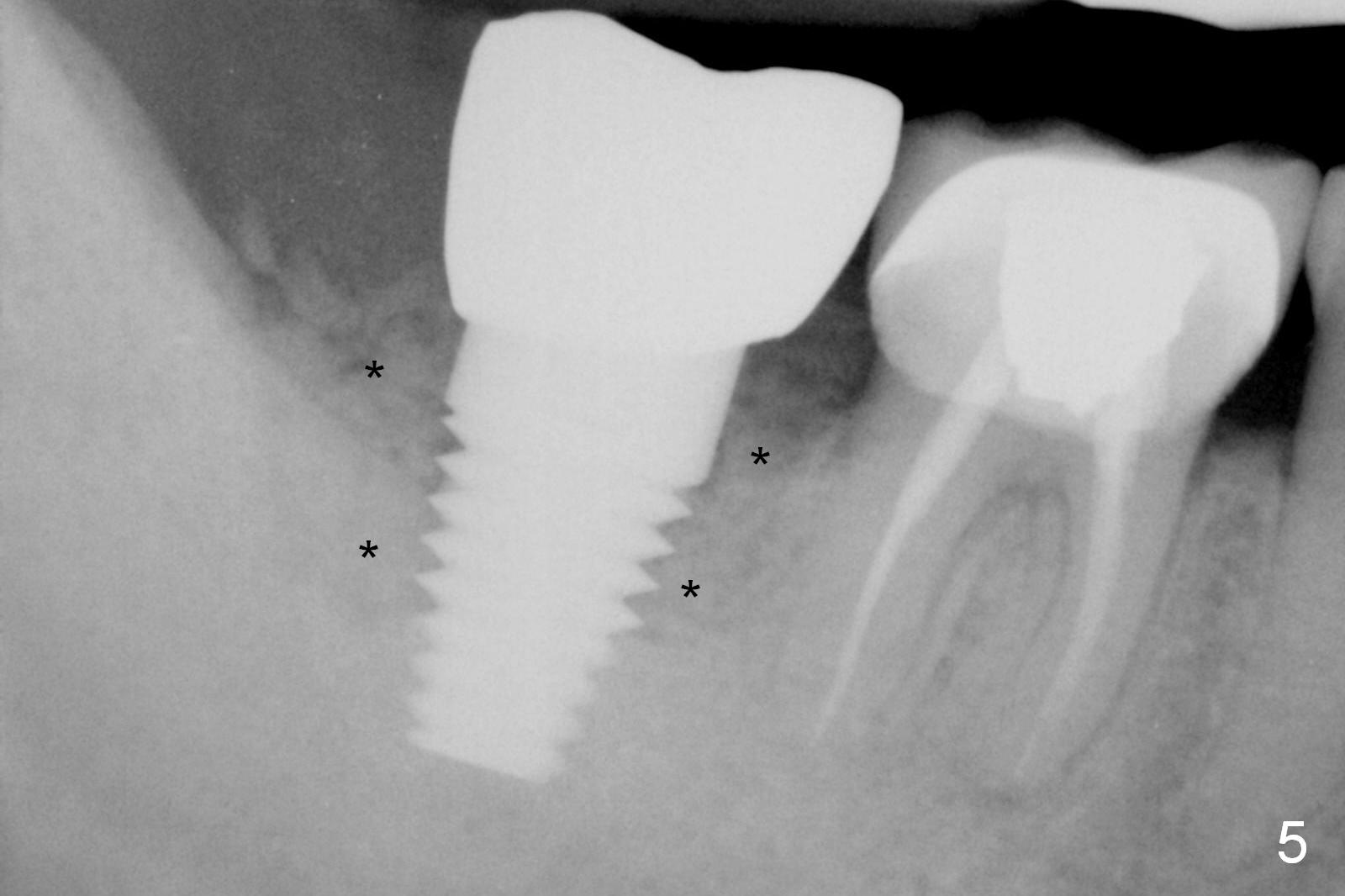
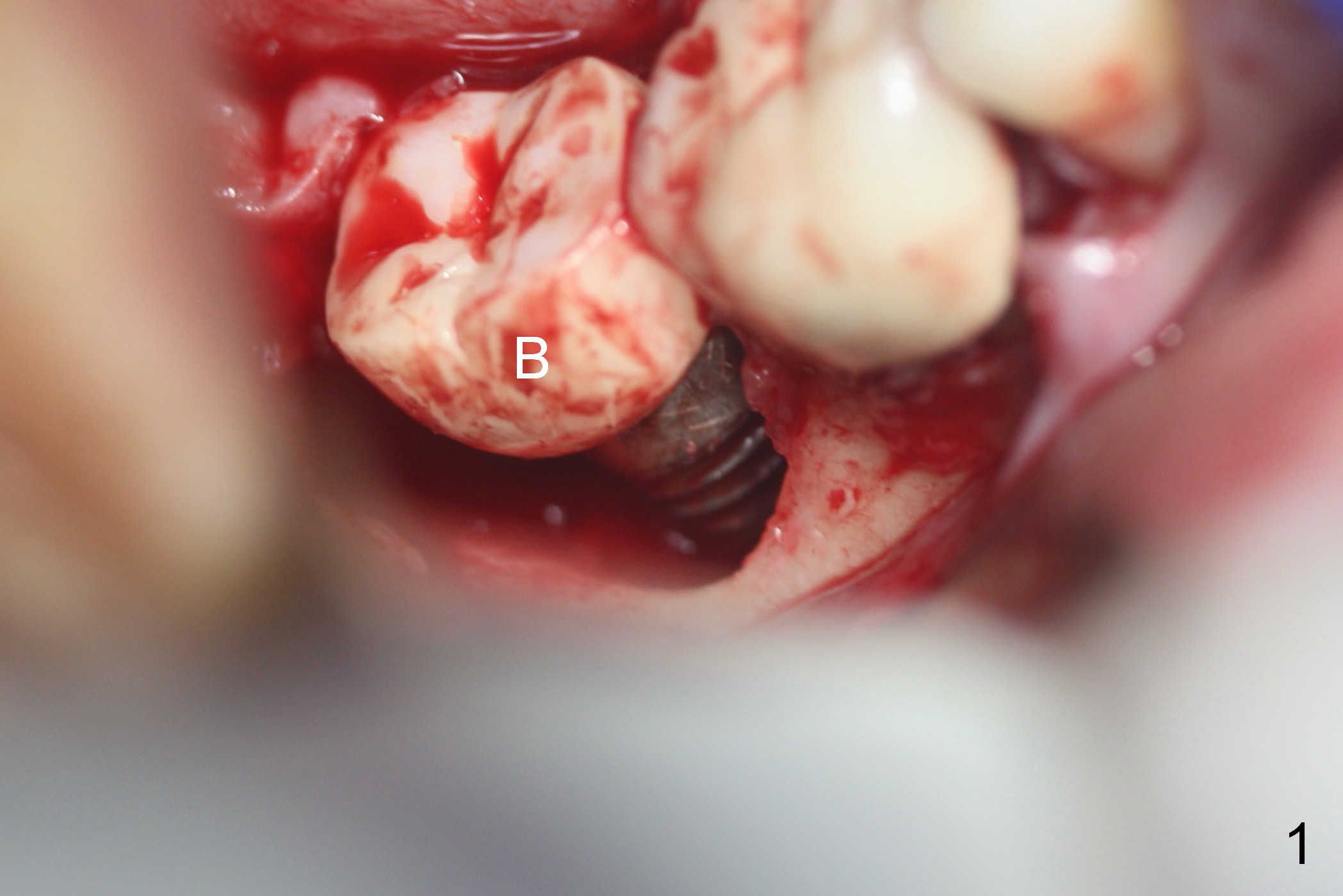
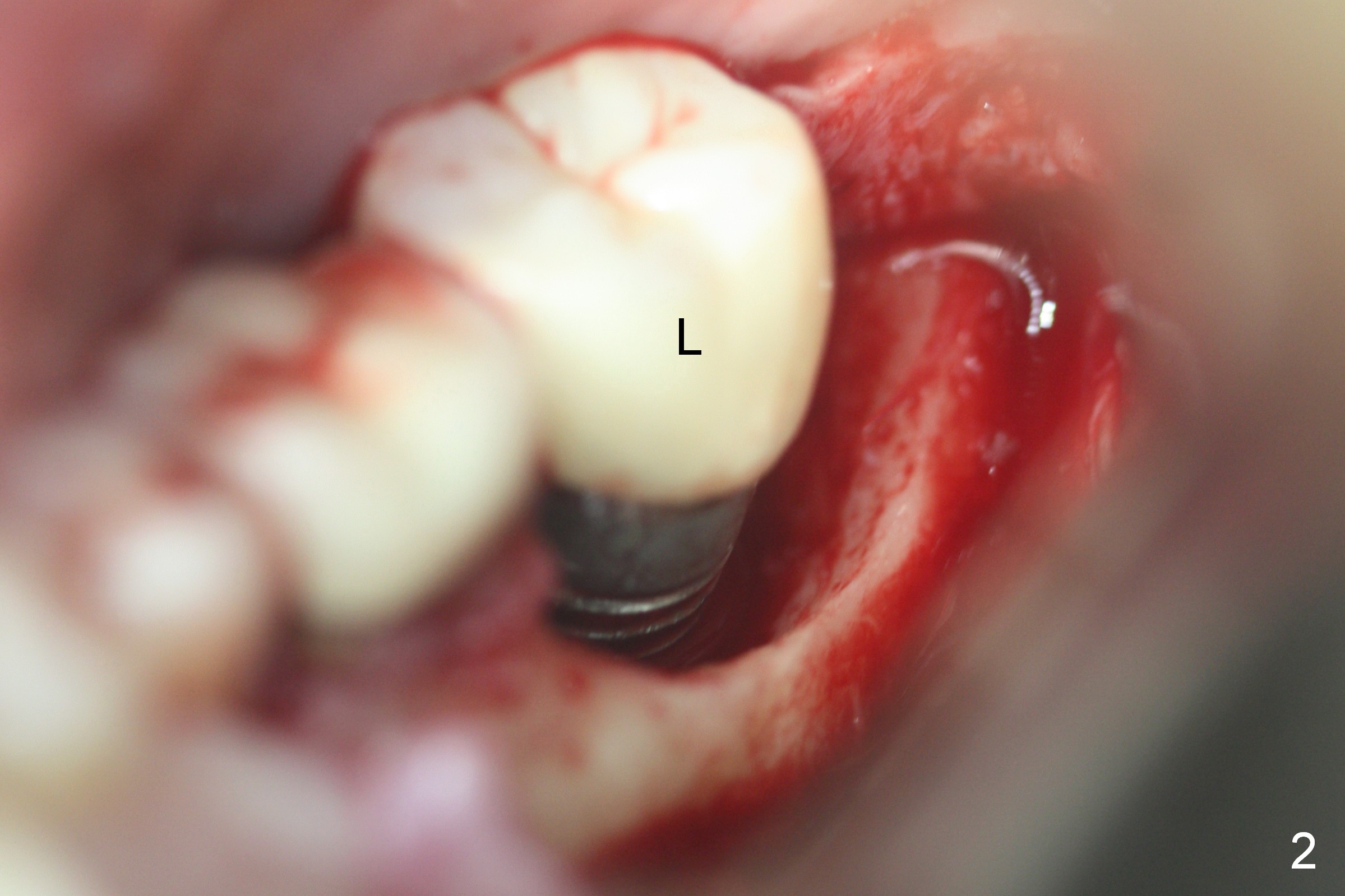
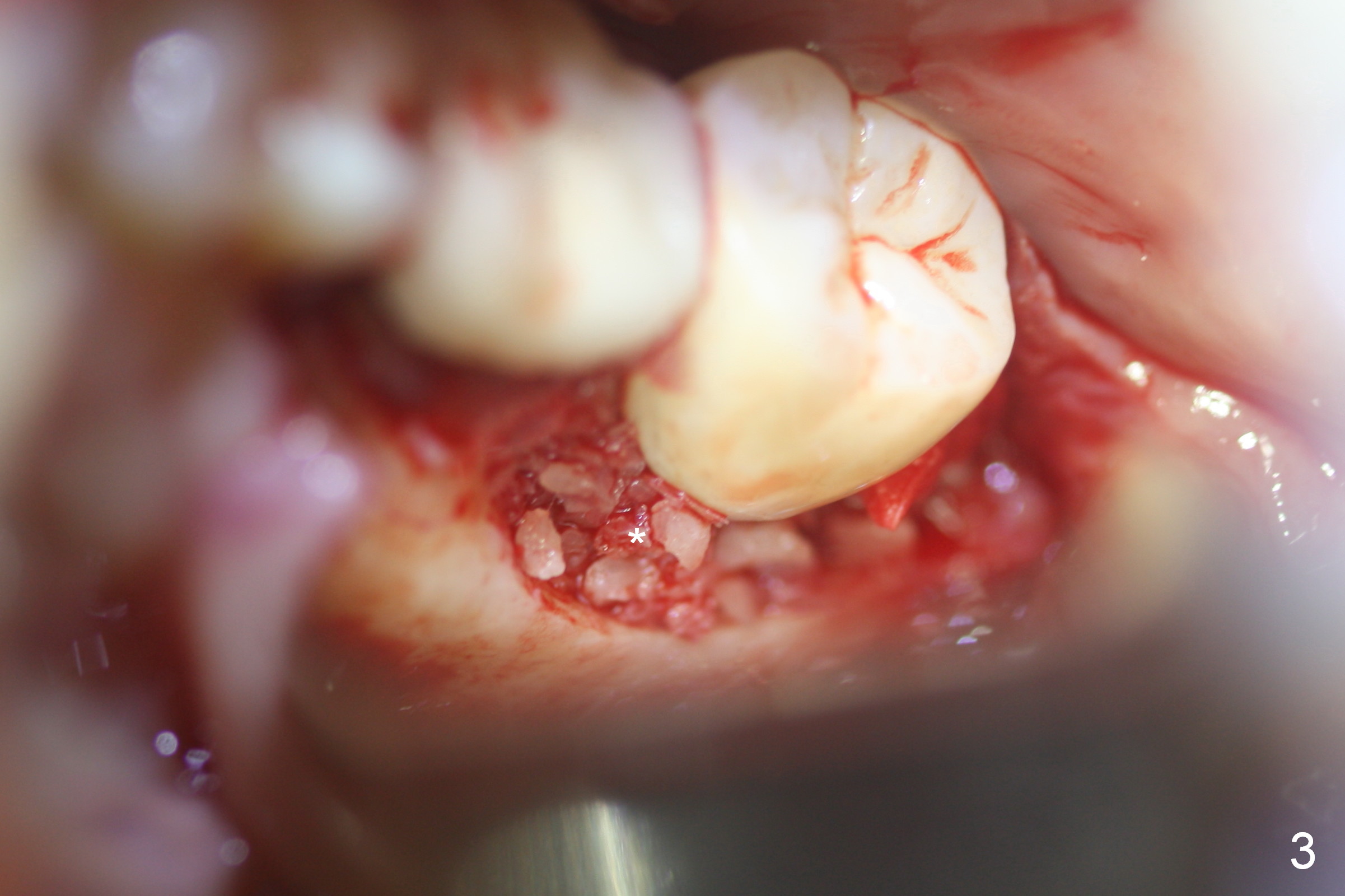
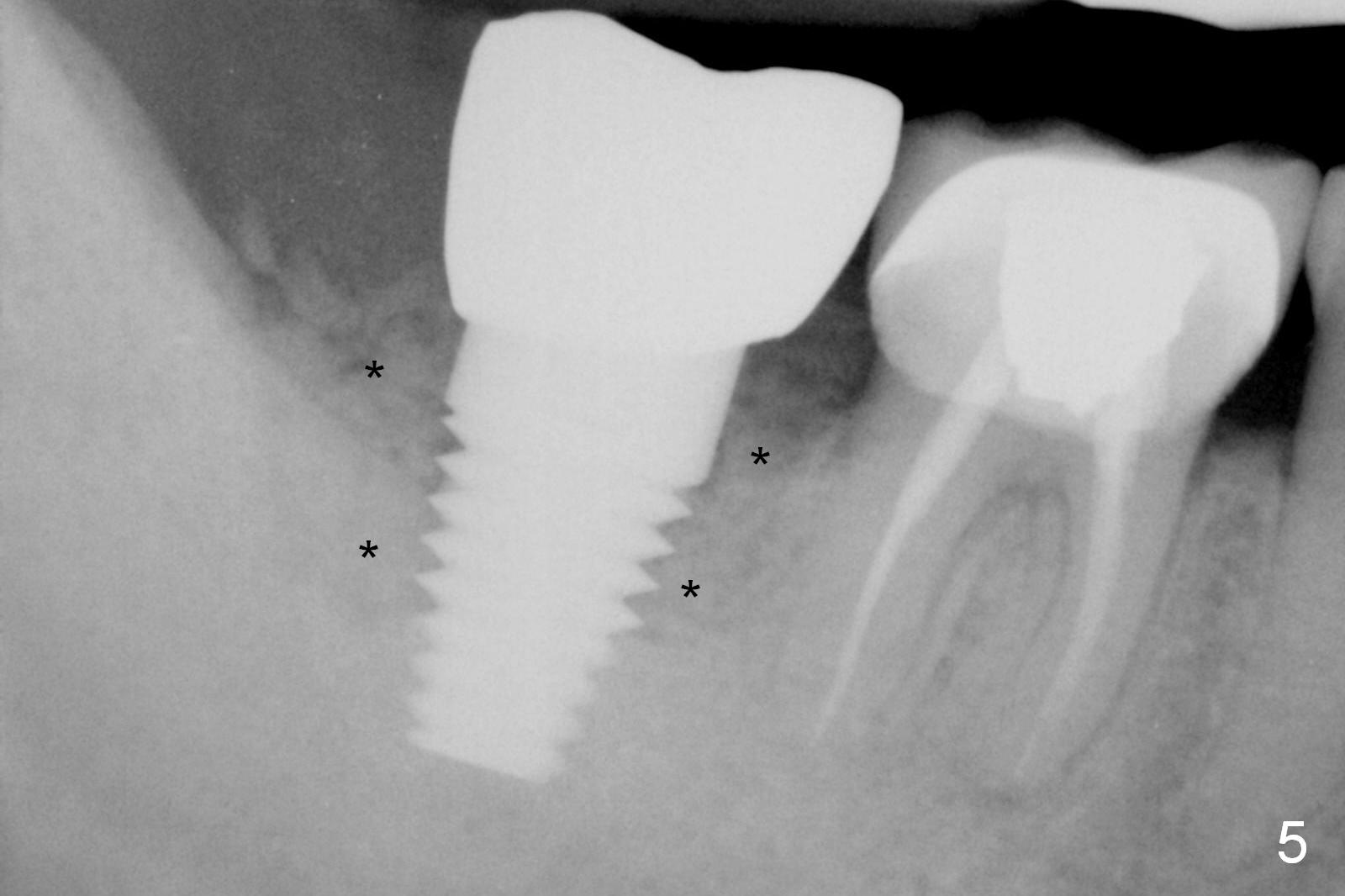
