



 |
 |
 |
 |
|
 |
 |
 |
||
Routine Immediate Implant is Not so Routine
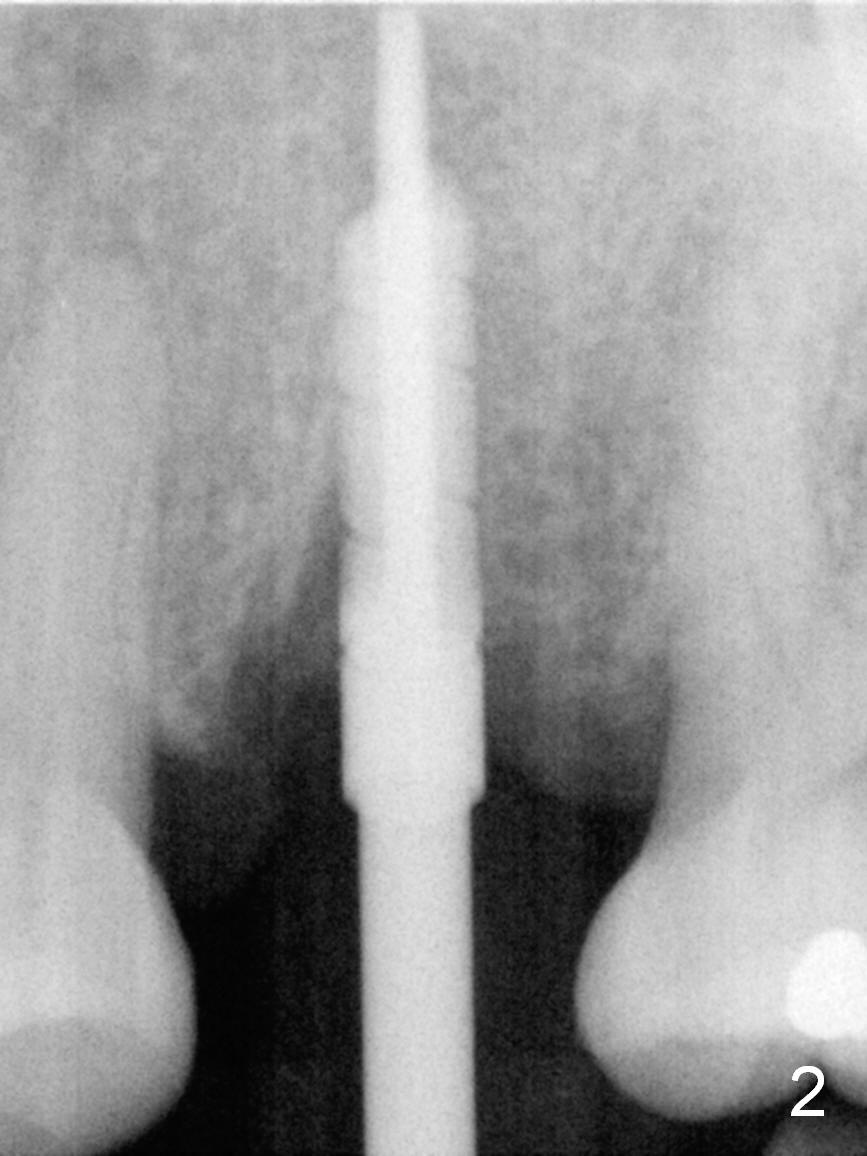
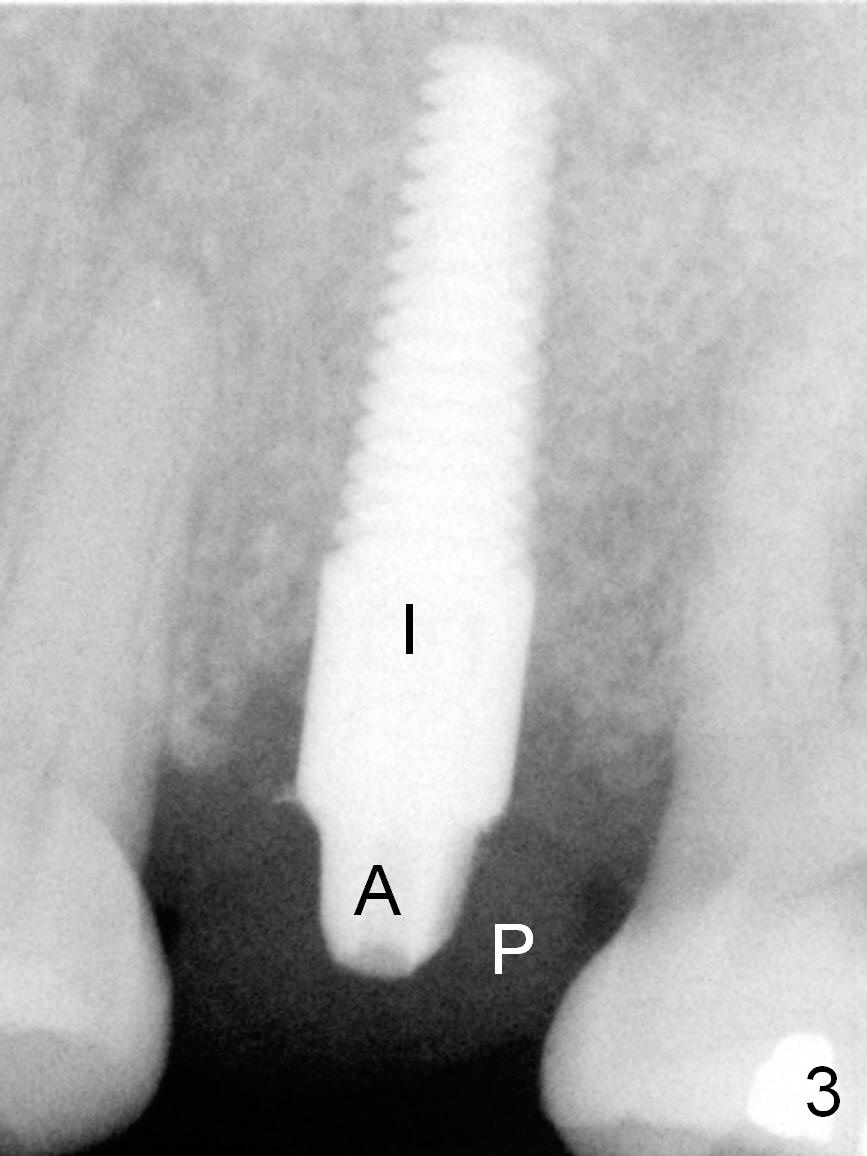
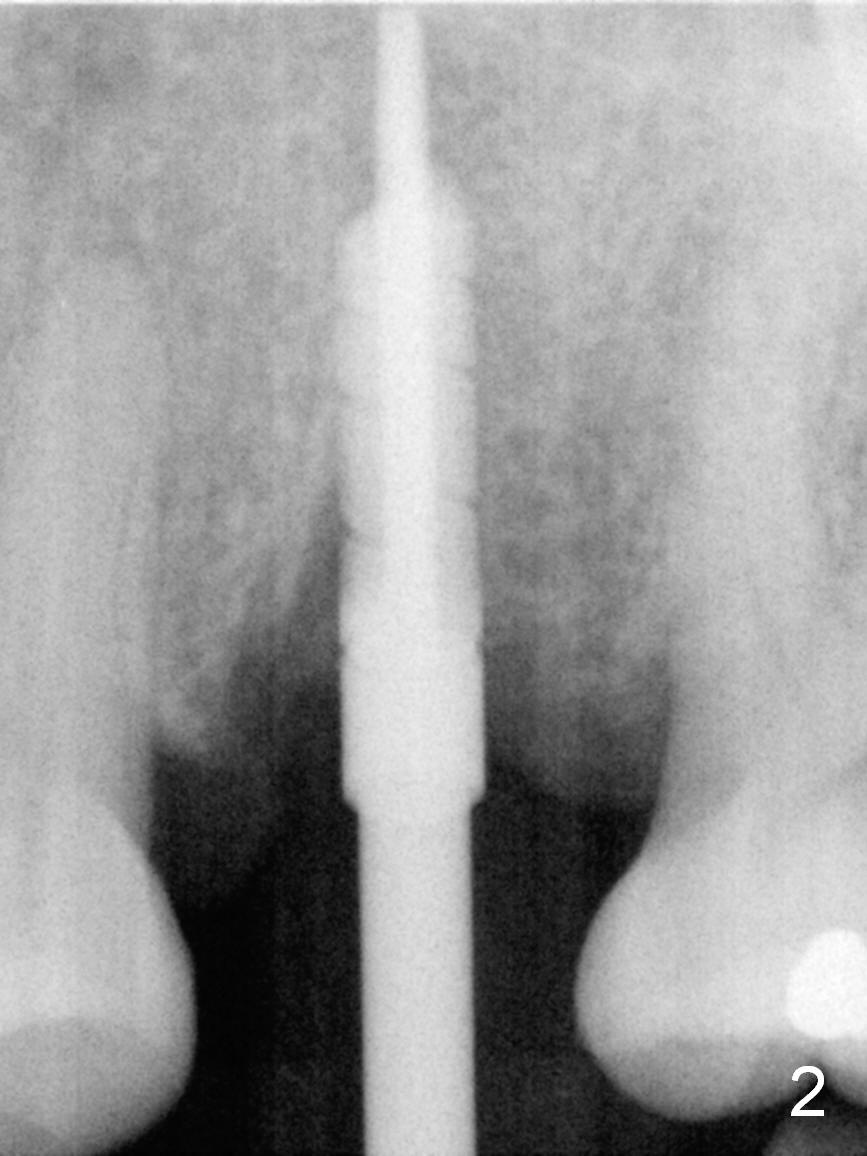
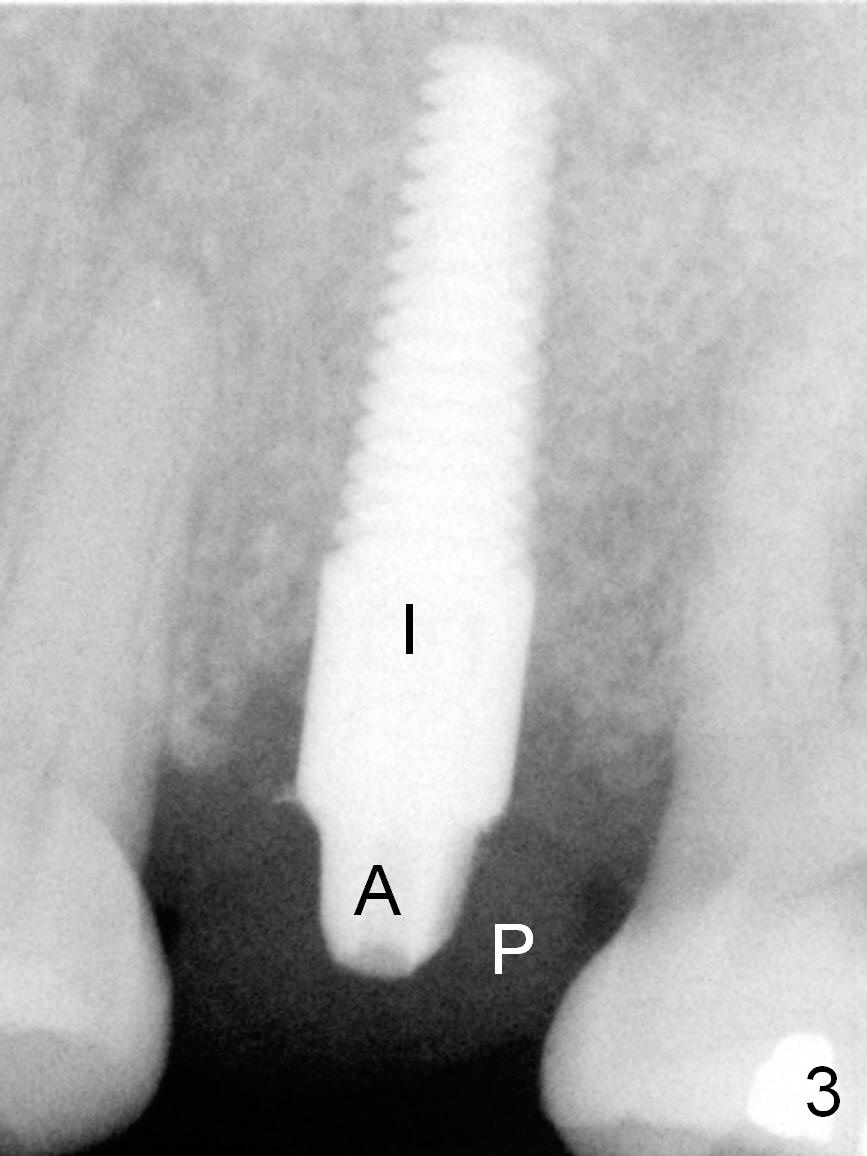
A 53-year-old lady (CM) has a residual root at #13 (Fig.13). Extraction is not so easy. Straight elevators have to be used in addition to proximators (periotomes). The elevators creates small defect in the distobuccal corner when the root is out. The socket is treated with Metronidazole. Osteotomy is initiated in the palatal aspect of the socket. An intraop PA is taken with a 3 mm reamer in place to confirm that the osteotomy does not violate the roots of the neighboring teeth (Fig.2). The 2nd challenge is buccal deviation of a 4.5x17 mm implant while it is being placed. The implant has to be backed up before re-adjusting its trajectory (Fig.3 I). There is buccal gap when the implant is finally seated. Primary stability is acceptable. A 3.5x3 mm abutment (A) is placed for an immediate provisional (P).
