






,%20mesial%20contact.jpg)
 |
 |
 |
 |
 |
 |
 |
 |
 |
 |
 |
 |
,%20mesial%20contact.jpg) |
 |
1st Guided Surgery
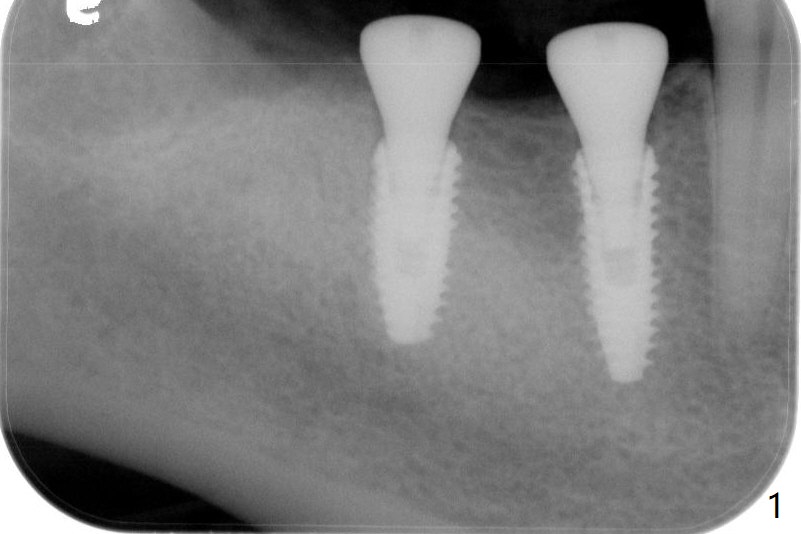
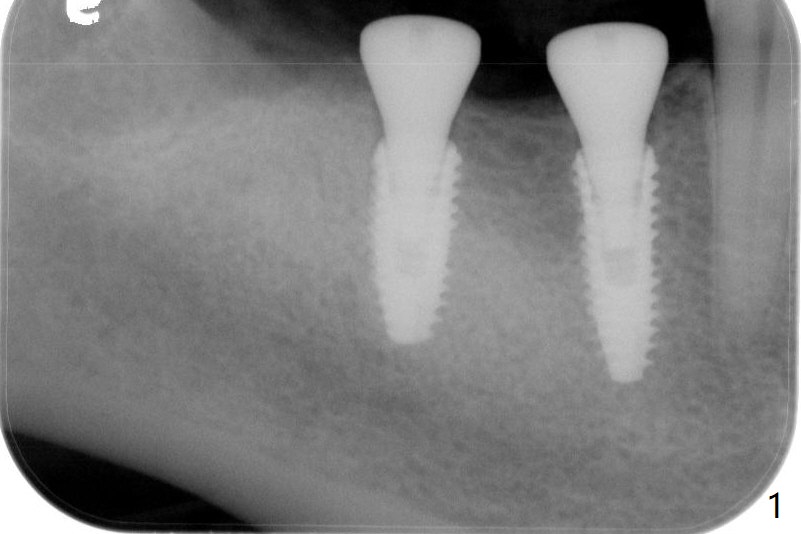
After infiltration and pdl anesthesia, the tooth #32 is extracted with elevators and forceps. Drilling protocol per CBCT plan, no deviation (see instruction sheets). Implants are placed subcrestal: 4.0x11.5 mm at #30 and 4.5x10 mm #31 with >50 Ncm. Healing abutments (6x4 mm) are placed (Fig.1,2). Resorbable suture is used to close #32 socket. Sensation returns. There is no hemorrhage. Although the wound looks healing 4 days postop and the healing abutments have normal position (Fig.3), the patient complains of fair amount of pain.
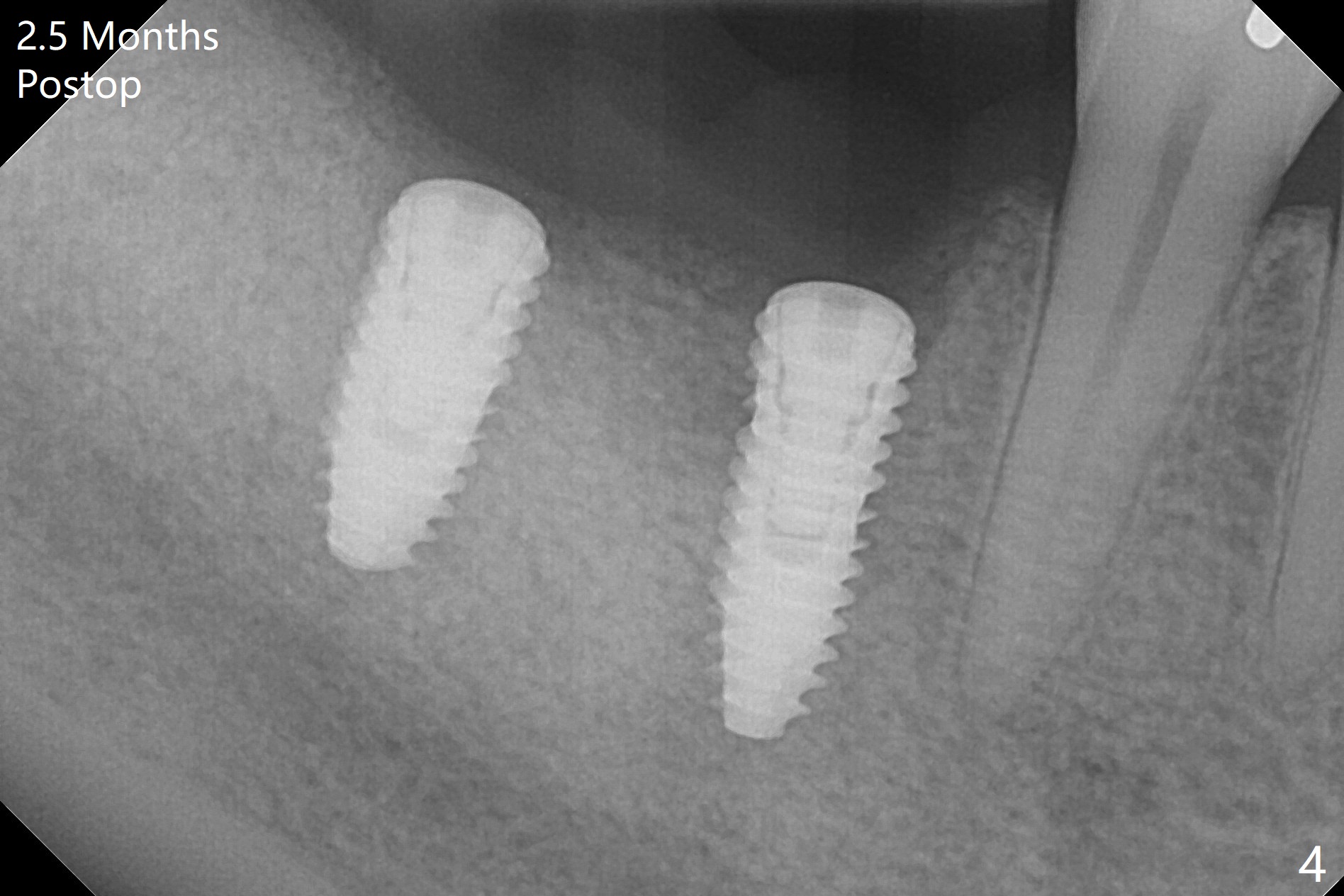
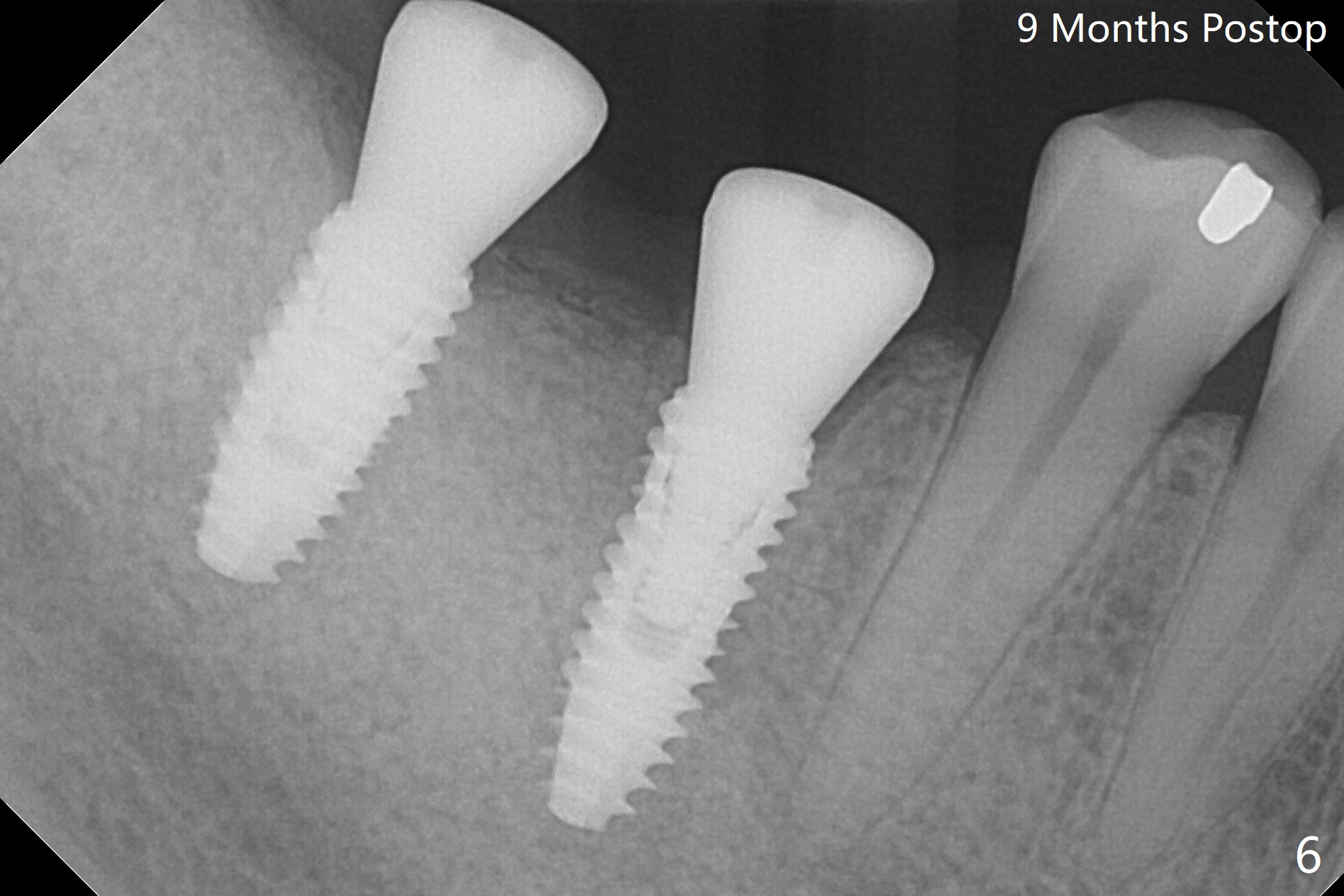
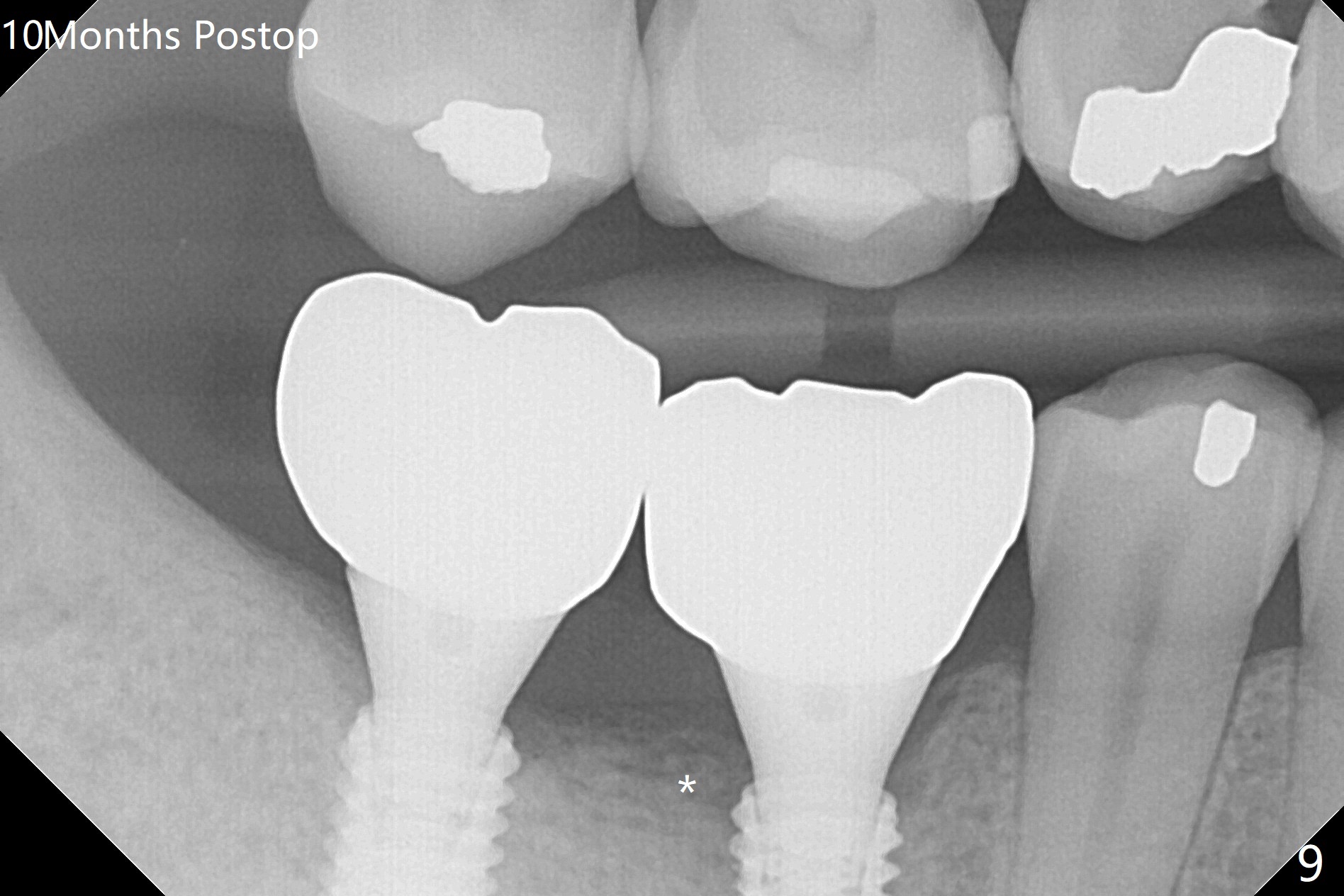
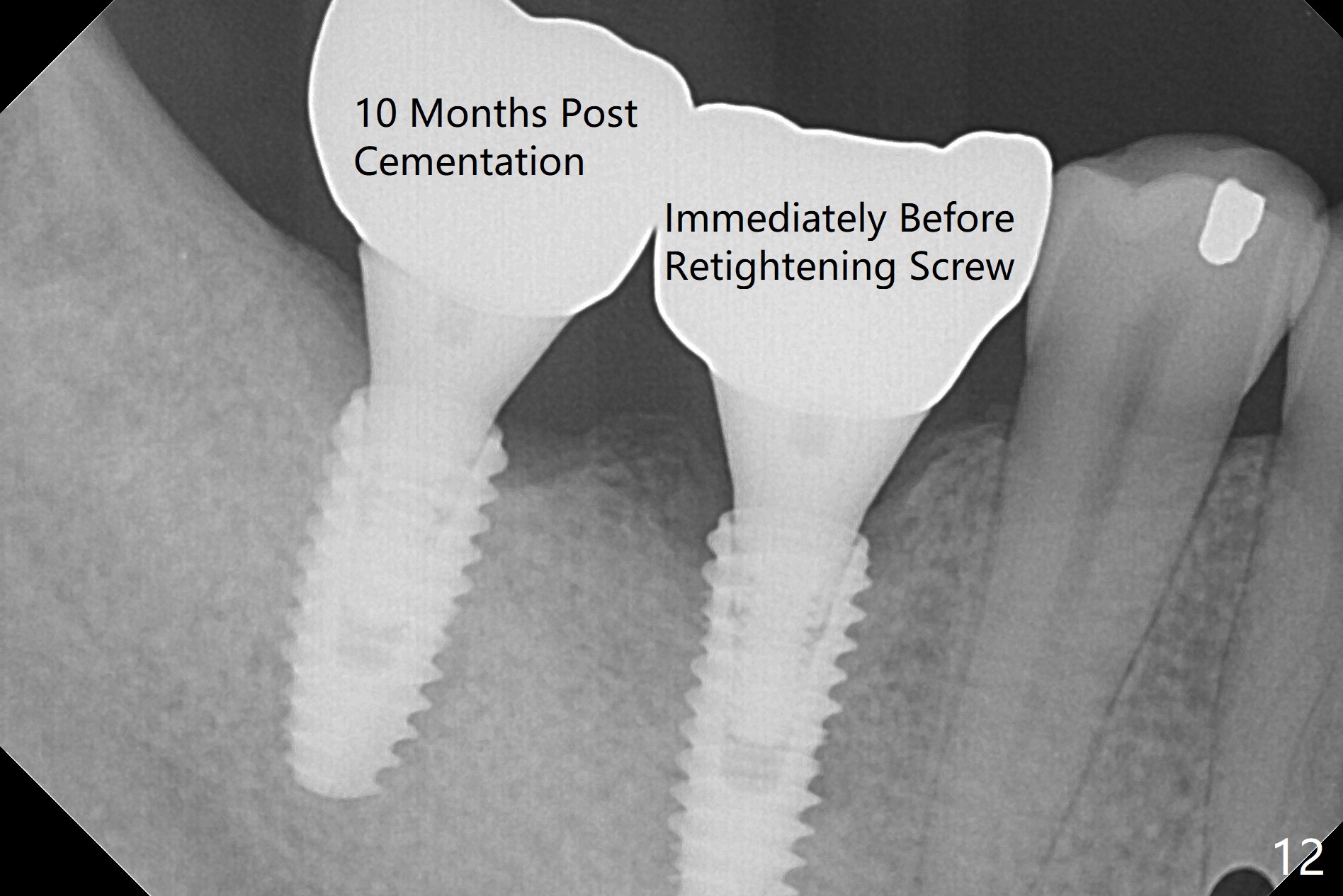
