





 |
 |
 |
||
 |
 |
 |
 |
|
 |
 |
 |
 |
 |
Periodontal Surgery In stead of Implant
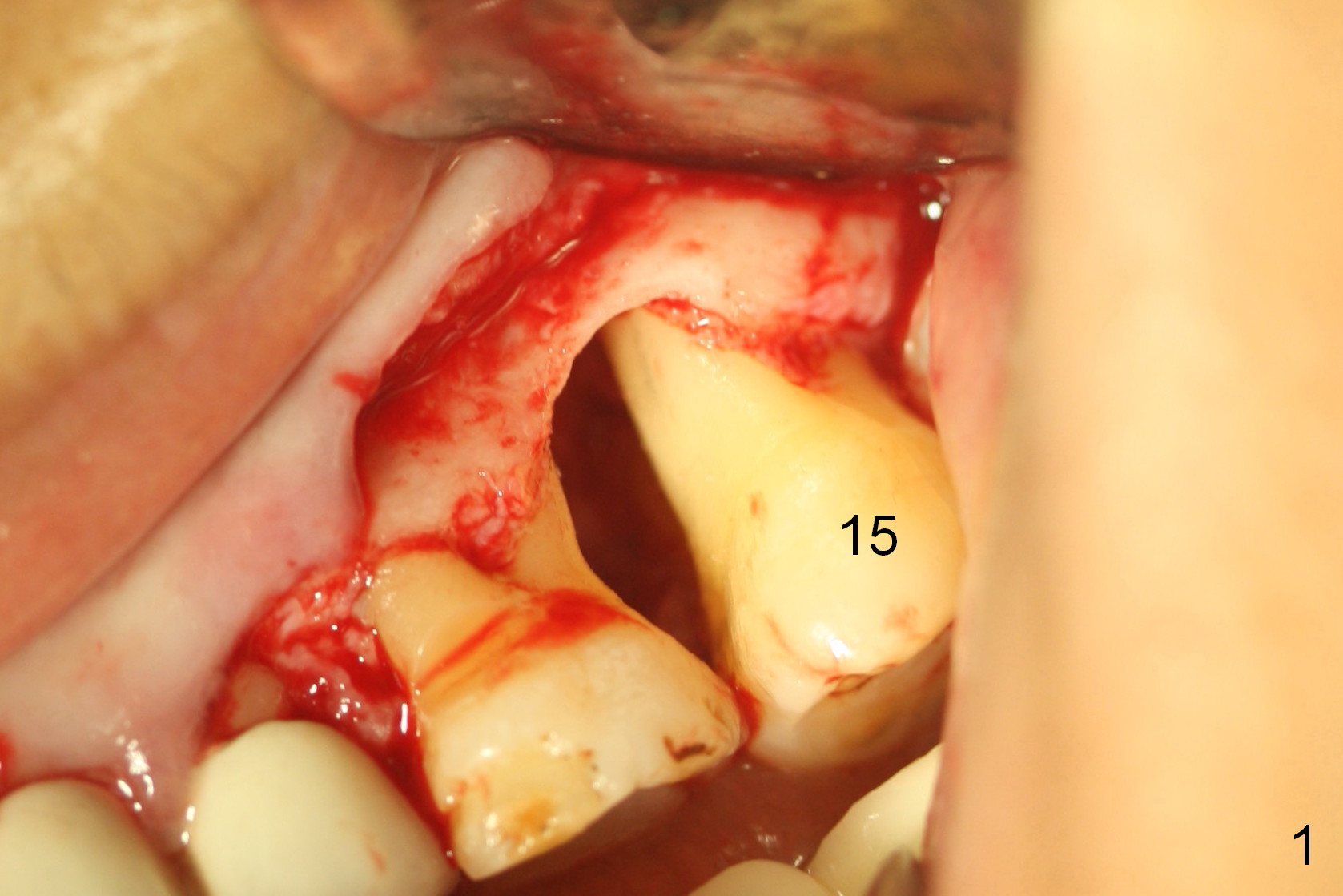
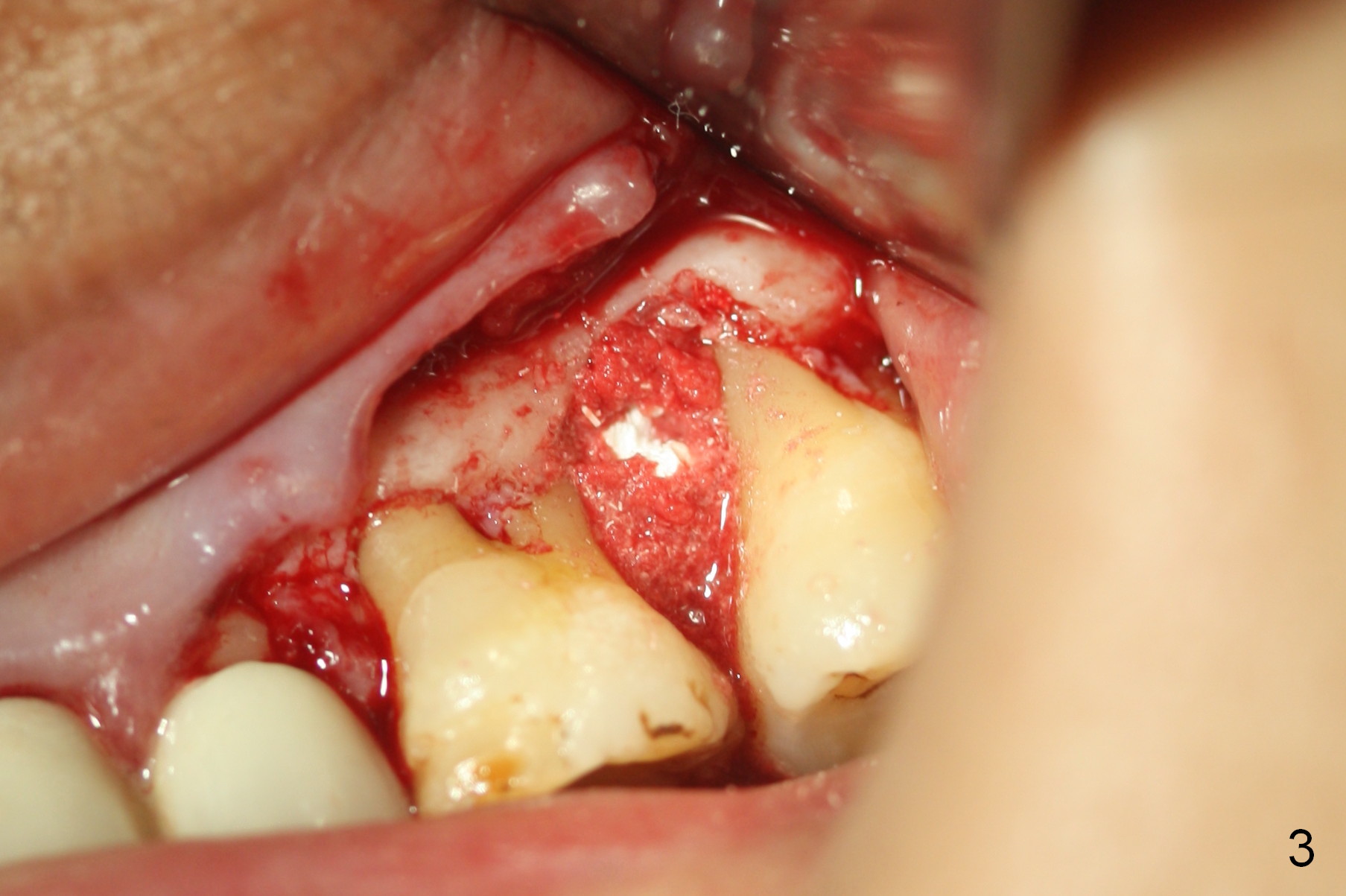
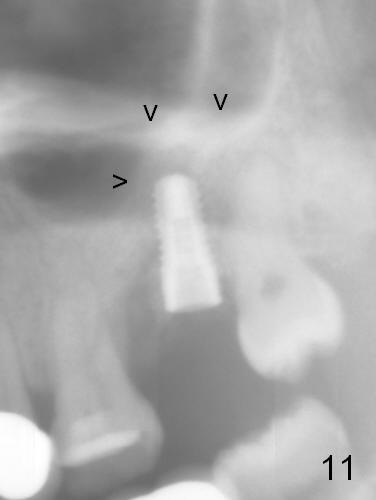
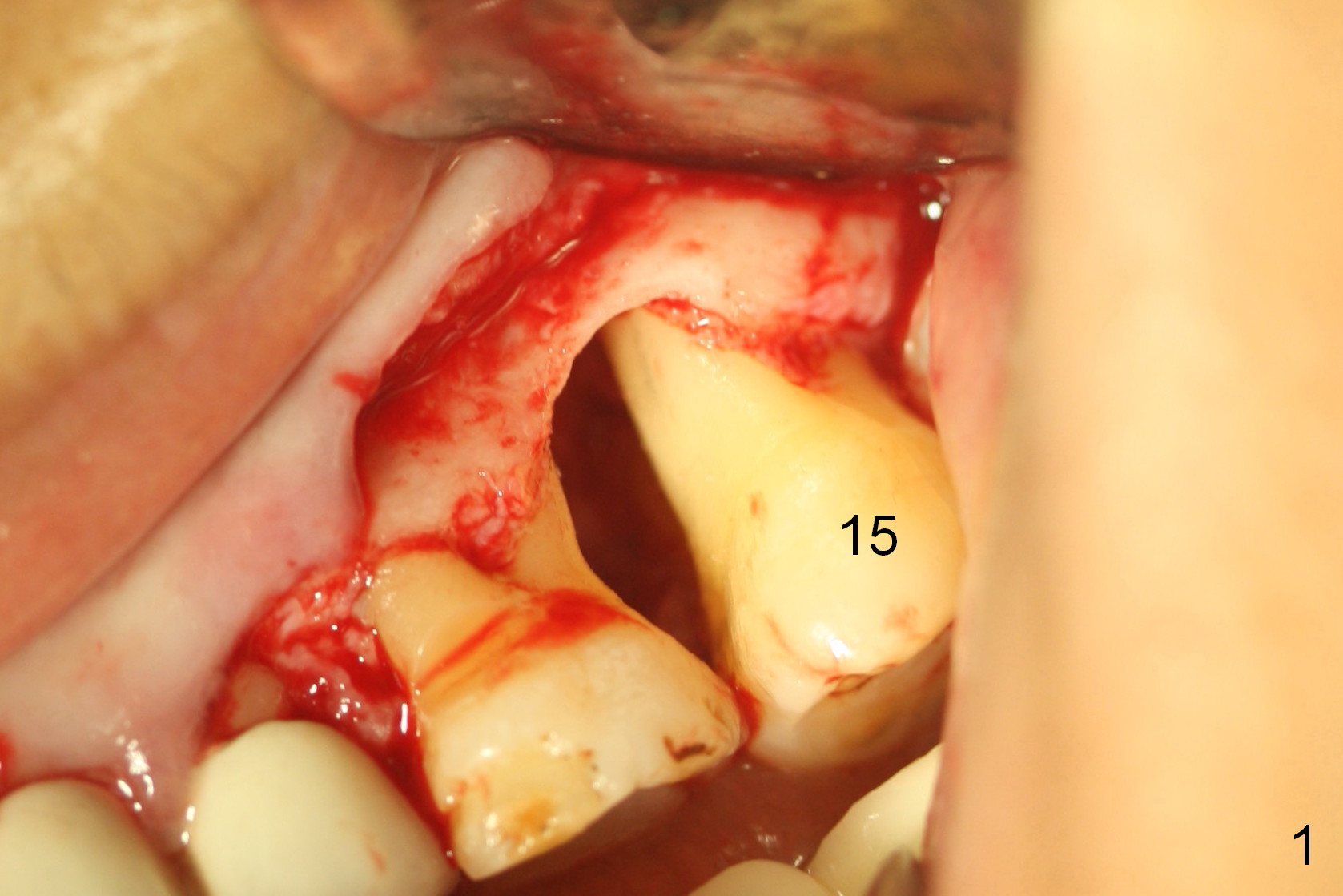
When the patient returns for #15 extraction and immediate implant, she is unwilling to have extraction. The tooth does not bother her, since she does not use it too much now and she can chew on the right side after ortho treatment. Preop examination shows deep pocket confined to the mesiobuccal area. Buccal incision confirms the finding (Fig.1 after debridement). After applying Endogain and filling the defect with mineralized cortical allograft and Osteogen (Fig.2), collagen plug is used to cover the bony defect between the molars (Fig.3). Fig.4 is a postop PA.
Severe cold sensitivity develops 3 months postop, but Endo ice does not elicit the same response. The bony defect appears not repaired (Fig.5,6). There is papillary recession between the adjacent molars (Fig.7).