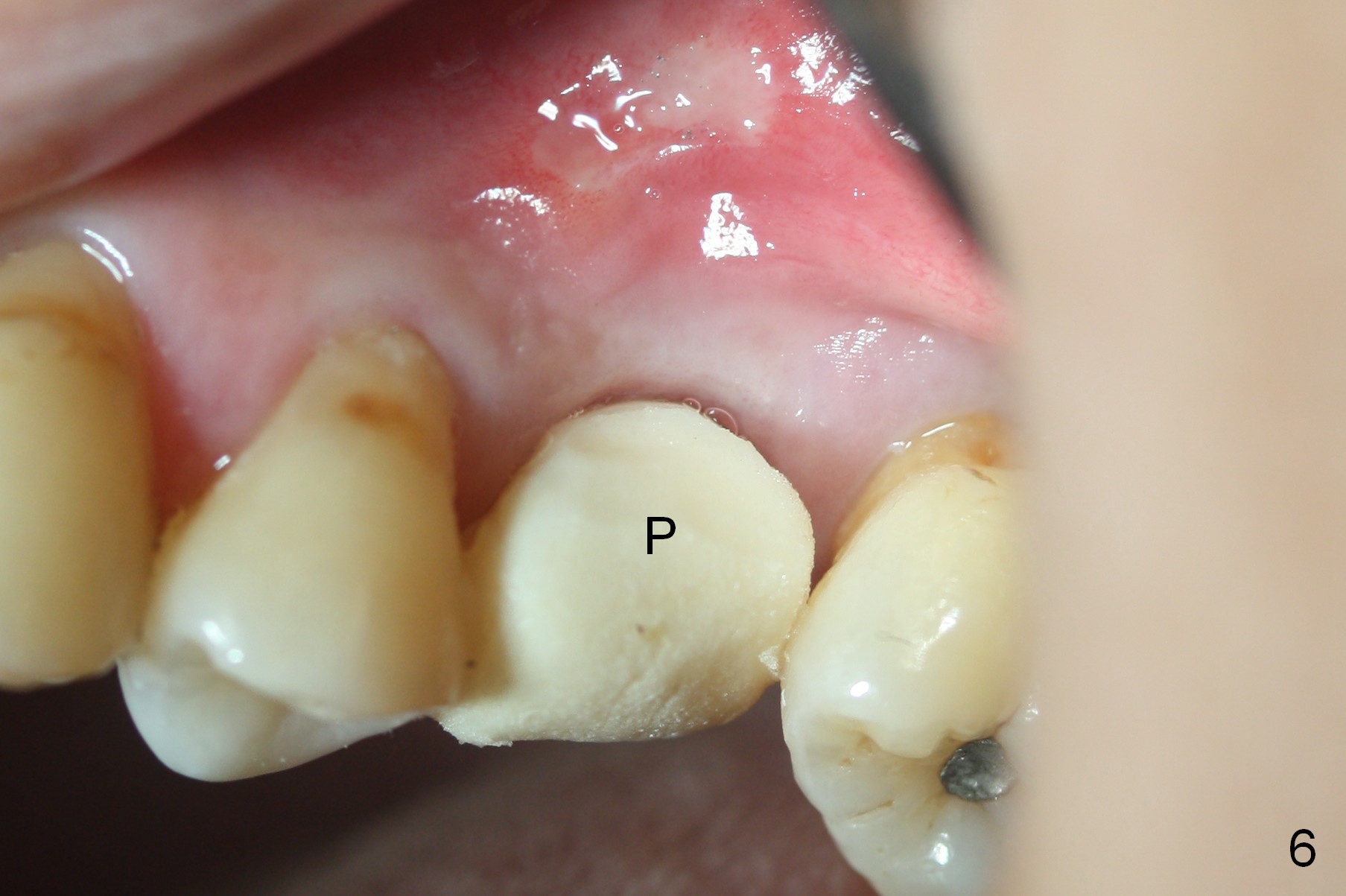
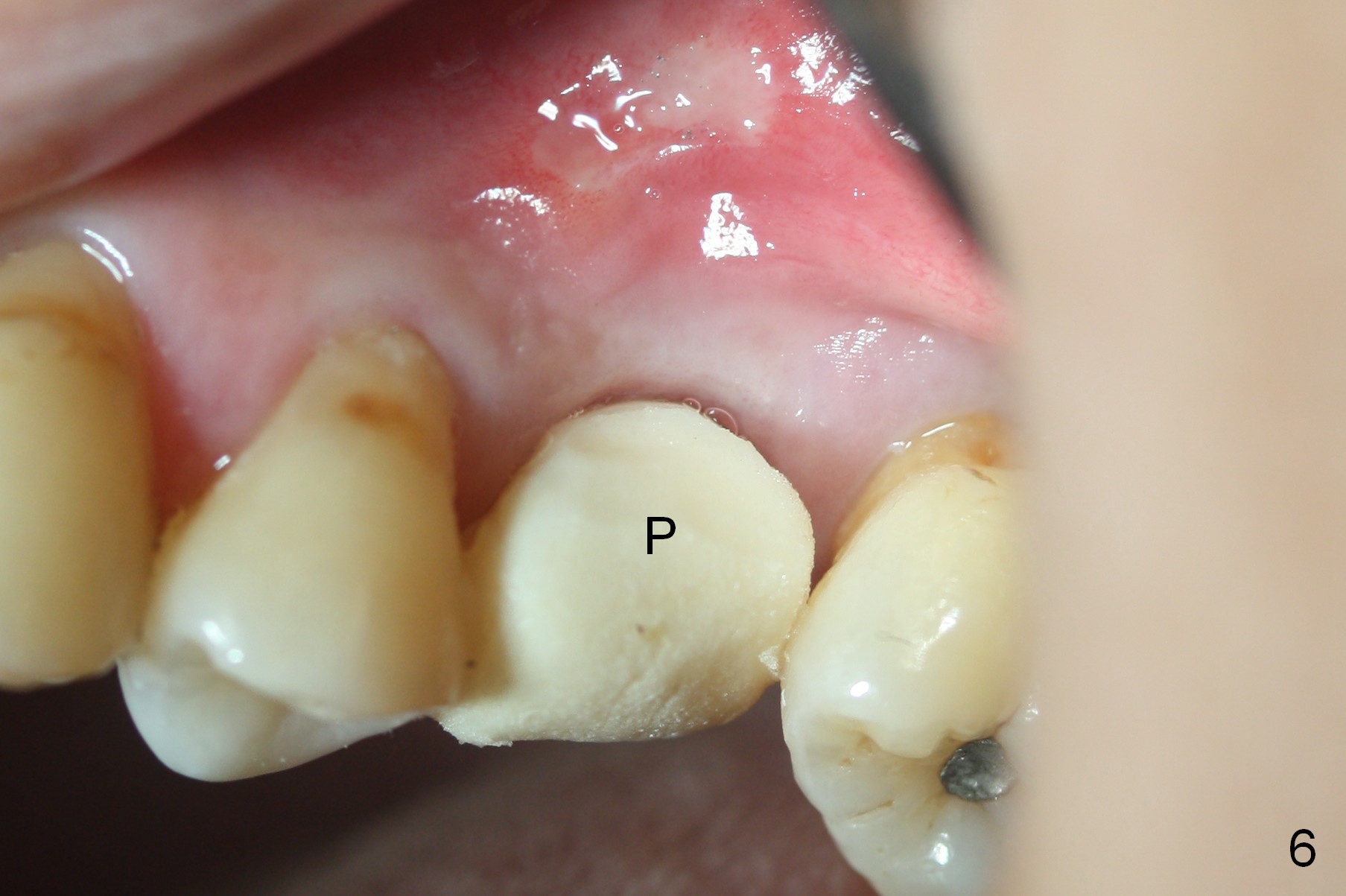
The bone around the implant undergoes normal change 3.5 months postop (Fig.4). After reprep, the buccal margin is slighly subgingival (Fig.5), whereas the palatal one supragingival (not shown). After reline, the immediate provisional (Fig.6 P) is temporarily recemented. The provisional looks wide mesiodistally, which is re-confirmed by the model (Fig.7). It appears that the wider edentulous space is due to premature loss of the 1st molar and incomplete mesial shift of the 2nd molar. In fact a wider implant should have been placed. CT is taken 7 months post cementation.
Return to Upper Premolar Immediate Implant,
Technicians
Xin Wei, DDS, PhD, MS 1st edition 11/03/2015, last revision 01/19/2018