
,%20Osteogen%20plug,%20autogenous%20bone,%20collagen%20plug,%20before%20temp%20seating.jpg)
,%20Osteogen%20plug,%20autogenous%20bone,%20collagen%20plug,%20more%20oblique.jpg)
 |
 |
 |
,%20Osteogen%20plug,%20autogenous%20bone,%20collagen%20plug,%20before%20temp%20seating.jpg) |
,%20Osteogen%20plug,%20autogenous%20bone,%20collagen%20plug,%20more%20oblique.jpg) |
 |
 |
 |
 |
 |
 |
 |
Repair Sinus Membrane Perforation
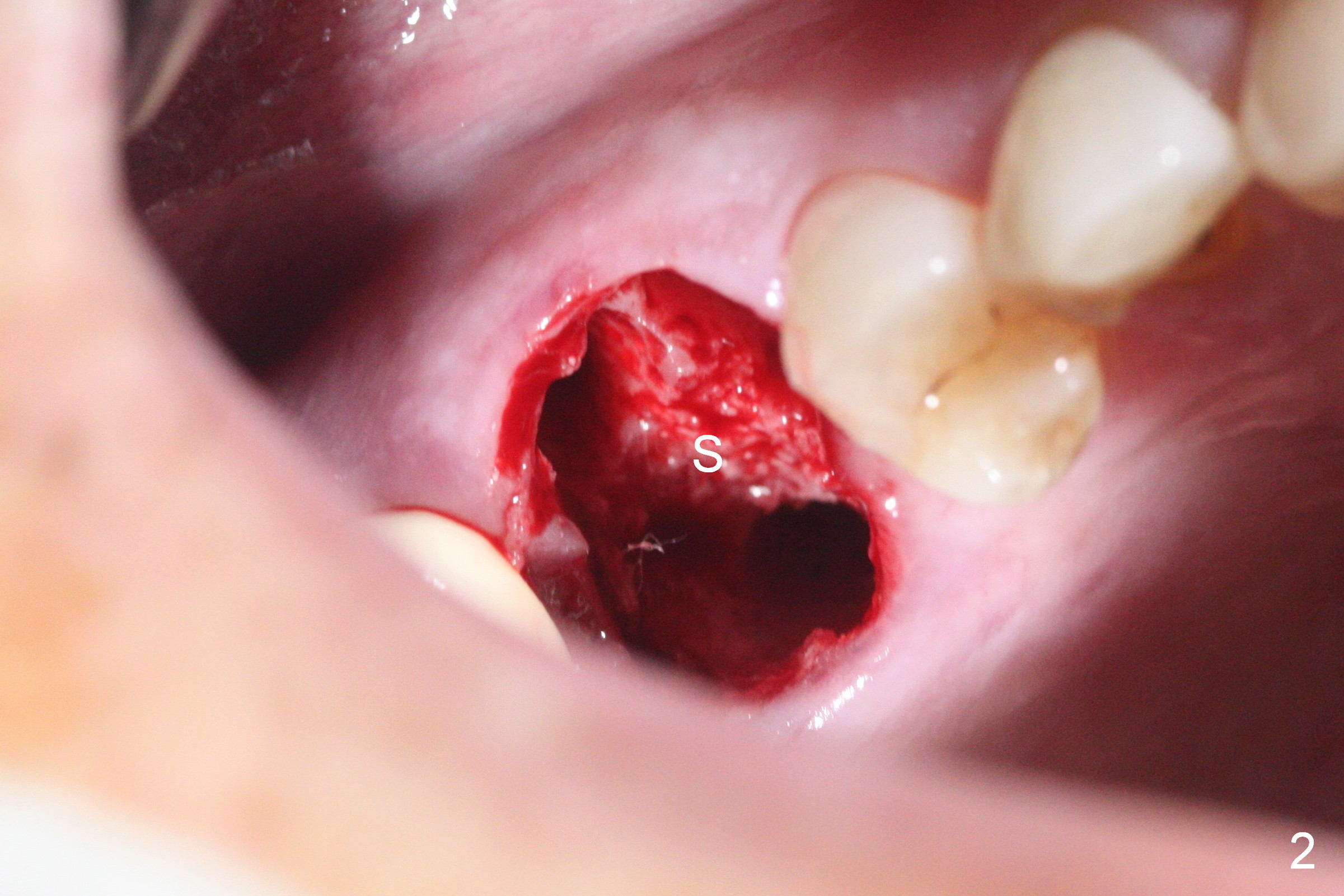
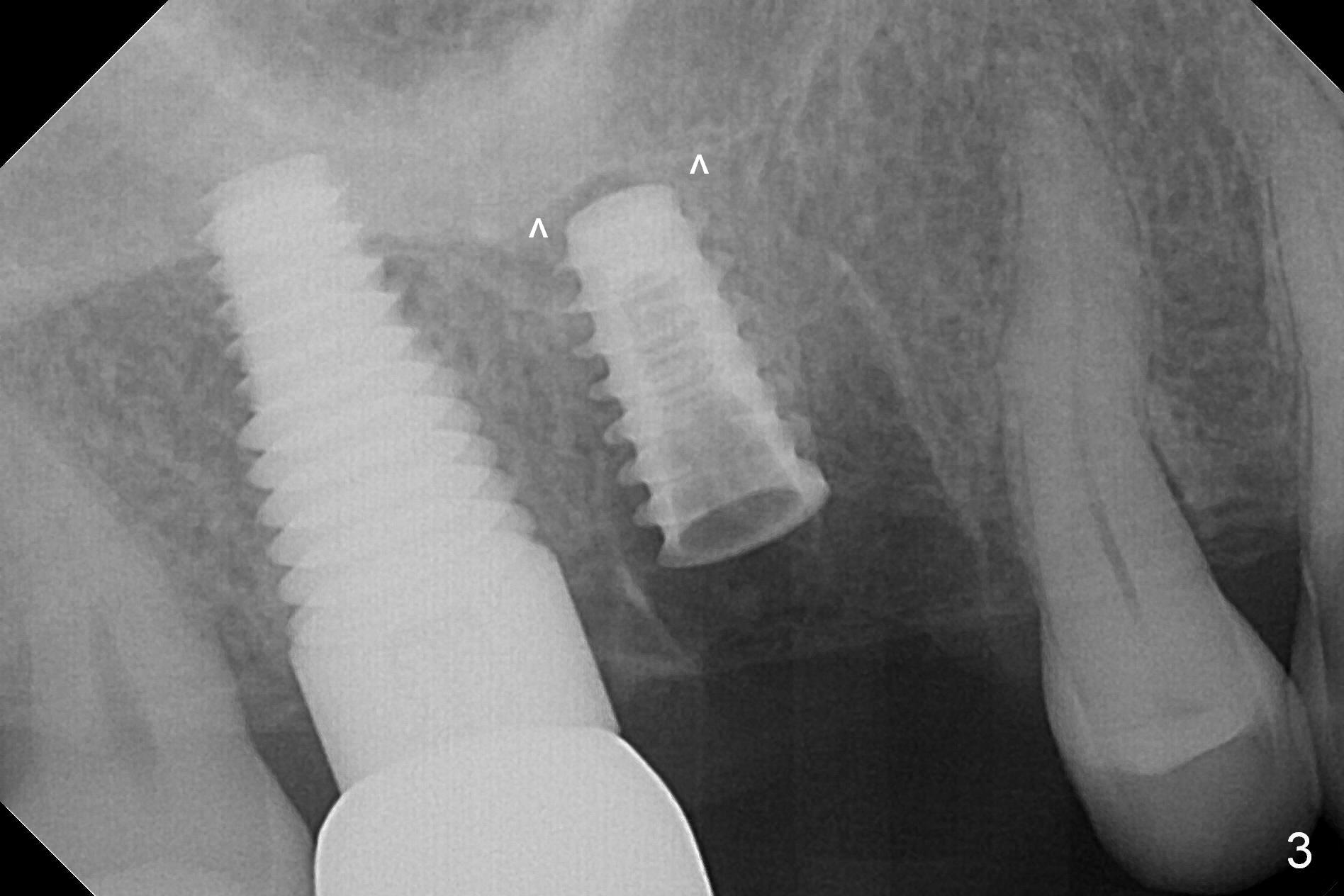
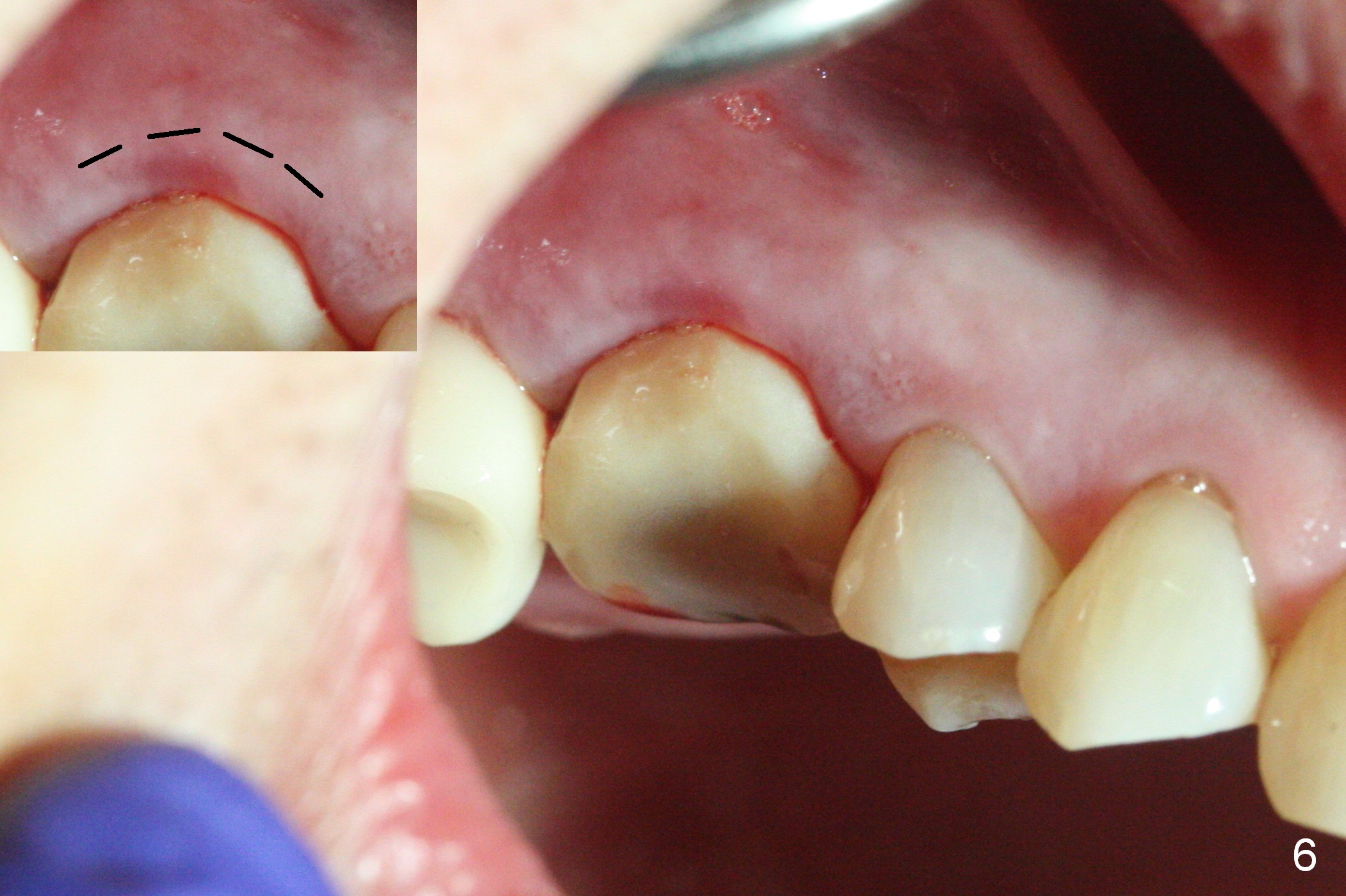
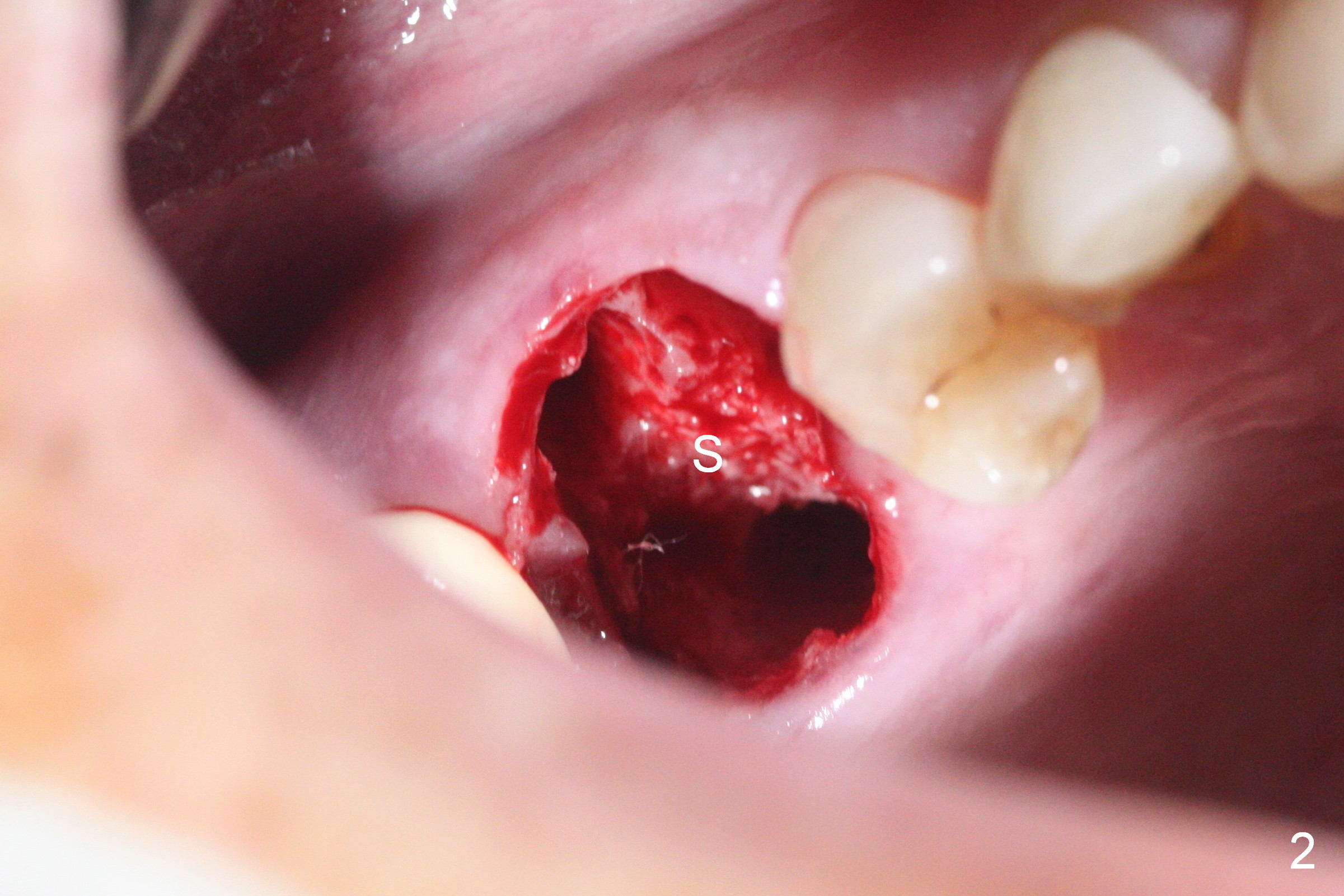
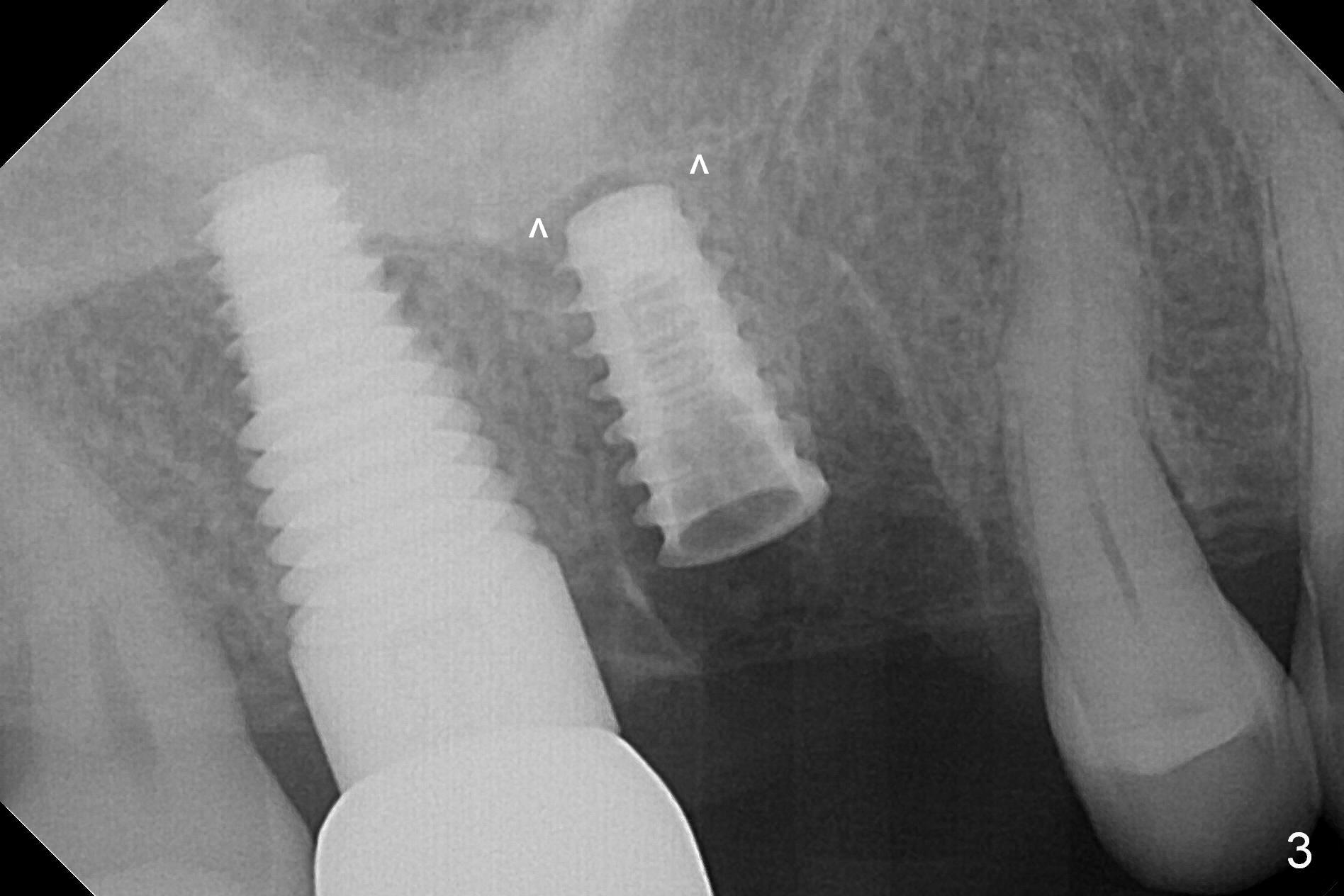
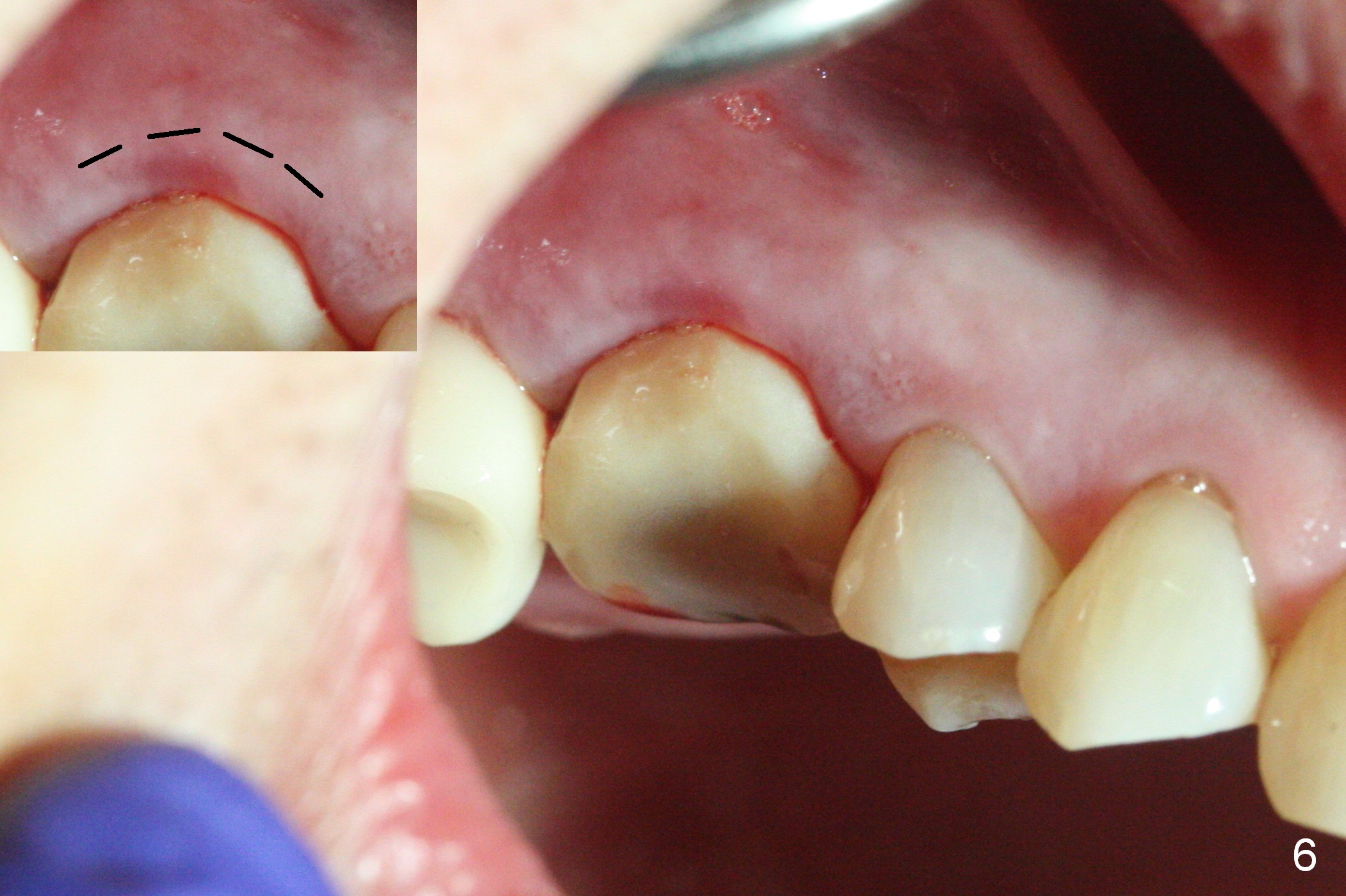