When the buccal flap is raised with removal of granulation tissue at #31 (Fig.1 B), there is a large bony defect with exposure of implant threads. After Titanium brush cleaning (Fig.2 (L: lingual)), large particulate allograft (.5-2 mm) is placed (Fig.3,5 *), followed by Osteogen plug (Fig.4 *). To reduce postop edema, Medrol Dose pack is prescribed.
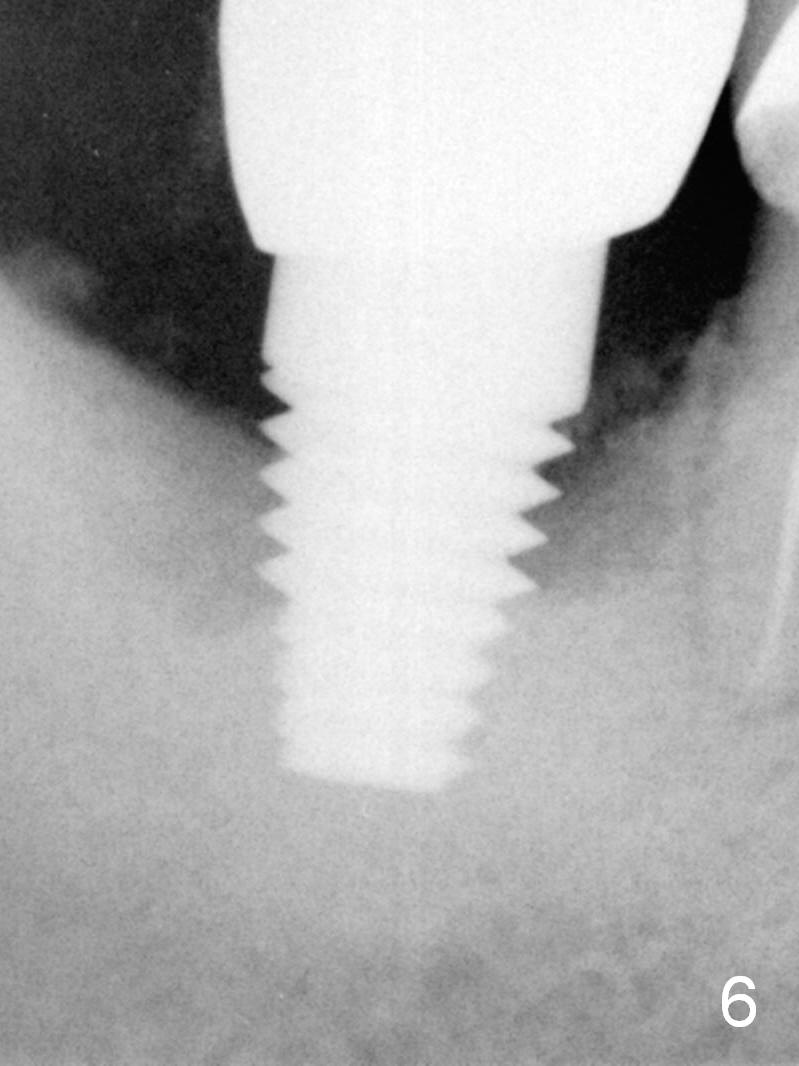
