.jpg)



 |
 |
 |
 |
|
.jpg) |
 |
 |
 |
|
 |
 |
 |
||
Incisive Canal
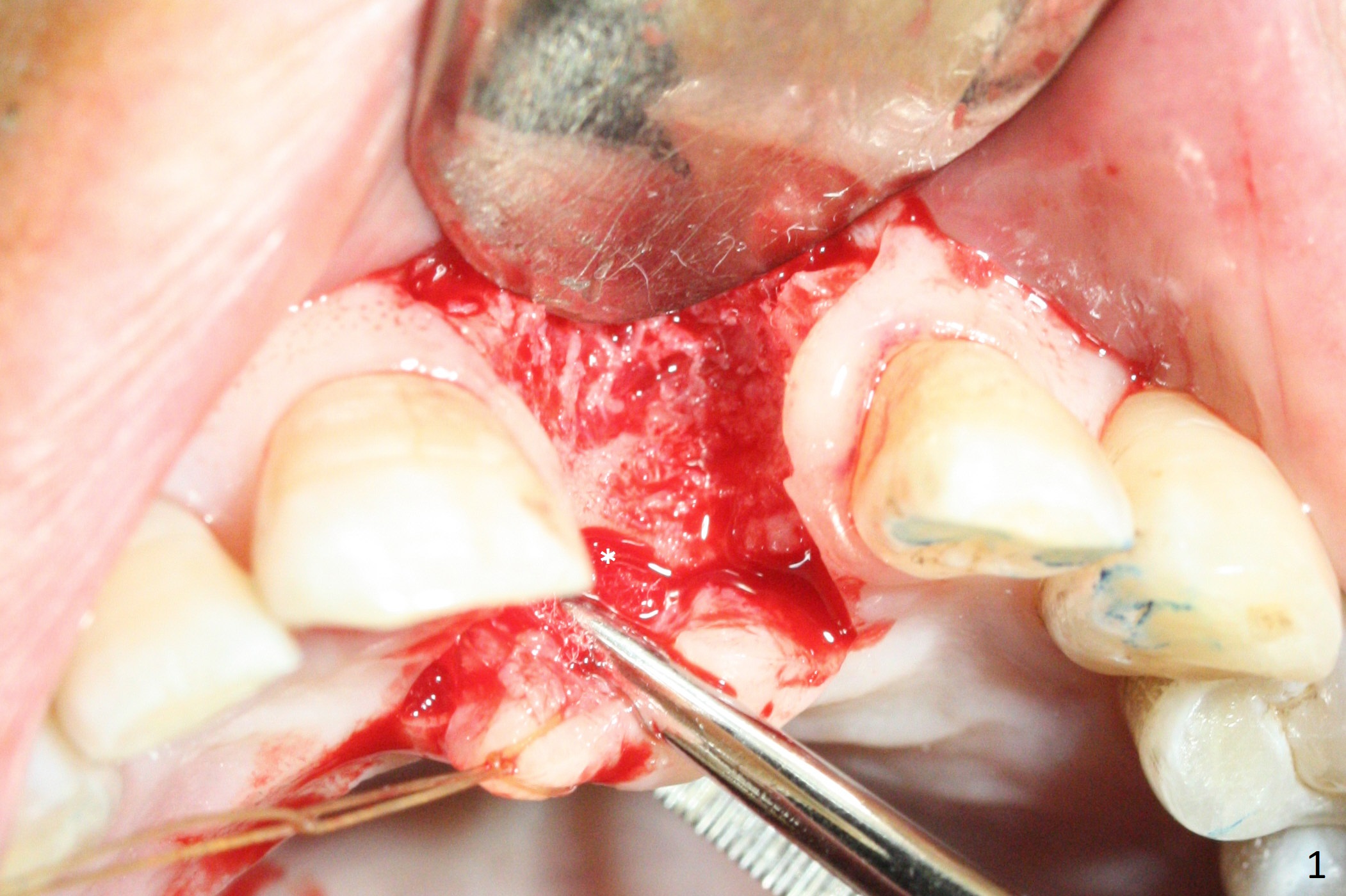
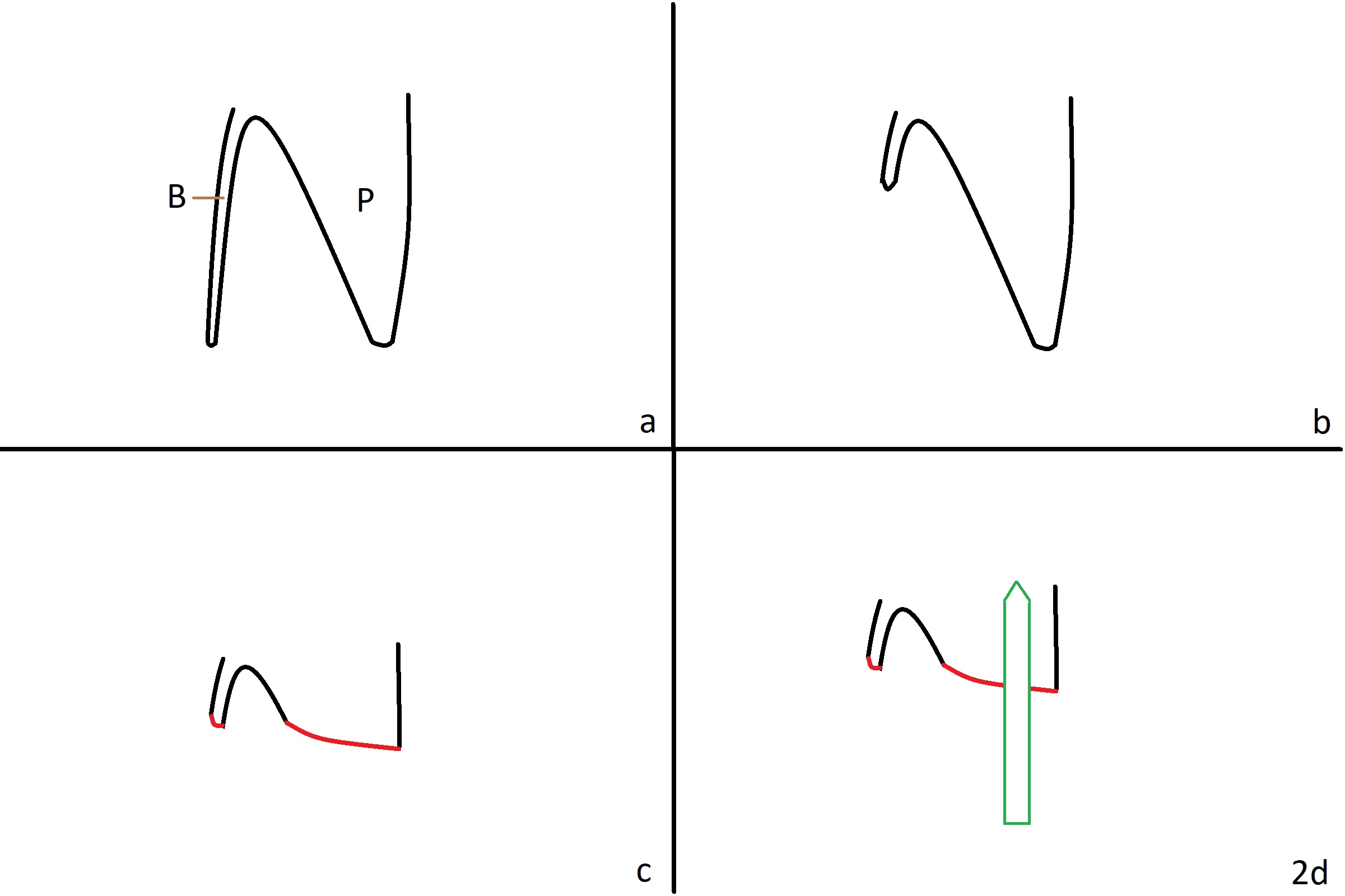
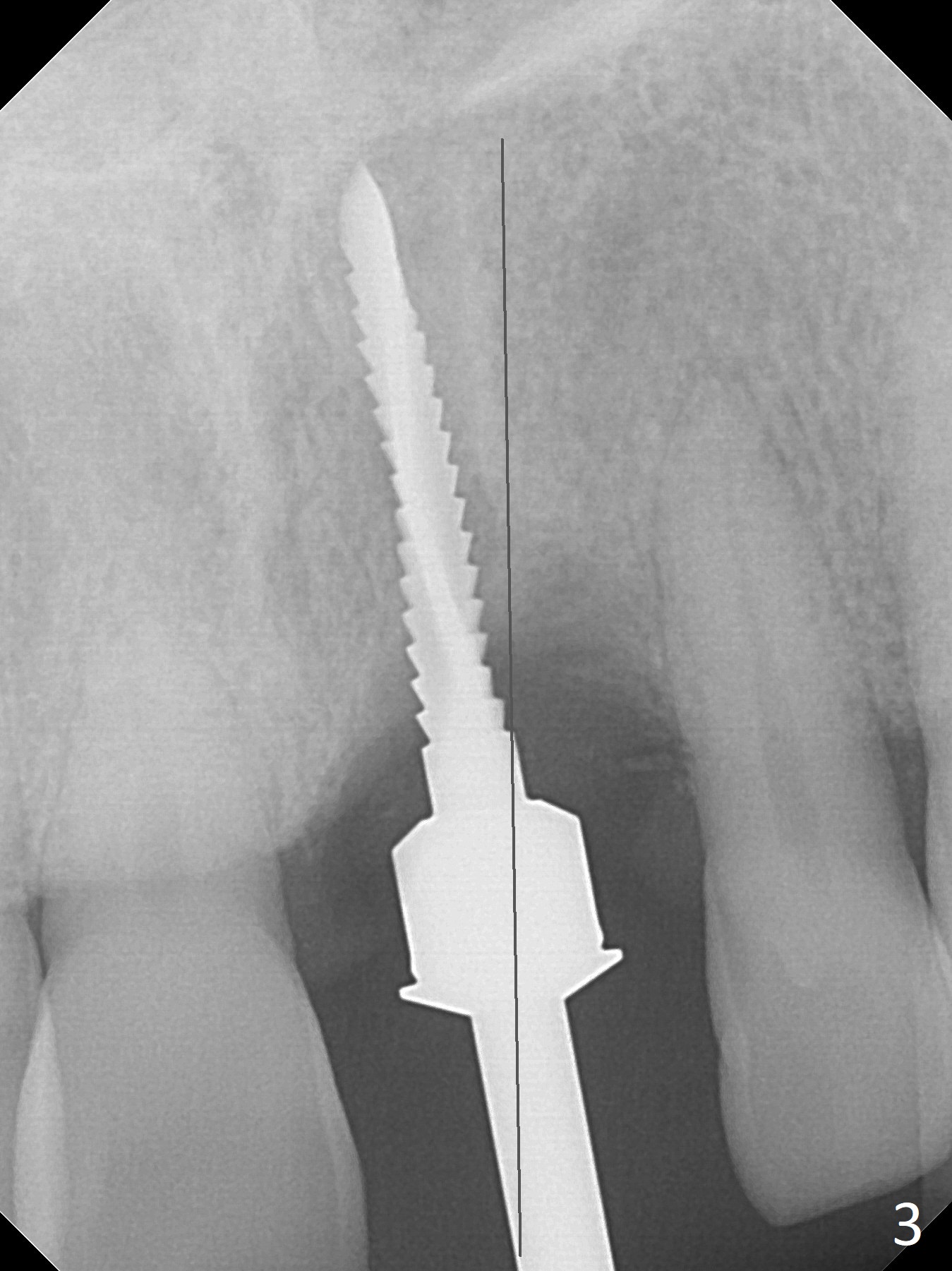
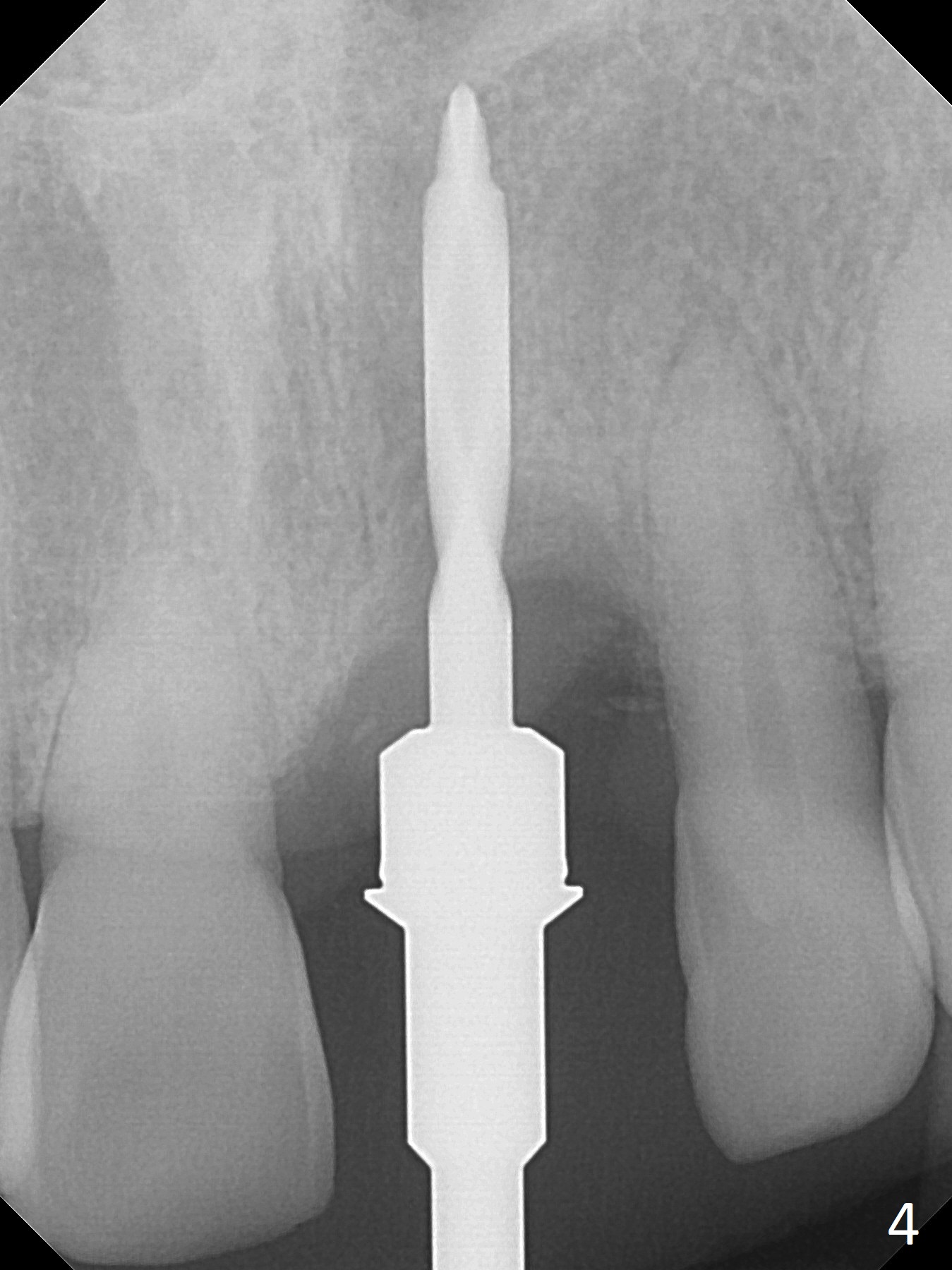
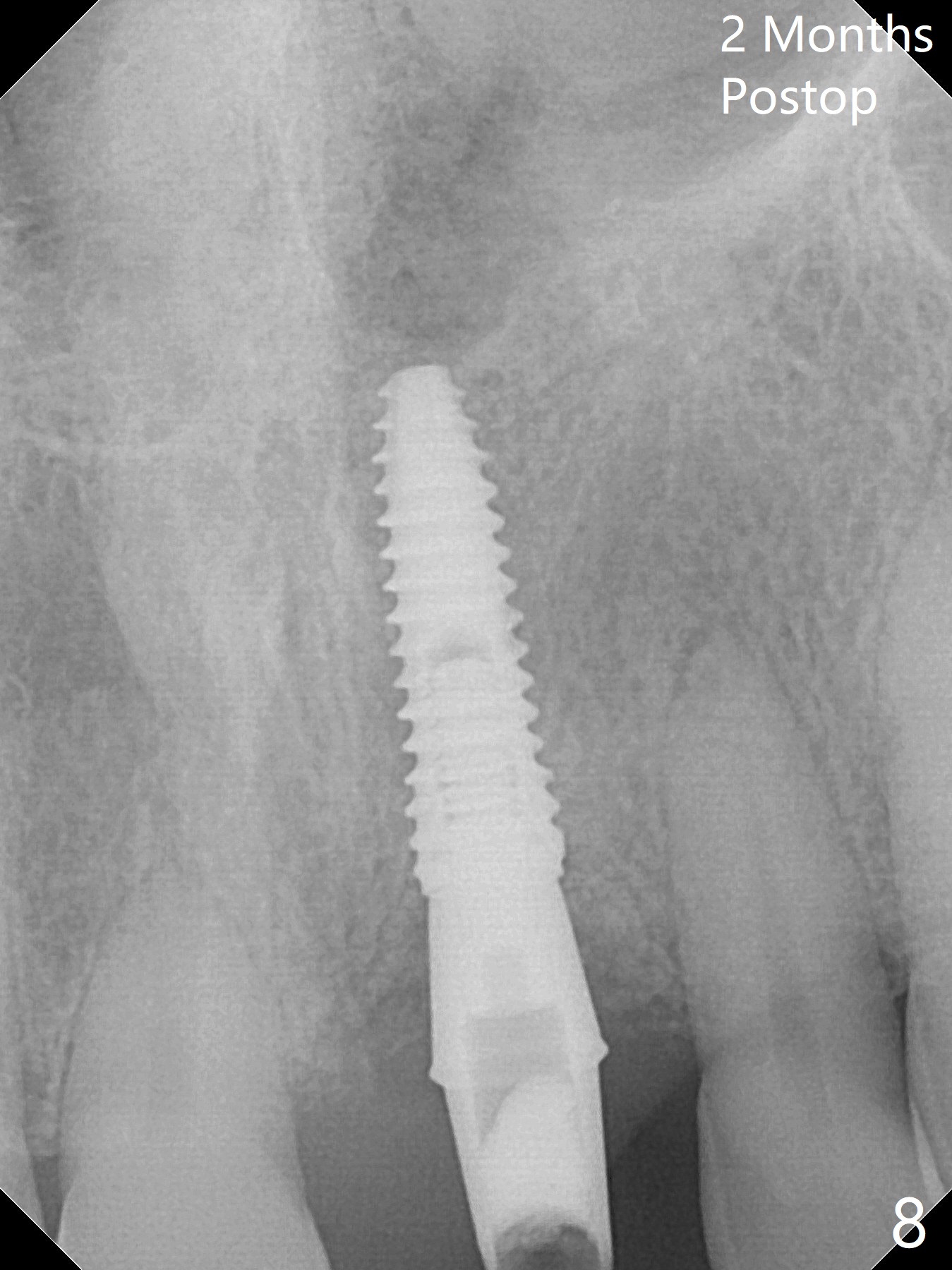