Heavy bruxism is characterized by the crack at #3 (symptomatic, requiring emergency extraction) and loss of the palatal cusp at #5 (Fig.1). Osteotomy is initiated in the septal slope (Fig.2 S) with a 1.6 mm pilot drill for 9 mm (with sudden empty feeling), followed by Marking bur. After 4.3 mm Magic Drill is used for ~ 9 mm, the sinus membrane is found to perforate. A dummy implant (5x9 mm, 2 mm shorter than design) is placed short of the sinus floor (Fig.3 ^). Prior to placement of 5.5x9 mm IBS implant (~ 35 Ncm, Fig.4,5), a piece of Osteogen plug is inserted into the osteotomy for repair of the perforation. The final implant is also shy of the sinus floor (Fig.5 ^). The Osteogen plug is apparently placed underneath the sinus floor so that it should be able to repair hard and soft tissue defects. The remaining sockets are mainly filled with Osteogen plug, while the implant plateau is covered by autogenous bone and Osteogen. When a 6.5x4(3) mm abutment is placed, an immediate provisional is fabricated (Fig.6) with its margin placed subgingival (Fig.6 inset dashed line). This innovative design of the provisional is to prevent collapse of the most coronal gingiva and loss of bone graft, particularly where the bony plate is defective. Although there is mild pain postop, nasal hemorrhage or discharge is absent.
