


 |
 |
 |
 |
 |
 |
 |
 |
 |
 |
Remove a Diseased Tooth, a New World Will be Born by Itself
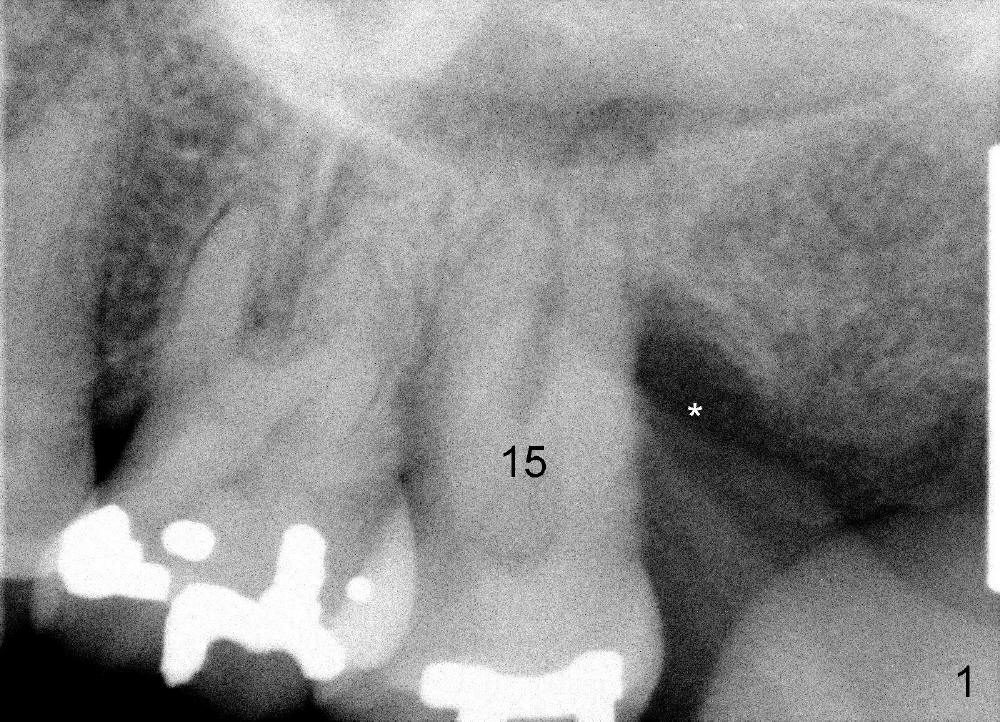
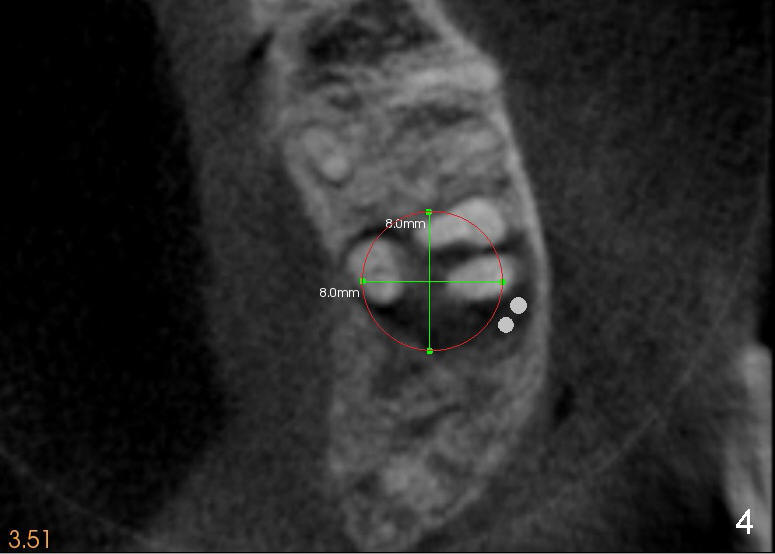
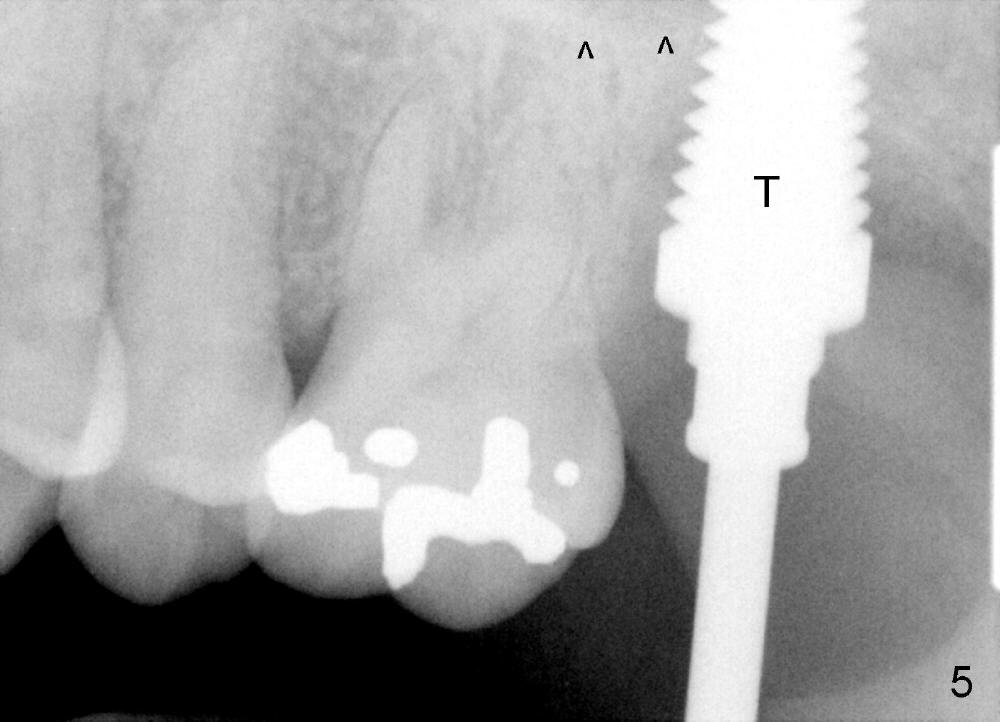
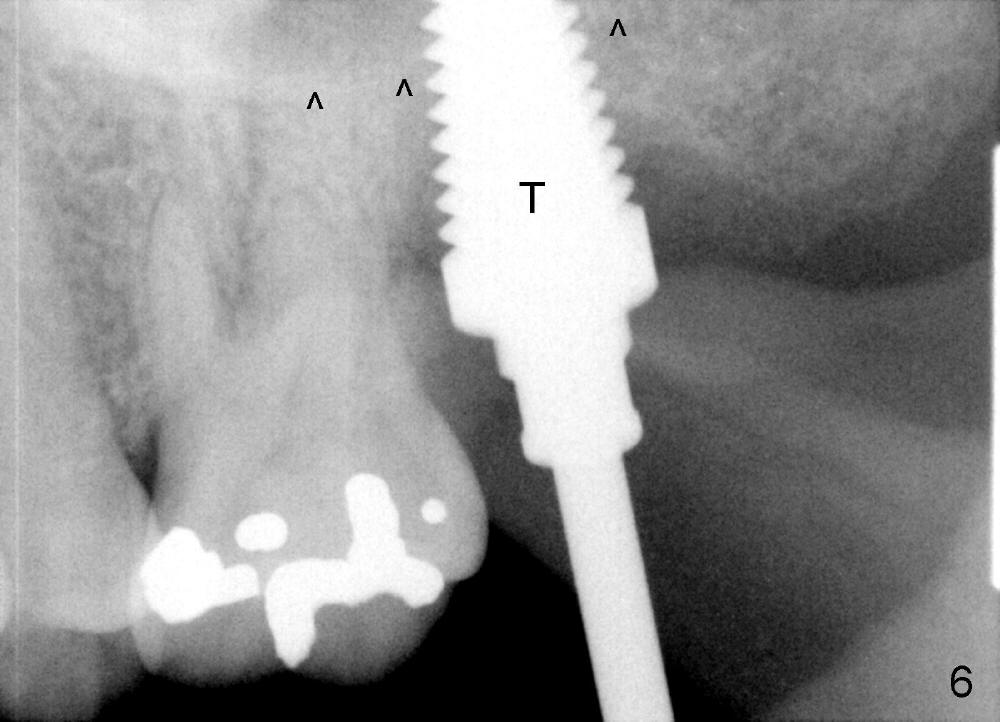
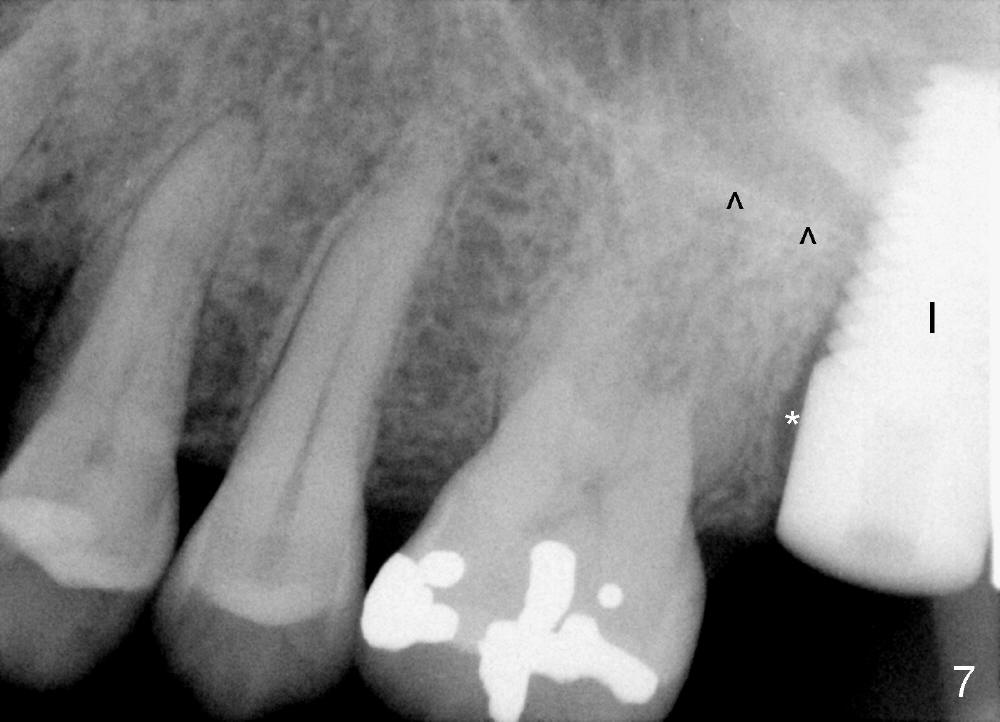