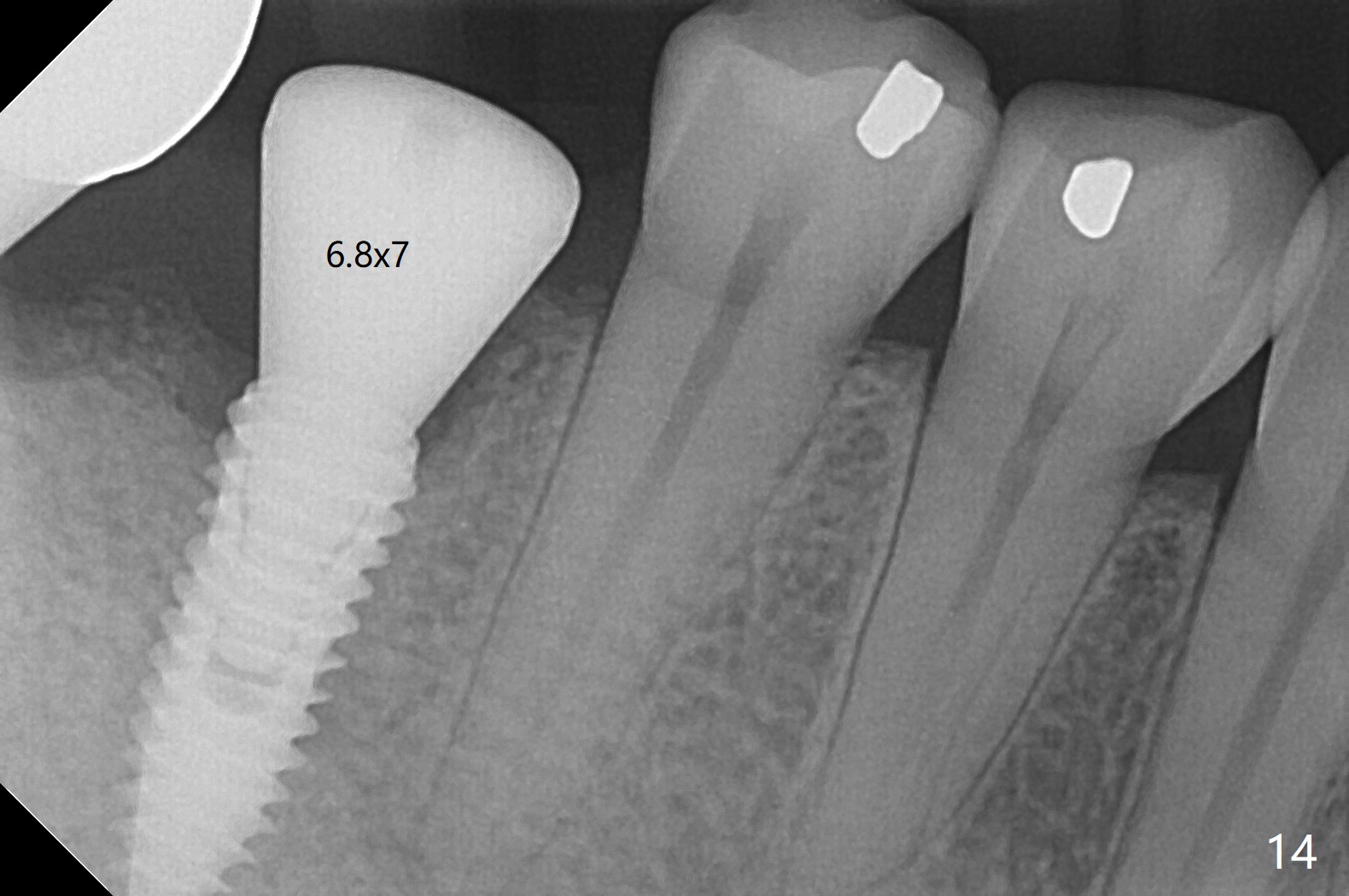
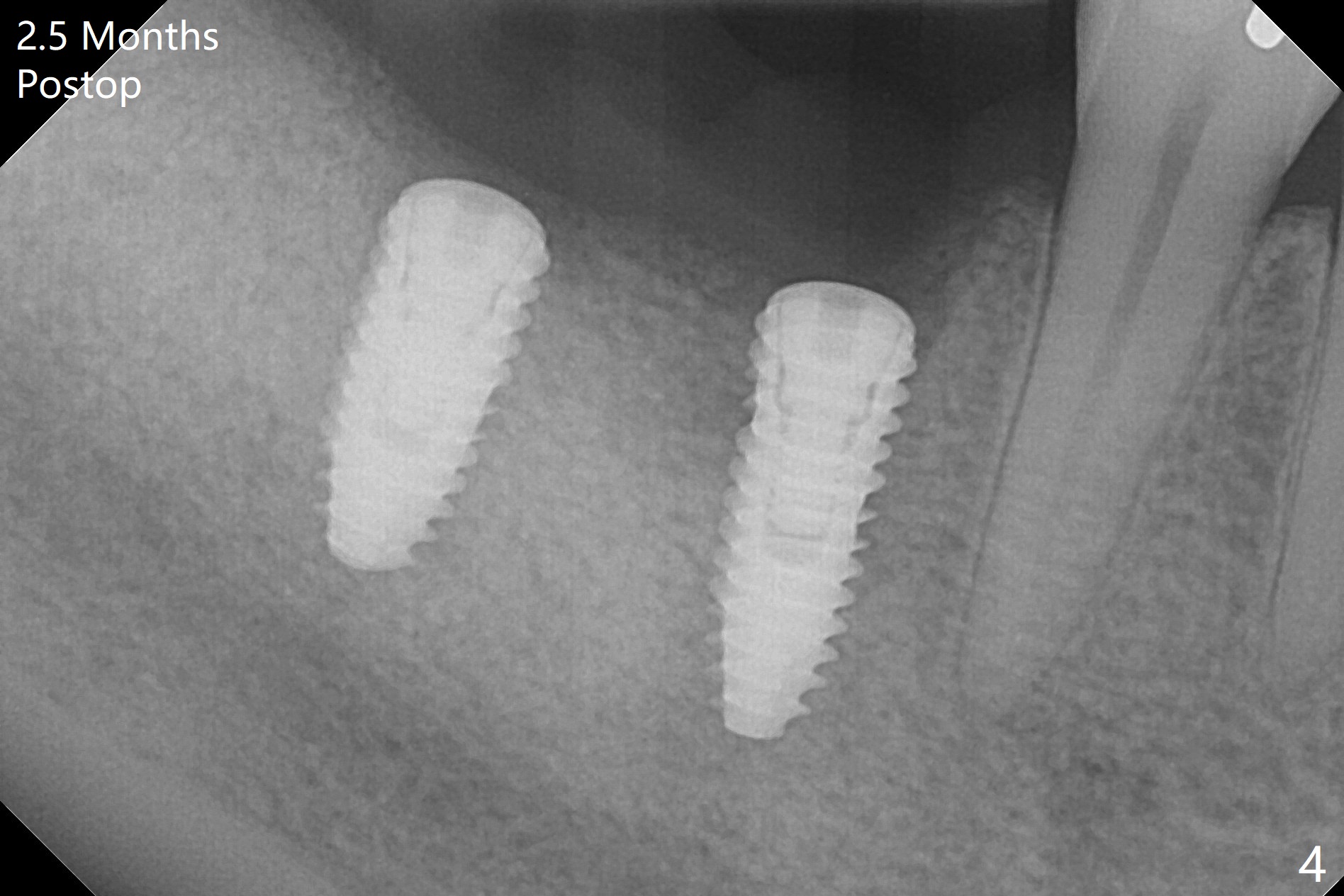
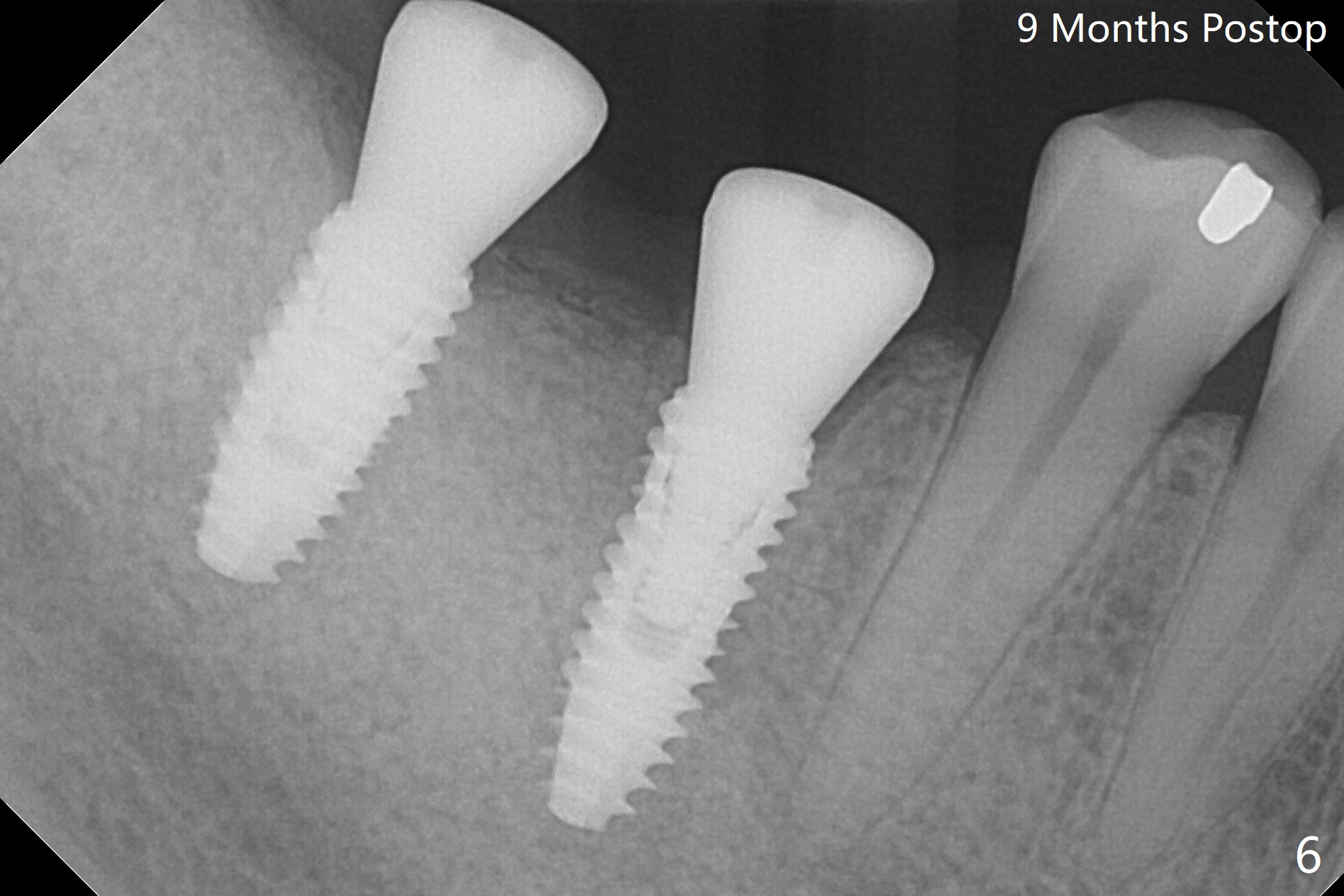
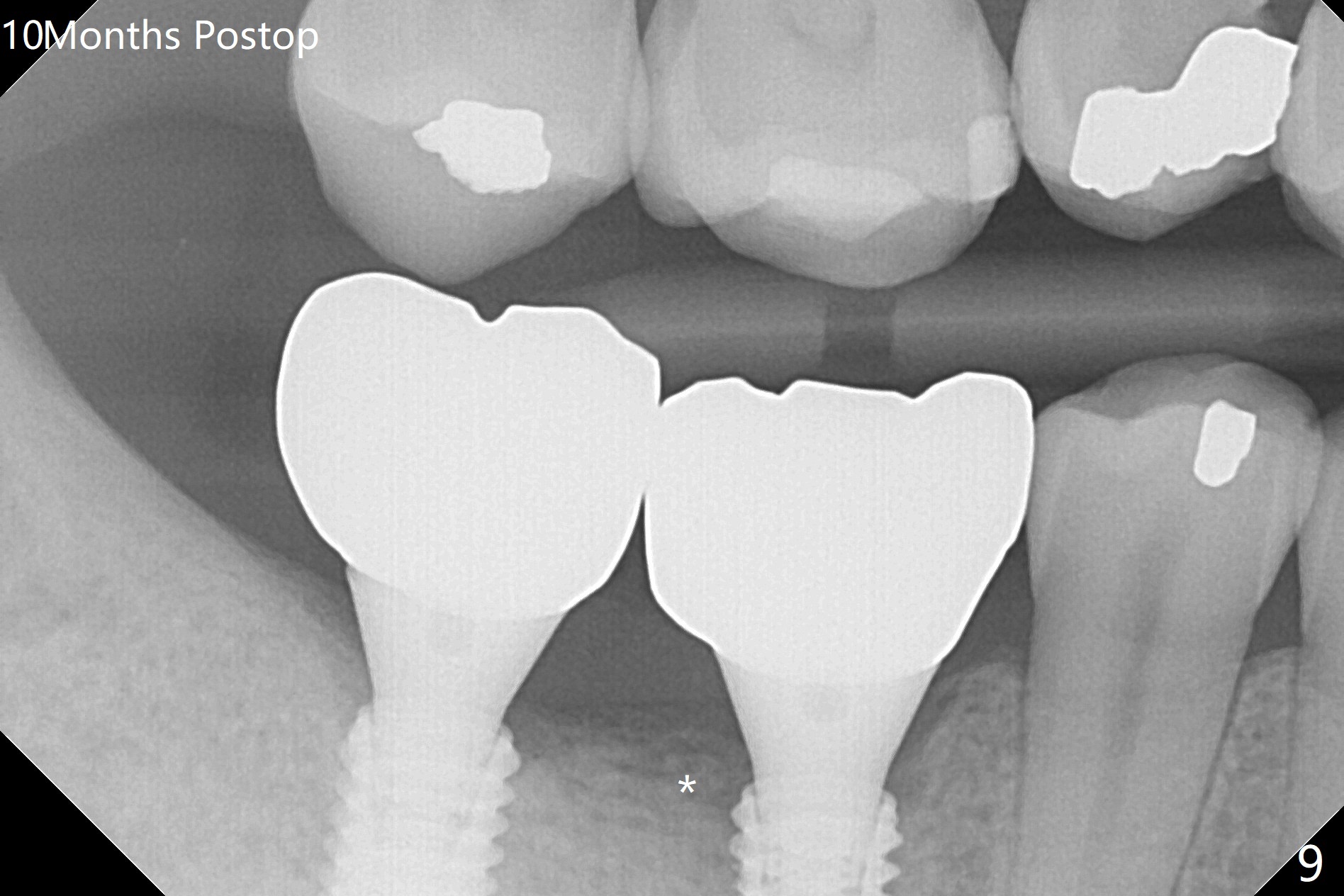
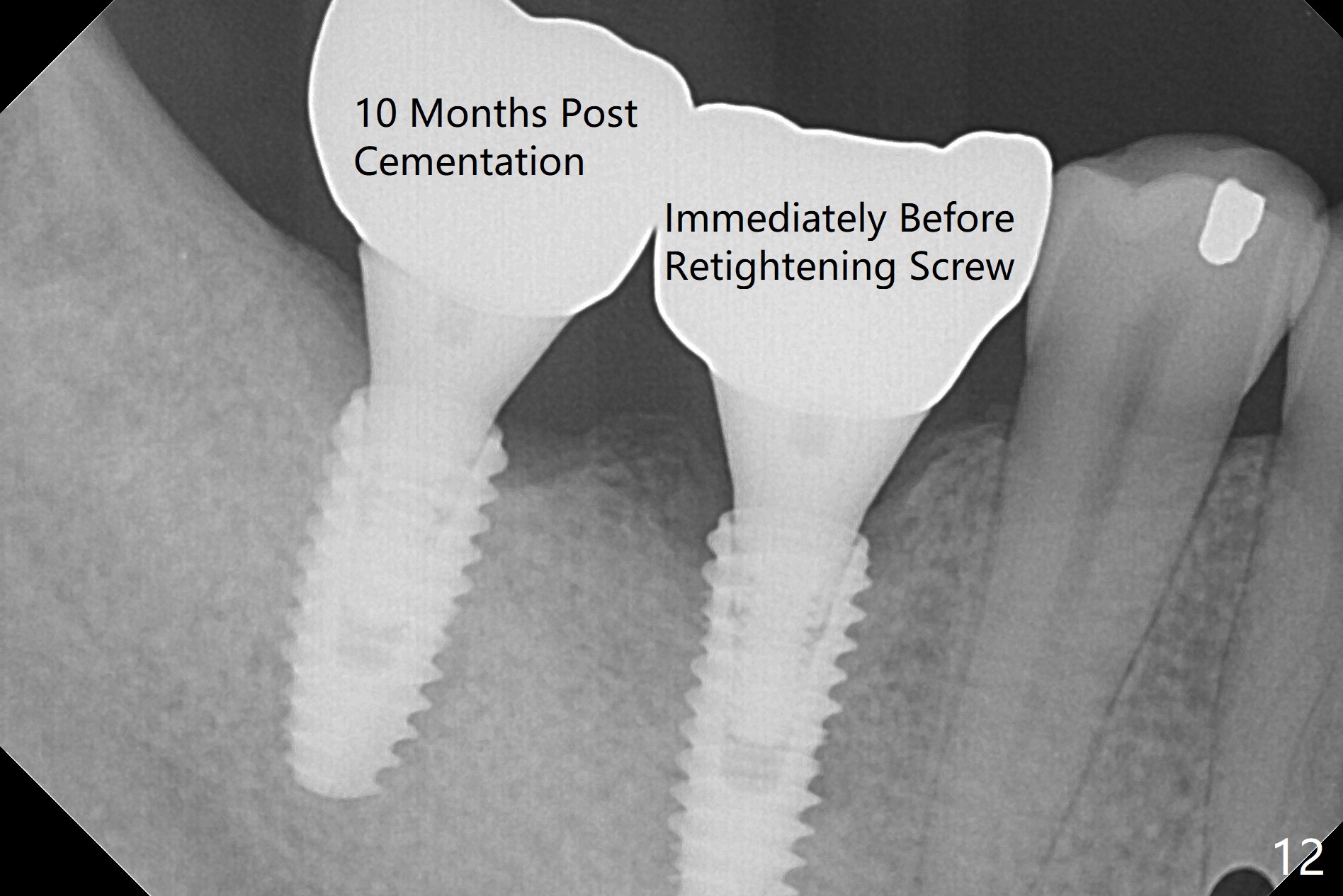
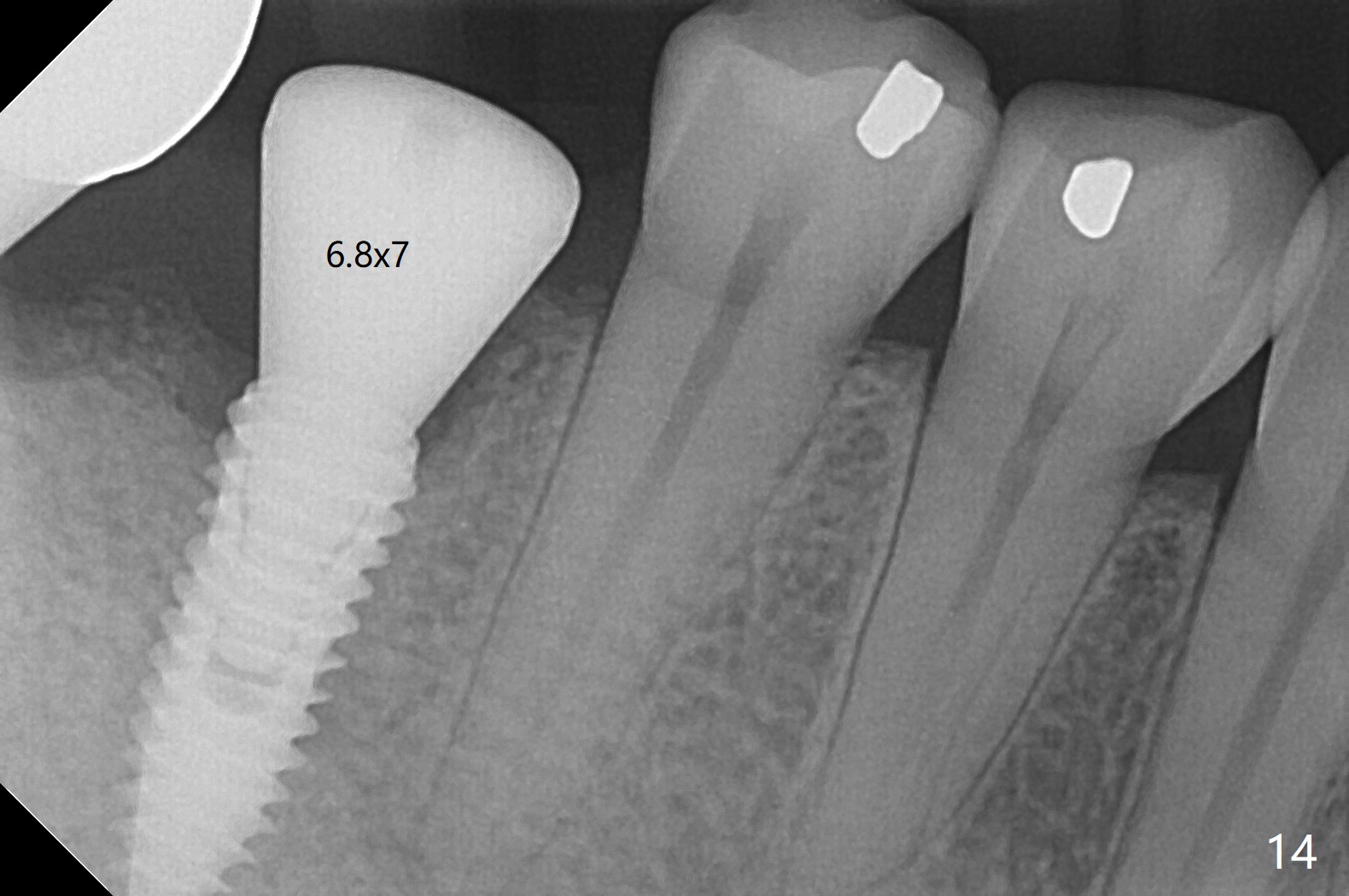
Infection is not so typical. There is no recent postop X-ray, just 18-19 days postop. Thanks for the reply. We will keep watching. The healing abutments, loose and associated