,%20Vanilla.jpg)





,%20nearly%202%20y%20postop.jpg)
 |
 |
,%20Vanilla.jpg) |
 |
 |
 |
 |
 |
 |
 |
 |
 |
 |
 |
 |
,%20nearly%202%20y%20postop.jpg) |
Repair of Large Buccal
Plate Defect M
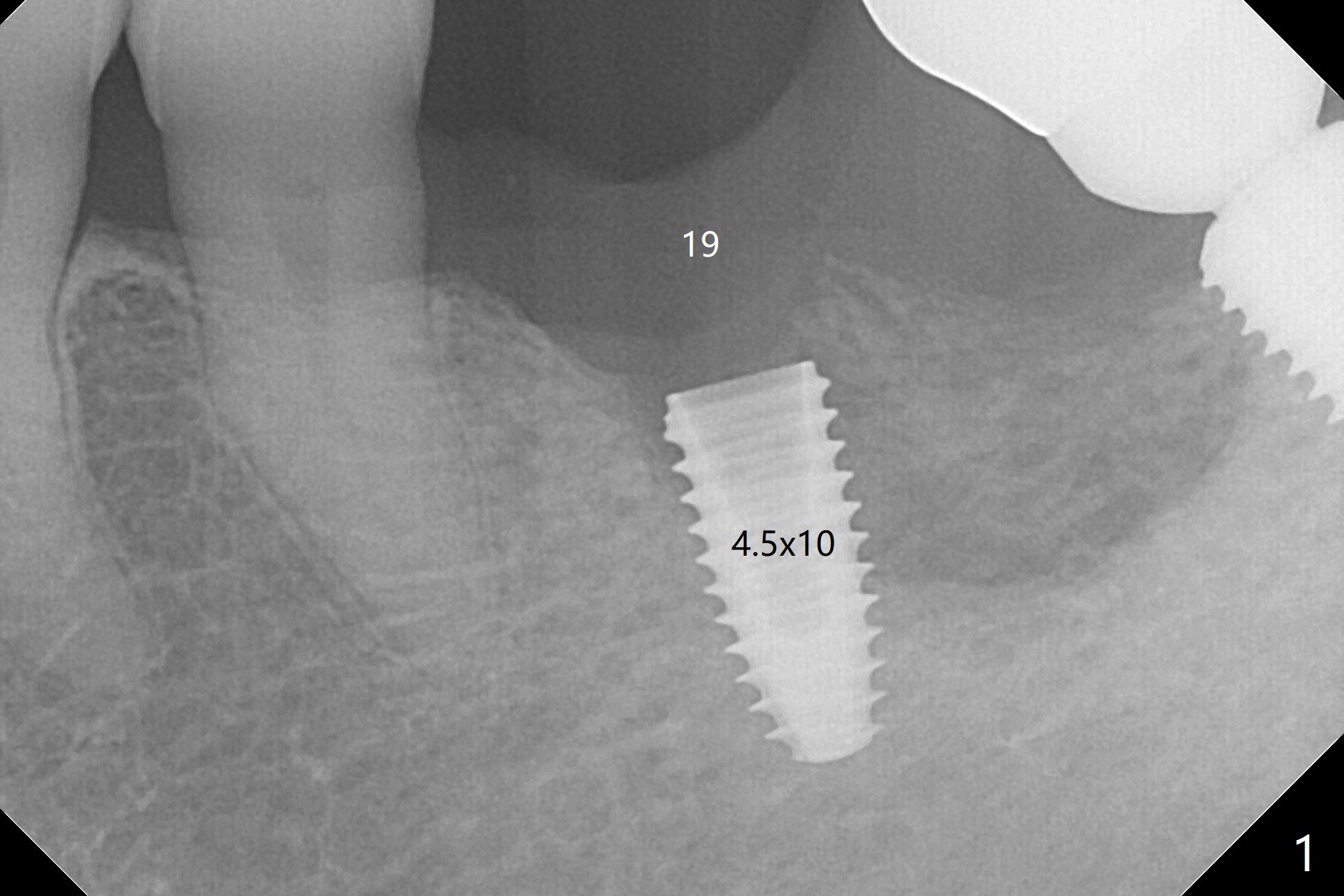
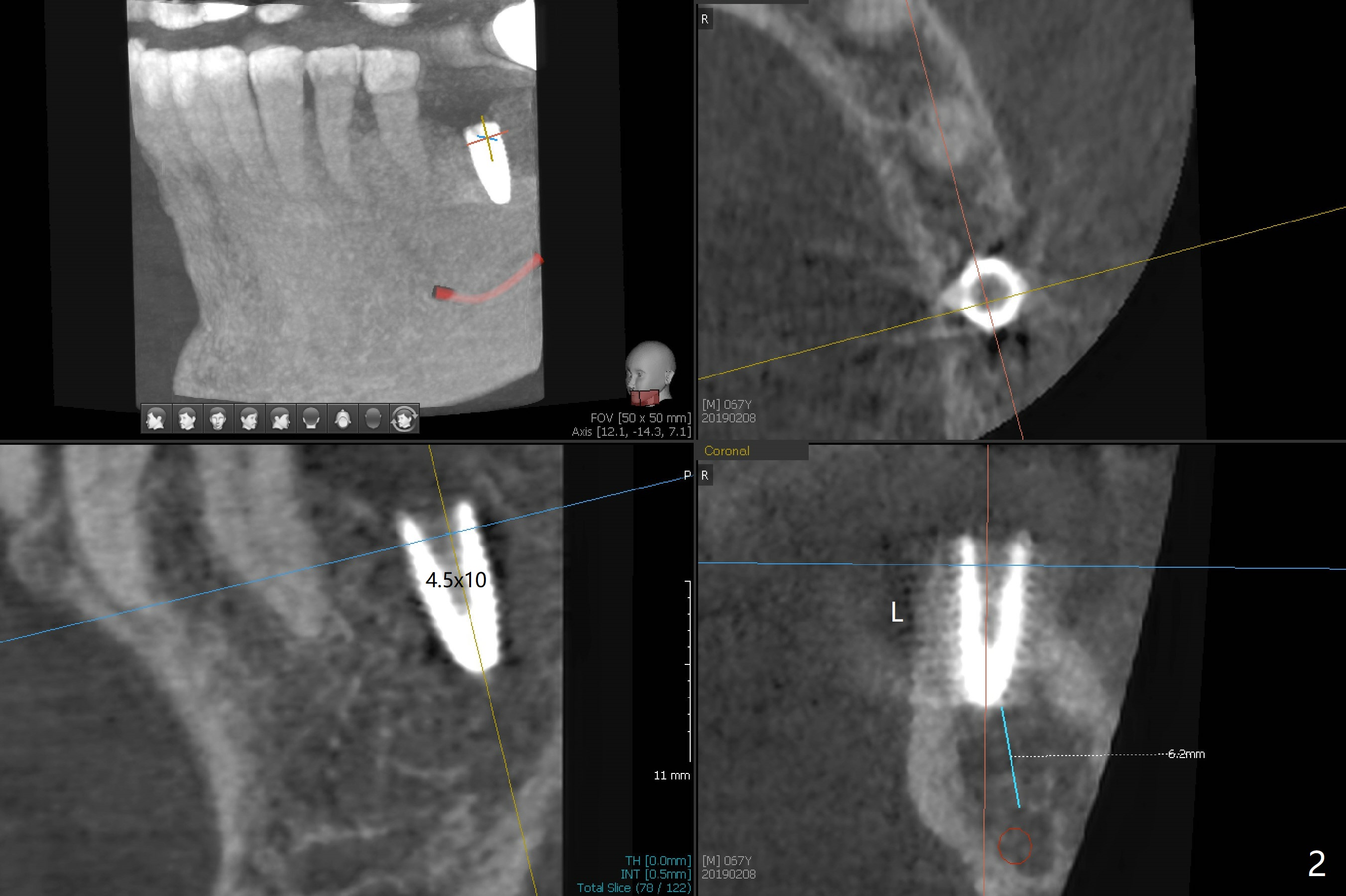
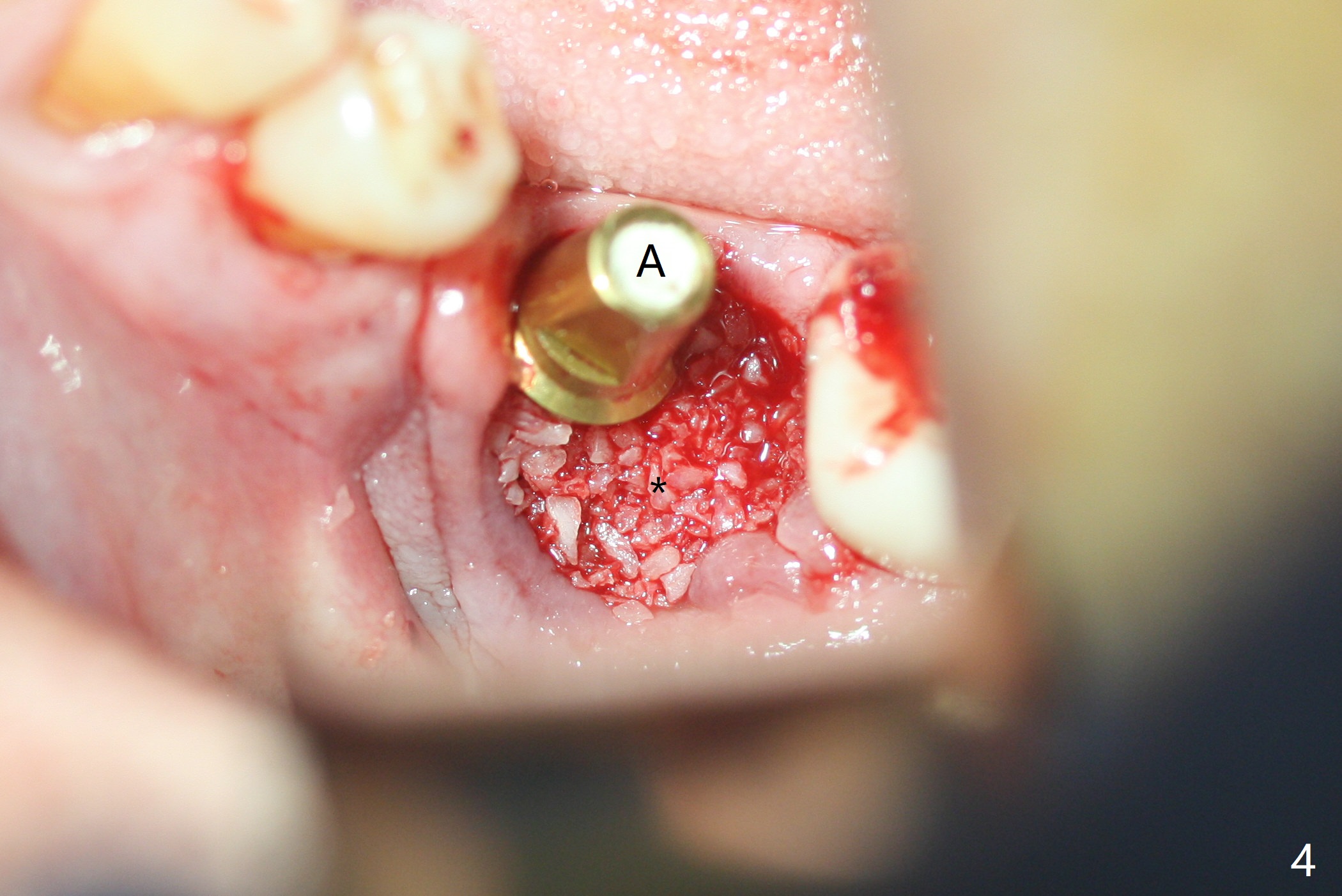
