%20before%20graft.jpg)

 |
 |
%20before%20graft.jpg) |
 |
 |
 |
 |
 |
 |
 |
Palatally Placed Implant
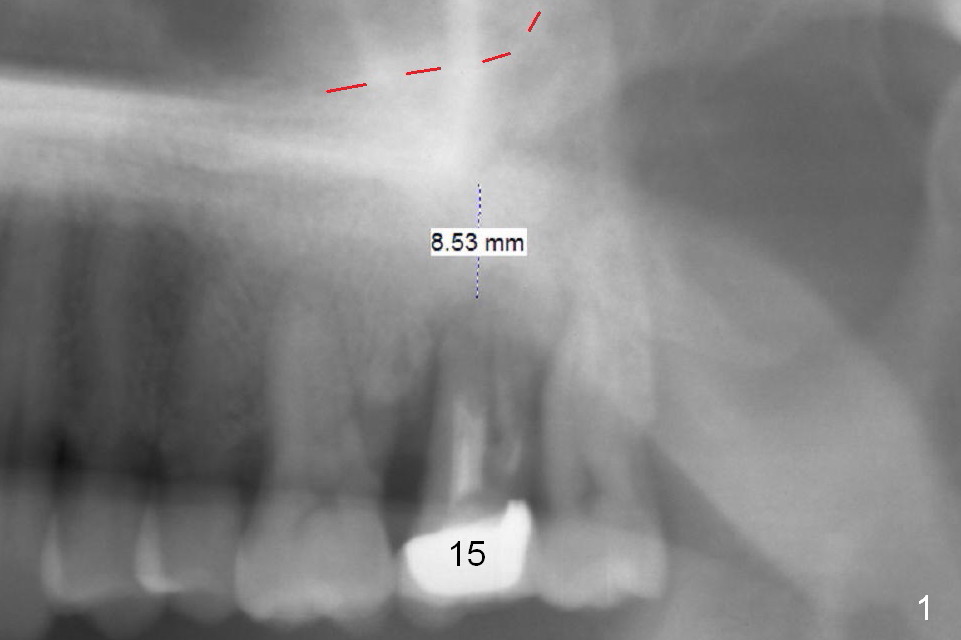
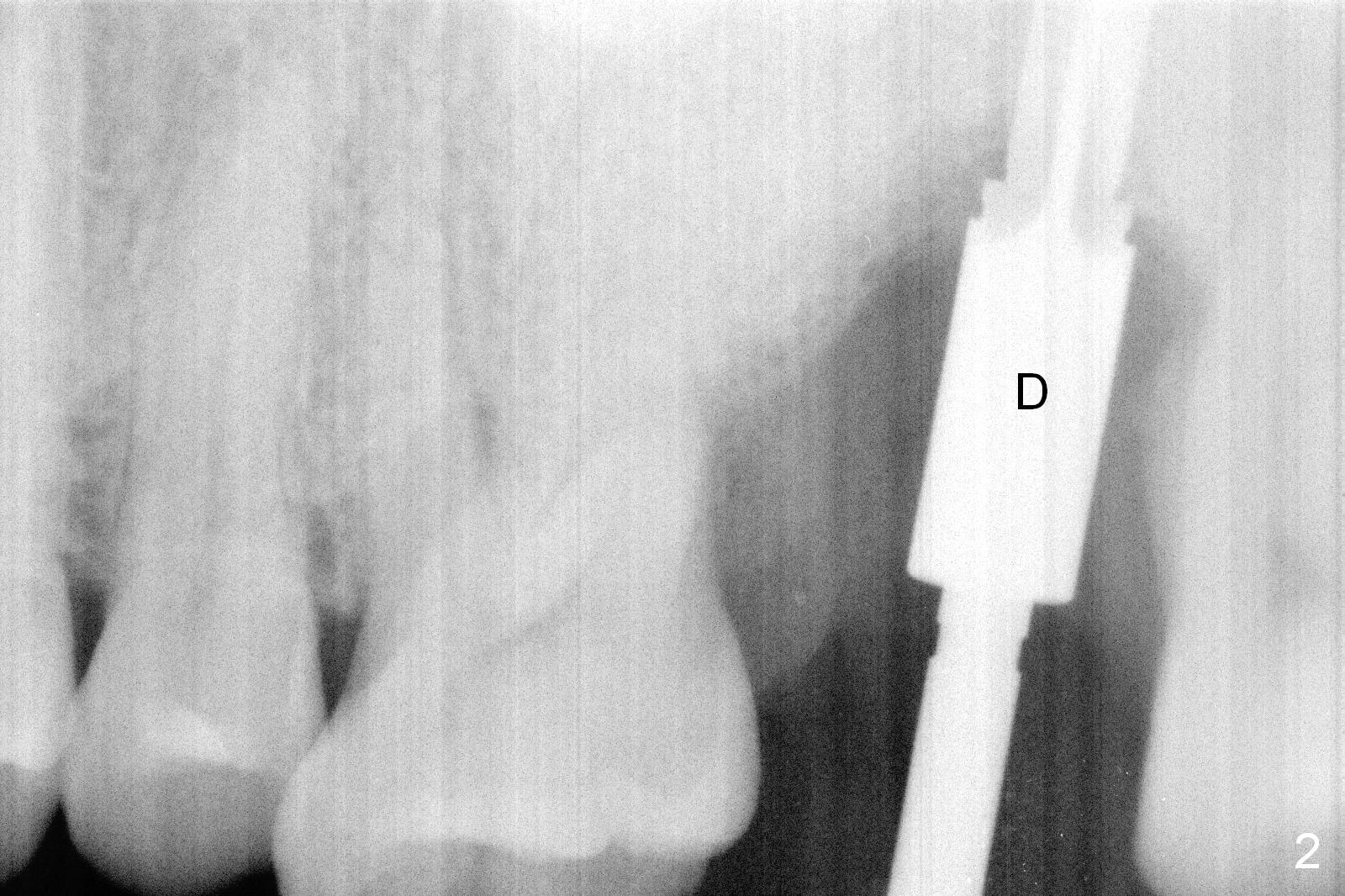
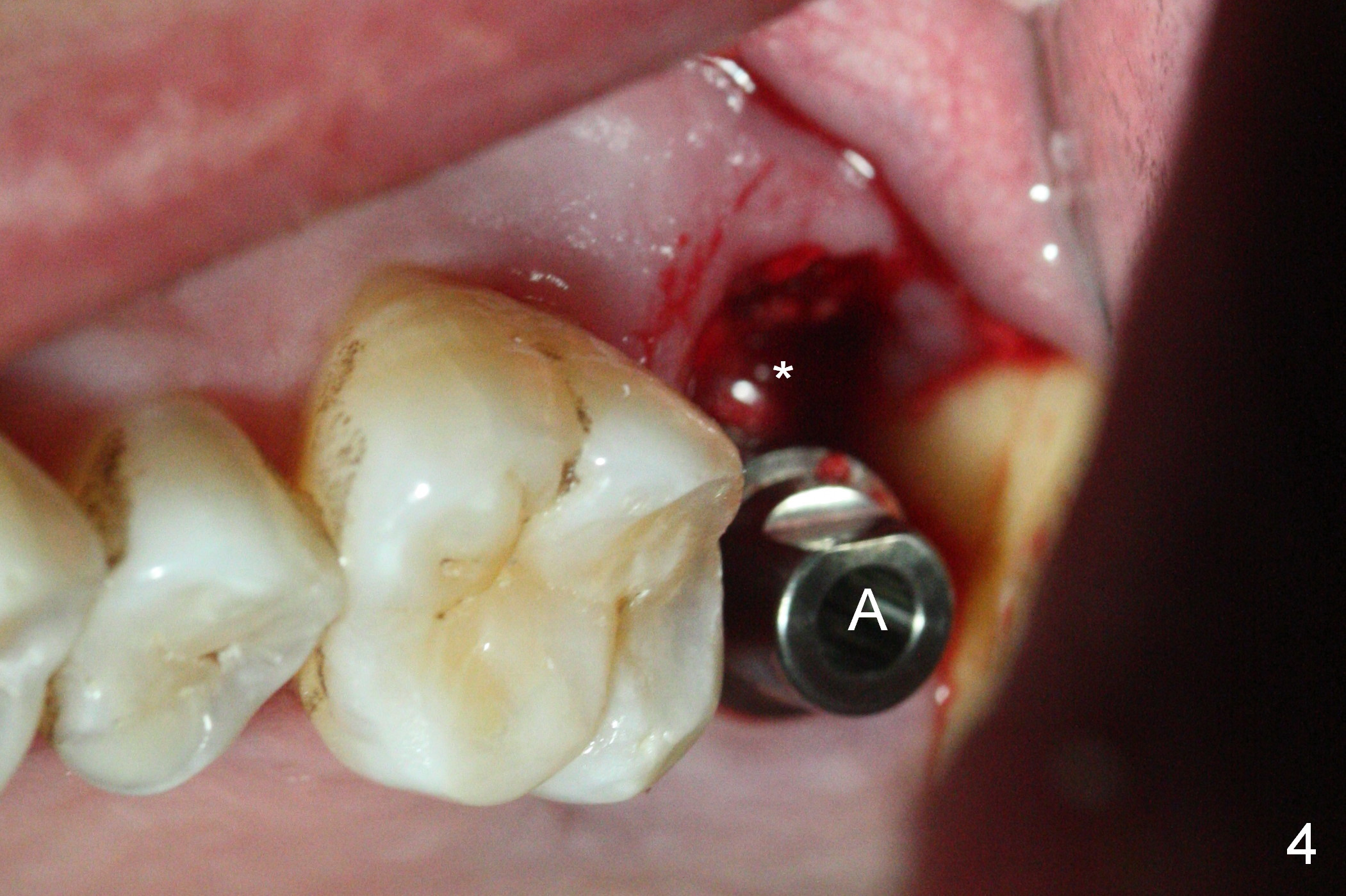
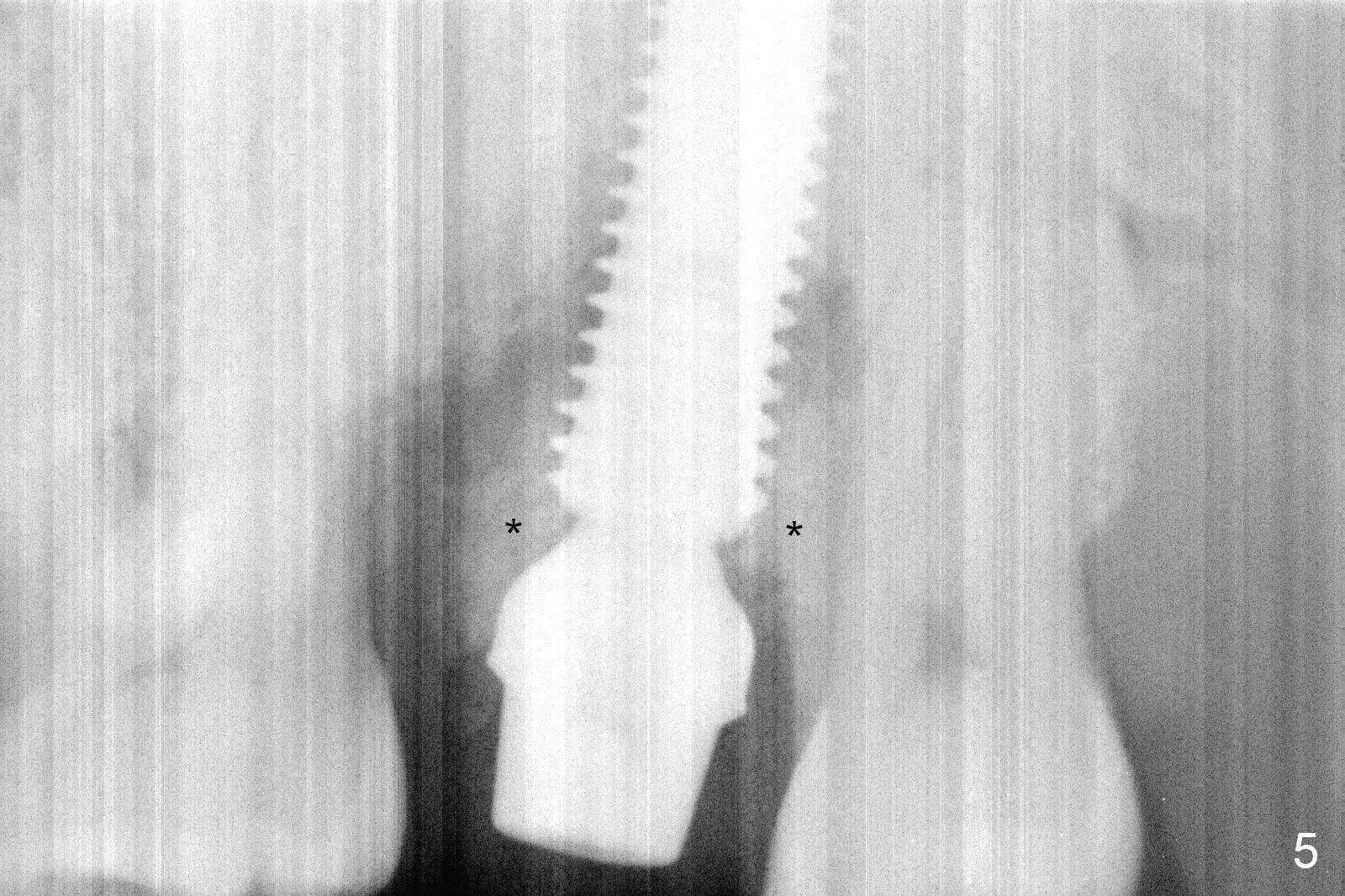
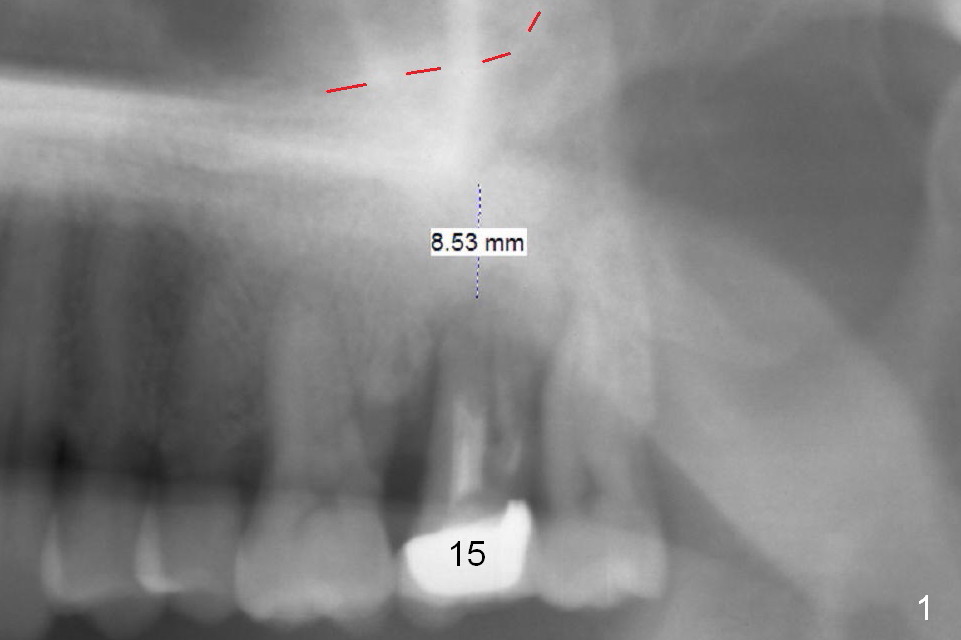