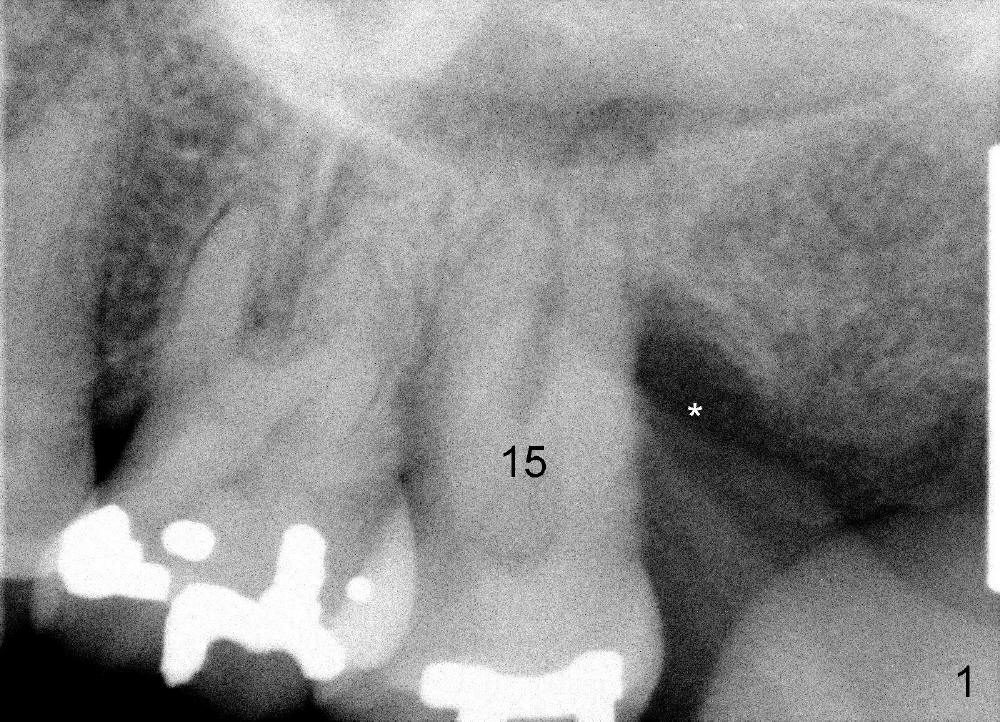
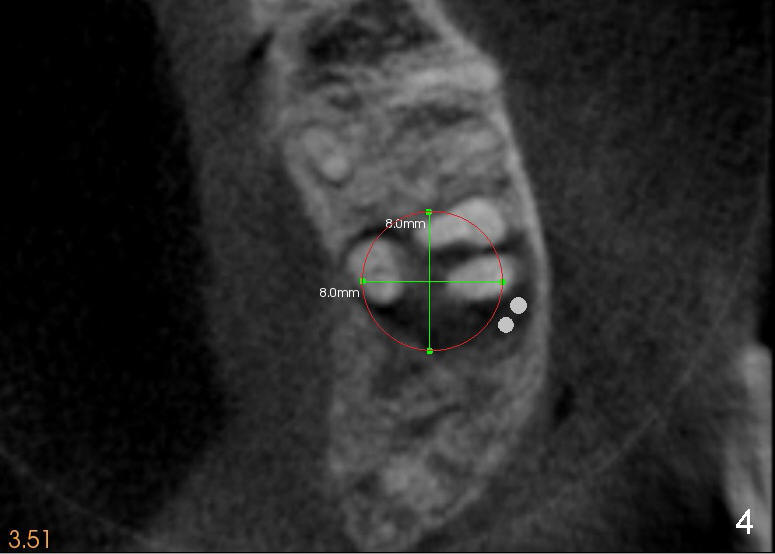
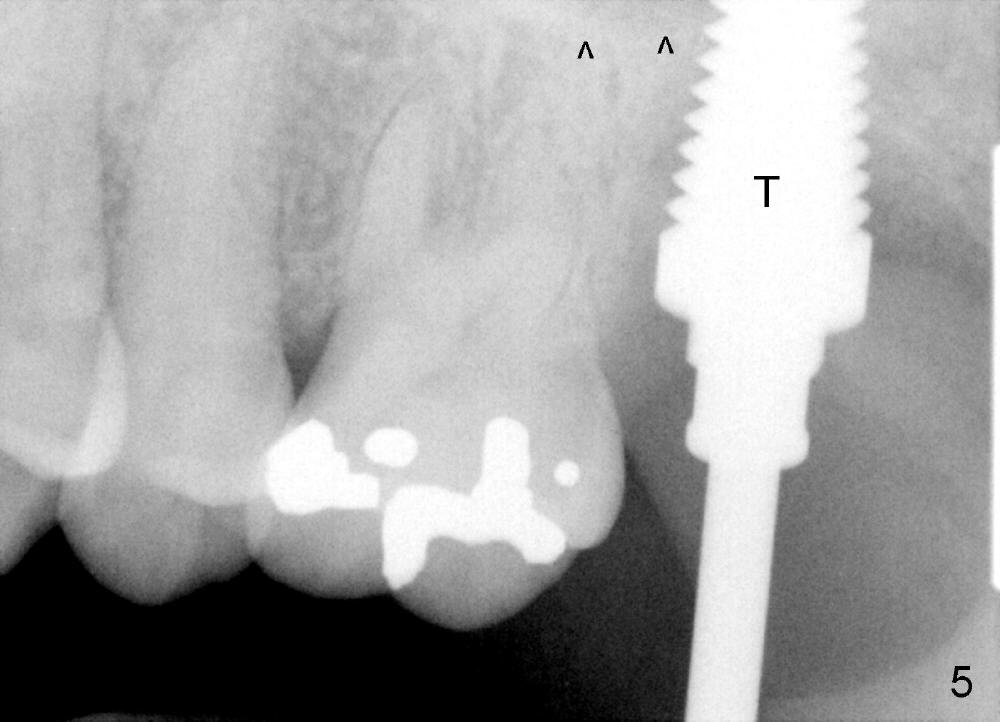
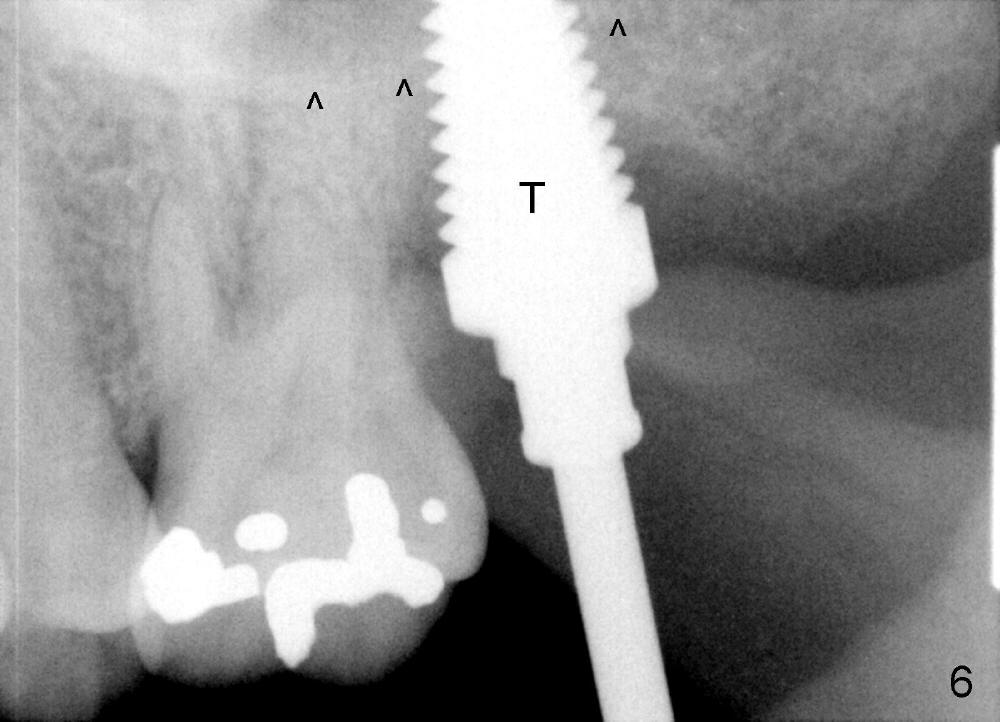
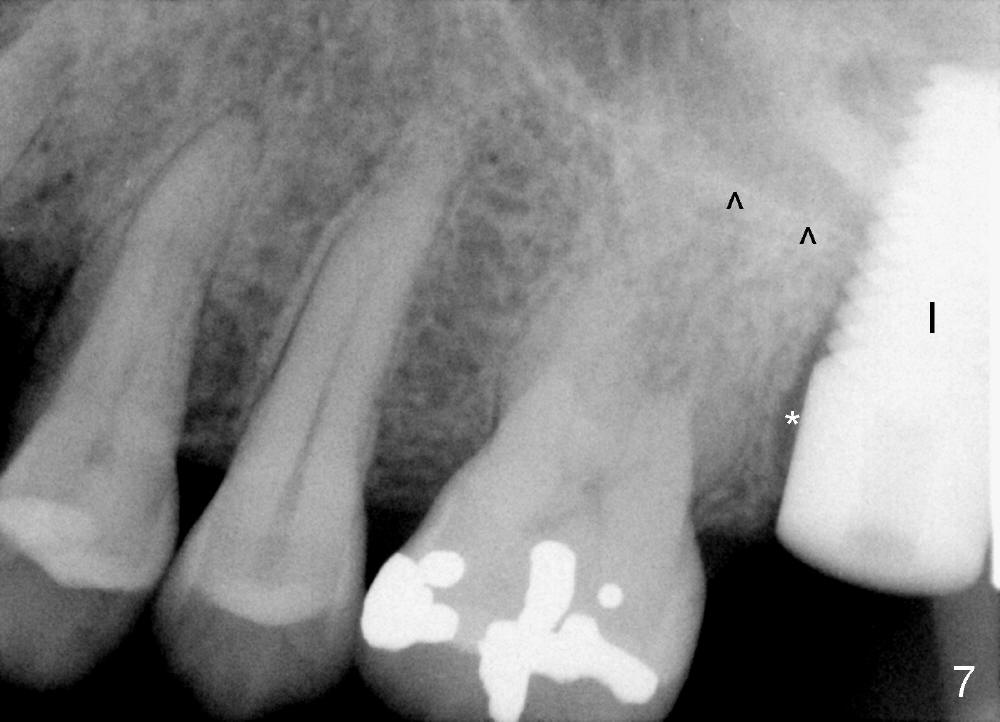
A 47-year-old lady has repeated history of swelling and pain associated with the upper 2nd molars. The left one is more severely affected (Fig.1) and is to be treated first. CBCT is taken to confirm its nonsalvageability. Sagittal (Fig.2), coronal (Fig.3) and axial (Fig.4) sections show that a 8x17 mm tapered implant is appropriate for the defect, supplemented by bone graft (Fig.2,4 grey circles). The periodontally affected tooth is extracted. The osteotomy forms by round tapered osteotomes 2-5 mm at the depth of 17 mm, followed by a series of tapered taps 4.5-7 mm at the same depth. Two PAs are taken to confirm that the sinus floor (Fig.5,6: ^) has been penetrated by a 7x17 mm tap (T). The tap has engaged into the site tightly. The same sized implant is inserted with torque of 45 Ncm (Fig.7). Osteogen is placed as planned. The patient is pain free; the wound is healing 8 days postop (Fig.8).