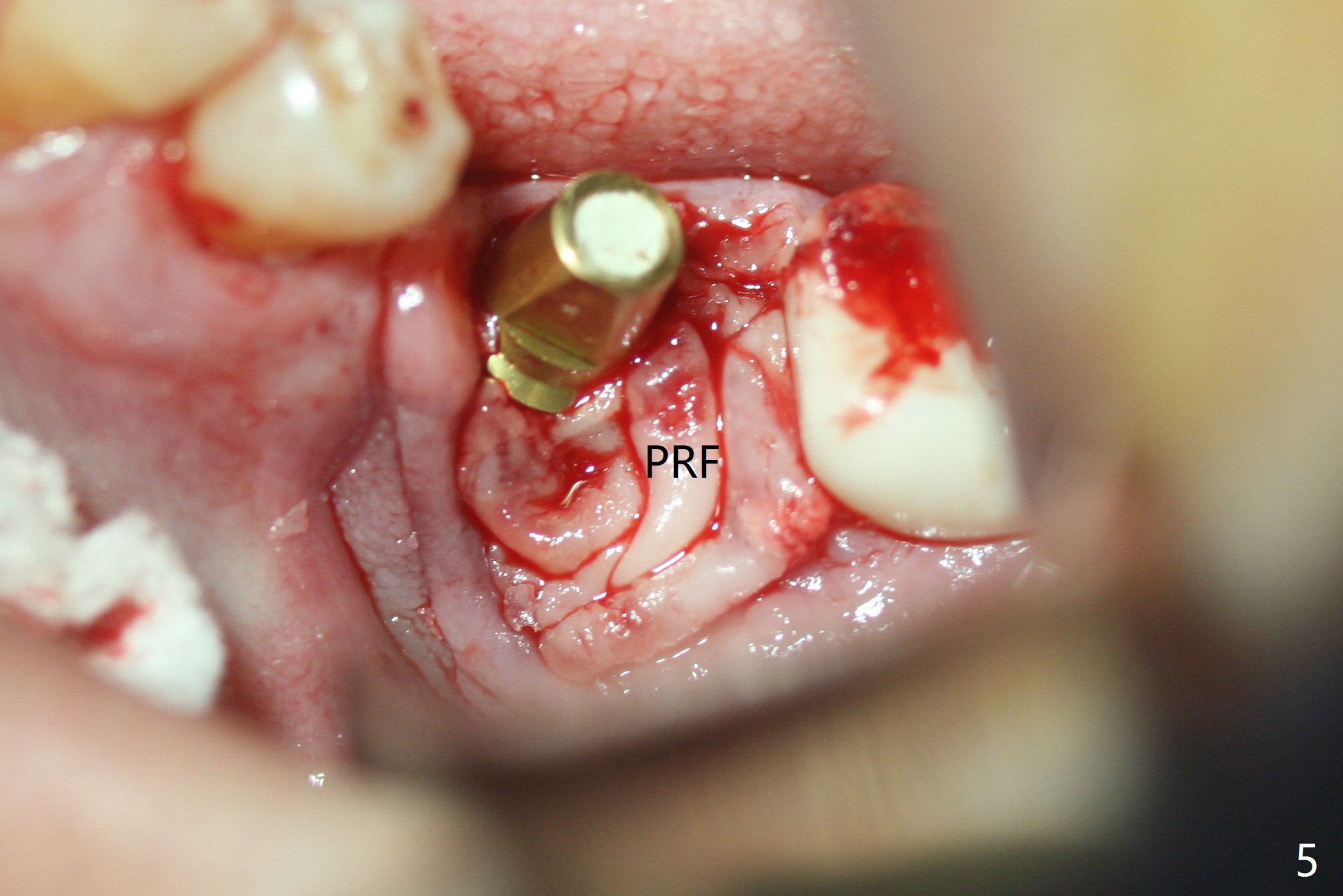
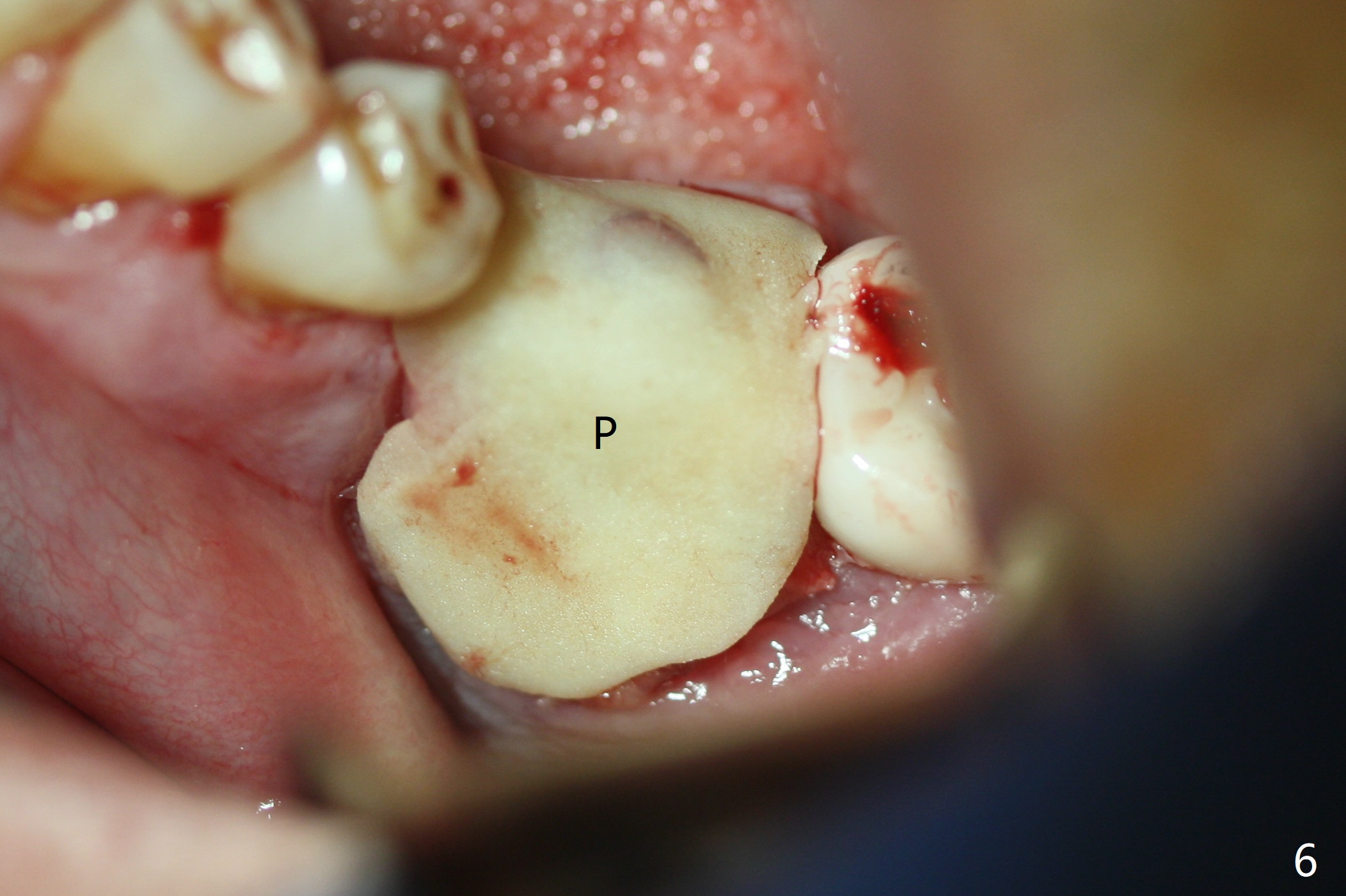
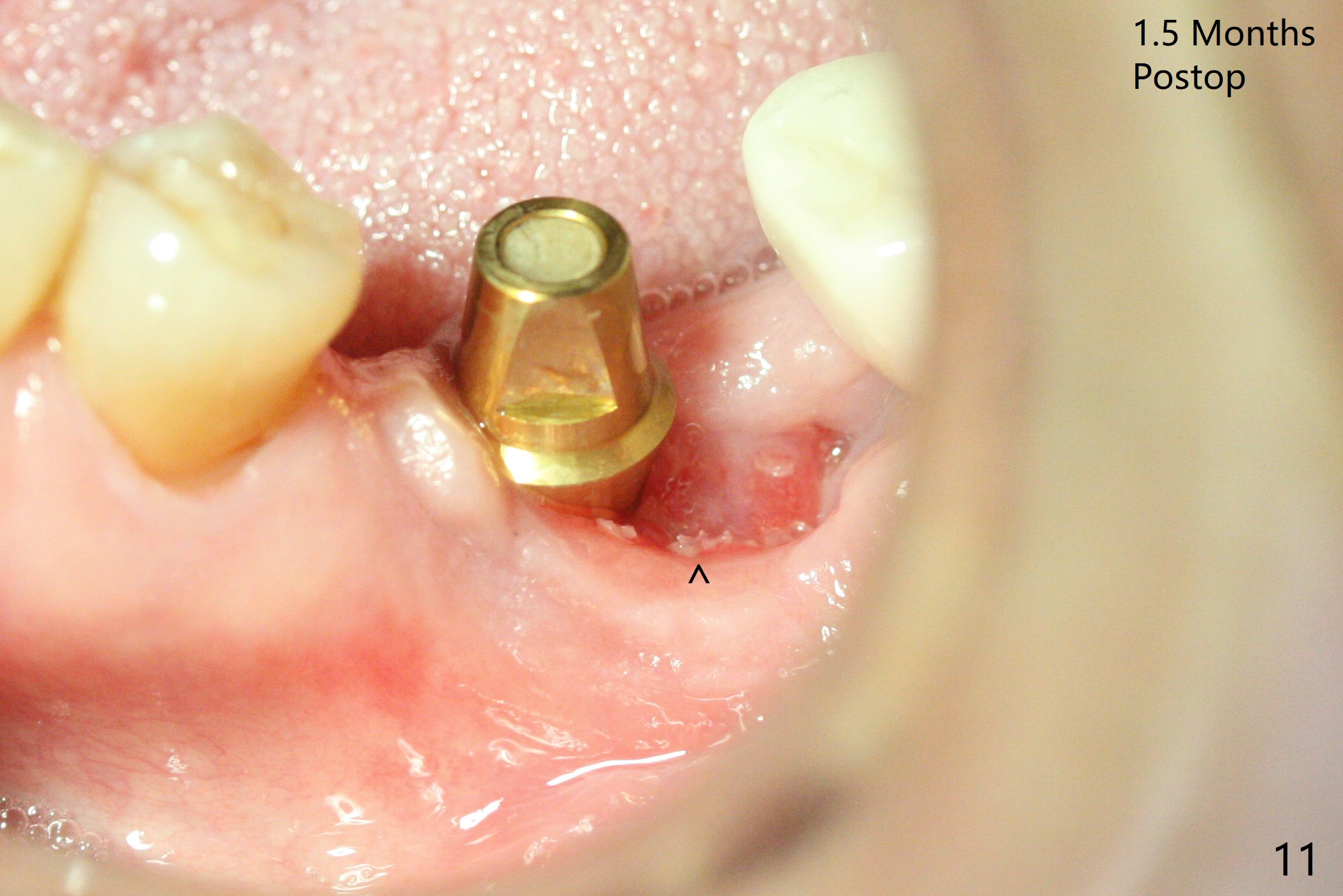
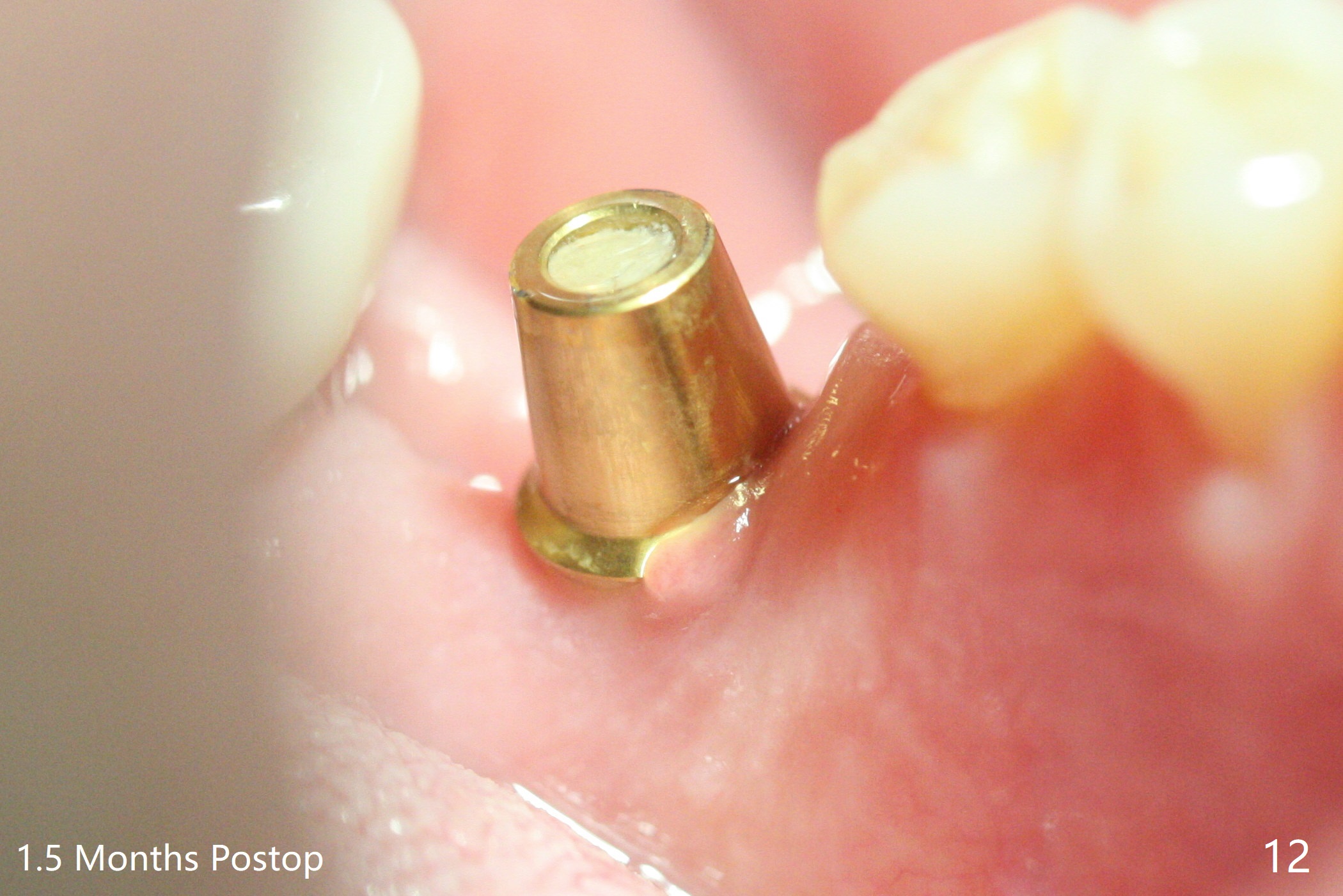
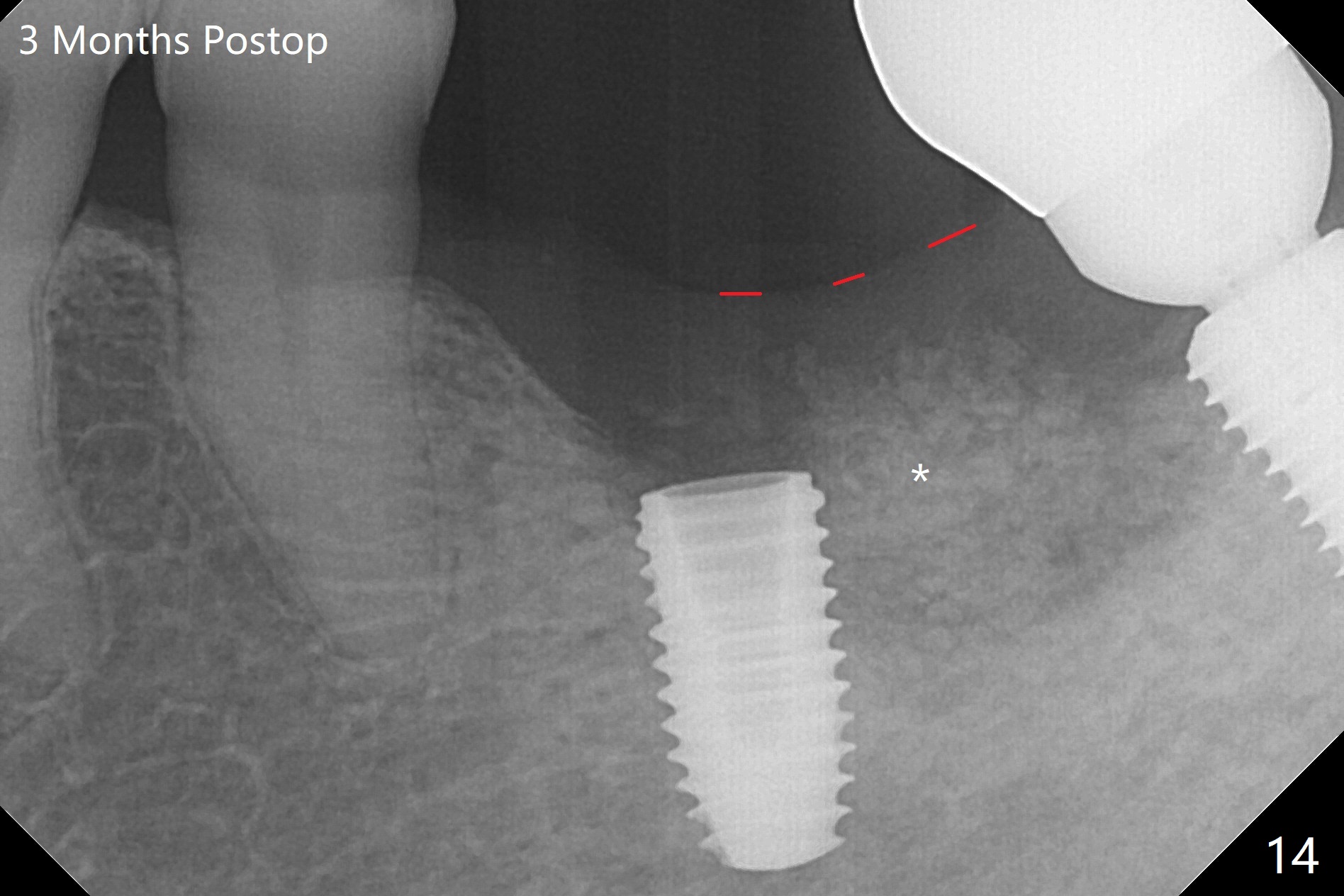
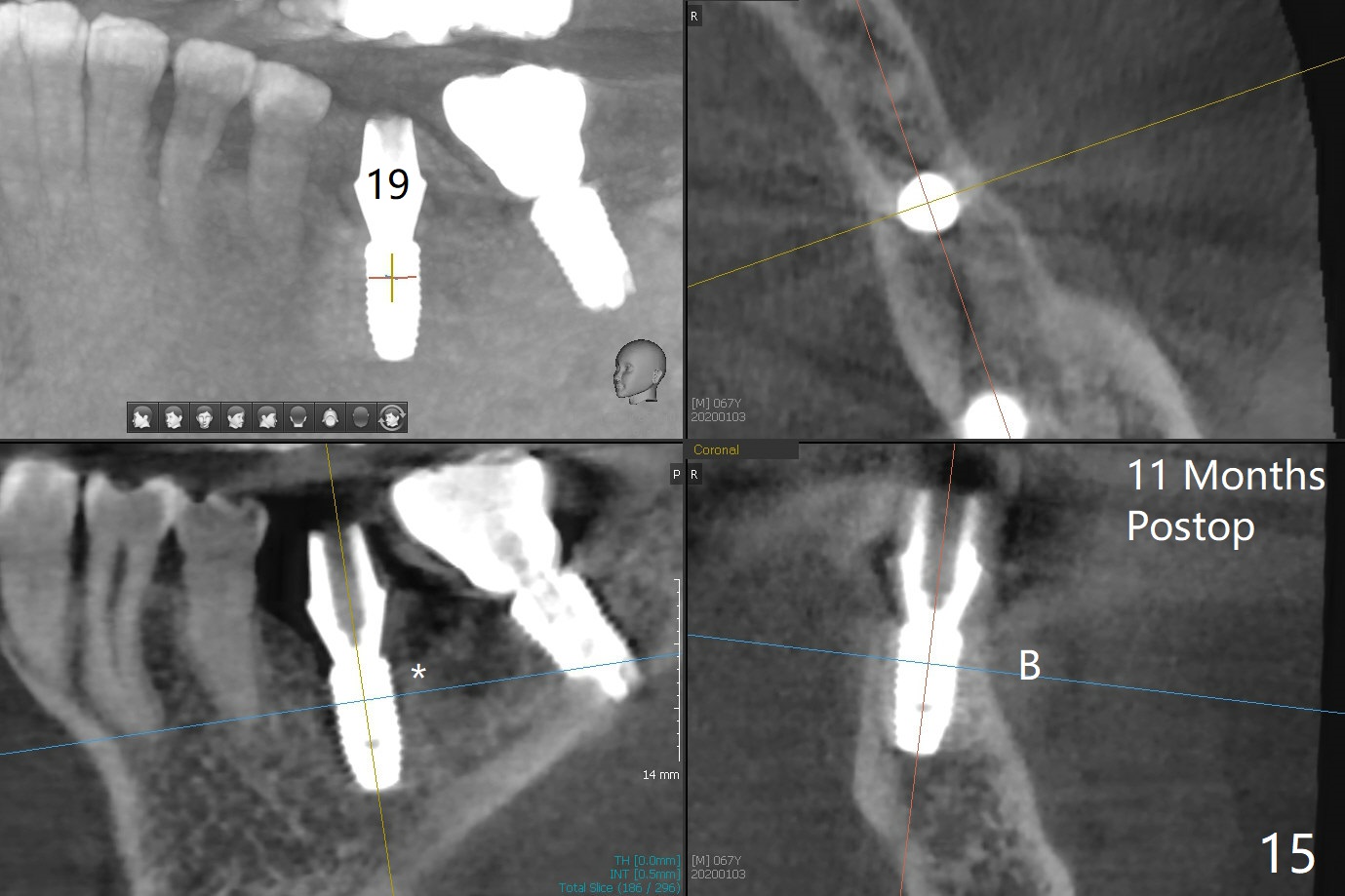
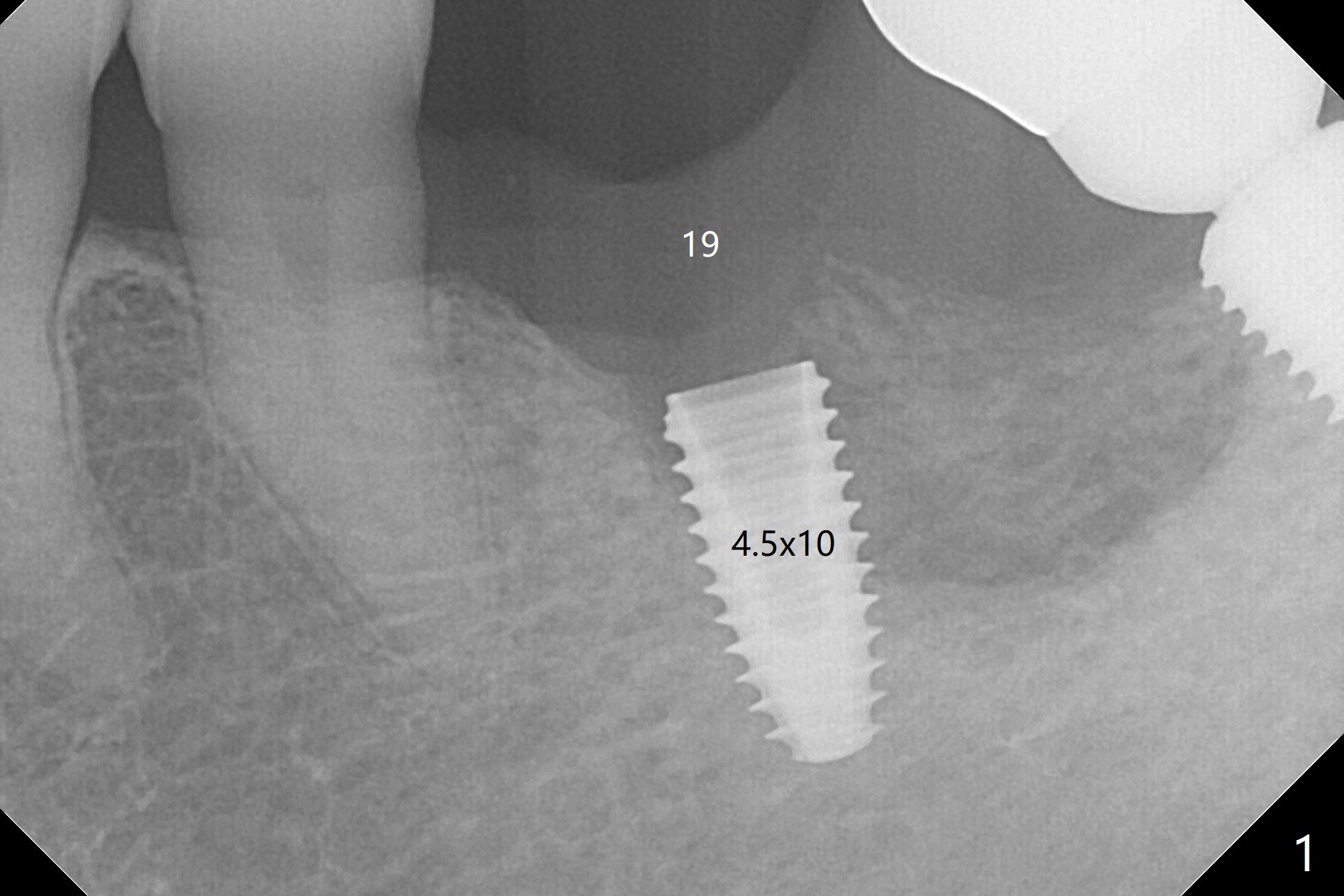
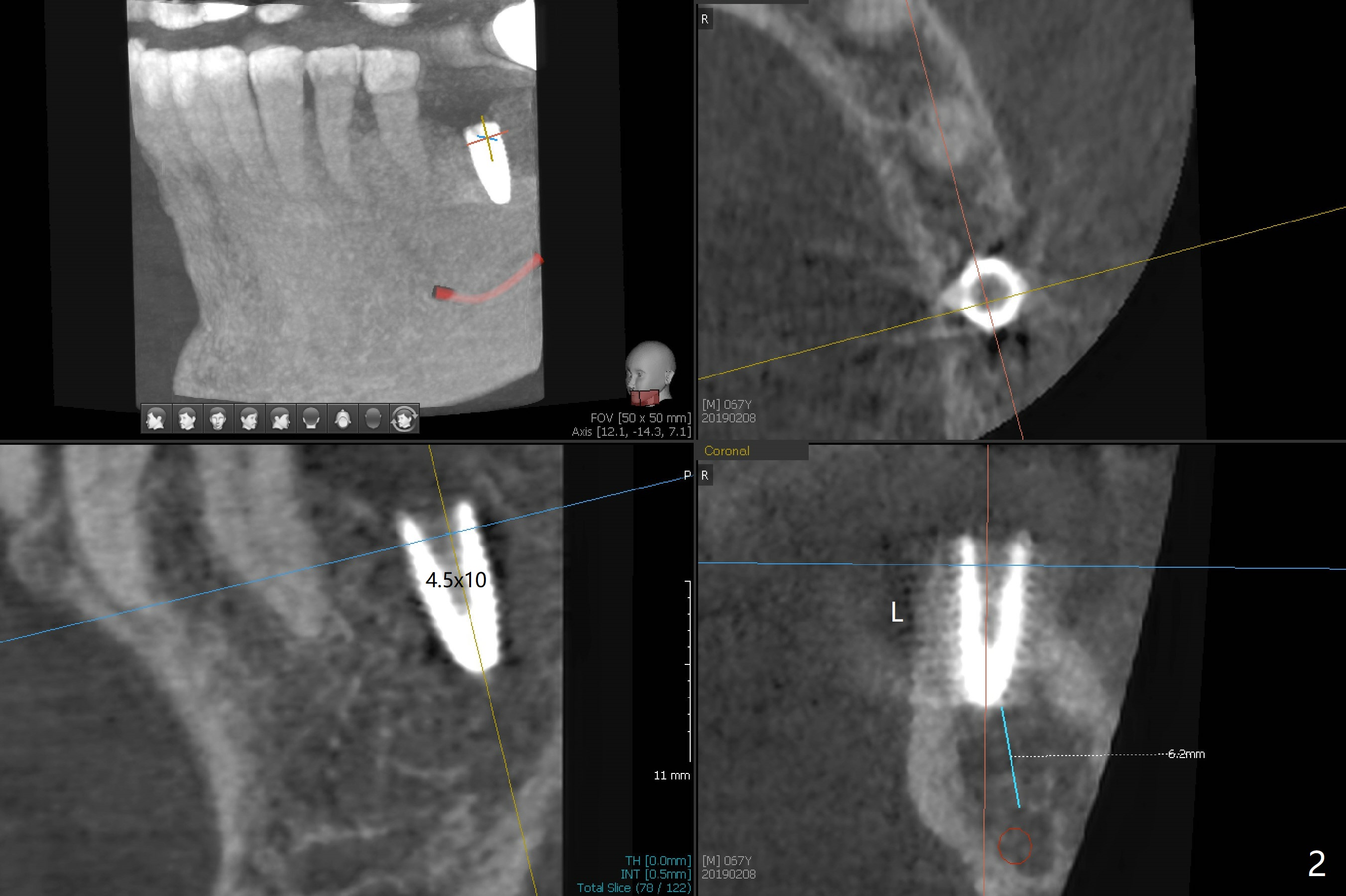