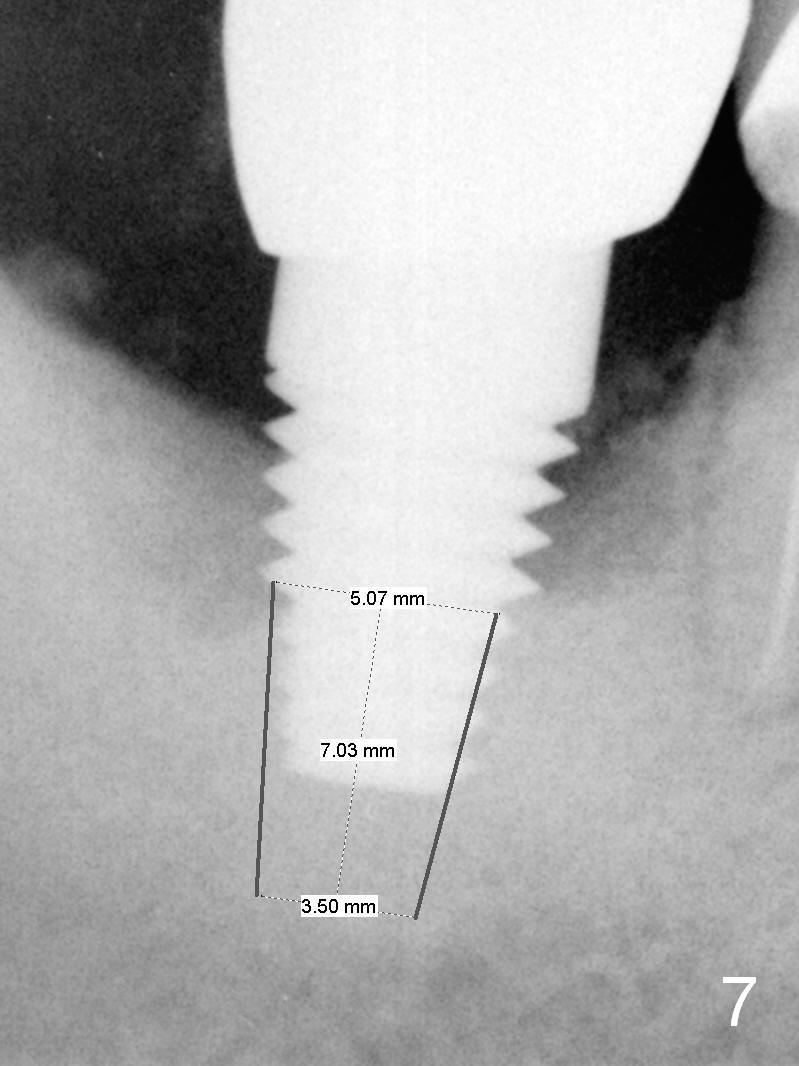
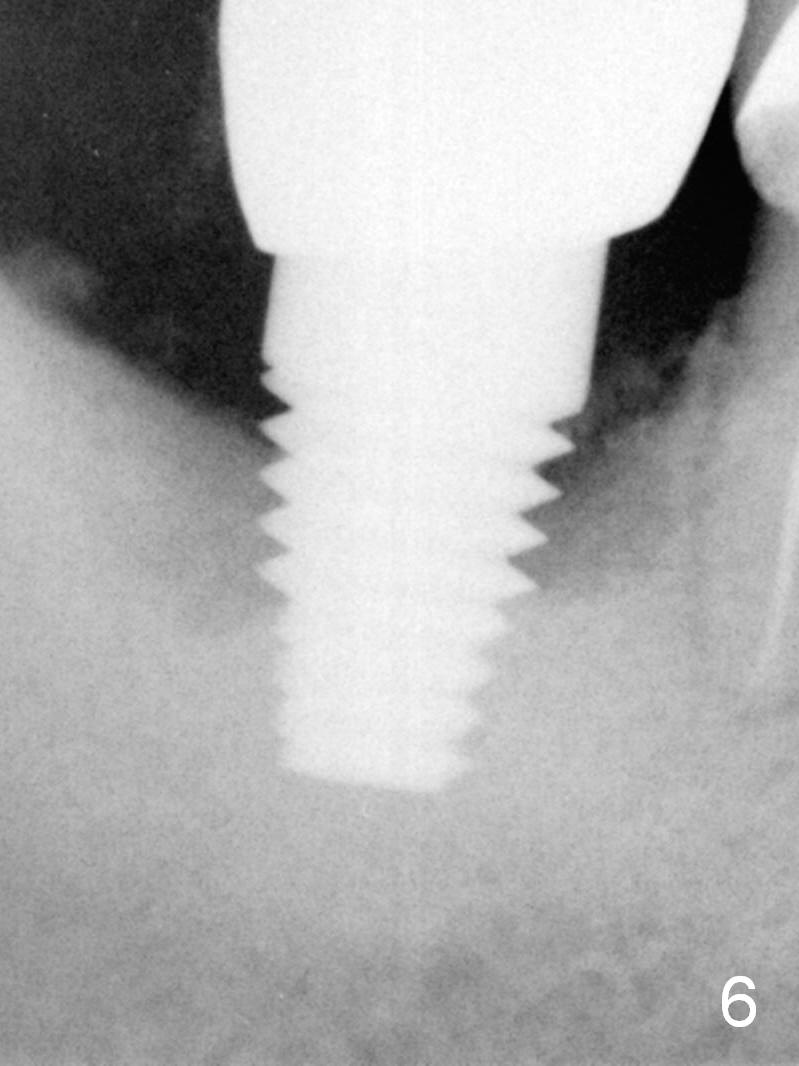
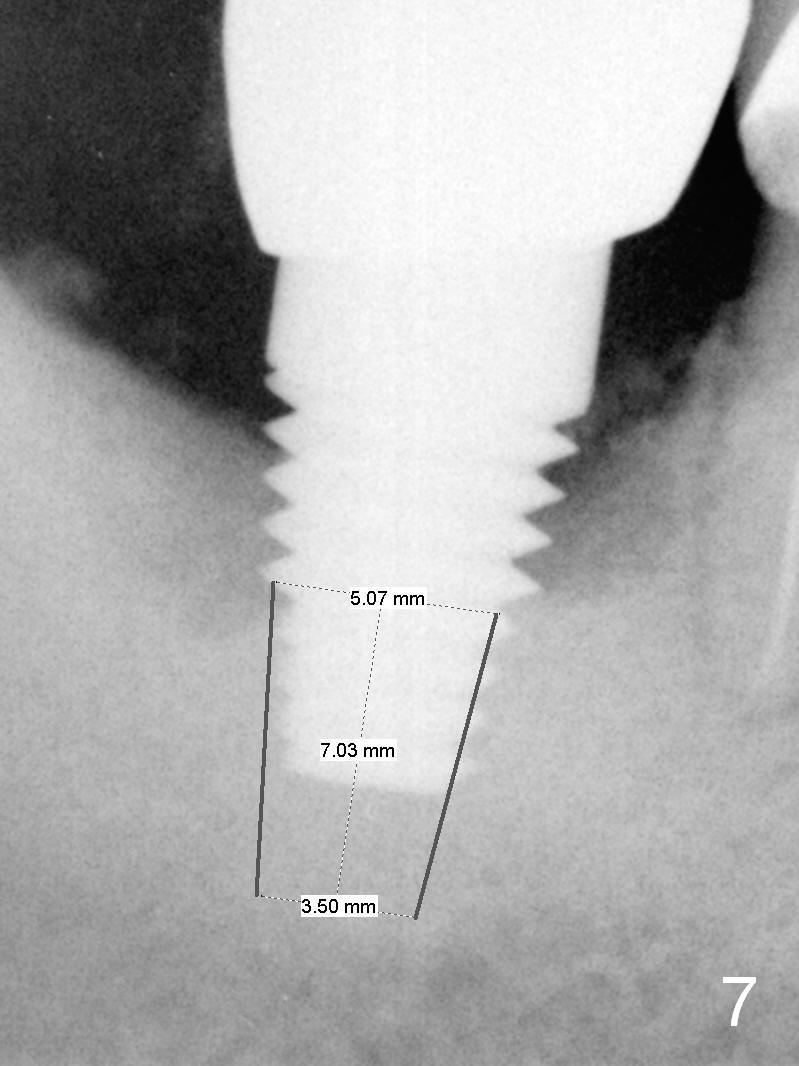
There is purulent discharge in the buccal vestibule with unknown origin 6 months postop. The gingiva looks healthy. There is bone loss (Fig.6). If the site becomes symptomatic, remove the tissue-level implant and place a short extra wide bone-level one (UF) in the native bone (Fig.7 (tilt mesially).