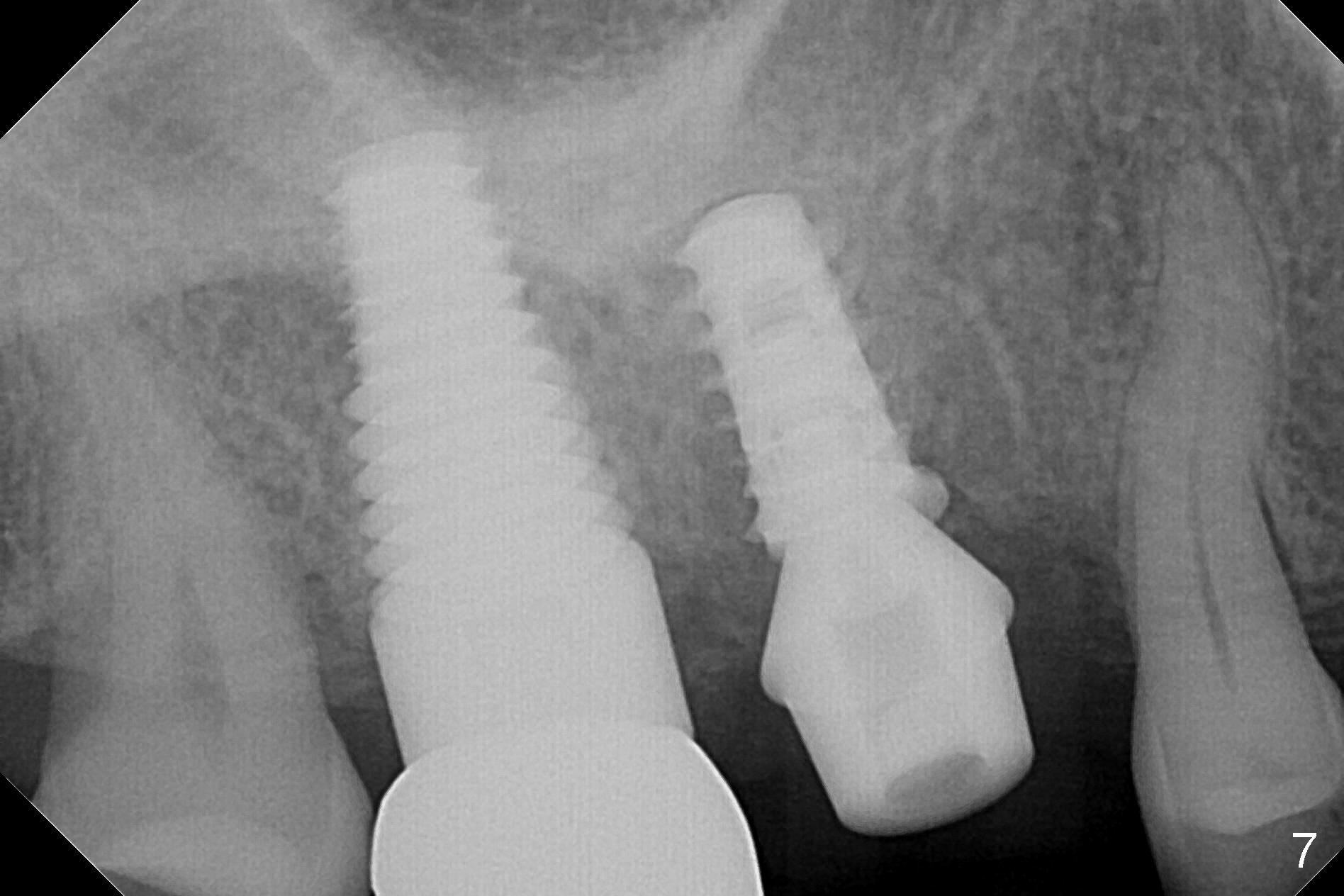
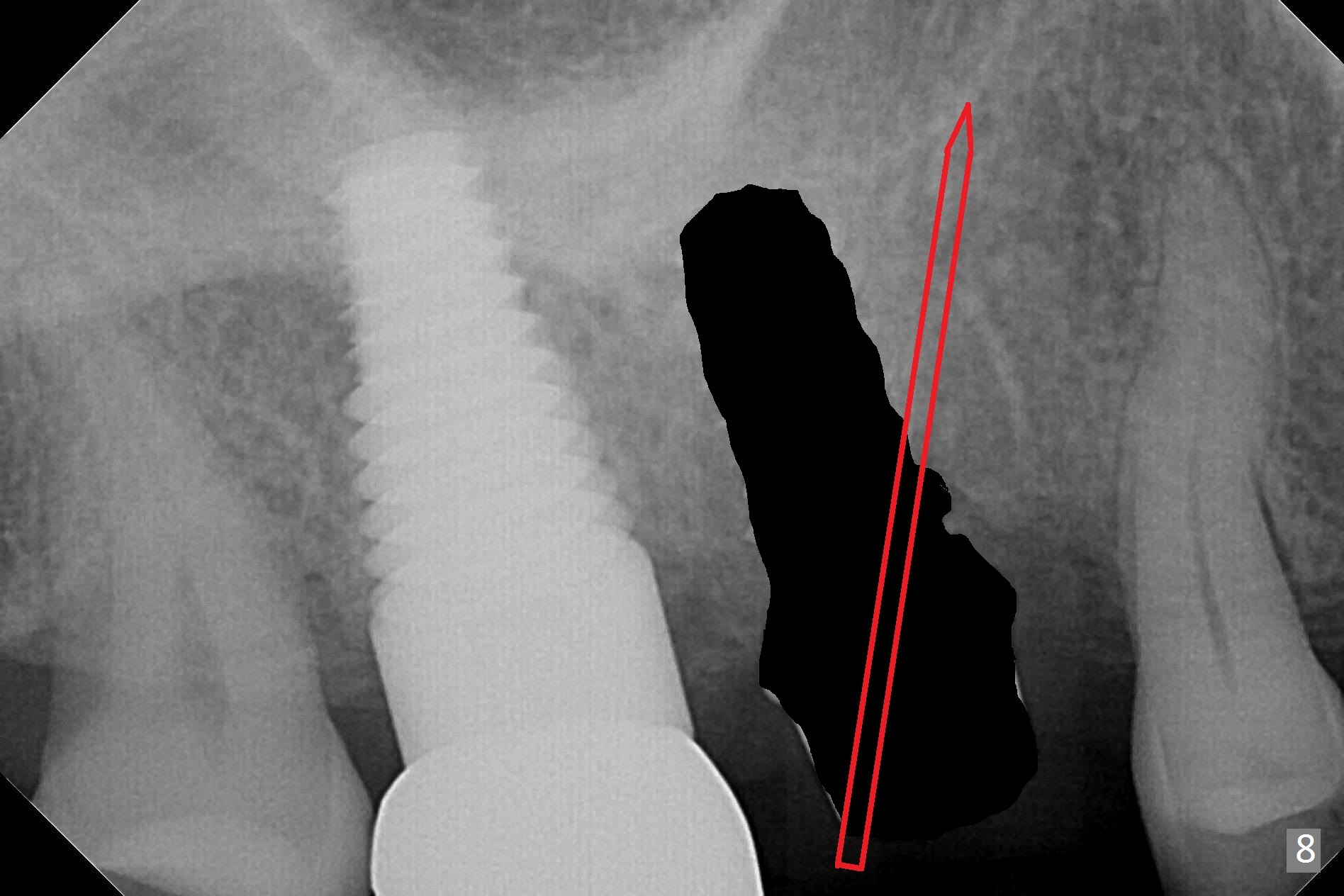
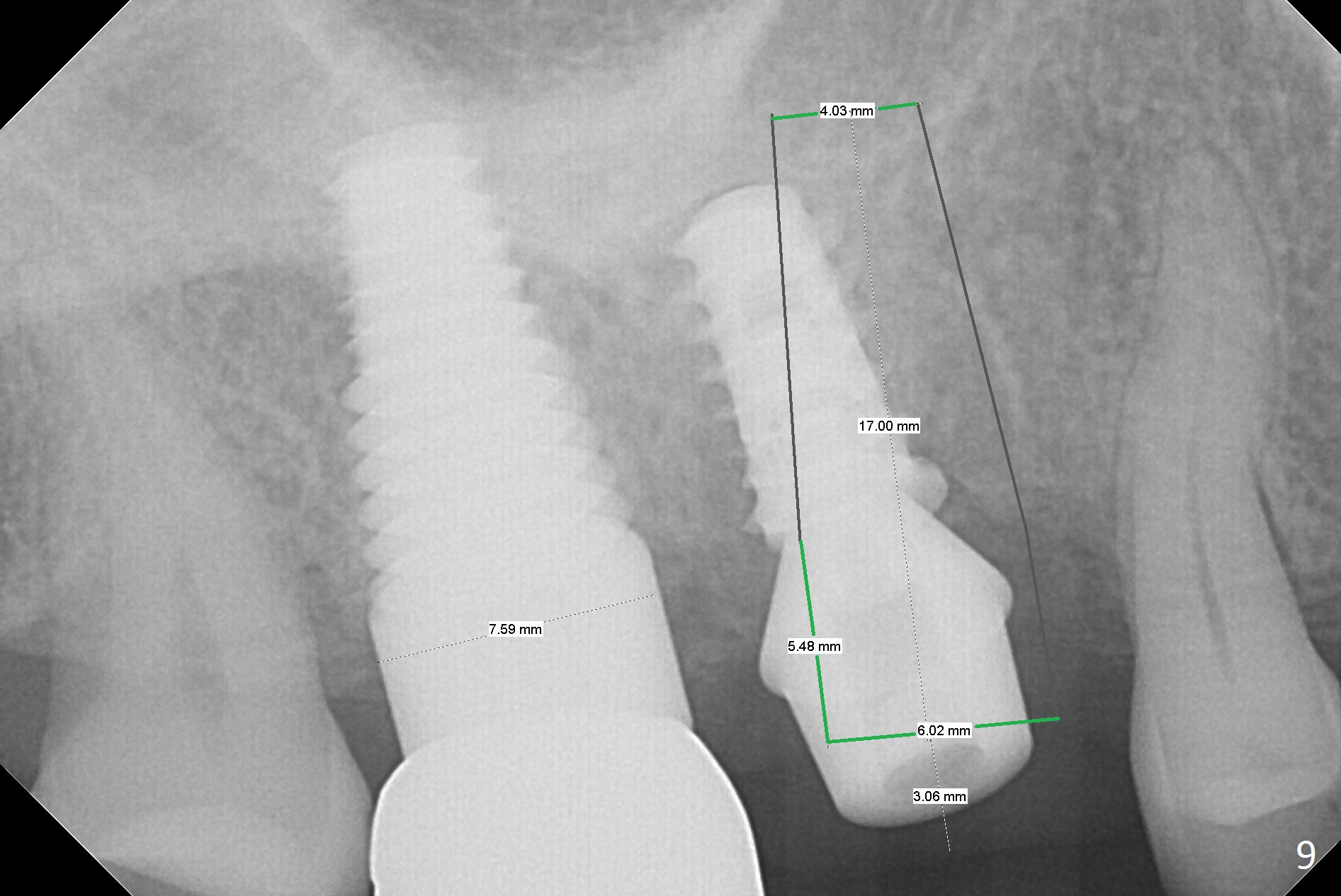
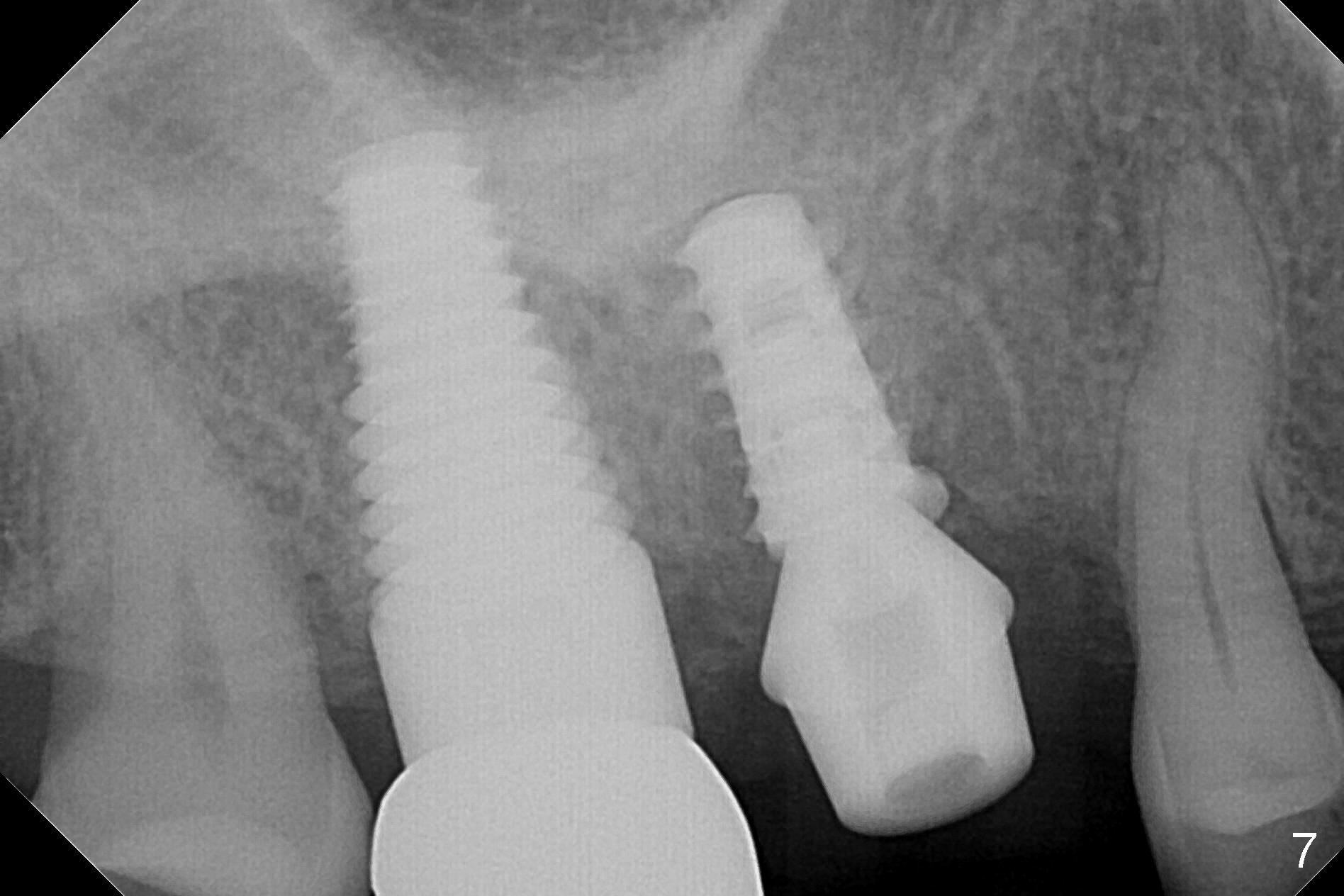
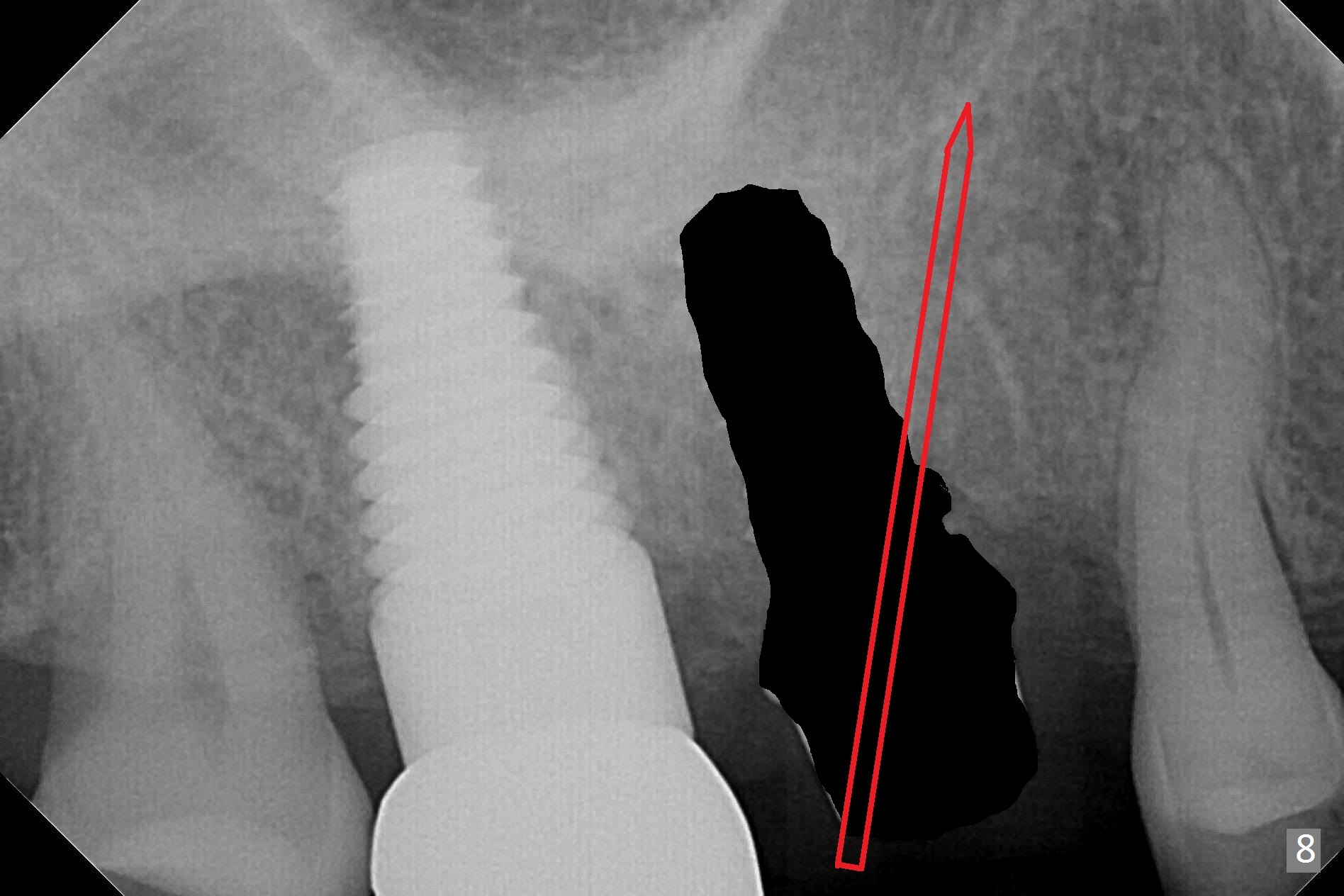
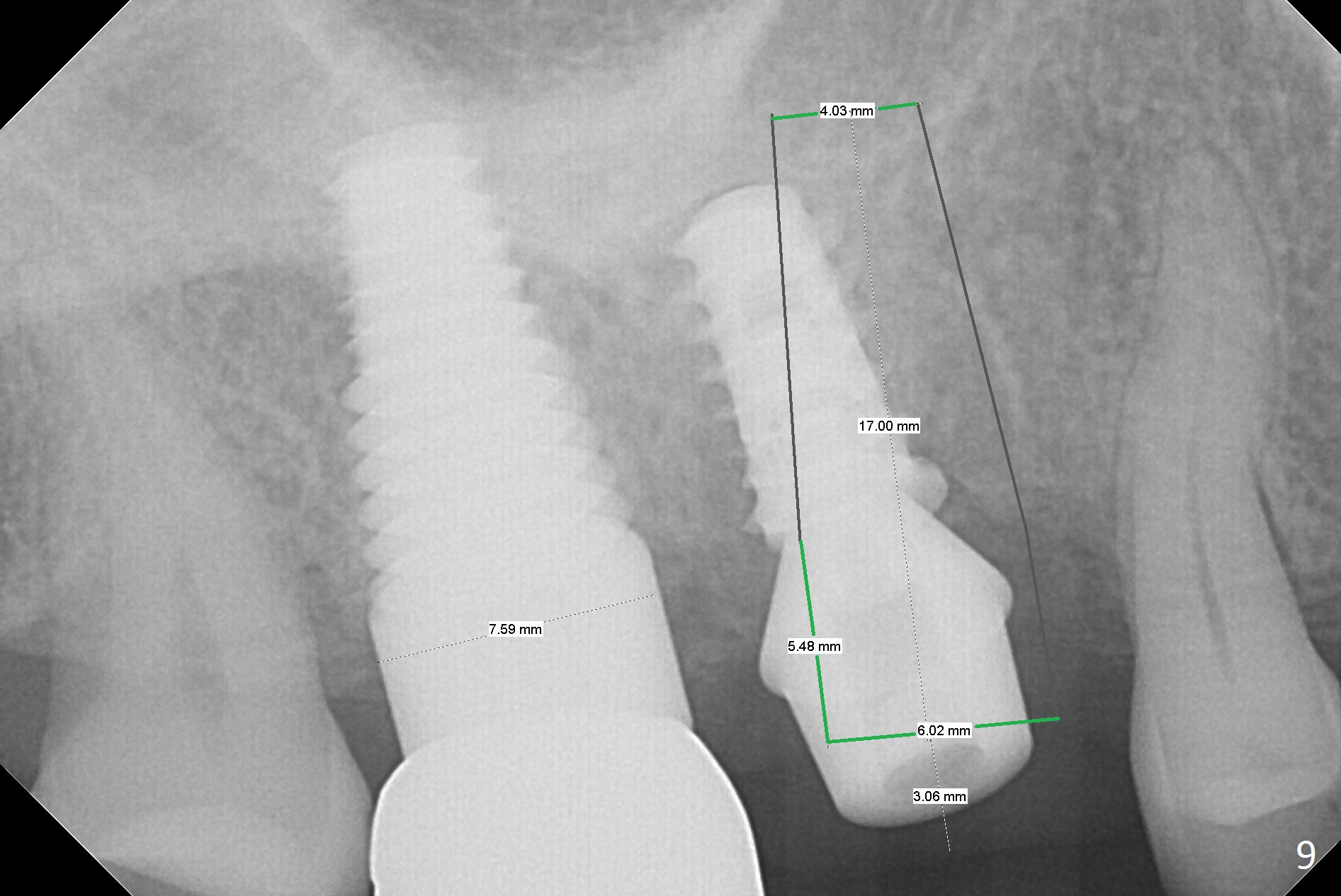