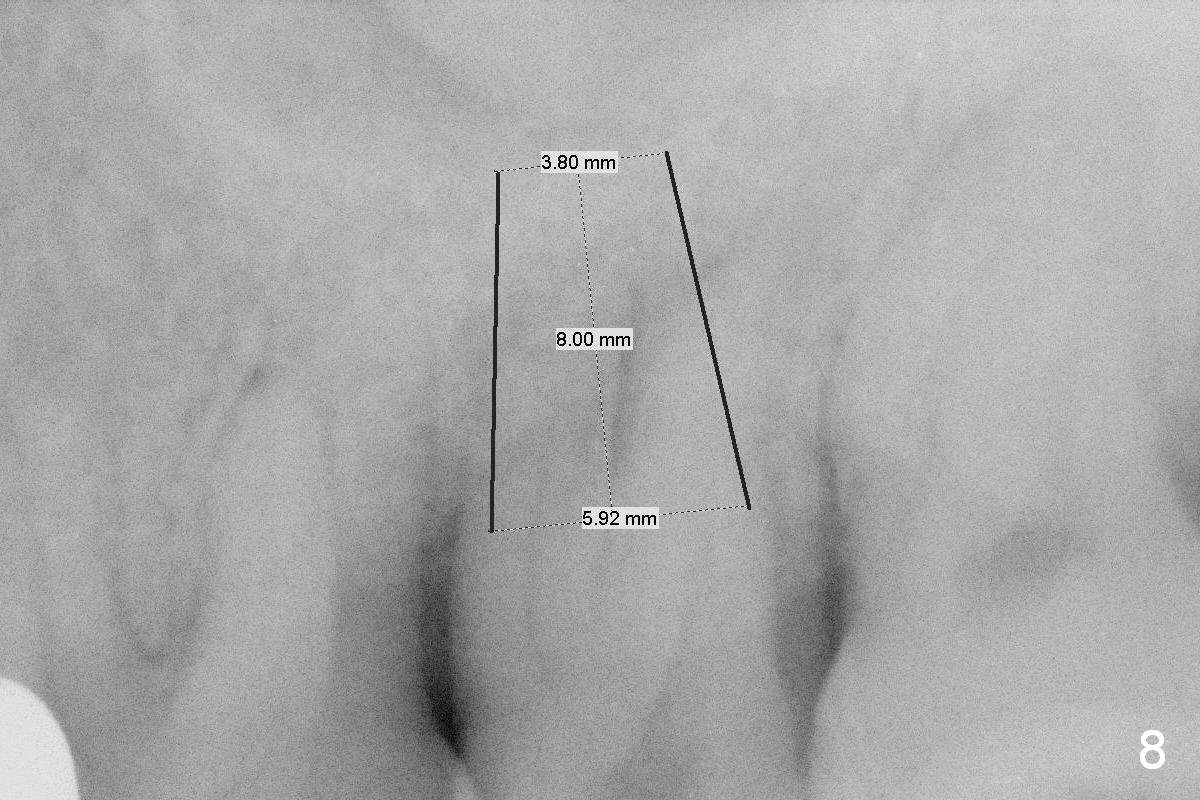
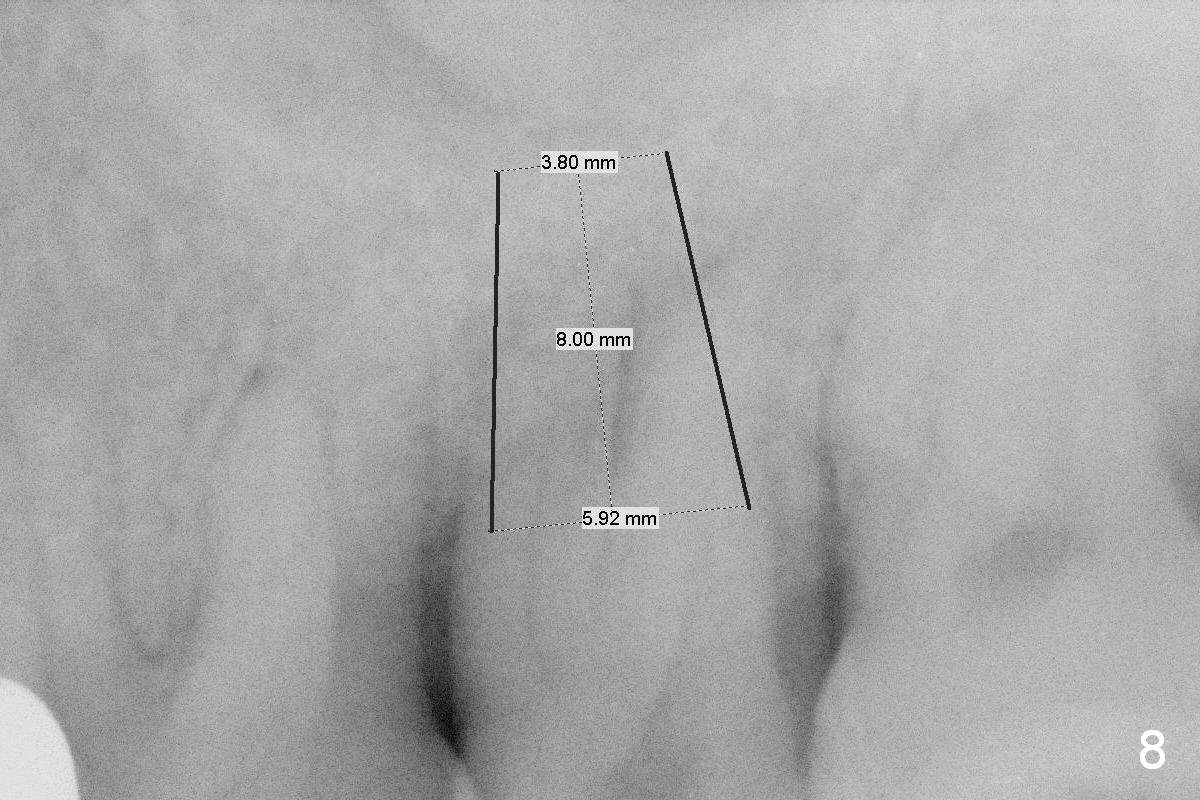
Finally the patient agrees with extraction and implant (Fig.8).