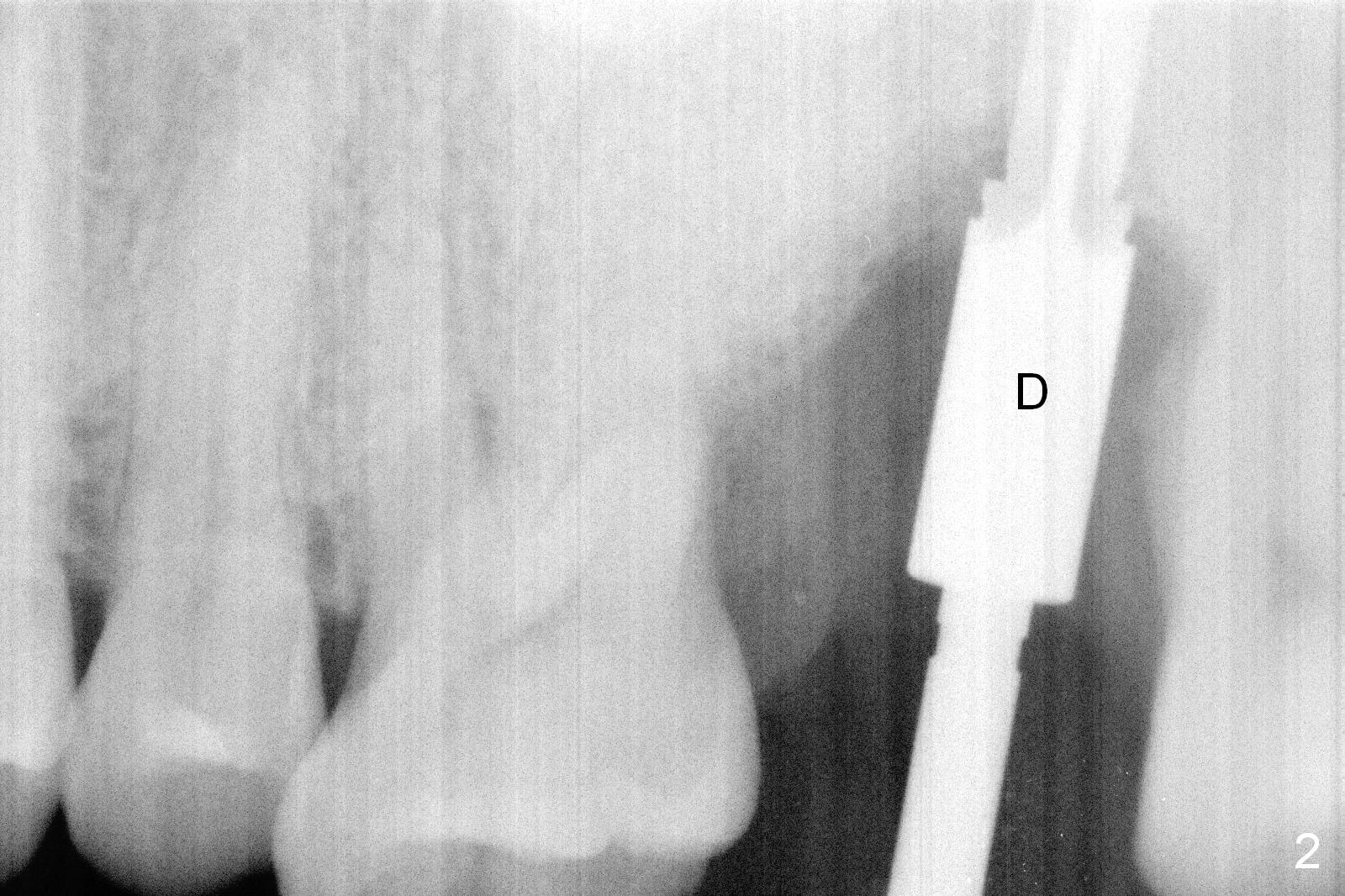
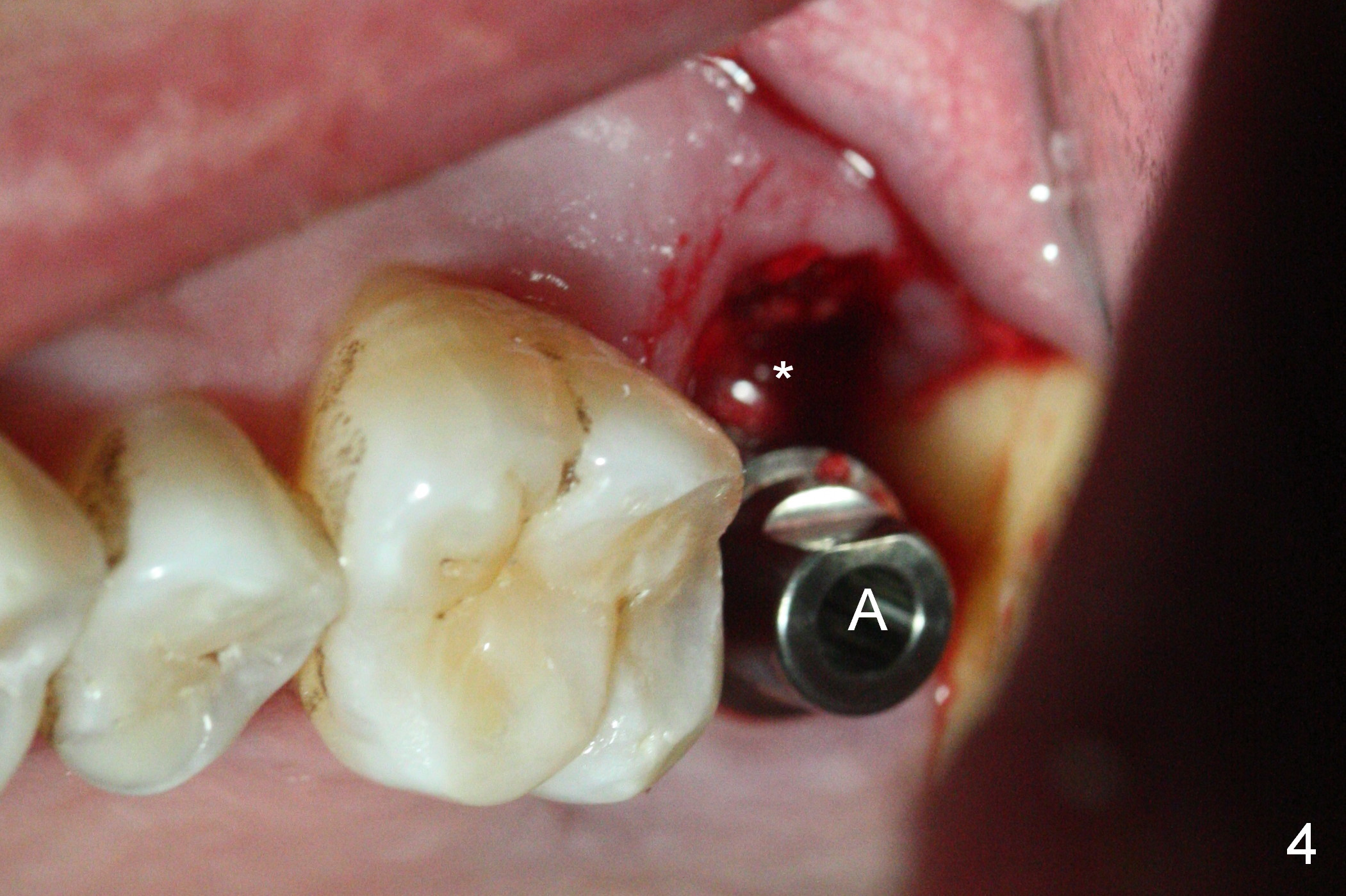
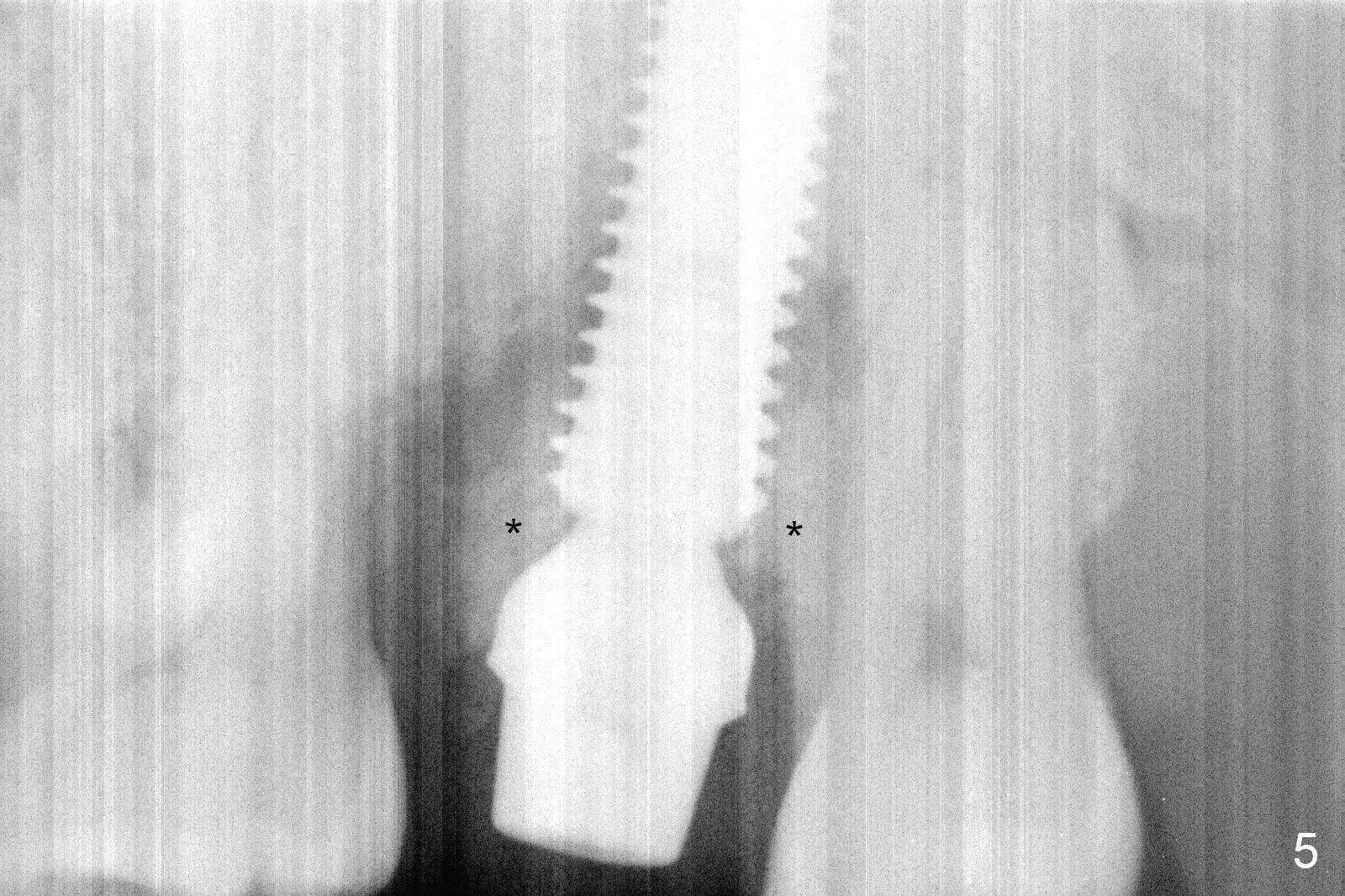
When the tooth #15 is extracted, the buccal plate is found to have been lost. The depth of osteotomy in the native bone is 8.5 mm (Fig.1,2). When a 5.5x15 mm implant is placed (Fig.3), the insertion torque is > 55 Ncm. The implant is palatally placed with a 10x10 mm Osteogen plug being placed in the deep portion of the buccal gap for buccal plate repair (Fig.4 *). The superficial portion of the remaining socket is filled with .5-1.5 mm allograft/autogenous bone/Osteogen (Fig.5 *). The drawback of this procedure is that the abutment is placed prior to placement of the graft. The latter fails to reach the deepest area of the defect. If periimplantitis develops because of insufficient graft, do it again in due time.