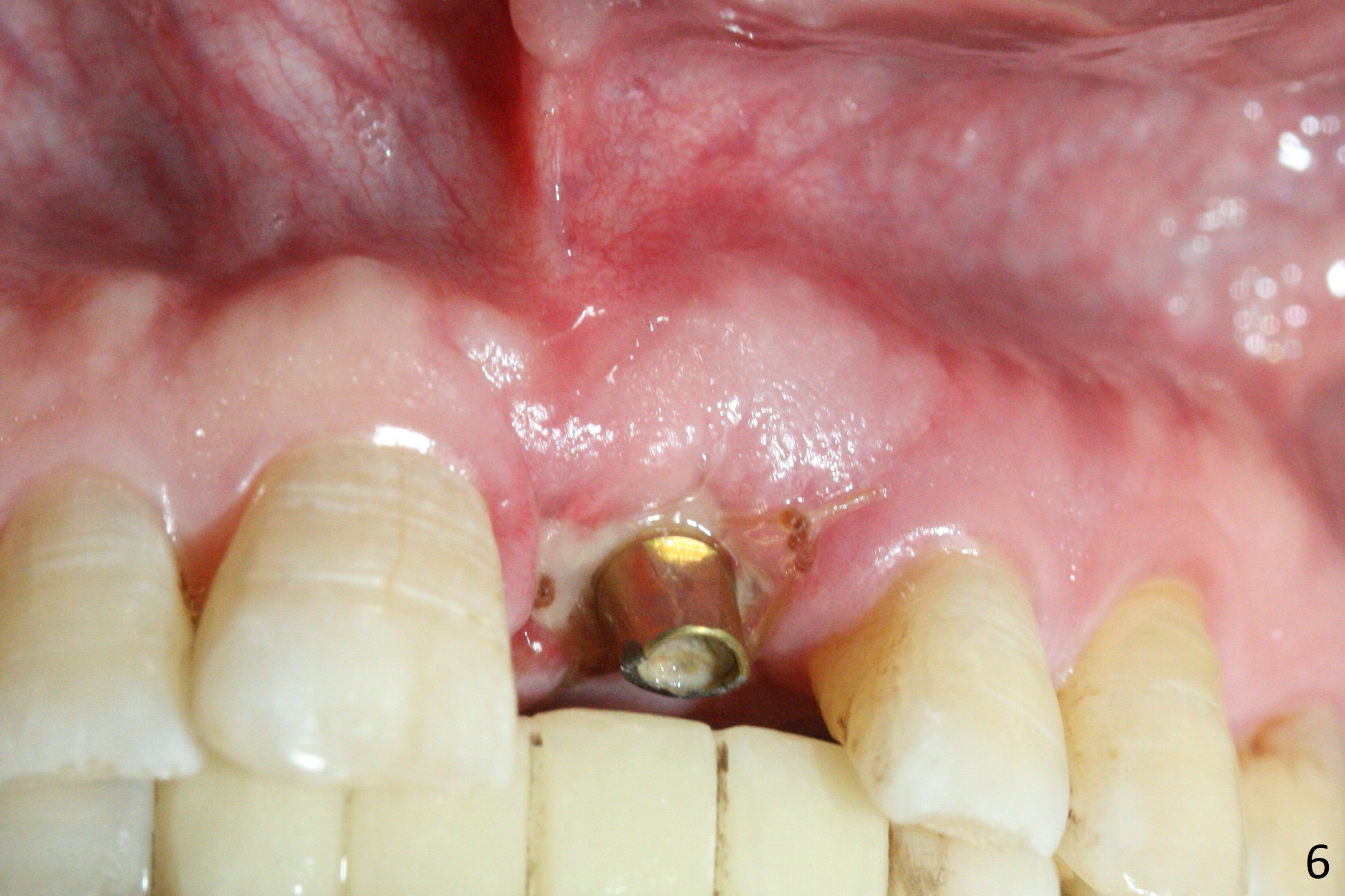
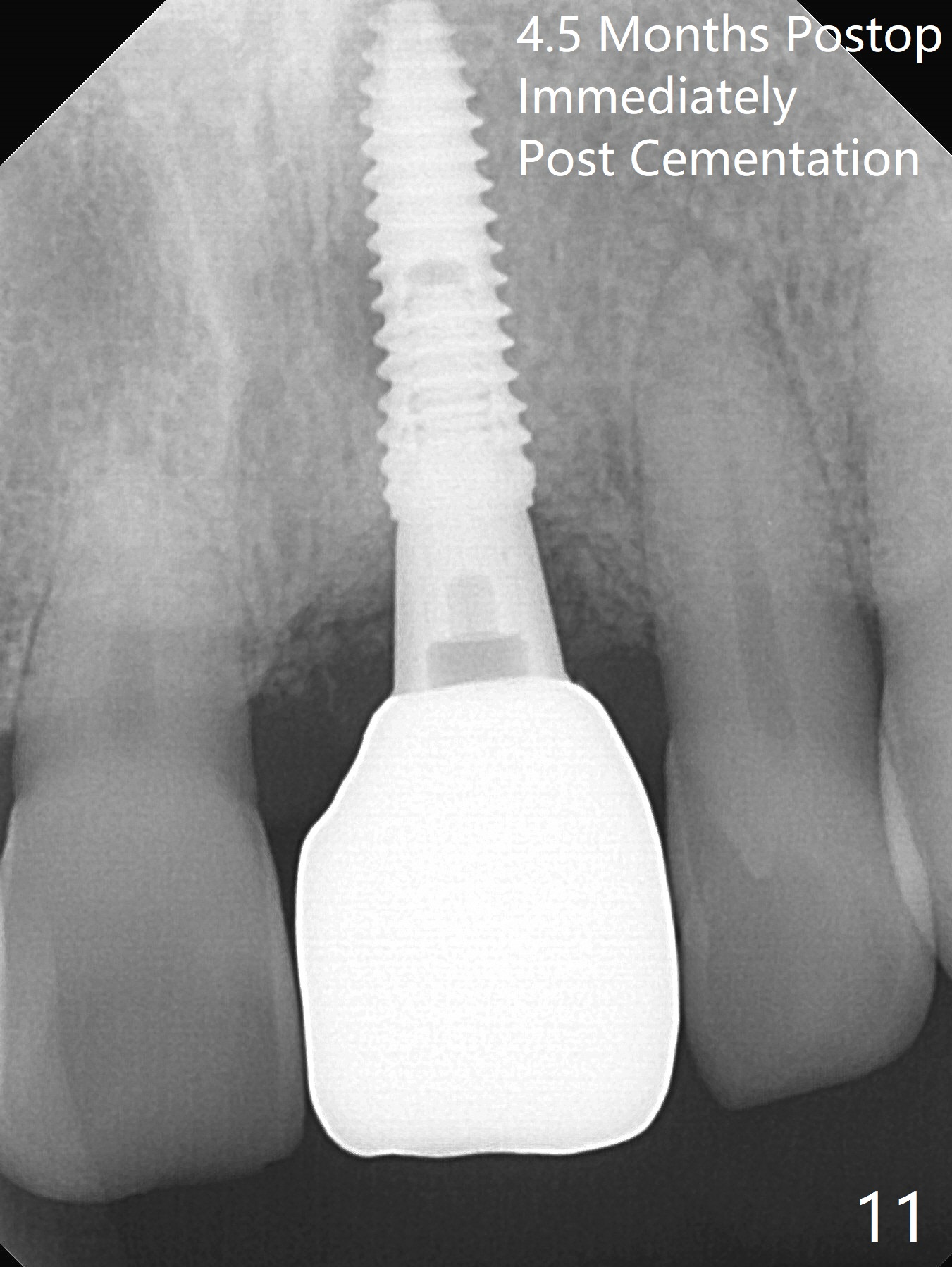
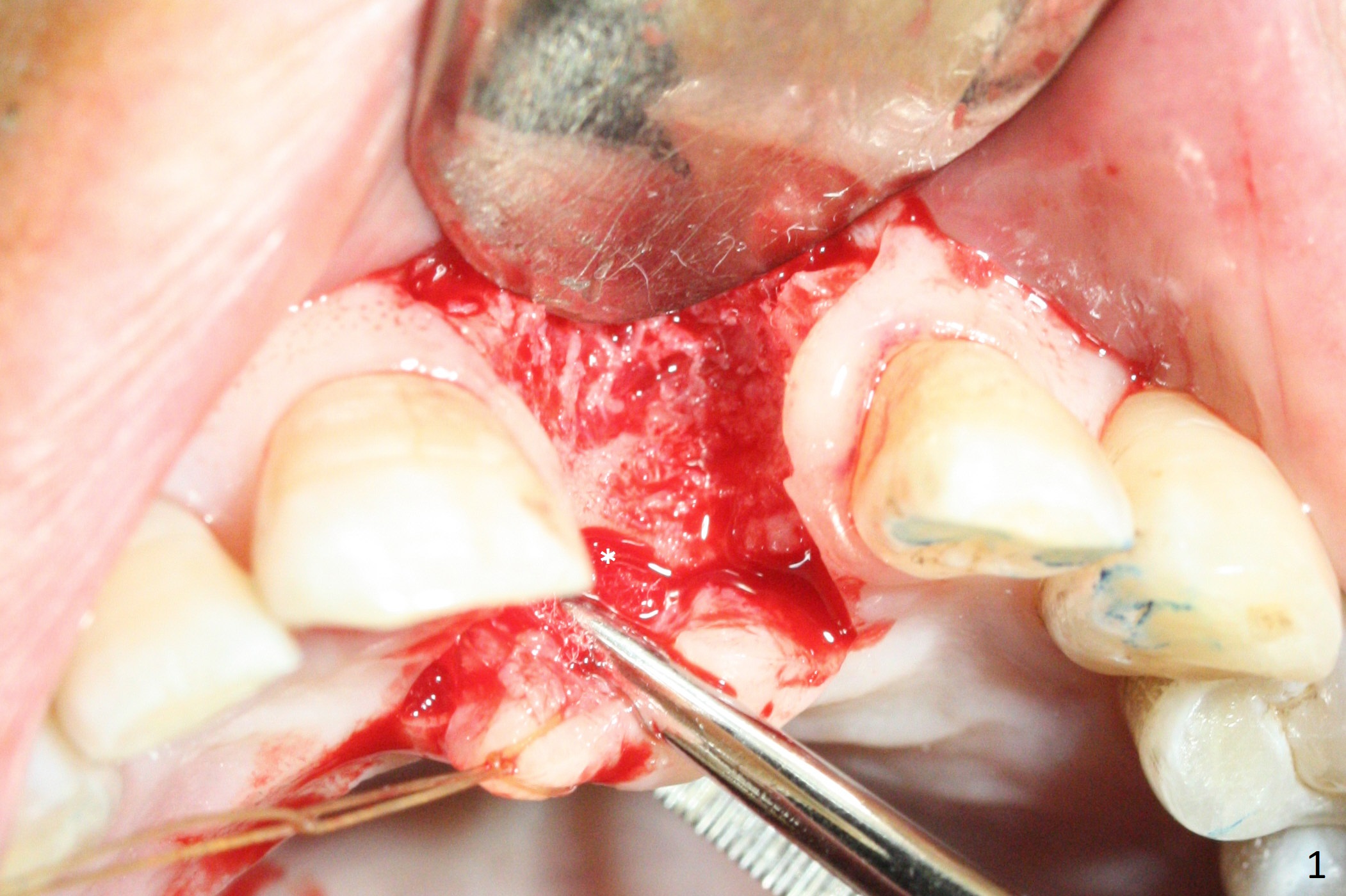
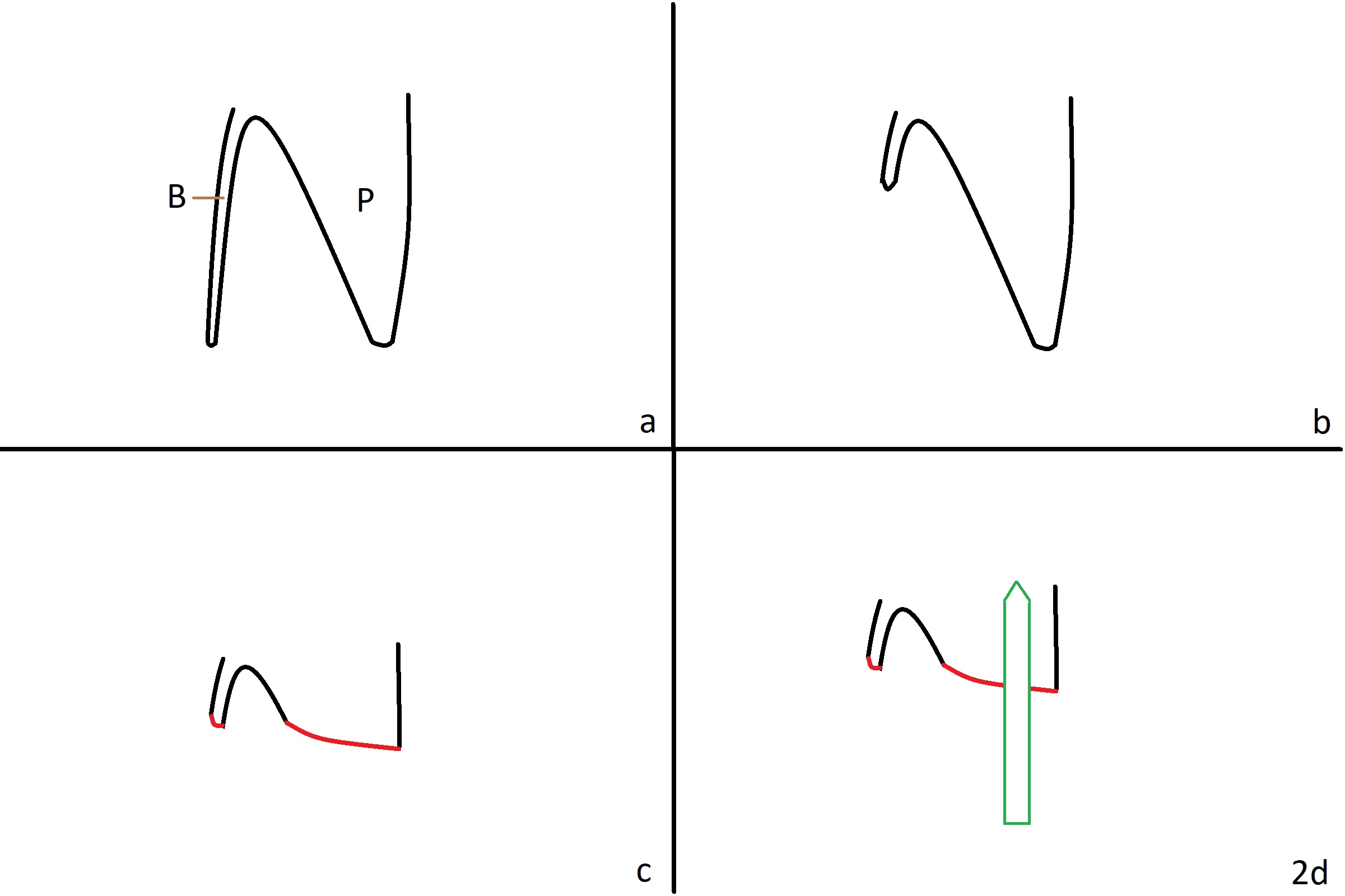
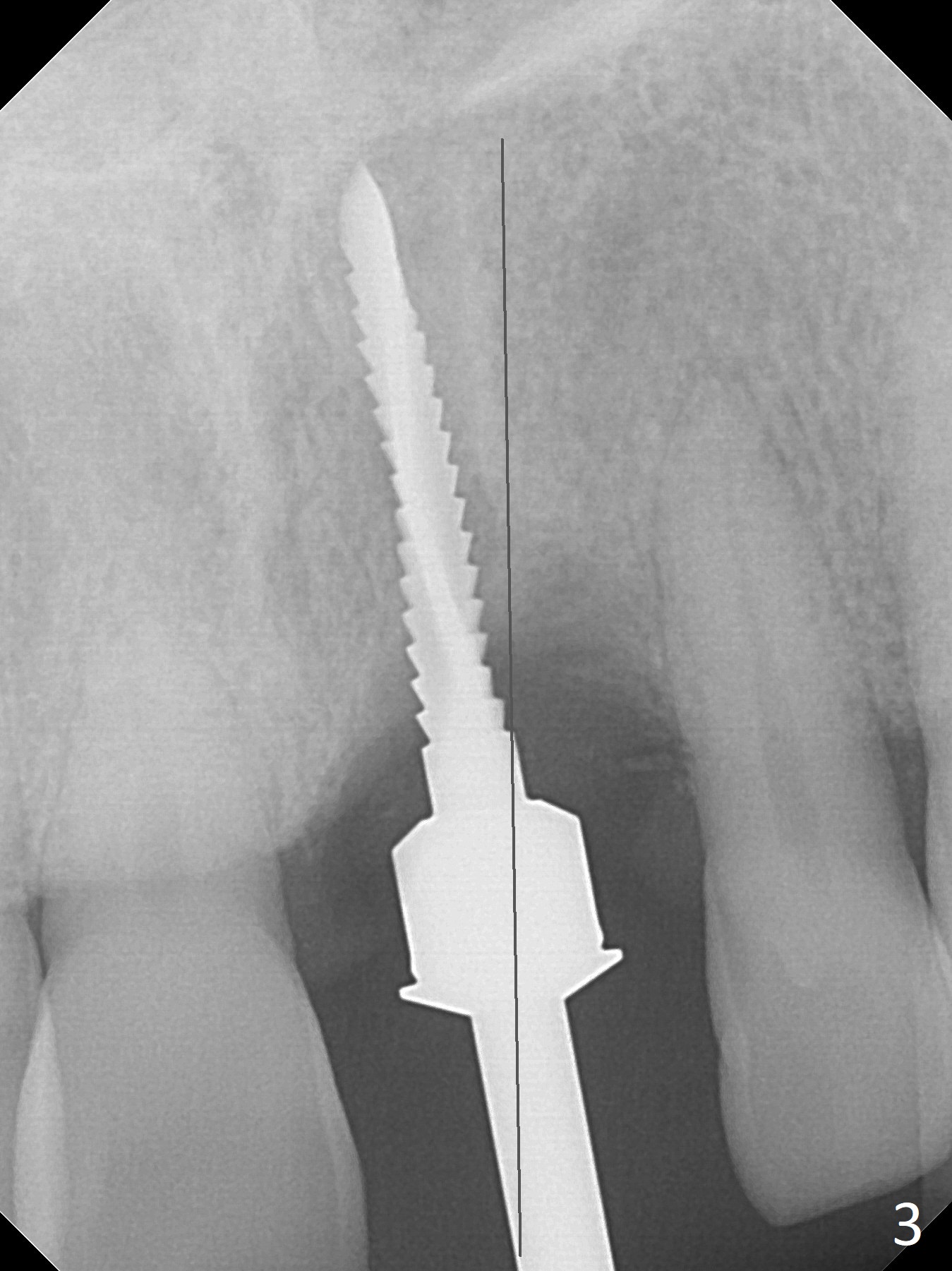
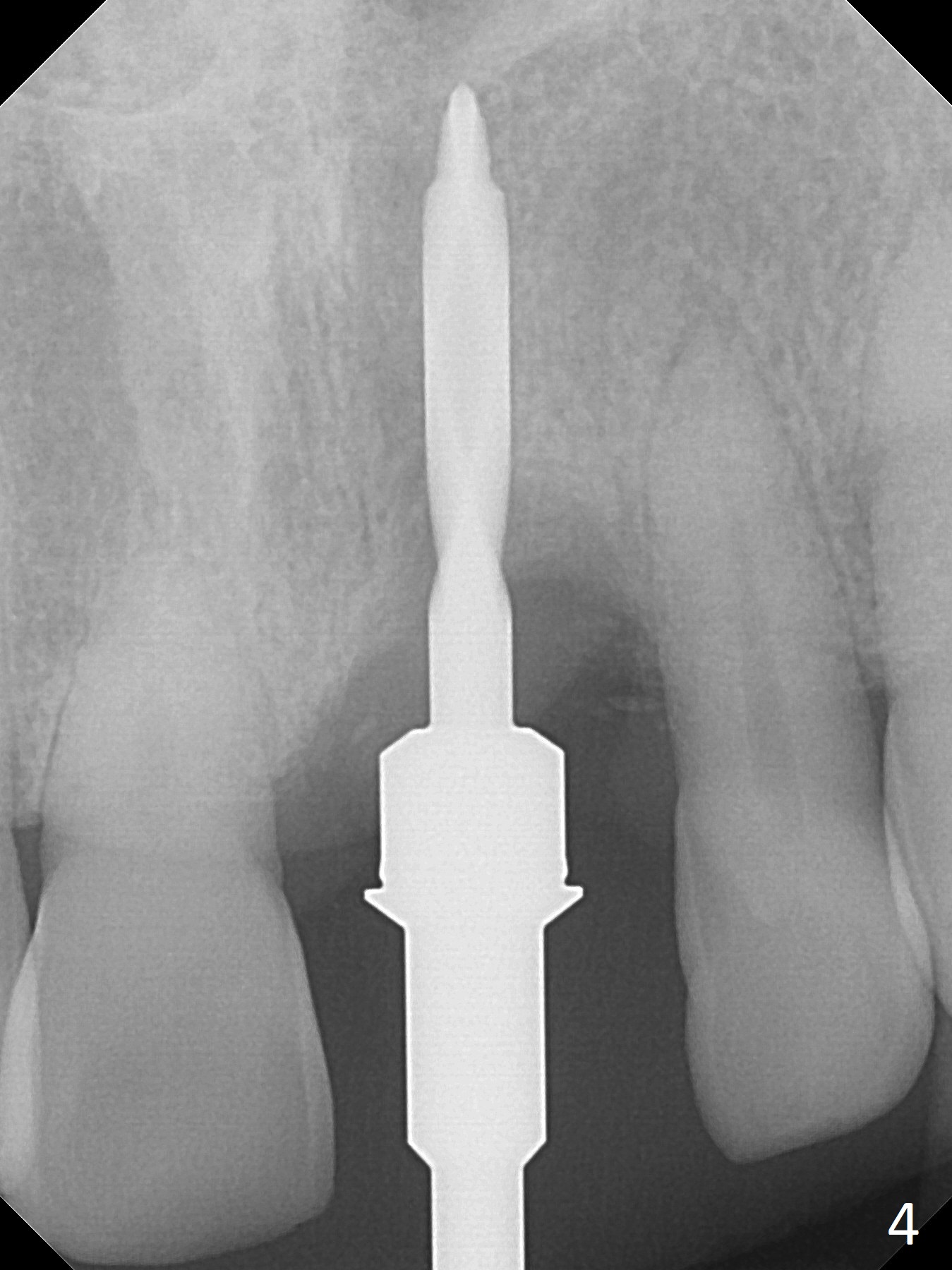
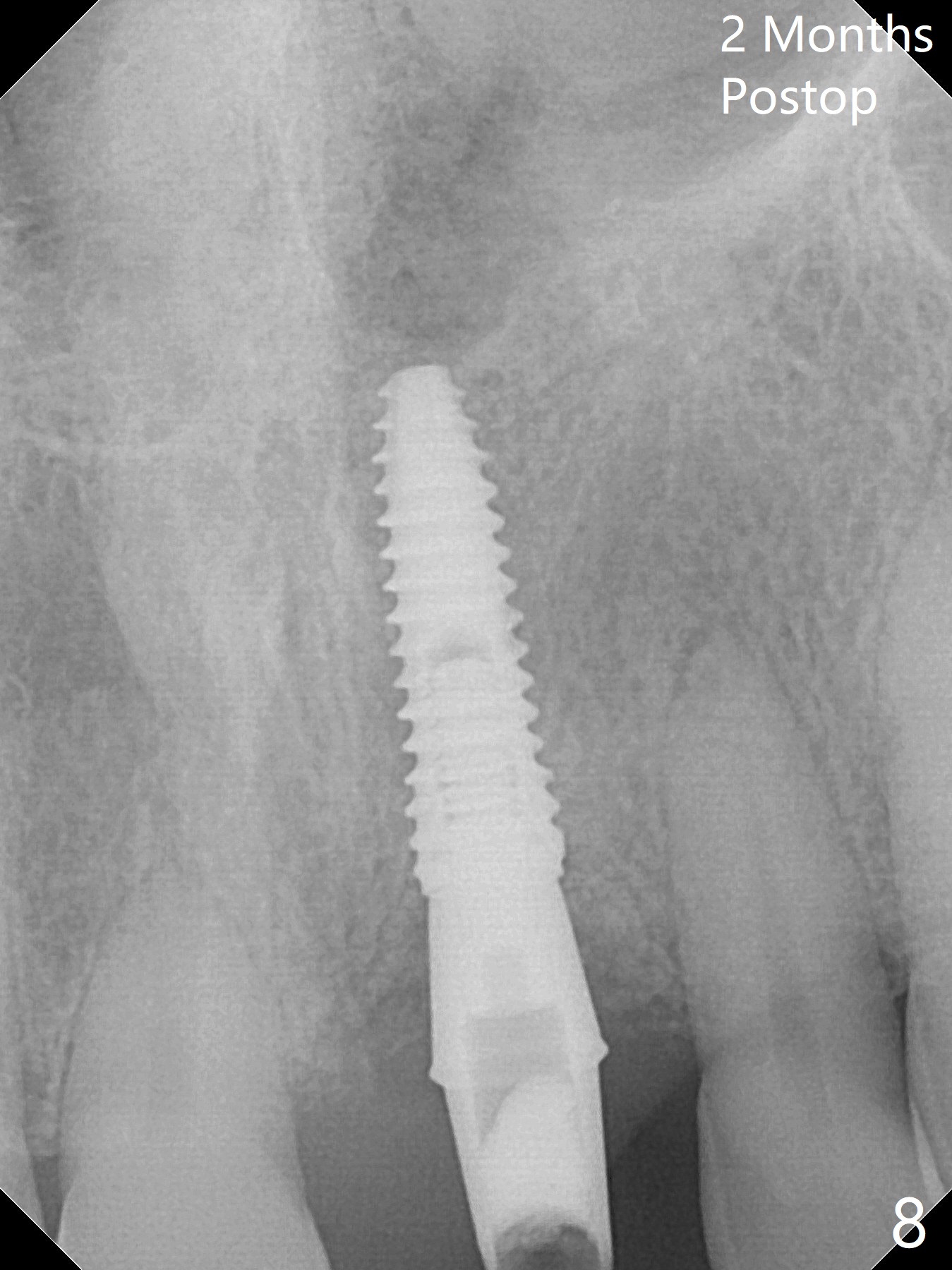