with gingival inflammation, are removed 2.5 months postop (Fig.4). There is crestal bone resorption, although the implants are stable. The crestal bone resorption persists especially #30 distal 4 months postop (Fig.5 *). When the implants are uncovered, there is mild bone loss distobuccal to #30 implant, consistent with early periimplantitis. Bone graft is placed after debridement and healing abutment placement. There appears no bone loss nearly 9 months postop (Fig.6). The soft tissue looks healthy. Cementation abutments (5.7x4(3) and 5.7x4.5(3) mm at #30,31, respectively) are placed for impression. The distobuccal gingiva at #30 is hyerplastic 10 months postop (Fig.7 *, immediately before cementation), which is consistent with bone loss (Fig.8,9 * (periimplantitis)). It is hoped that the infection will dissolve with improved oral hygiene (water pik) over the smooth final restoration. In fact it is, i.e., the implants at #30 and 31 remain asymptomatic with the healthy gingiva 6 months post cementation (Fig.10,11). There is mild crestal bone loss at #30 and 31 ten months post cementation (Fig.12). Crown/implant ratio is the basis for screw loosening. In fact the crown/abutment at #30 is loose 4 months later. Incomplete seating of the abutment may be a culprit (Fig.12). The gingival cuff is not healthy; a 6.8x7 mm healing abutment is placed with gingival blanching with Cetacaine and antibiotic ointment. Next visit place a new smaller diameter abutment (4.5 or 5.2) with probably longer cuff (4 mm) or the existing abutment with no proximal contact crown, torque 25-30 Ncm and take BW with sensor 2 or PA with sensor 1. In fact there is resistance to hand tighten a 4.5x4(4) mm healing abutment, which is due to contact with the mesial crest (Fig.13 *). After use of 5.5 and 6.0 mm profile drills, the 6.8x7 mm healing abutment is reseated. The latter appears to contact the mesial crest (Fig.14). Later a 6x5 mm healing abutment is placed. New crowns with new abutments are delivered 2 years 3 months postop (post Coronavirus lockdown).
Return to Lower Molar Immediate Implant, Armaments, 8, 10,19 4 手术 Application Xin Wei, DDS, PhD, MS 1st edition 01/21/2018, last revision 01/31/2021