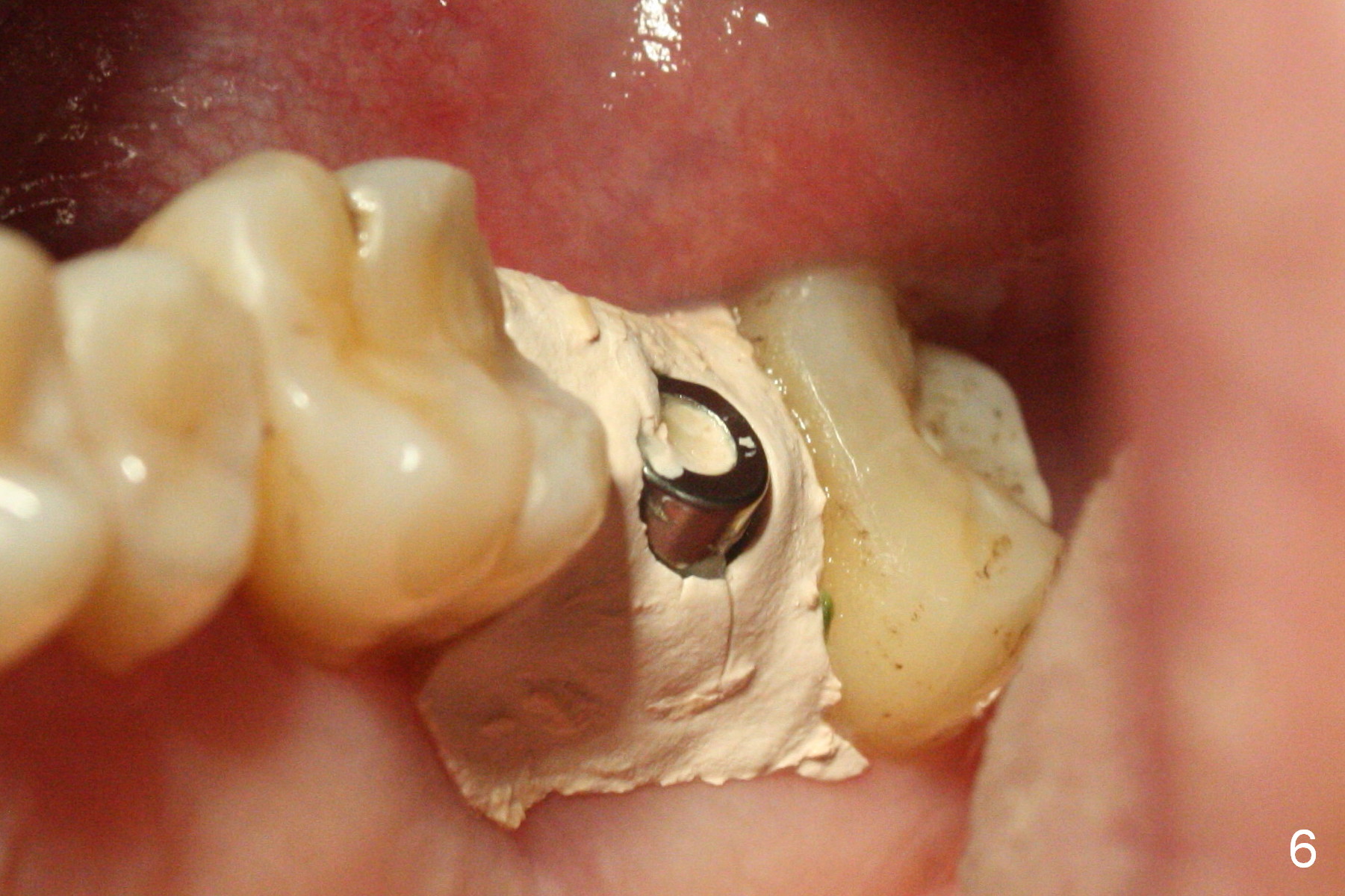
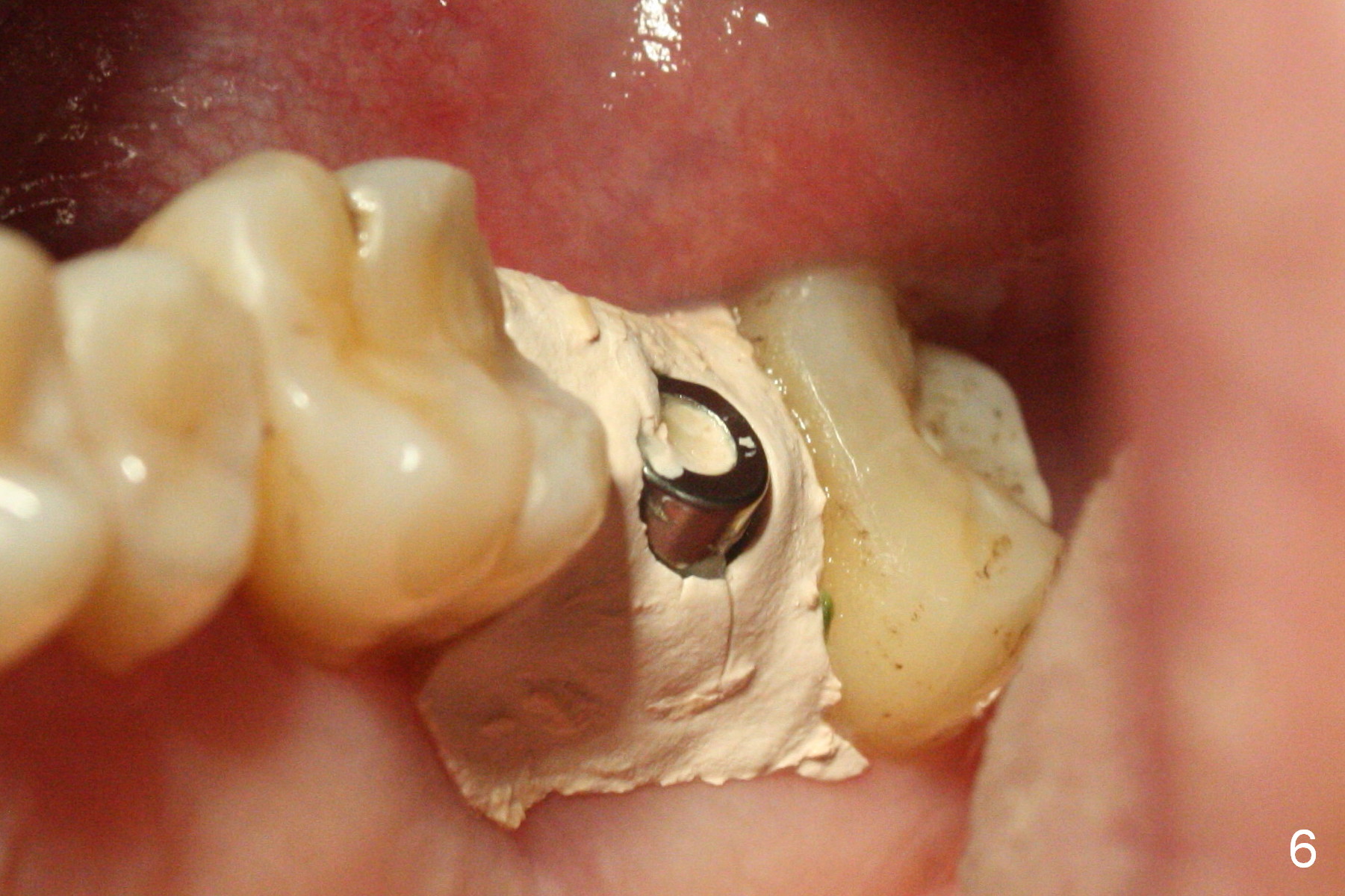
An immediate provisional is laid outside the buccal gingiva to prevent loss of bone graft, but a large gap develops underneath the provisional buccally with loss of bone graft, noted 1 month postop. The buccal gingiva is also found to perforate after removal of the provisional. These are related to the extensive preop buccal plate loss. The buccal threads are exposed. After induction of hemorrhage from the surrounding healthy granulation tissue, Osteogen plug is placed in the buccal gap, covered by periodontal dressing, which stays 9 days postop (Fig.6).
Ideally, the provisional should have been fabricated with a buccal extension placed inside the buccal gingiva for support and more secure holding bone graft in place.