The patient returns with chief complaint of crown is loose with pain 3 months postop (Fig.7). Under local anesthesia, the provisional is removed. The gingiva is erythematous. The implant has mobility. A healing abutment is placed (6x2 mm). One month later, the implant remains unstable. The patient is scheduled to return 3.5 months postop to either retighten the implant with healing screw or replace with a 6x17 mm Tatum implant (Fig.9) after changing trajectory (Fig.8 red arrow).
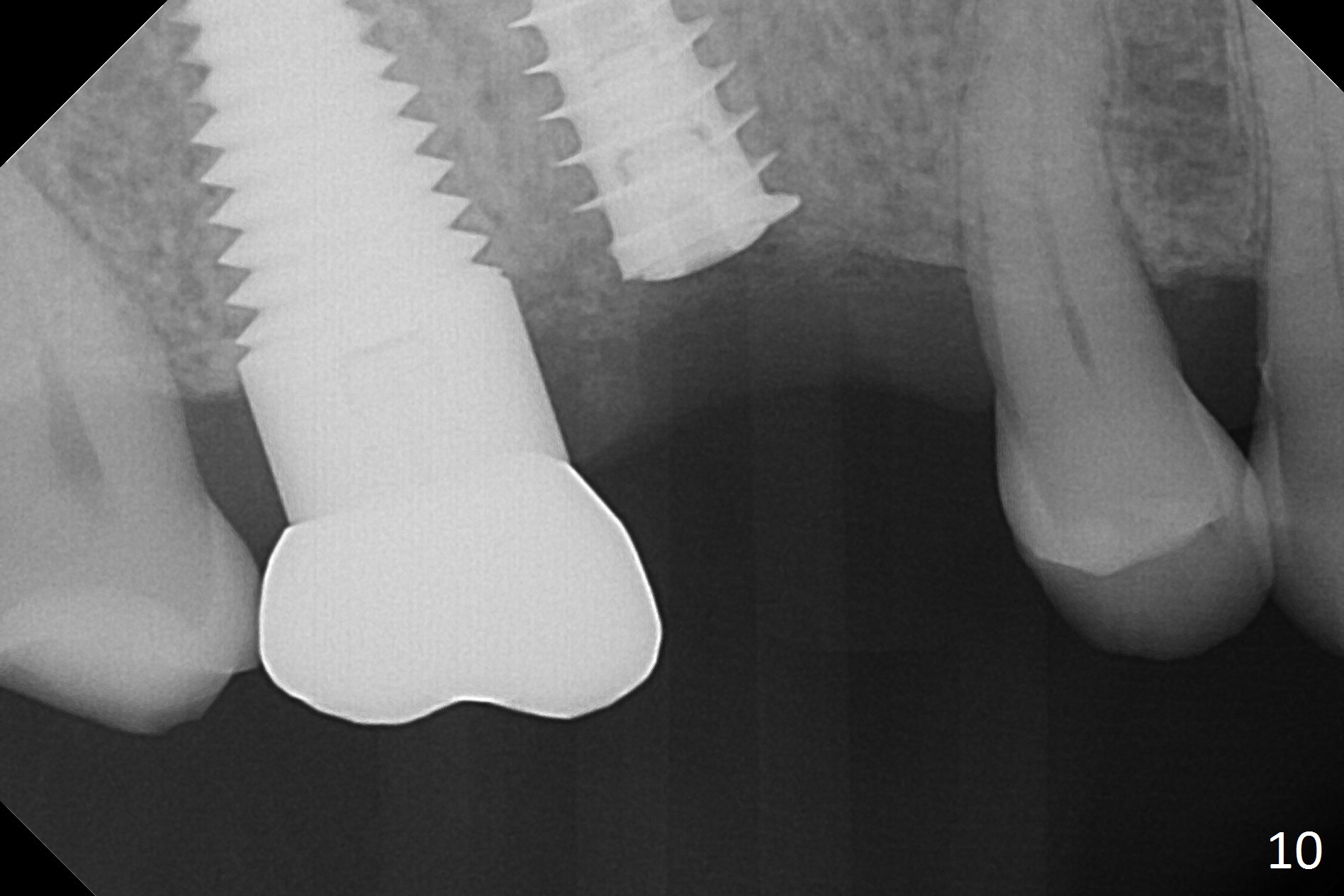
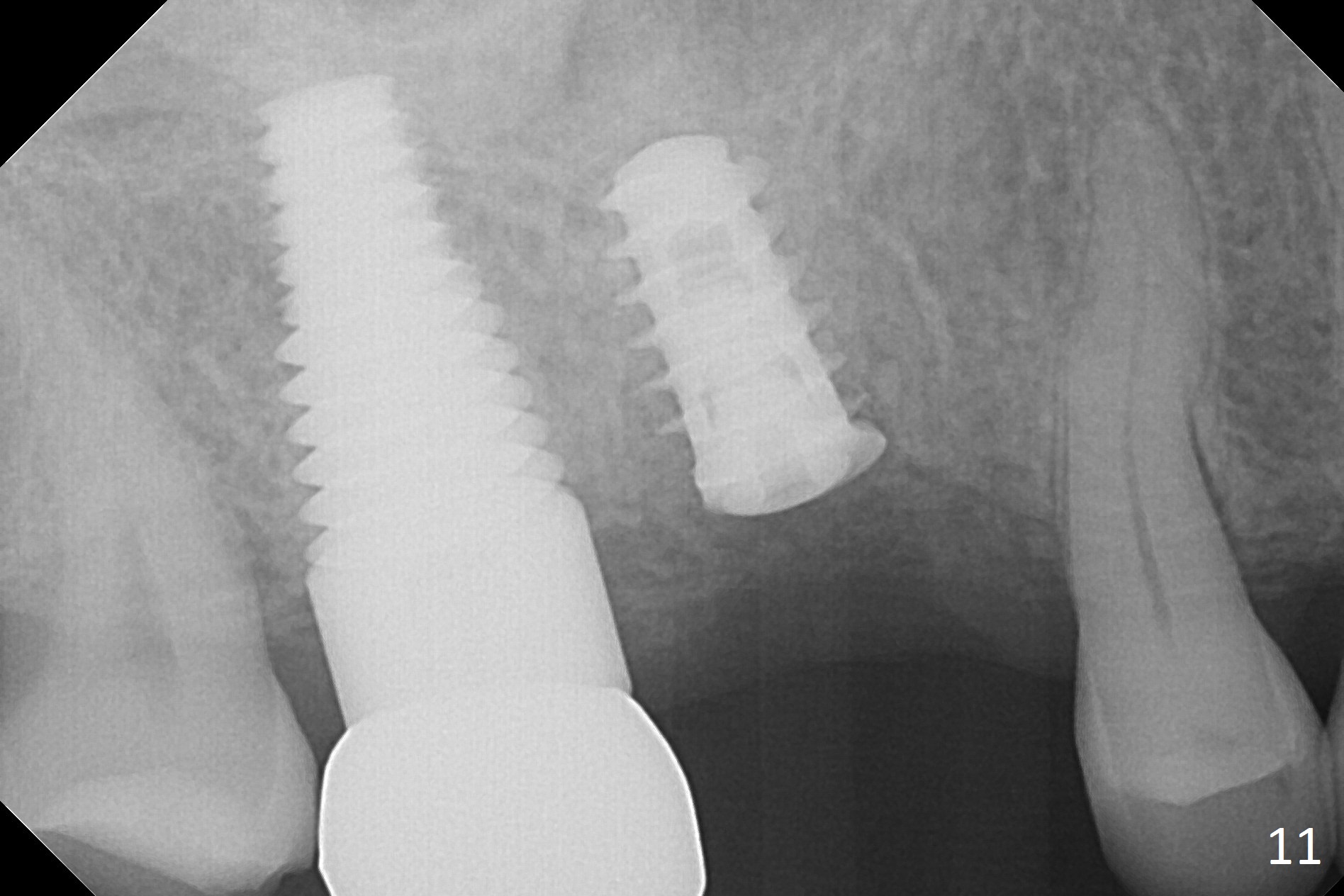
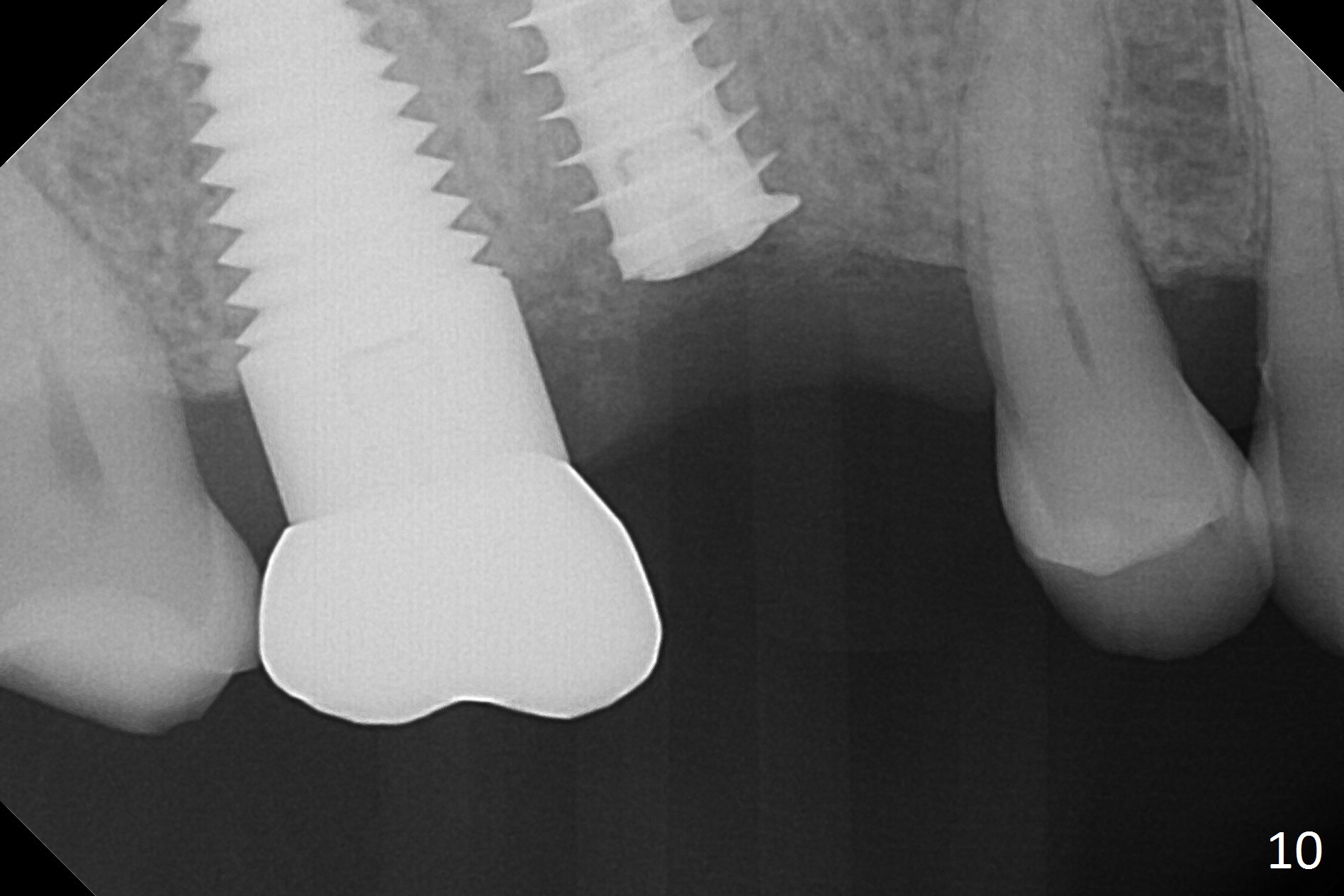