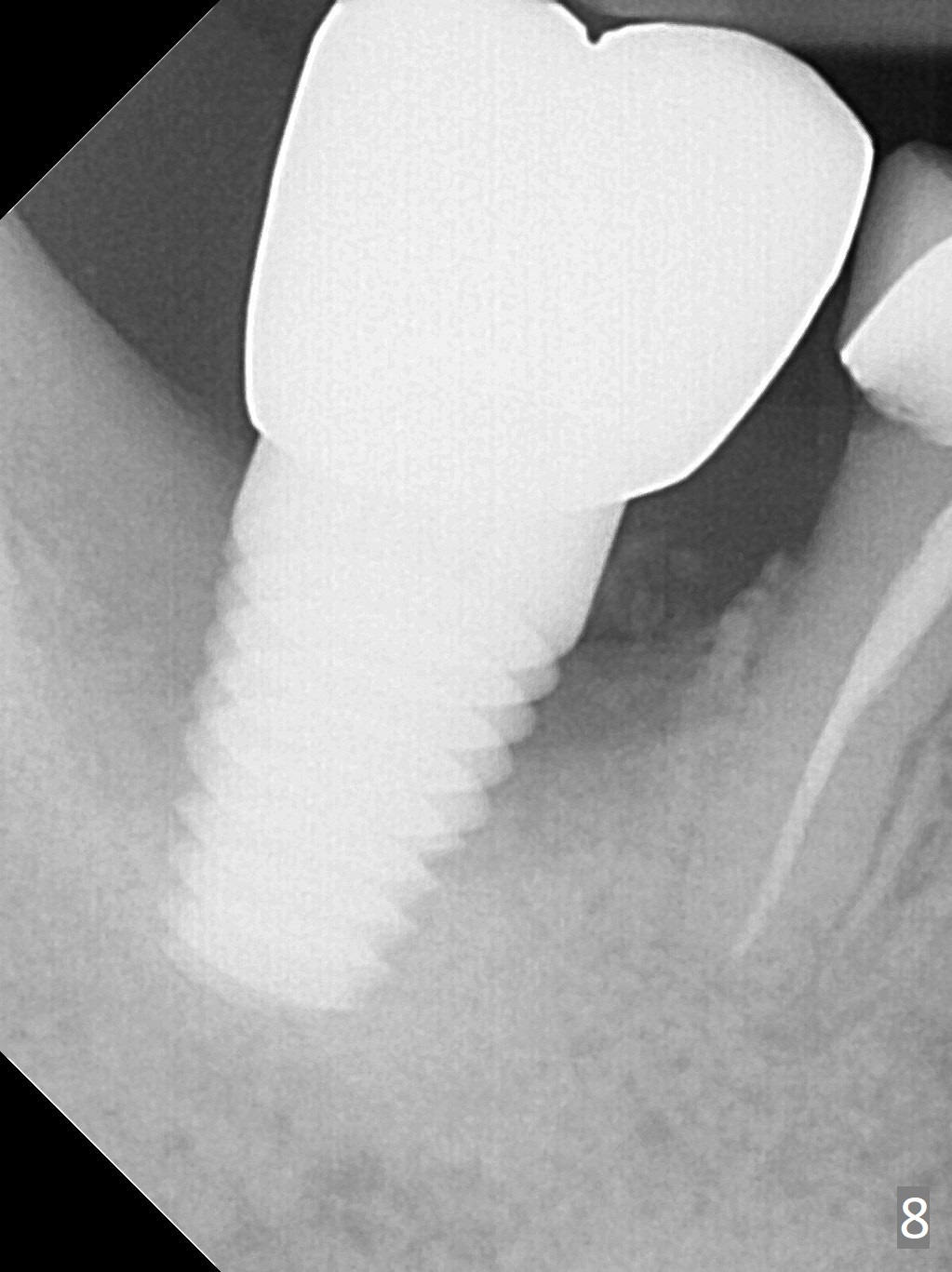
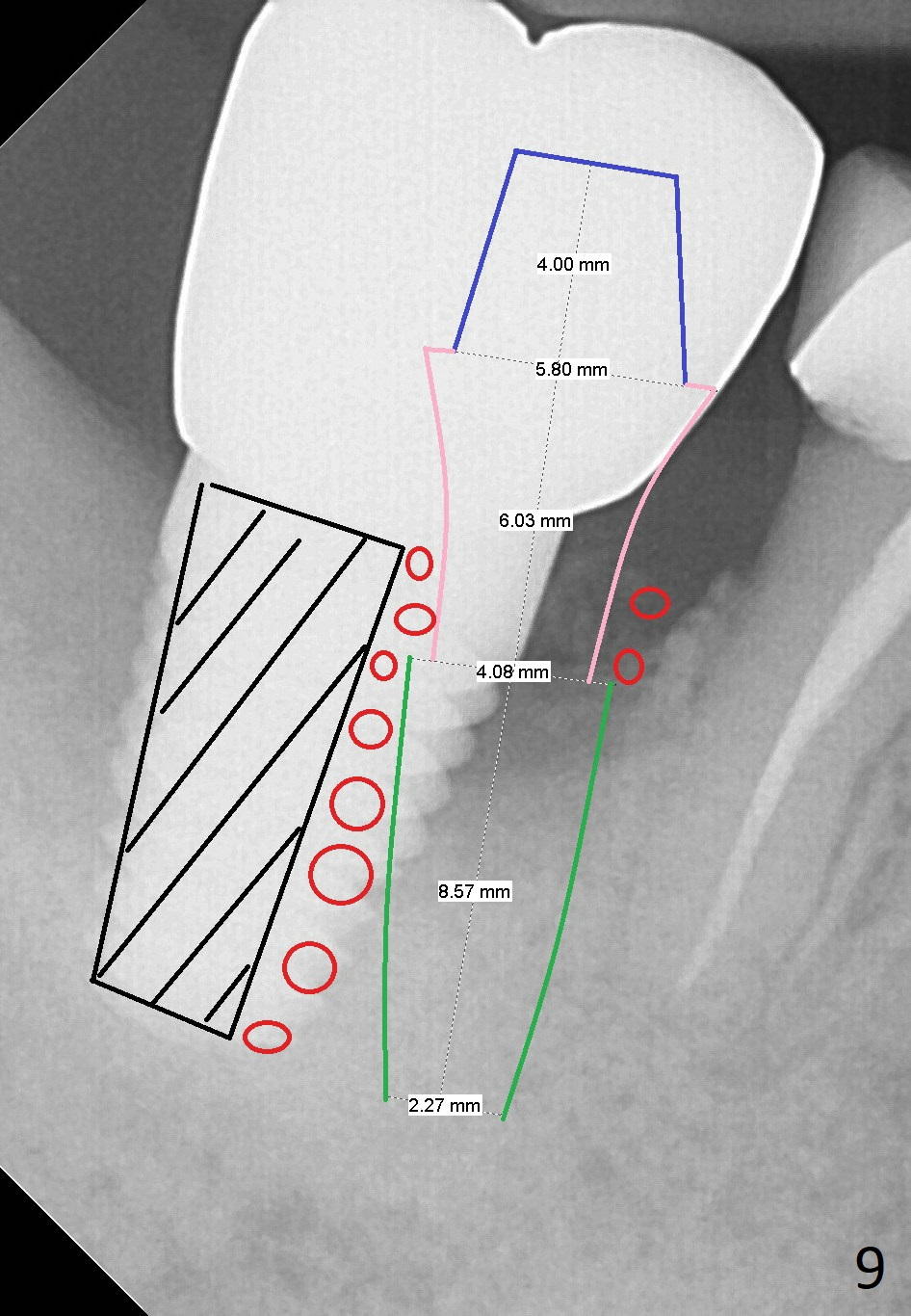
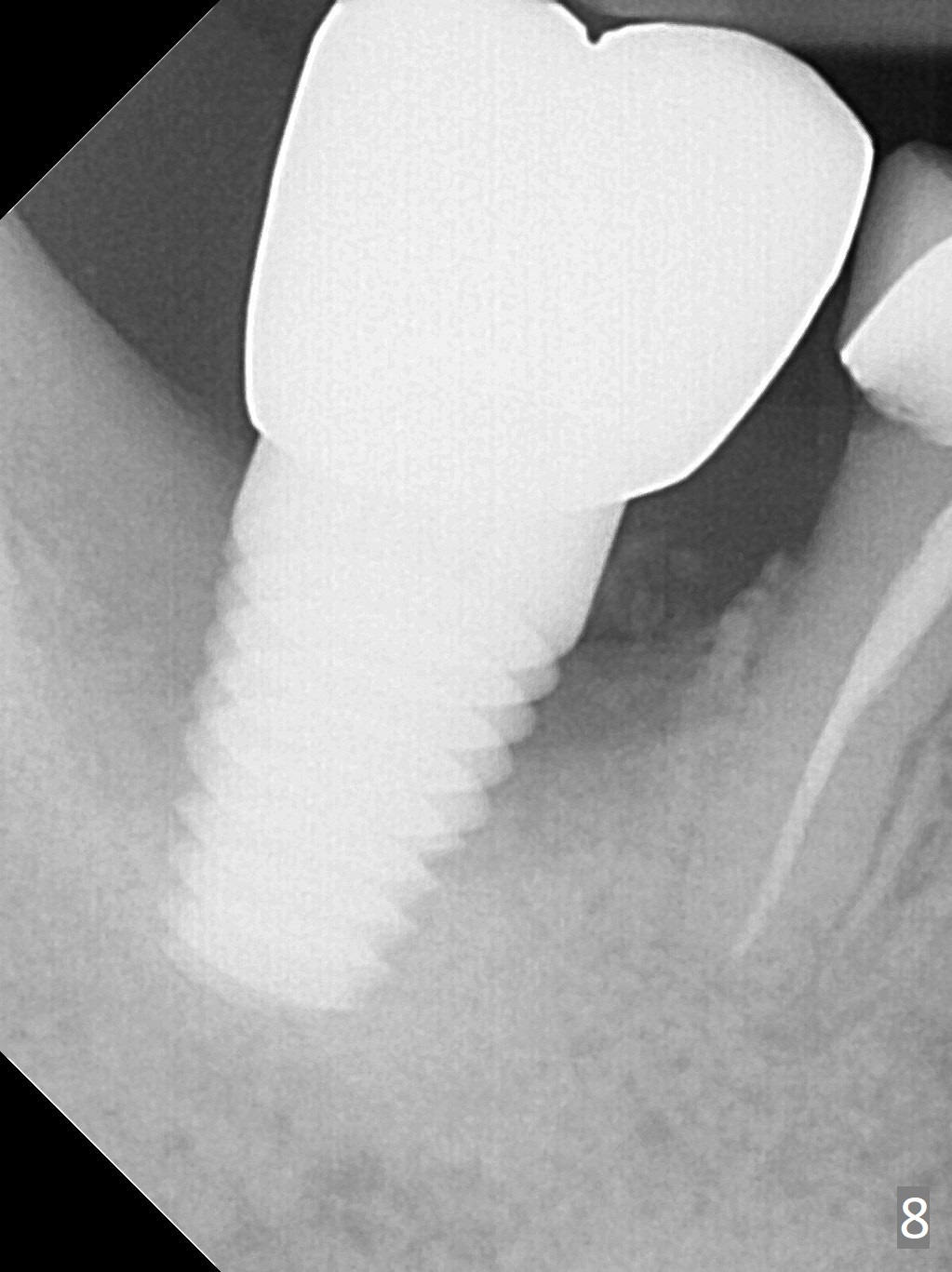
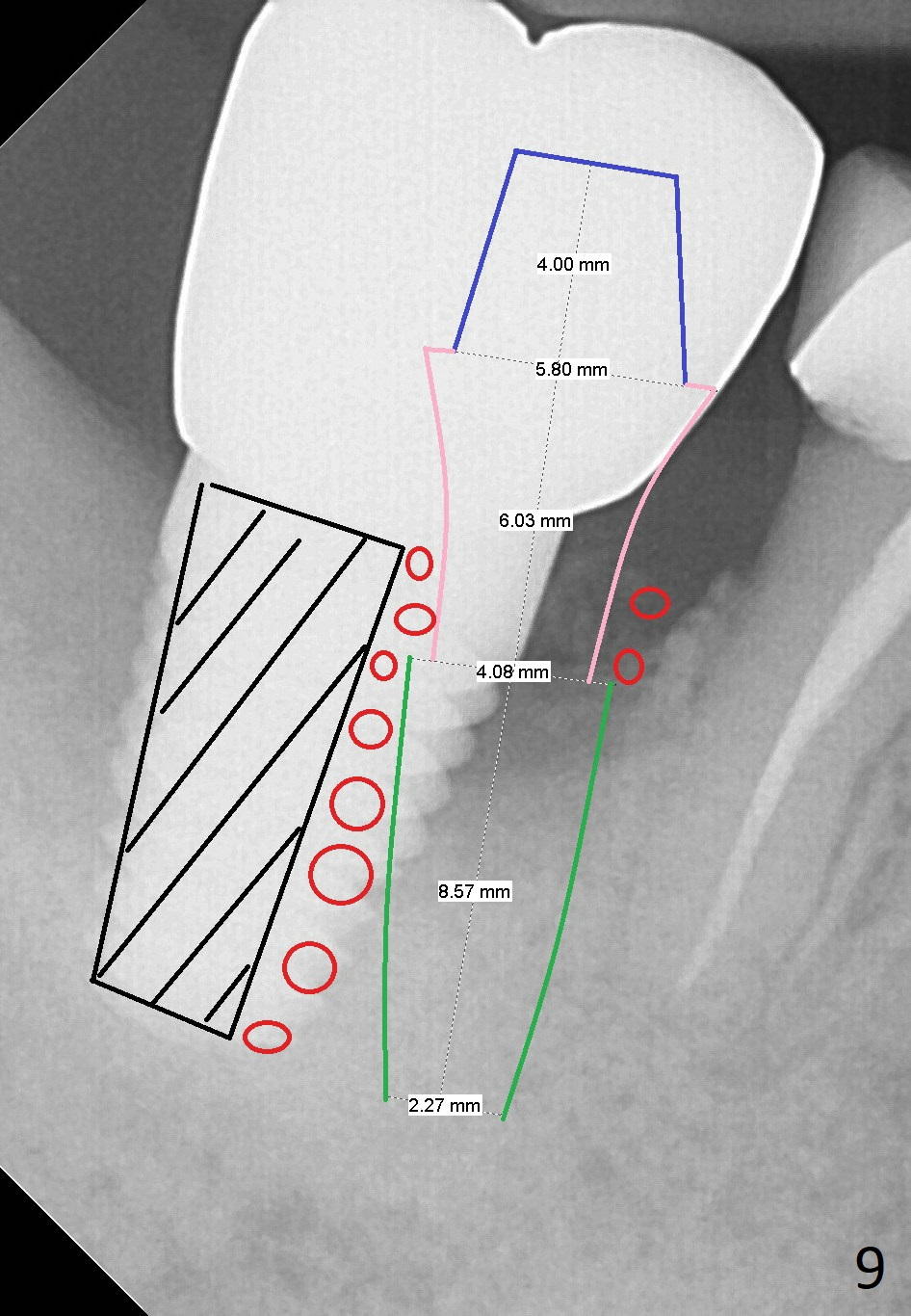
For the next 20 months, the patient uses water pik with complaint of pain when water touches the affected area. The buccal plate looks concave with a mesiobuccal fistula. The bone loss persists (Fig.8). The implant will be removed. A narrow UF implant will be placed in the mesial wall of the original osteotomy (Fig.9 green). The remaining distal defect will be filled with Osteogen plug (black area) before bone graft (red circles) being placed immediately to the implant. Use Metronidazole for disinfection.
Return to Lower Molar Immediate Implant, Periimplantitis, Armaments Xin Wei, DDS, PhD, MS 1st edition 03/09/2016, last revision 03/04/2018