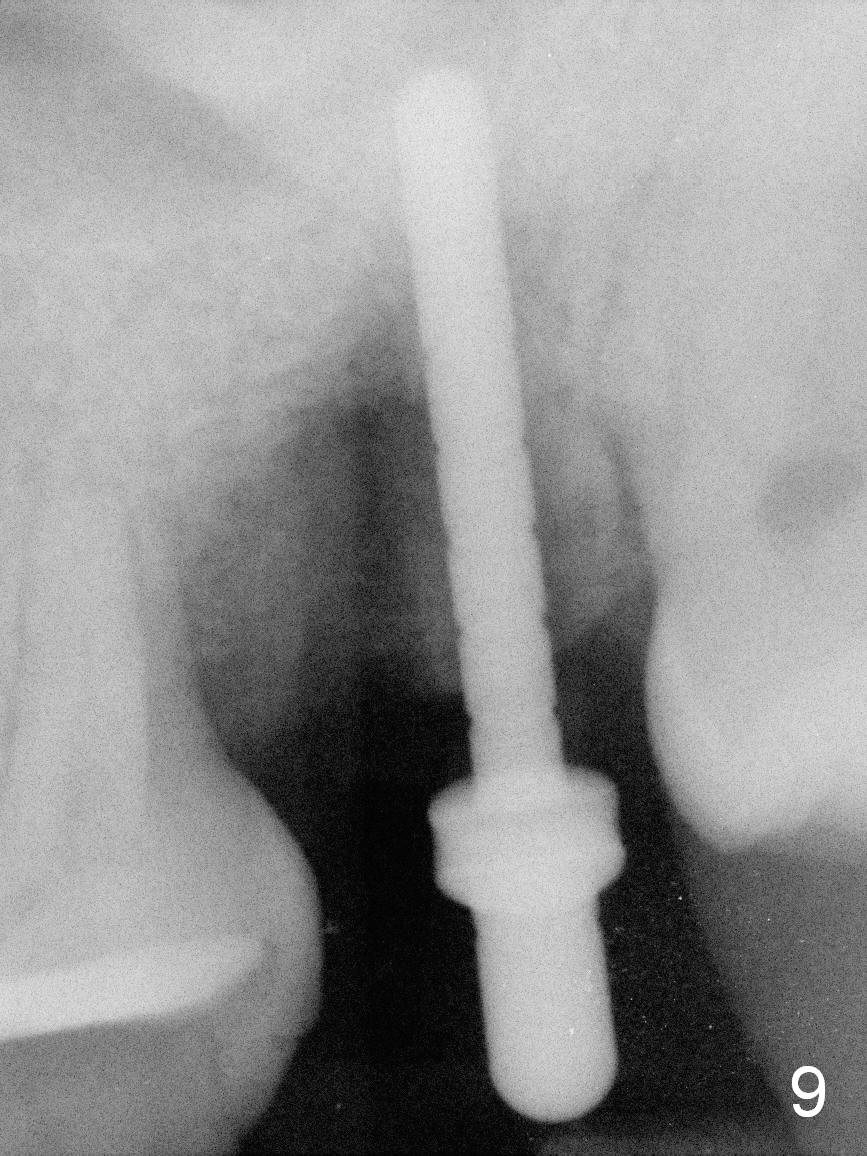
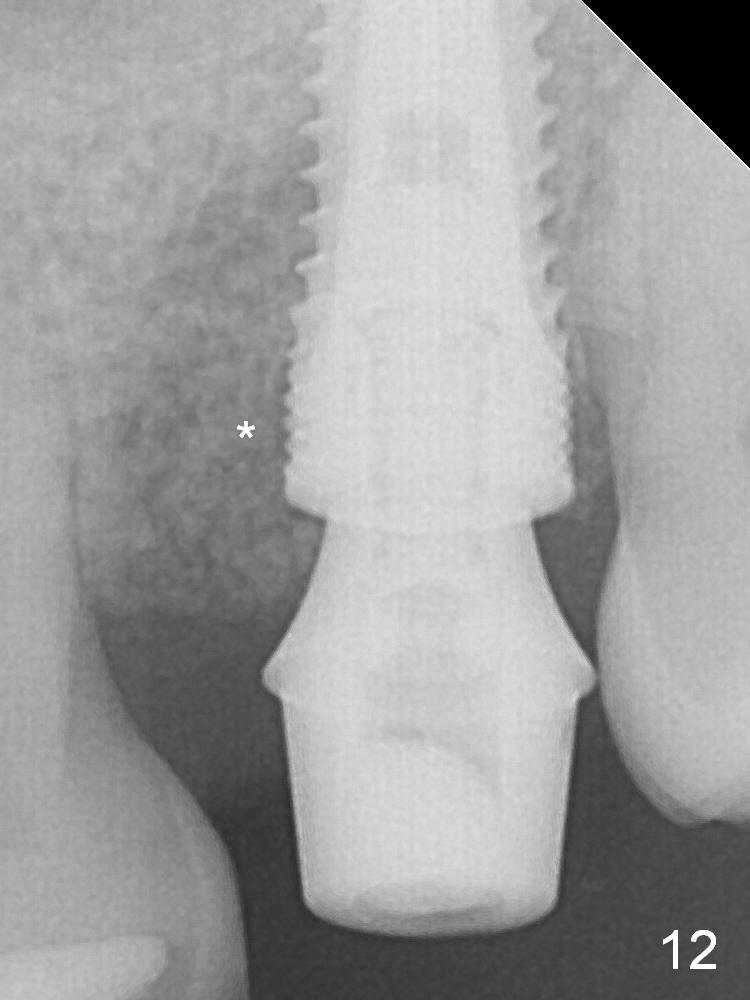
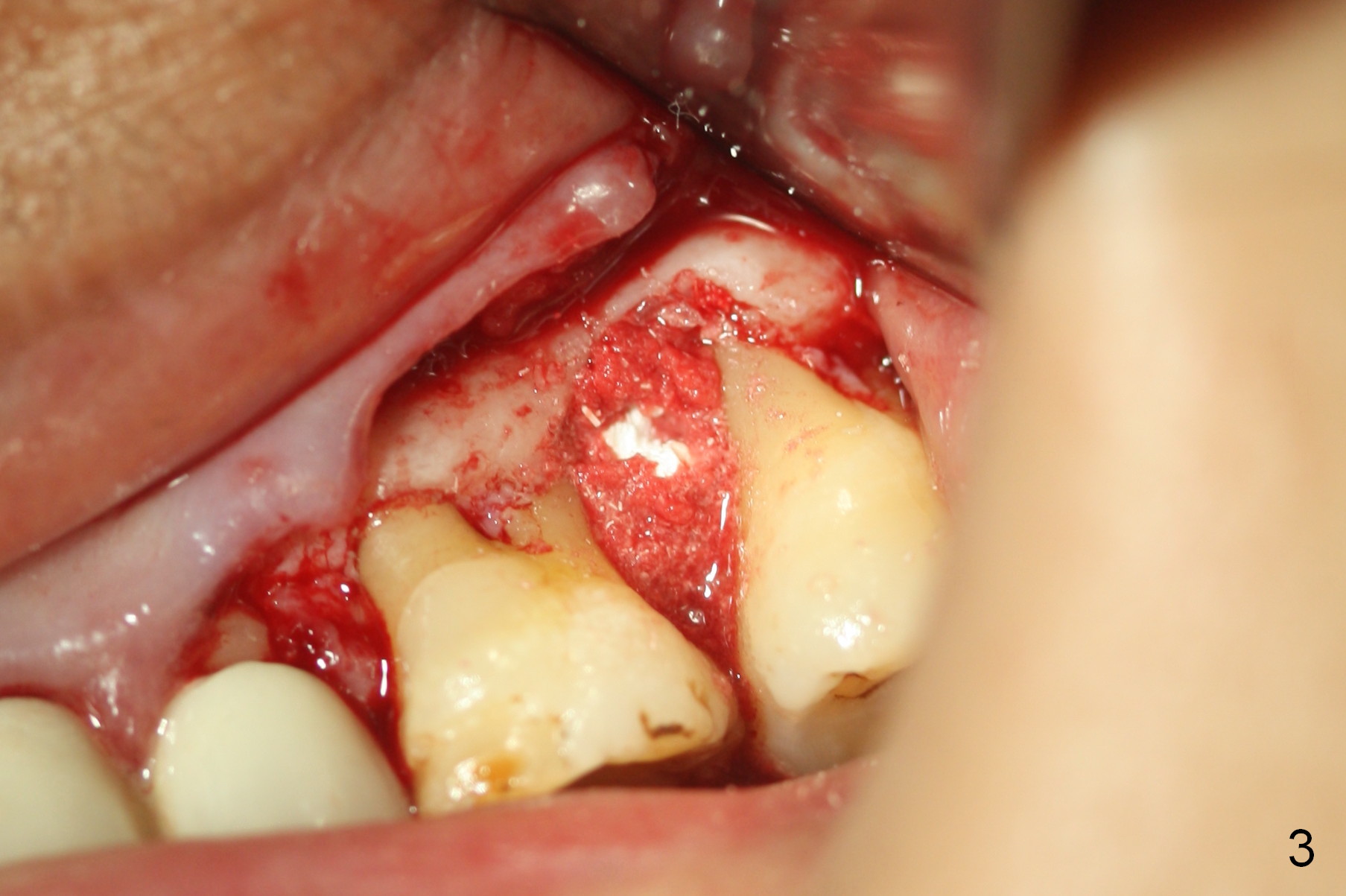
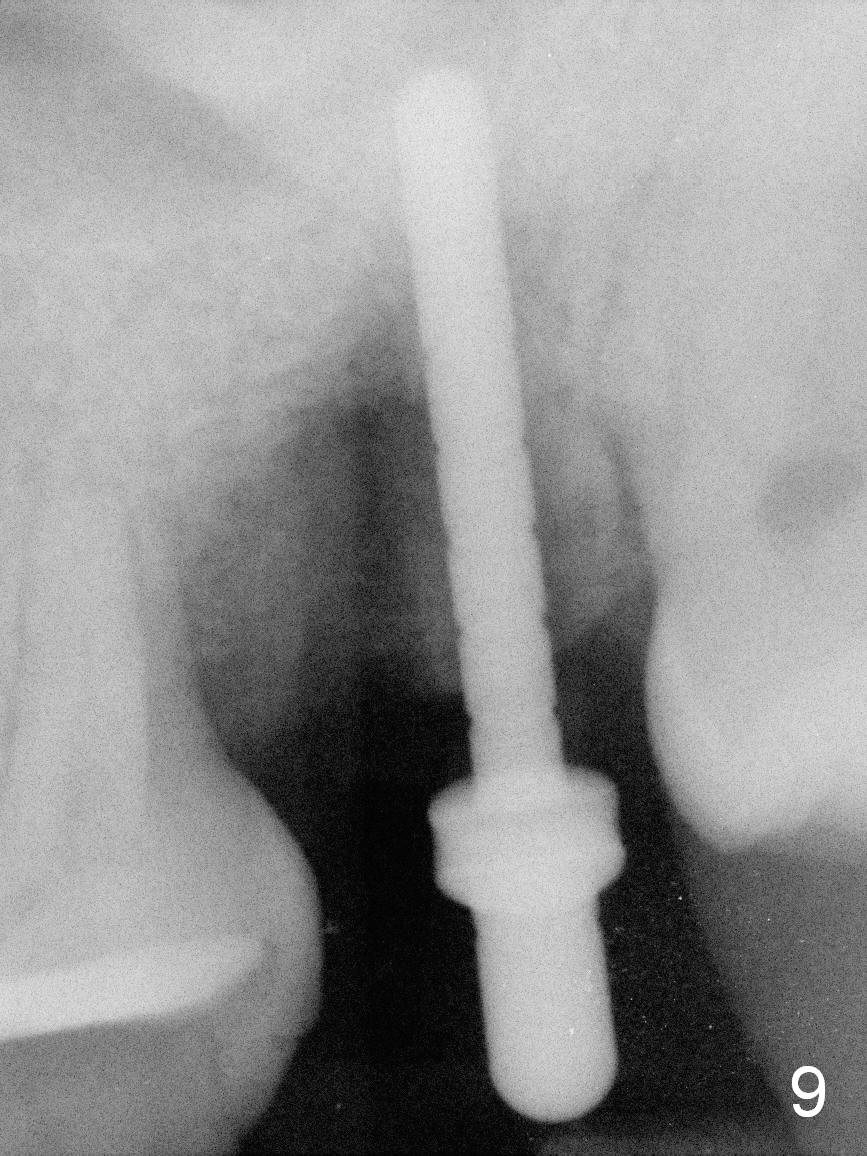
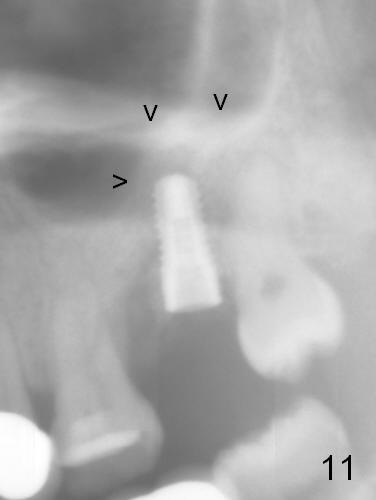
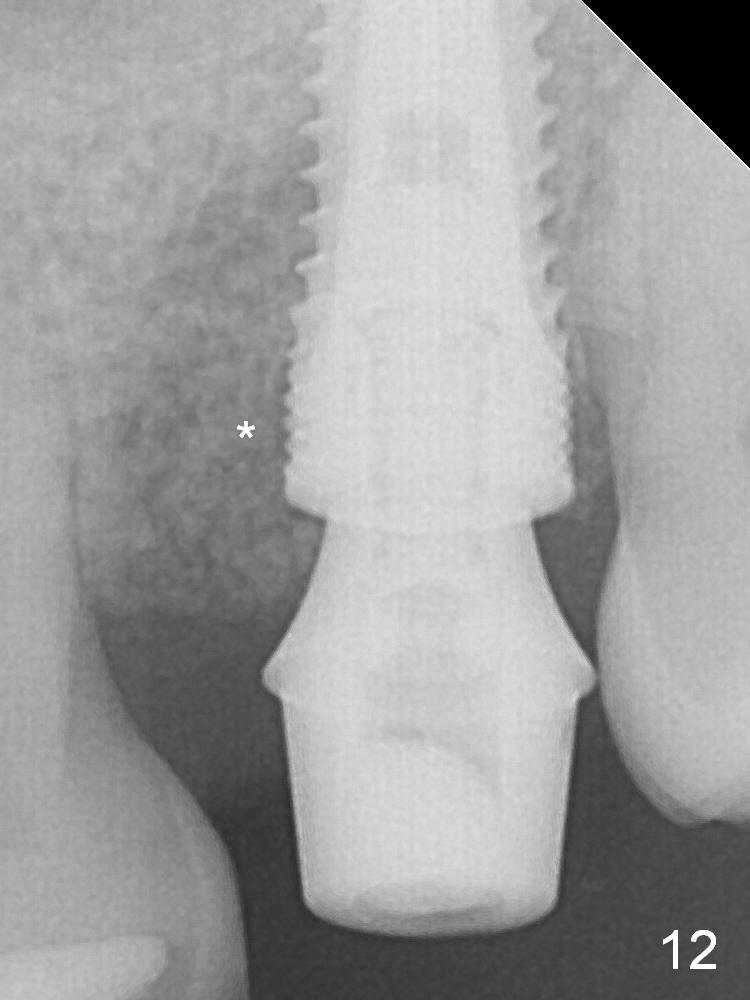
In fact, there is no gross buccal plate defect. No blood is collected for PRF. Osteotomy is difficult due to limited space with a parallel pin in place (Fig.9). After a 5x10 mm bone level implant is placed (~35 Ncm), allograft (mixed with autogenous bone and Osteogen) is packed in remaining socket (Fig.10 *). Immediately postop panoramic X-ray shows sinus lift (Fig.11 arrowheads). A 5.8x4(3) mm abutment is placed for an immediate provisional. There seems to be bone regeneration or reorganization around the implant 8 months postop (Fig.12 *).
Take photos to show gingival regrowth when the patient returns for impression.
In fact, the implant proves to be fibrointegrated.
Return to Upper Molar Immediate Implant
Xin Wei, DDS, PhD, MS 1st edition 01/17/2016, last revision 02/04/2017