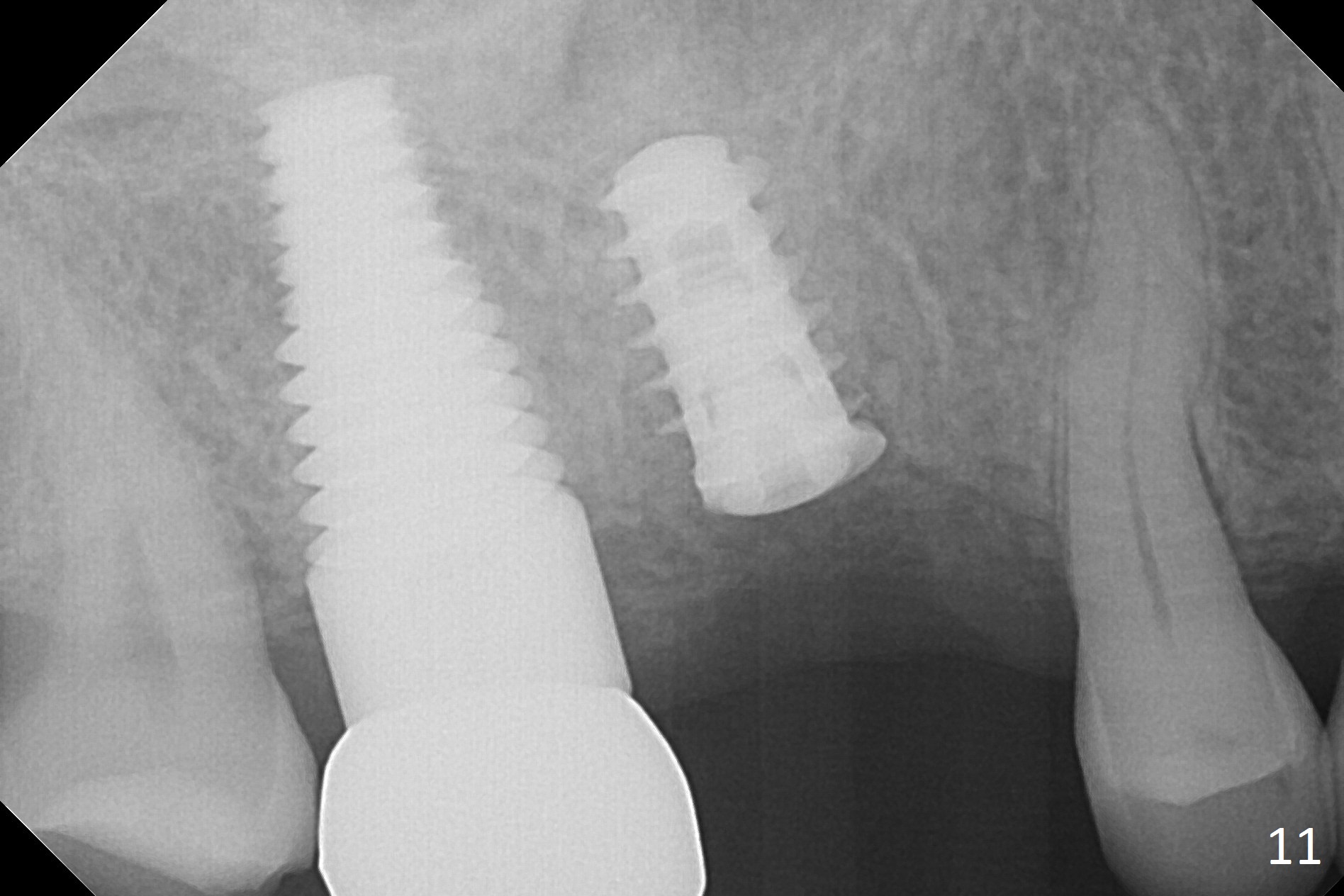
In fact, local anesthesia is required to remove the healing abutment. The gingival cuff is apparently healthy. The implant does not turn when torque reaches 45 Ncm. After placing a healing screw, PAs seem to show that the implant is osteointegrating (Fig.10,11).