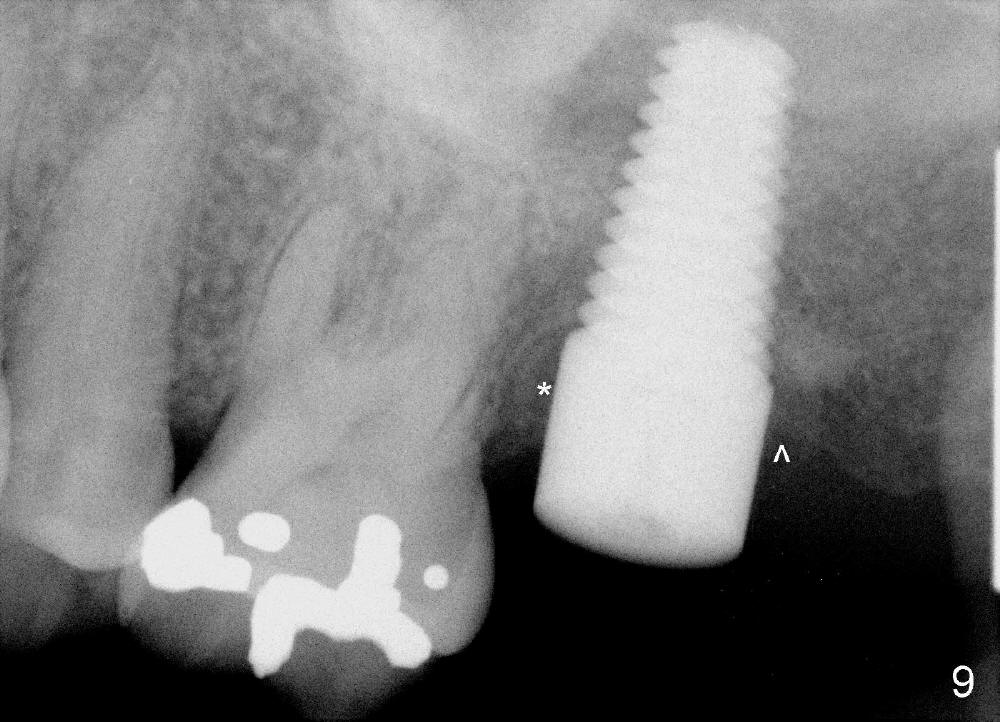
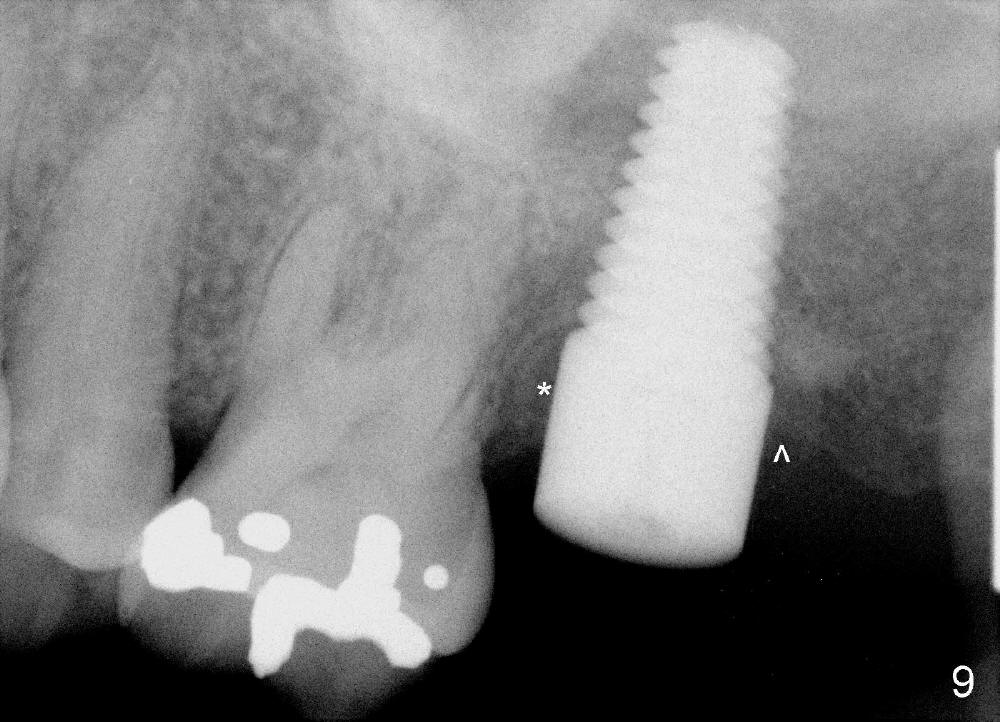
Four months postop, the mesial space and the distal defect have been repaired (Fig.9, as compared to Fig.1 and 7). With removal of a lesion, the implant osteointegrates while the bone regenerates. The new world is going to be built.