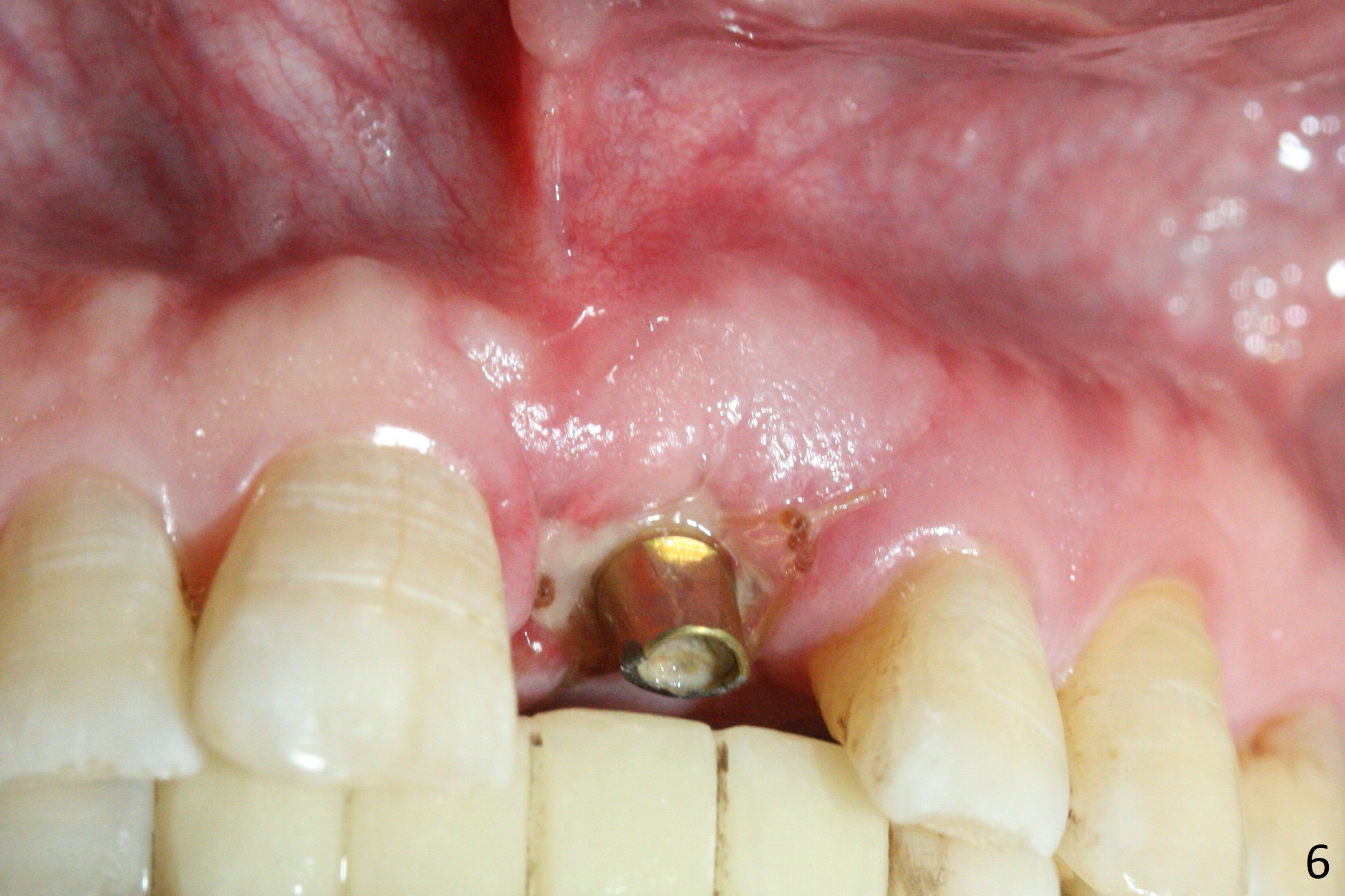
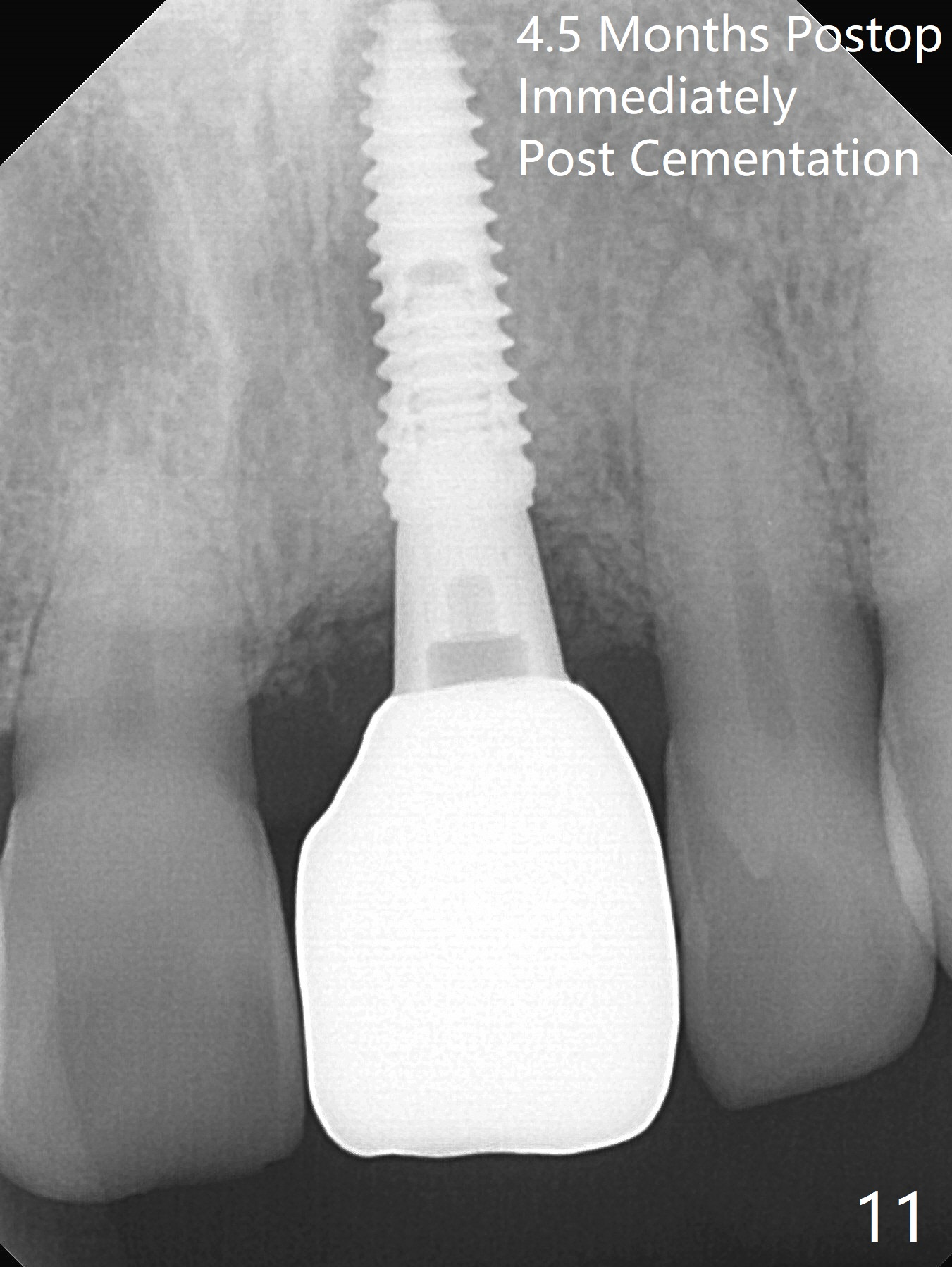
Preop examination shows mobility I of the teeth #8 and 10 and apparent occlusal trauma from #22-26 implant bridge. After occlusal equilibrium, incision reveals low, but moderate ridge at #9 (Fig.1). Fig.2a