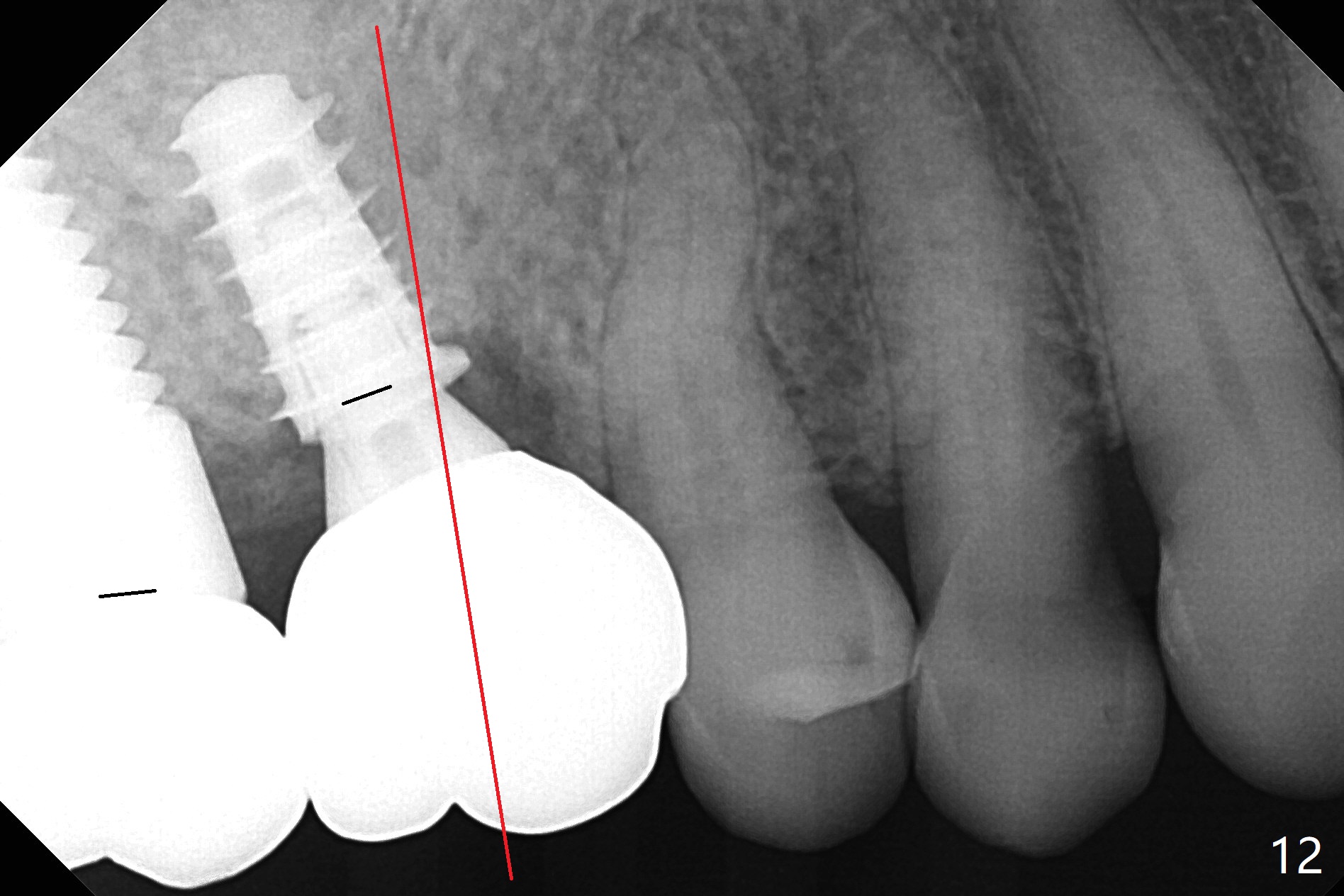
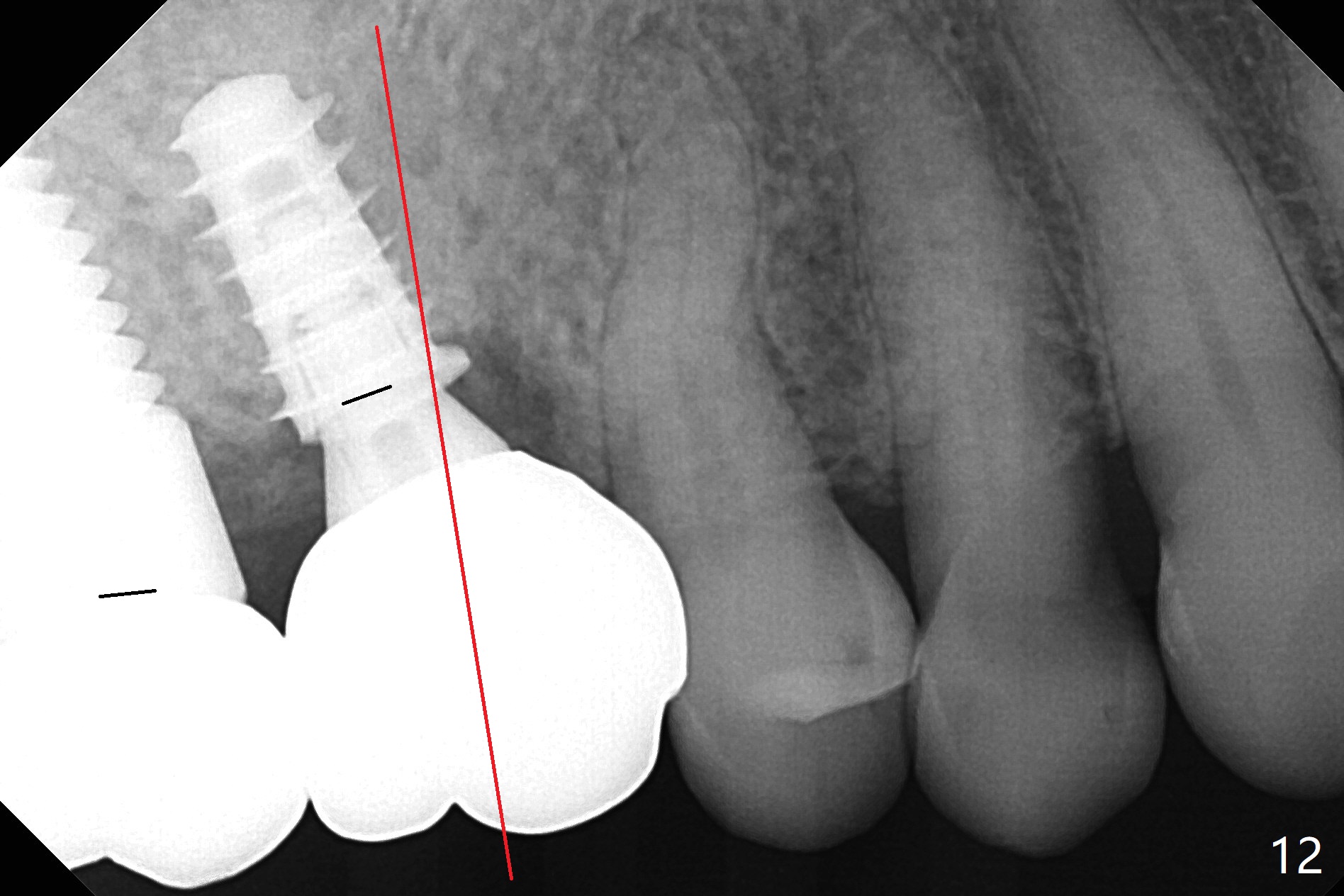
The abutment screw is loose 2.5 months post cementation (Fig.12), but the bone density in the previous mesiobuccal and distobuccal sockets increases. The patient chews crab leg. The other two contributing factors to screw loosening are poor trajectory (as compared to the long axis (red line)) and poor crown/implant ratio associated with the bone-level implant as compared to that in the tissue-level one (at #2). It appears appropriate to choose the latter for a bruxer. Take PA as early as possible in osteotomy to determine trajectory.
Return to
Upper
Molar Immediate Implant, Prevent
Molar Periimplantitis (Protocols,
Table),
Advantage of Tissue-Level Implant
2
Xin Wei, DDS, PhD, MS 1st edition 12/29/2016, last revision 01/19/2018