The patient is supposed to return for restoration for the upper left 2nd molar, but she experiences pain in the upper right 2nd molar and wants extraction and immediate implant instead. We are going to help her break down the old world and build a new world again.
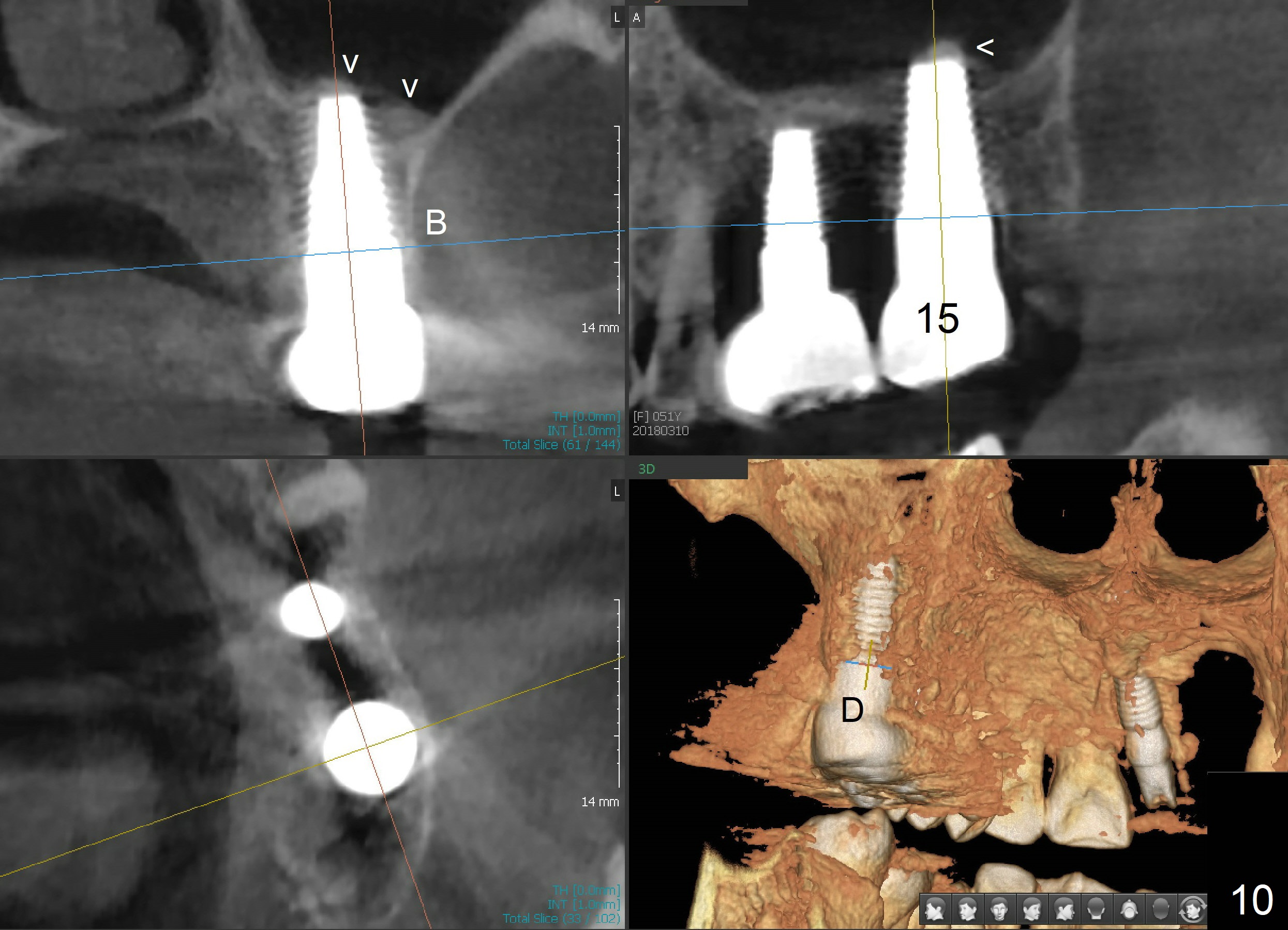
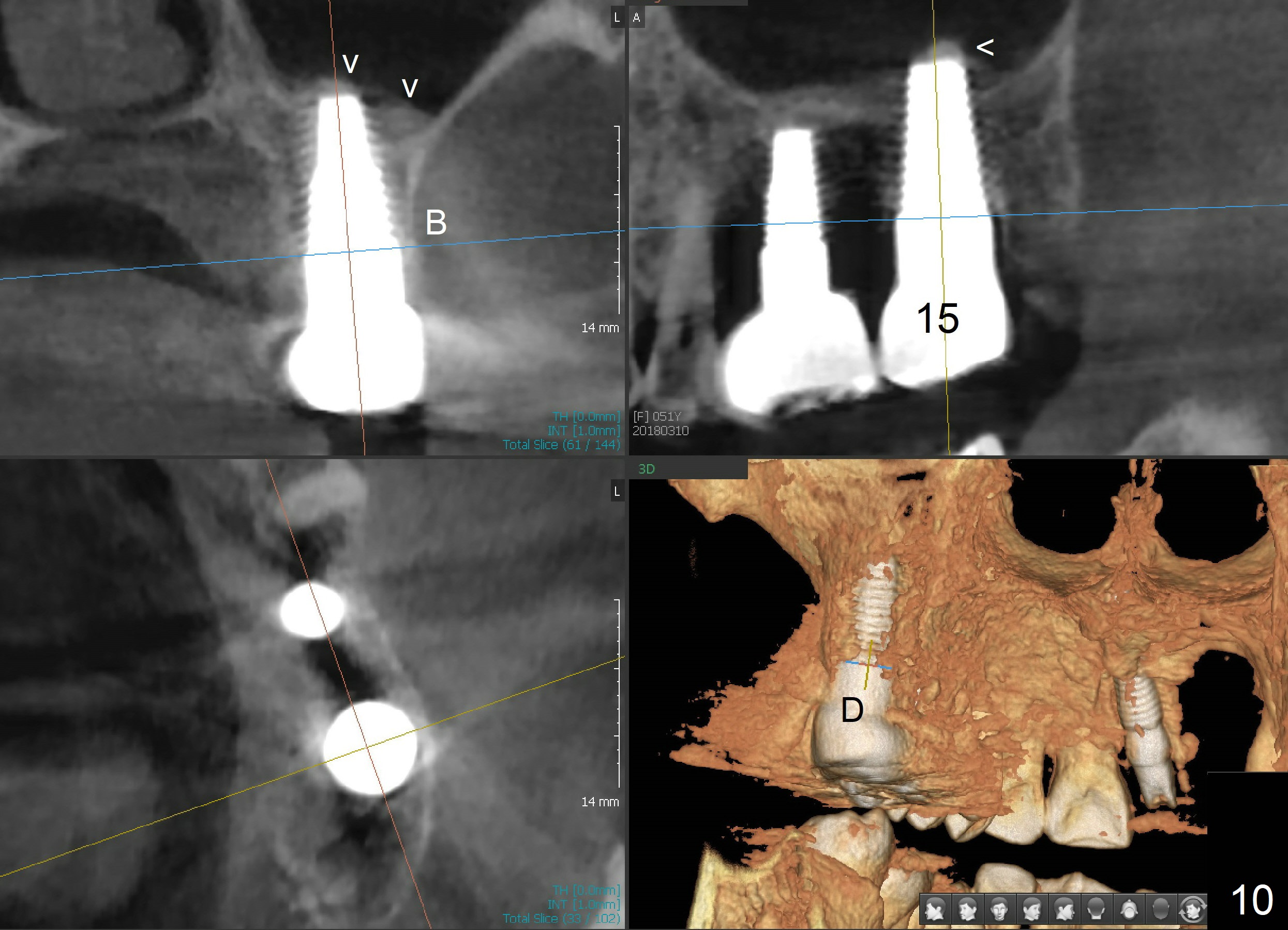
When the crown at the site of #2 is just cemented, there is an abscess associated with the tooth #14. To save money, the patient does not get treatment as quickly as possible. Instead, she waits for insurance to pay for the treatment. In addition, she appears to be a bruxer. There is no bone resorption 3 years post cementation; CBCT shows central implant placement with sinus lift (Fig.10 arrowheads).
Return to Upper Molar Immediate Implant
#2,6,14
Xin Wei, DDS, PhD, MS 1st edition 04/27/2014, last revision 05/29/2018