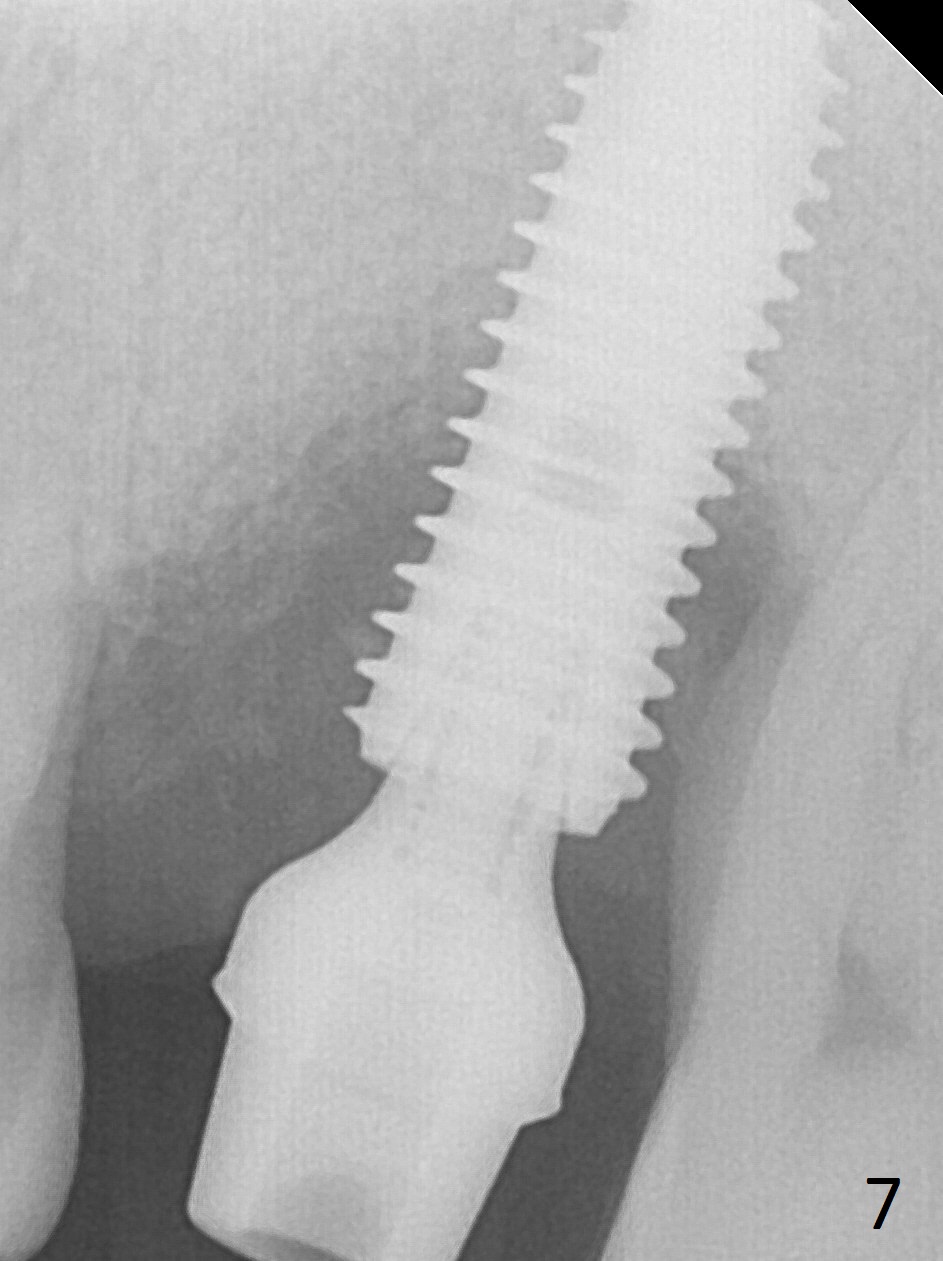
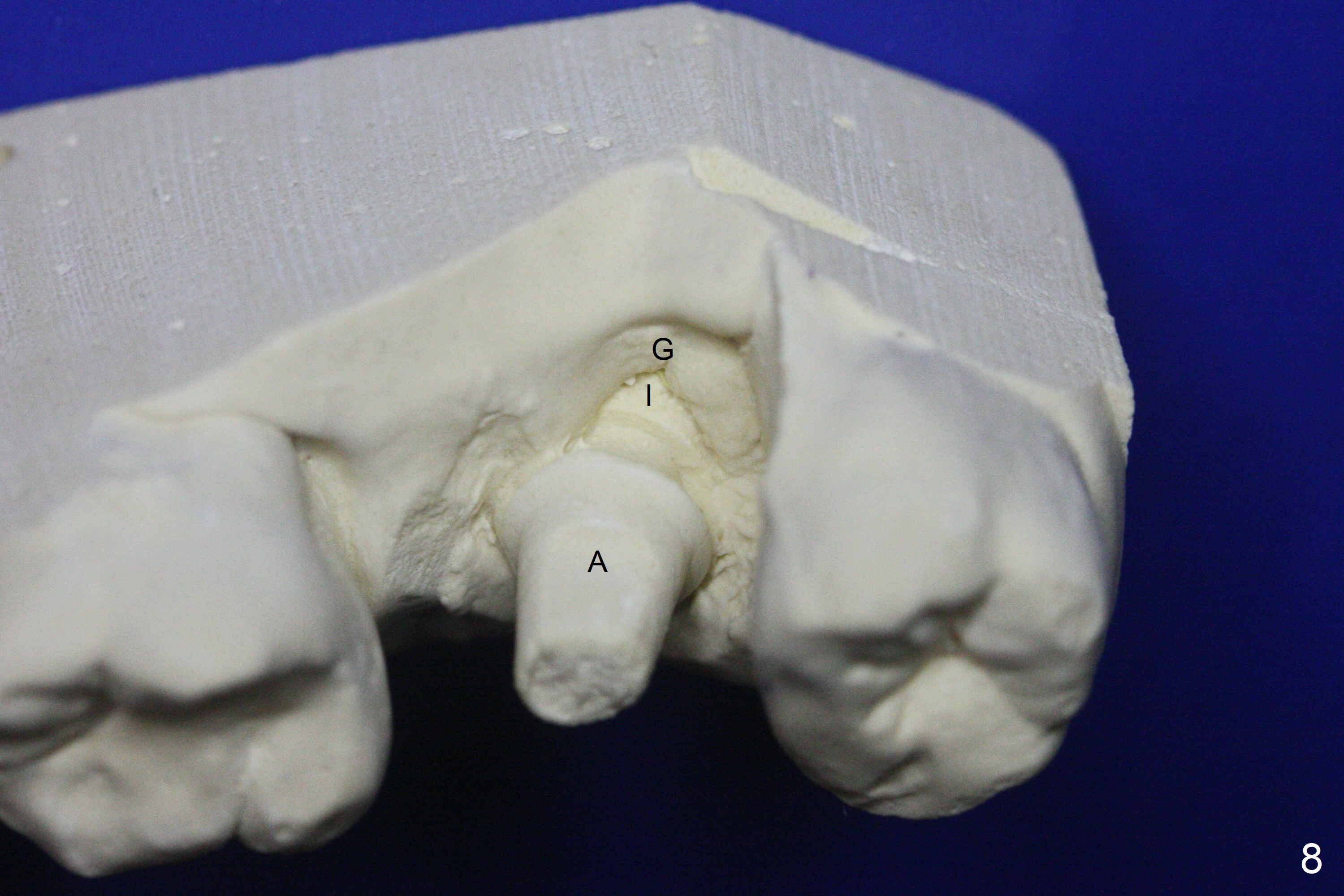
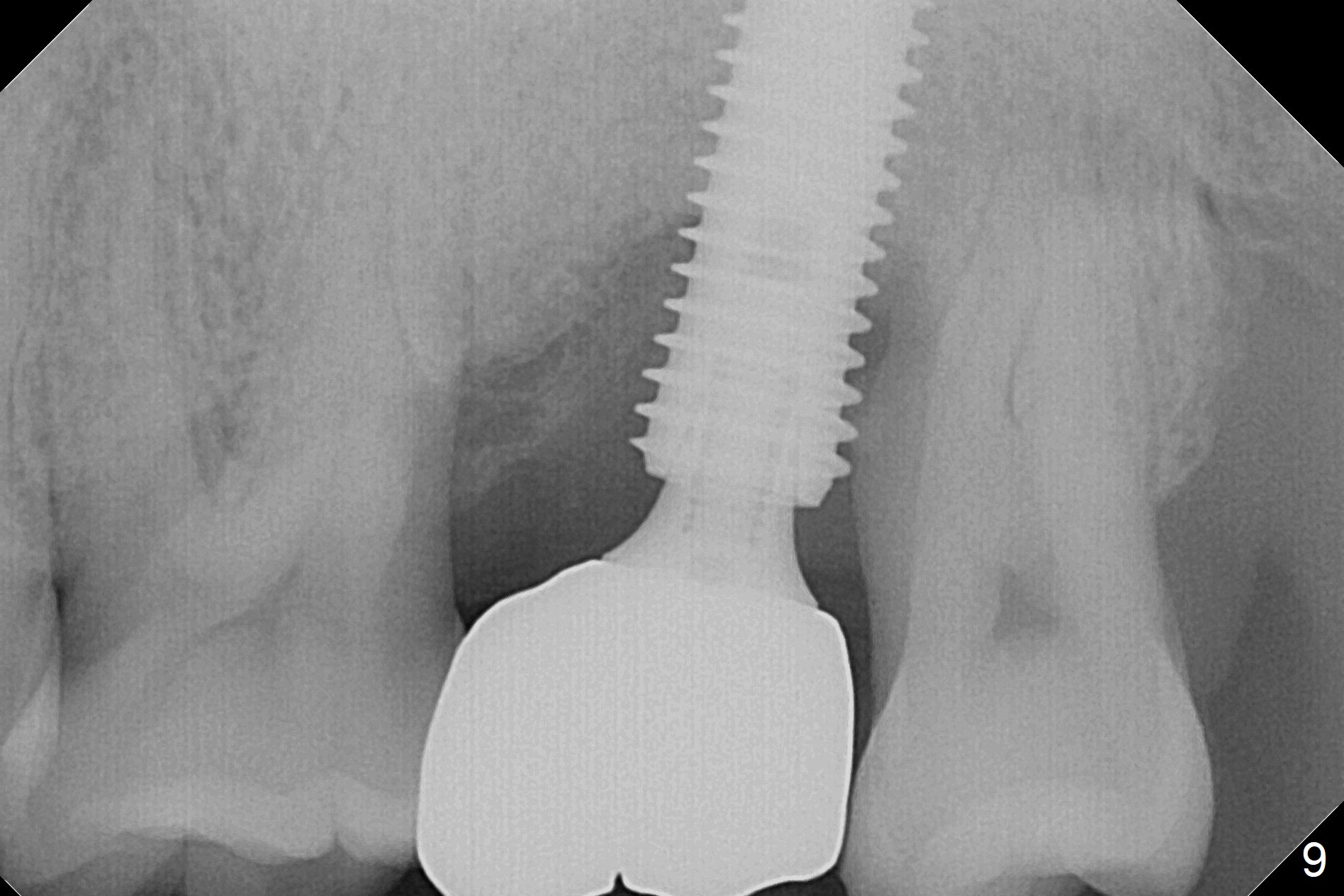
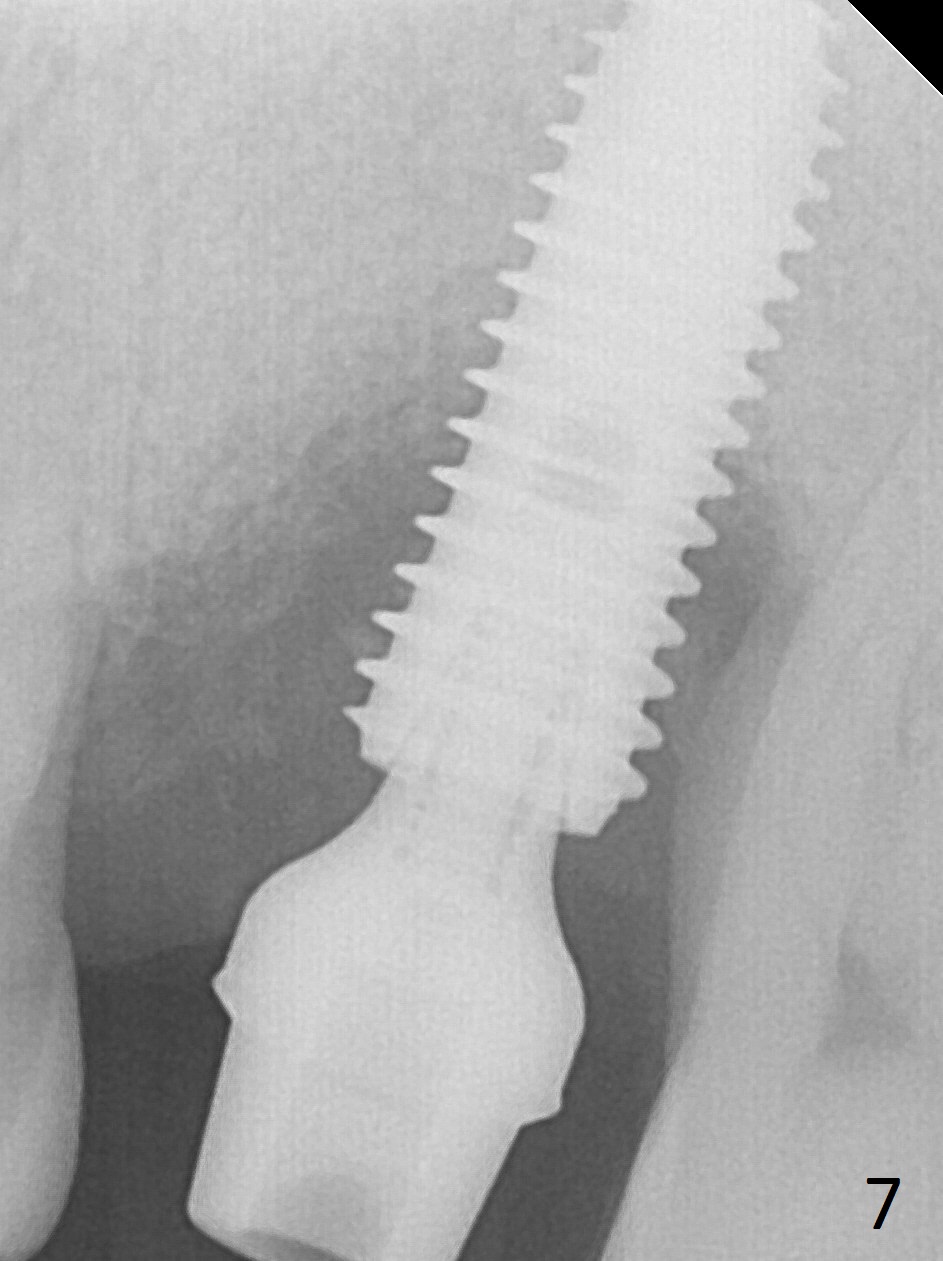
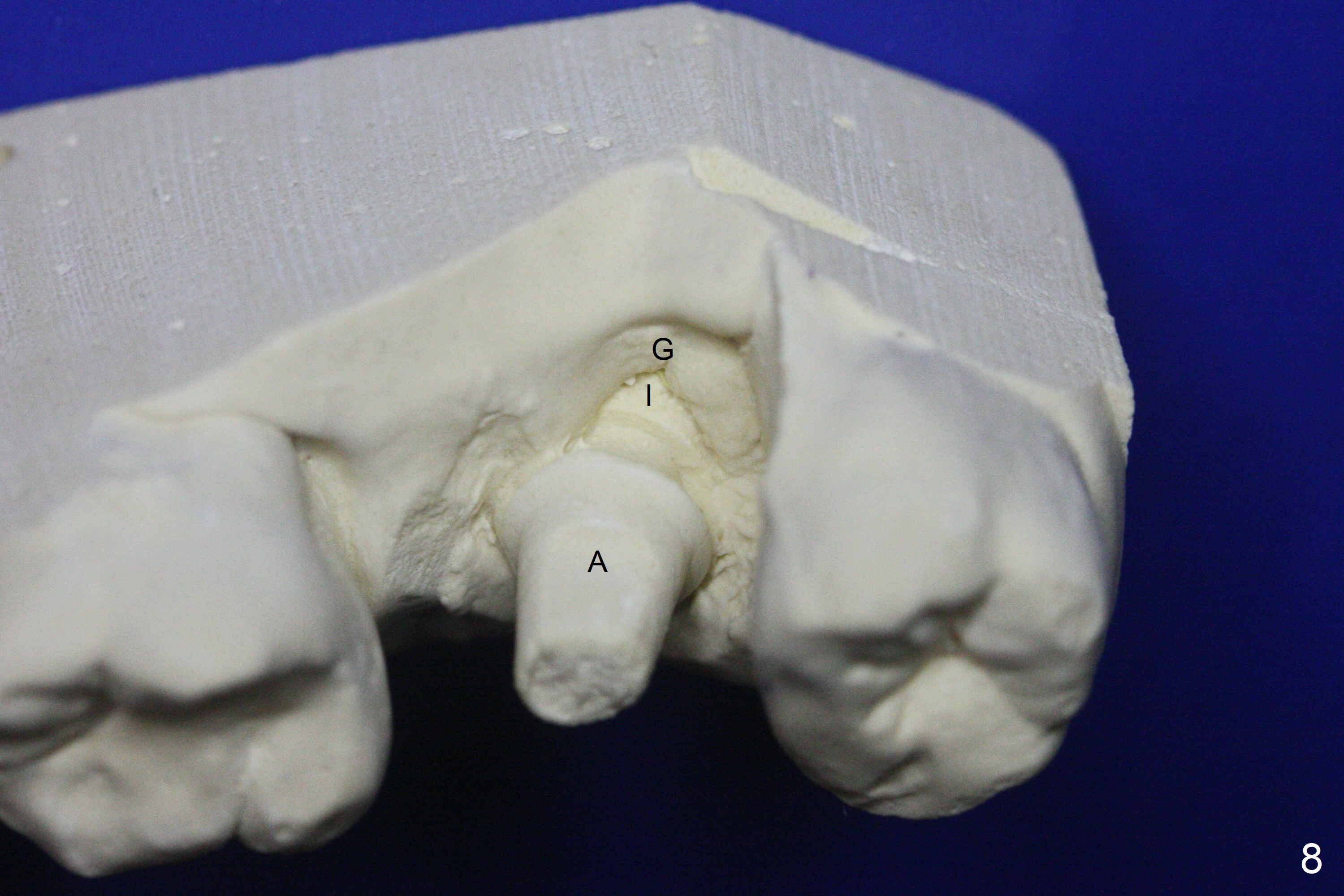
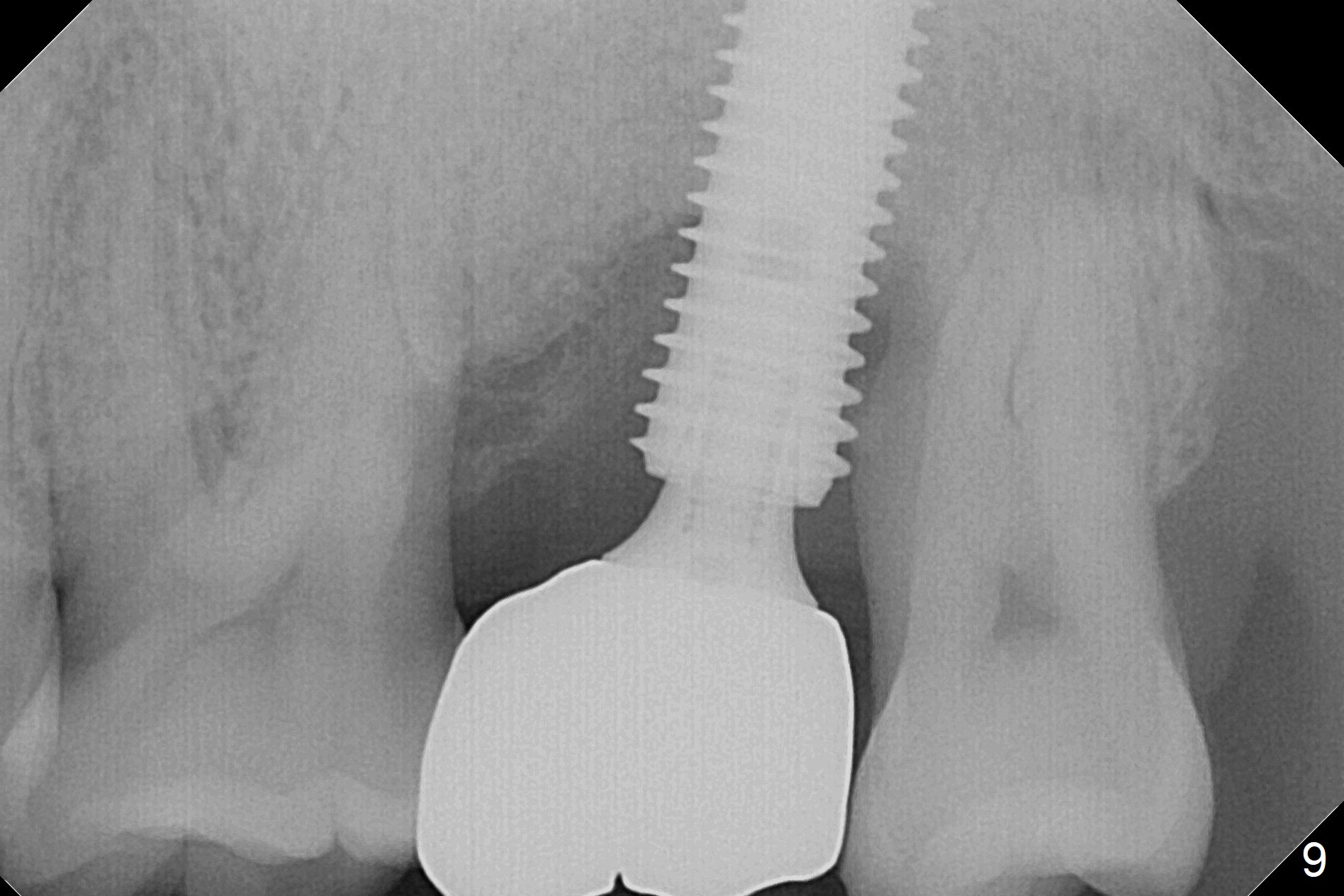
There is severe gingival recession: 15 DB, implant plateau exposure, surrounded by healthy granulation tissue, 3.5 months postop. PA shows #15 + implant osteointegration and bone loss coronally (Fig.7). Afterward, the abutment is changed from 6.5x4(4) to 5.5x5(2) mm with fabrication of a provisional. The patient feels that it is easier to brush with a temporary crown. Model shows gingival recession (Fig.8 G) with implant thread exposure distobuccally (I). Although there is no obvious change in bone regeneration 7.5 months postop (2.5 months post cementation, Fig.9) as compared to Fig.7, there is no more distobuccal gingival recession (data not shown; due to use of Water Pik). To avoid the gingival recession, the implant should have been placed more mesial and deeper (Fig.10 green) with use of a longer-cuff (pink) abutment.
Return to
Upper
Molar Immediate Implant, Prevent
Molar Periimplantitis (Protocols,
Table),
IBS
Xin Wei, DDS, PhD, MS 1st edition 11/22/2016, last revision 07/07/2017