is a cross section of a normal upper incisor socket with thin buccal plate (B) and thick palatal one (P). It is difficult to initiate osteotomy in the oblique palatal wall when the buccal plate is resorbed (Fig.2b). In this case with horizontal buccal and palatal plate bone loss, the socket bottom is flat (Fig.2c), easy for osteotomy (Fig.2d green arrow, Fig.3). The initial osteotomy deviates mesial (Fig.3). To avoid perforation into the Incisive Canal, the trajectory is changed (Fig.4). After use of the final drill (3 mm), the coronal Incisive Canal is perforated. Following placement of a 3.5x13 mm implant and 4.5x5.5(4) mm abutment, Vanilla Graft is placed (Fig.5 *) to repair the perforation. Retrospectively, the coronal end of the Incisive Canal is revealed at incision (Fig.1 *). The initial osteotomy should be slightly more distal (Fig.3 black line). The buccal plate looks bulky due to placement of the abutment and bone graft 1 week postop (Fig.6,7 (crown dislodgement)). The bone graft appears to remain in place 2 months postop (Fig.8). Impression is taken because of instability of the immediate provisional (Fig.9 after Laser gingivectomy). The gingiva and buccal plate remain healthy 4.5 months postop (Fig.10). A permanent crown is cemented (Fig.11).
Return to Upper Incisor Immediate Implant, Armaments Xin Wei, DDS, PhD, MS 1st edition 12/04/2017, last revision 04/17/2018