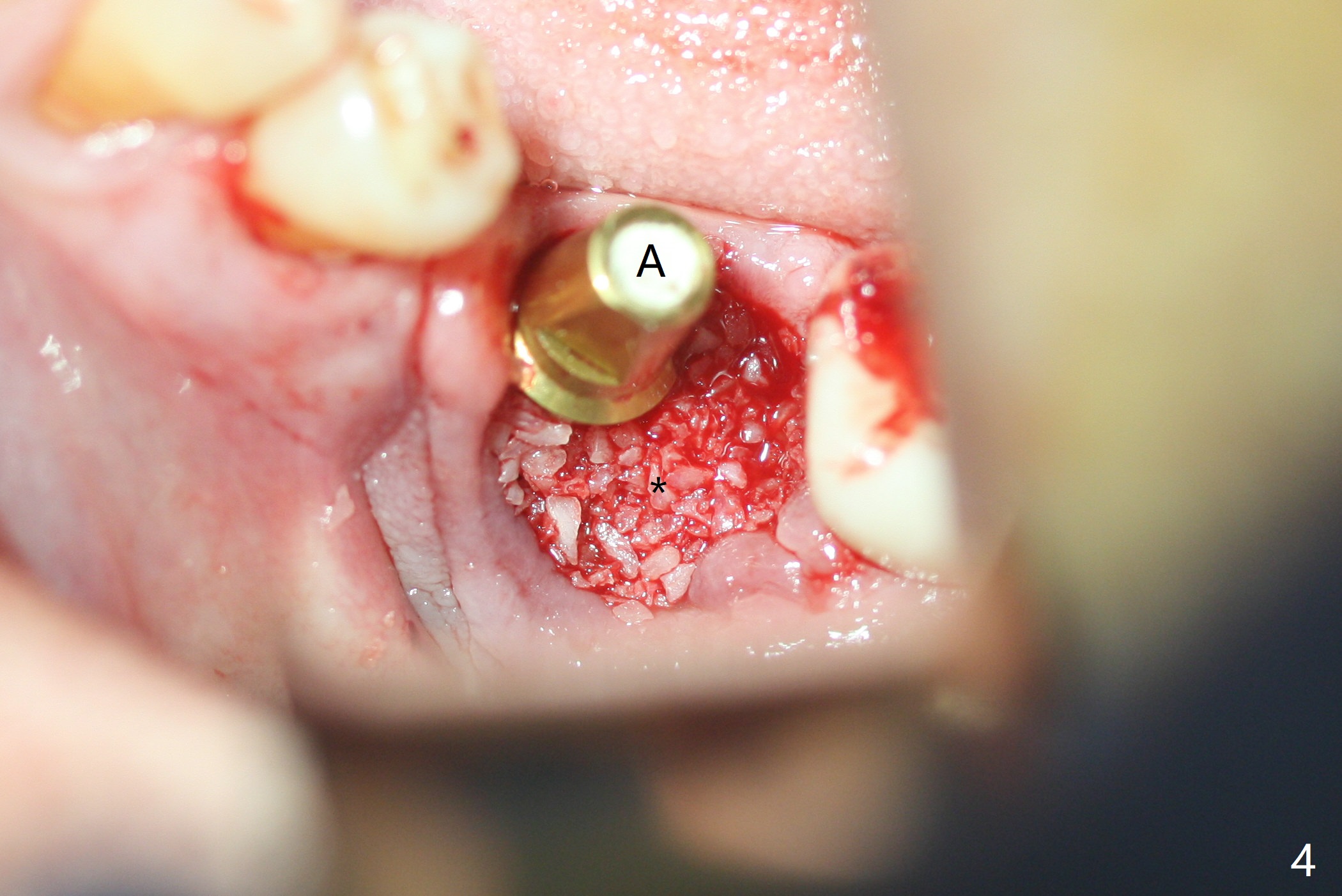
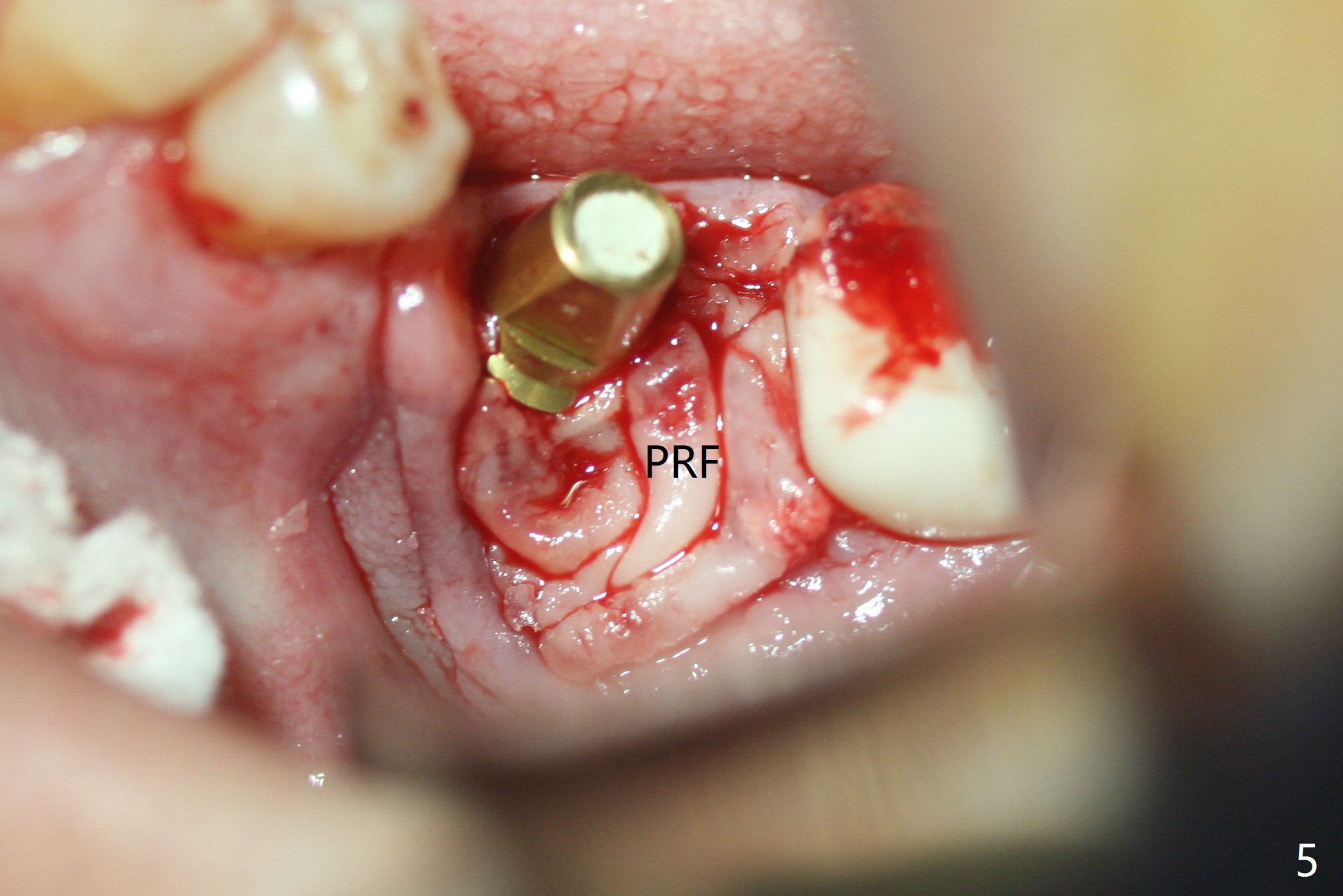
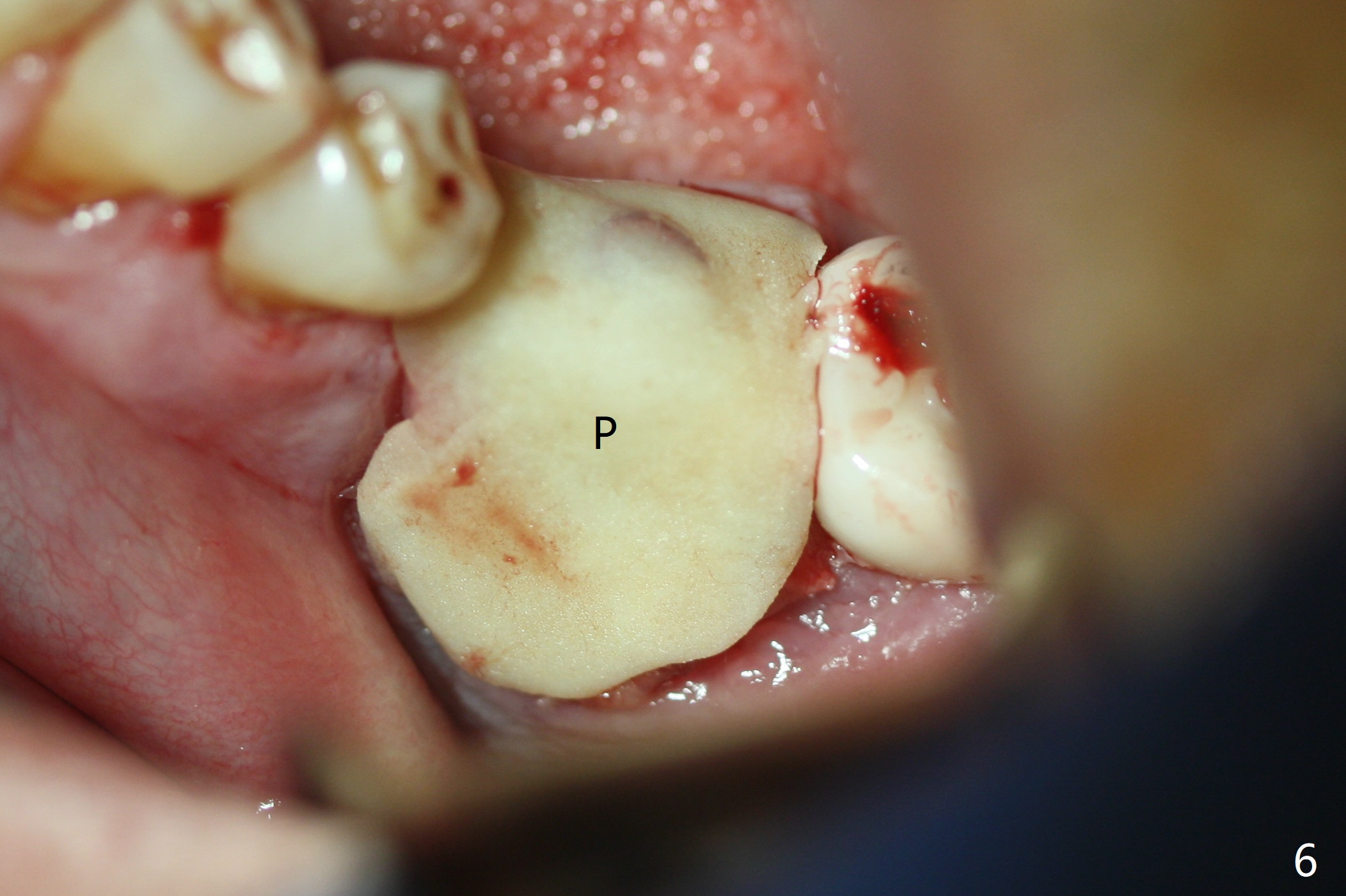
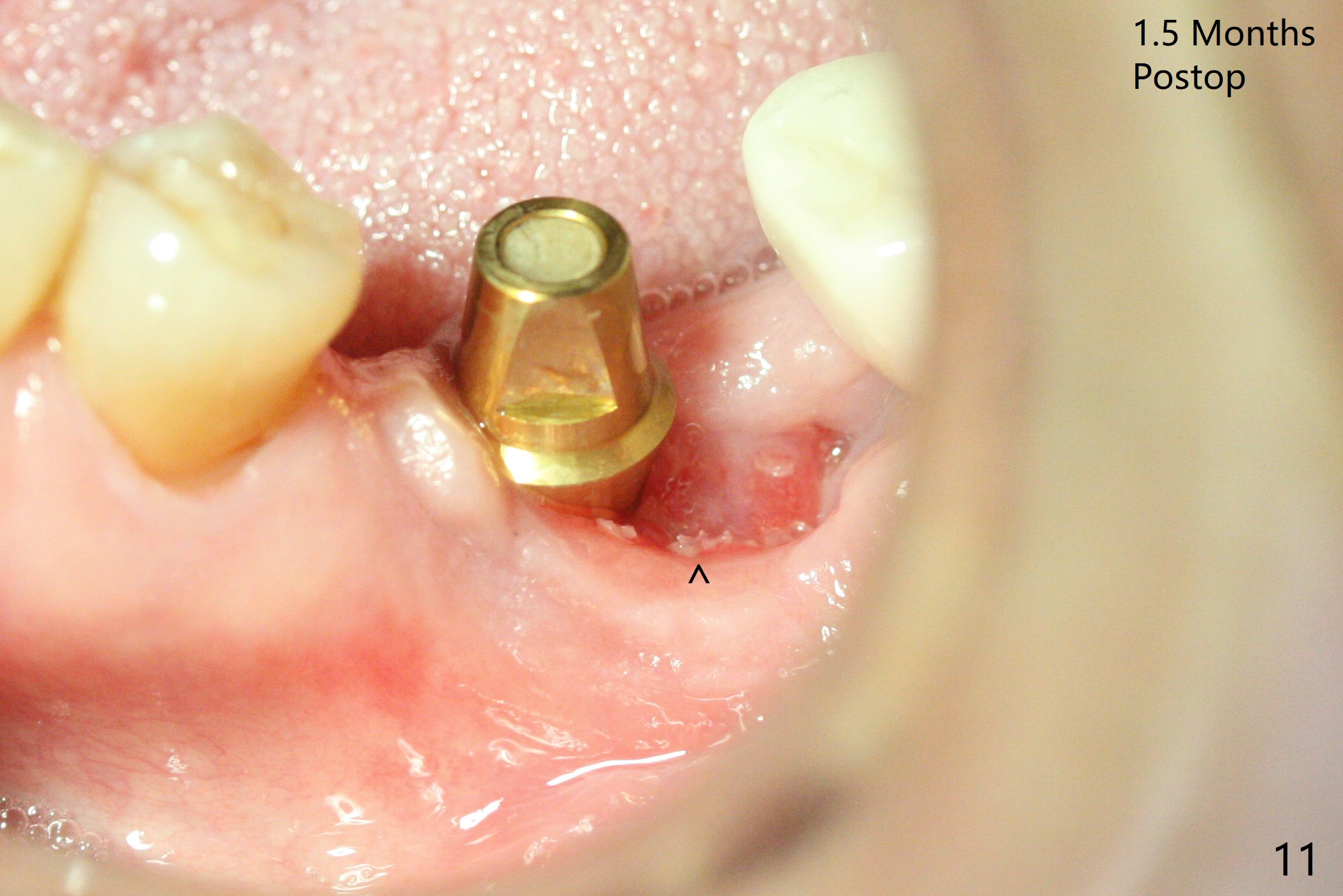
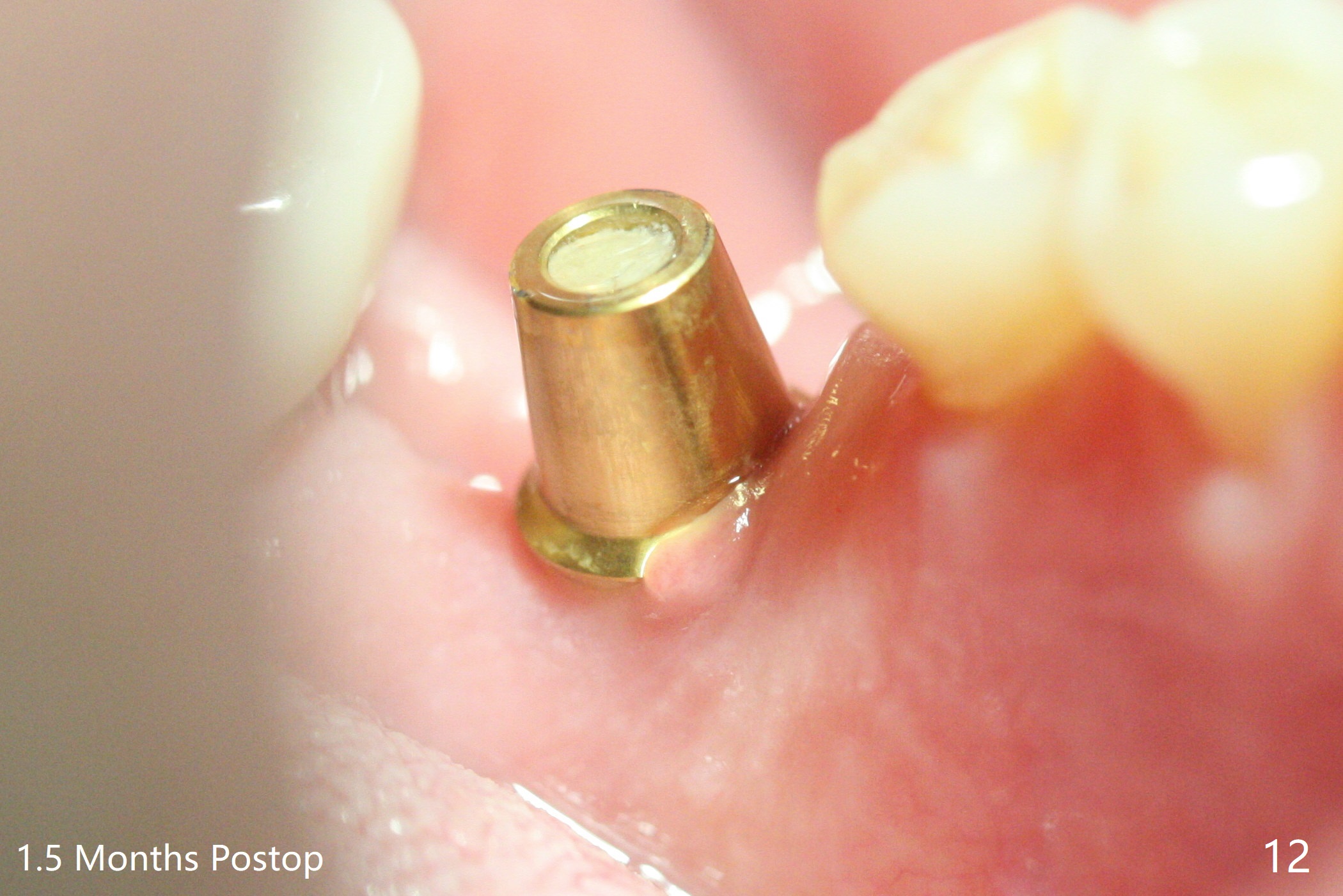
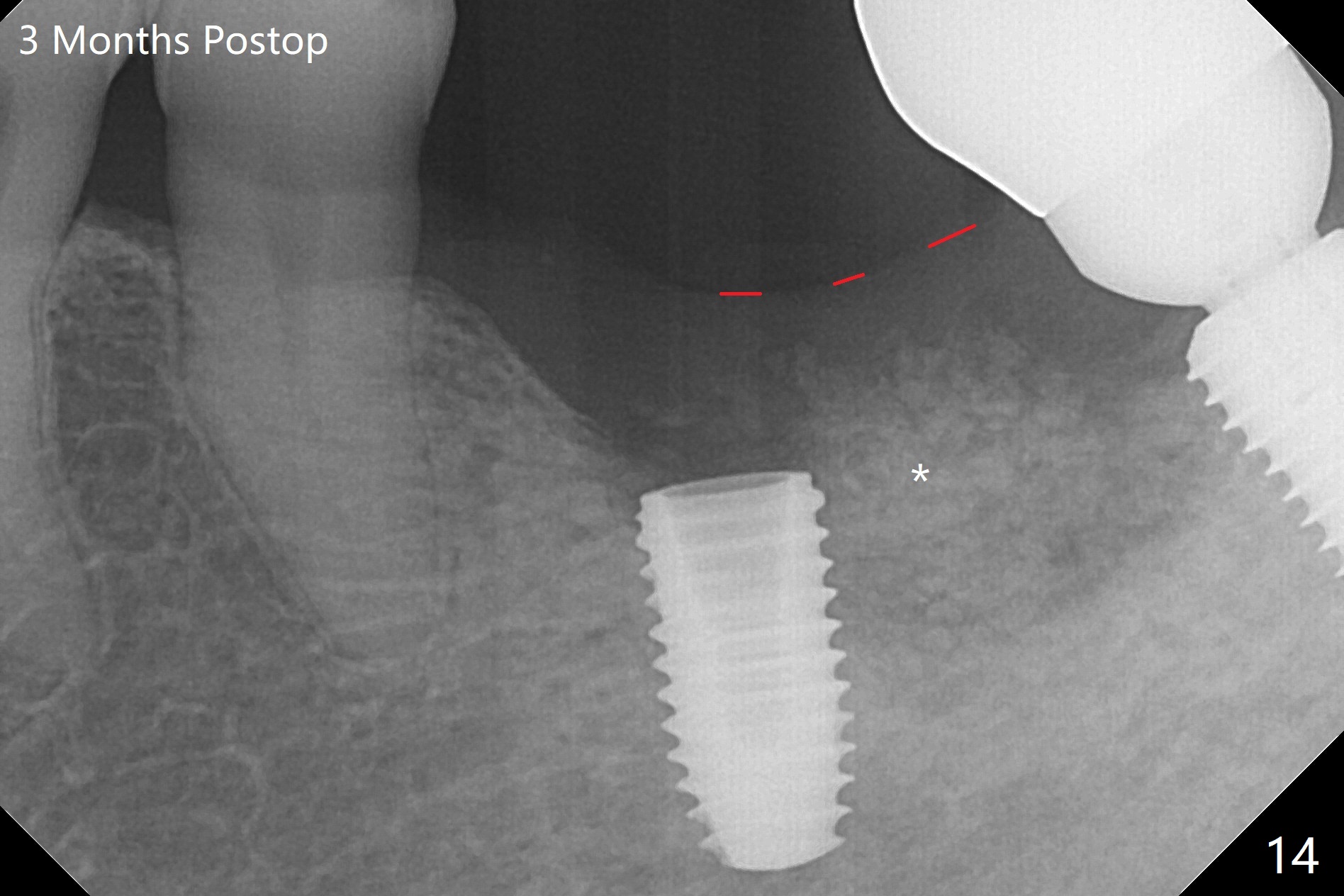
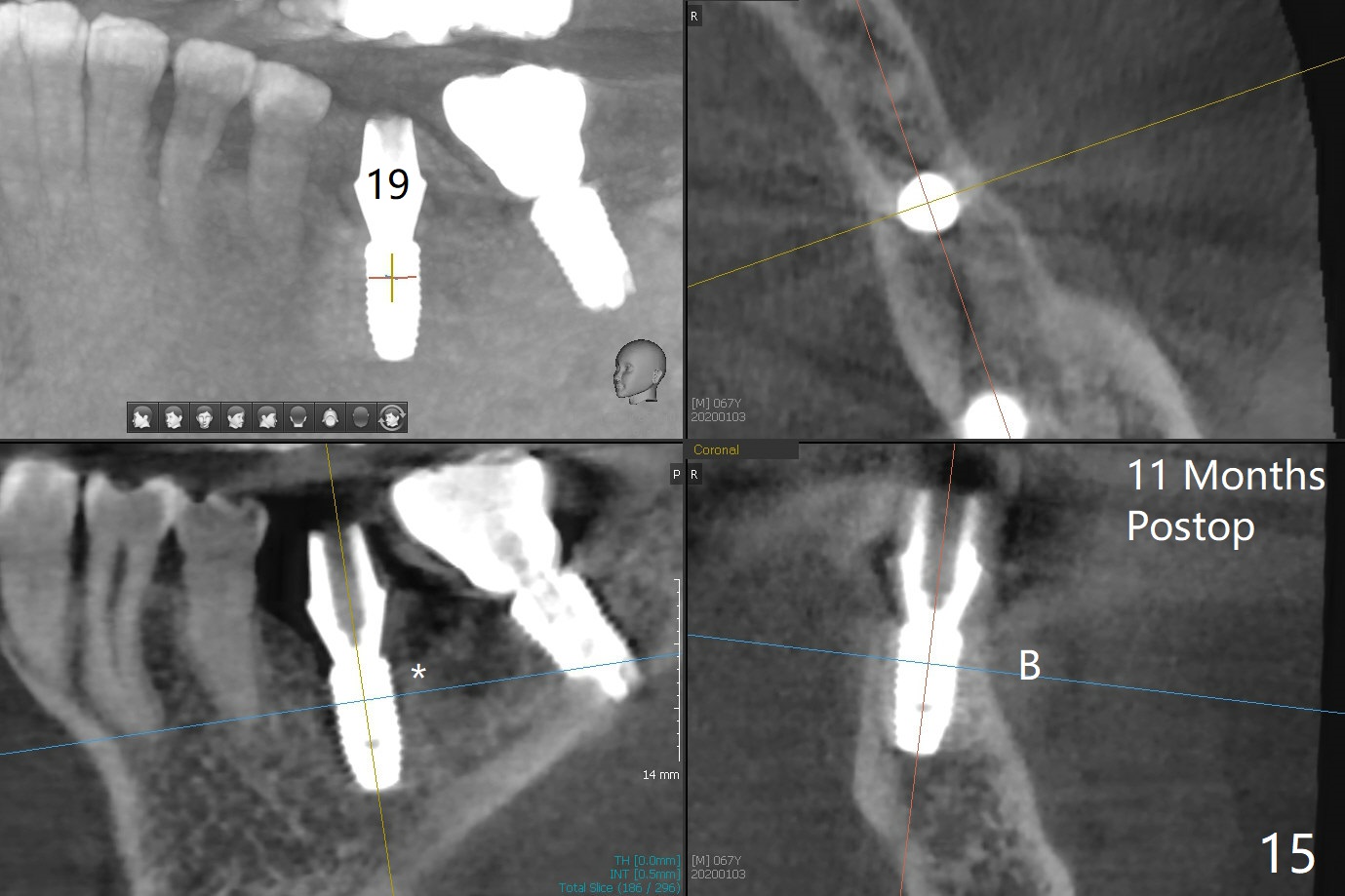
Probably due to severe infection at #19, pain control is difficult. Osteotomy has to be stopped 1.5 mm short of the design. PA taken with a 4.5x10 mm dummy implant does not show the Inferior Alveolar Canal (Fig.1), whereas CT does (Fig.2). With 6 mm clearance, block anesthesia is administered. A 5x10 mm definitive implant is placed with ease (Fig.3). The buccal bony defect is repaired by allograft (Fig.3,4 *), while the soft one by 3 pieces of PRF membrane (Fig.5). The latter is fixed in place by applying setting acrylic as an immediate provisional (Fig.6 P) over the wound, around the abutment (A) and locking into the undercut of the neighboring tooth/implant crown. The patient feels great postop. The gingiva is healthy around the provisional 8 days postop (Fig.7). The patient remains asymptomatic with the healthier gingiva surrounding the simplified provisional 22 days postop, as compared to 8 days postop (Fig.8). The socket heals when the simplified provisional is removed 1.5 months postop (Fig.9-12). The bone graft (Fig.11 ^) seems to have become a part of the regenerated gingiva. The abutment has been dislodged for 2 week (Fig.14 (3 months postop). The bone graft, albeit decreased, is 2 mm subgingival (red dashed line). There is bone distal to the implant 11 months postop (Fig.15 *). There is no bone loss 2 years postop; the UF abutment is completely seated (Fig.16).
Return to
Lower
Molar Immediate Implant,
Prevent Molar Periimplantitis (Protocols,
Table),
Trajectory,
Metronidazole
31
7
Application
临时牙冠失败病例
第一磨牙即种
Xin Wei, DDS, PhD, MS 1st edition
02/08/2019, last revision
04/28/2021