










 |
 |
 |
 |
 |
||
 |
 |
 |
 |
 |
 |
|
 |
 |
 |
 |
|||
 |
 |
 |
 |
|||
 |
 |
 |
||||
Repair the Lingual Plate Defect Prior to Immediate Implantation and Early Provisional
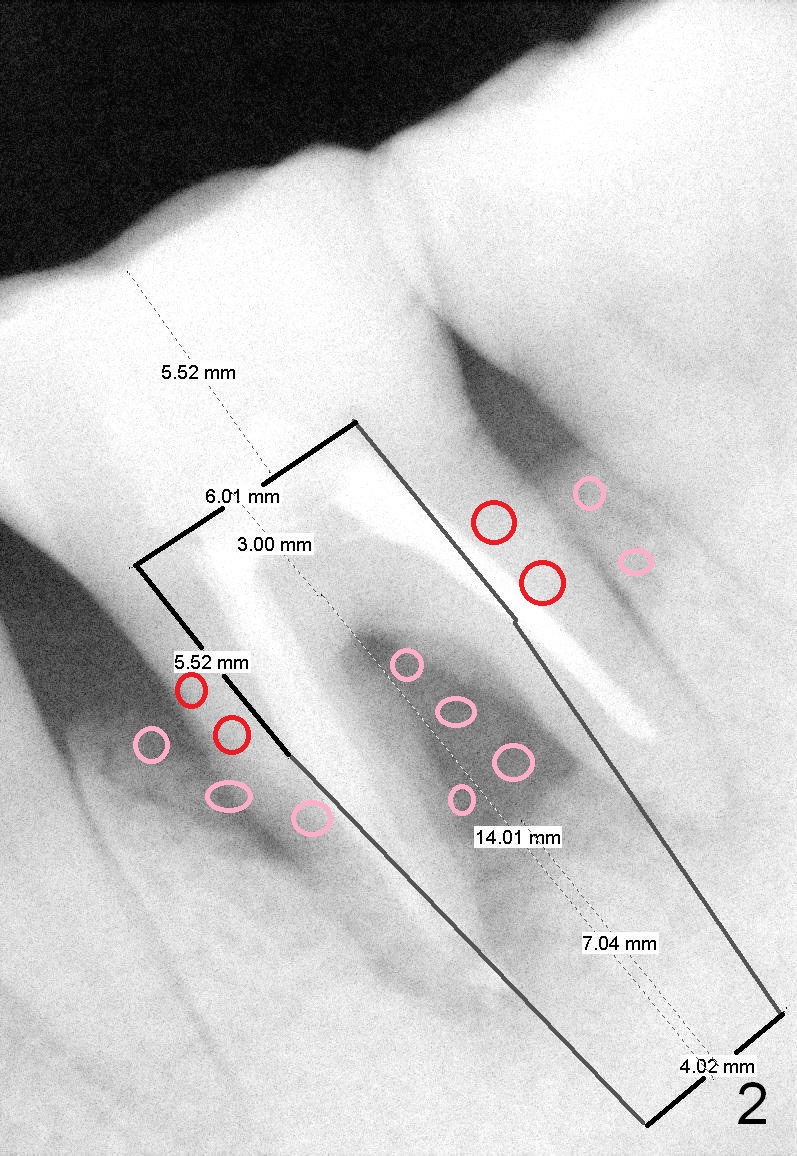
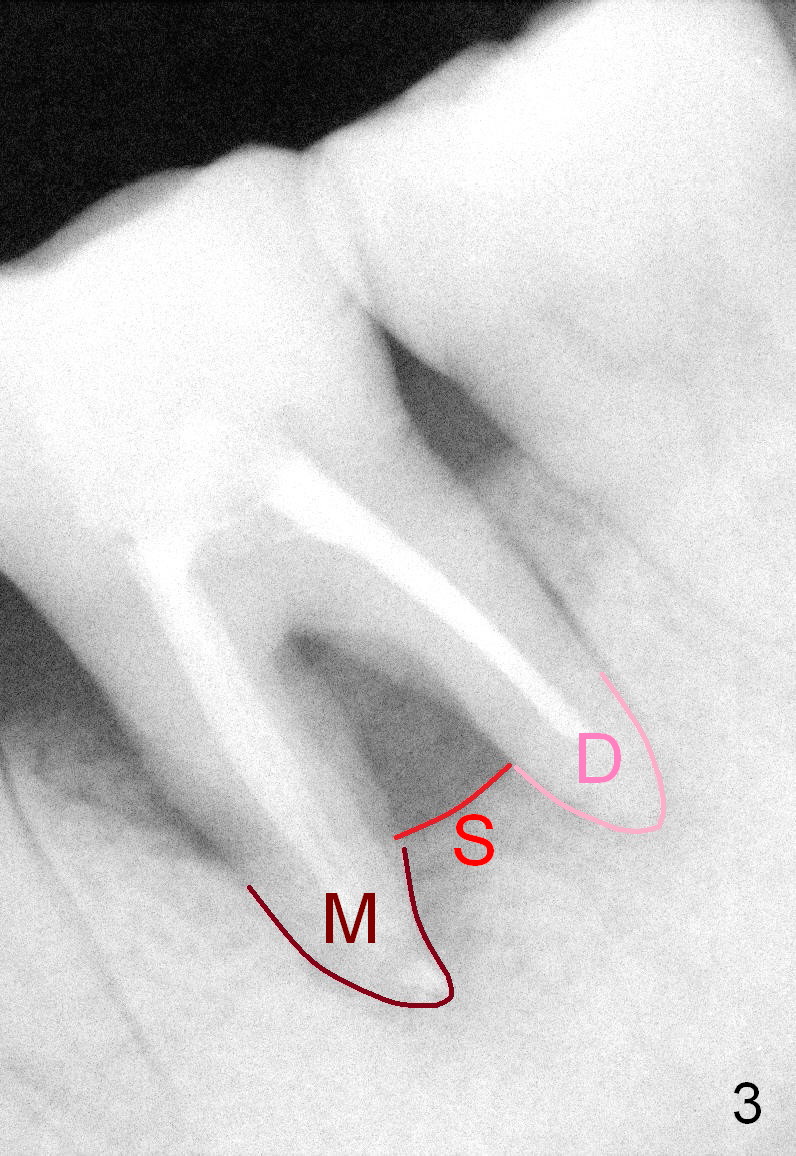
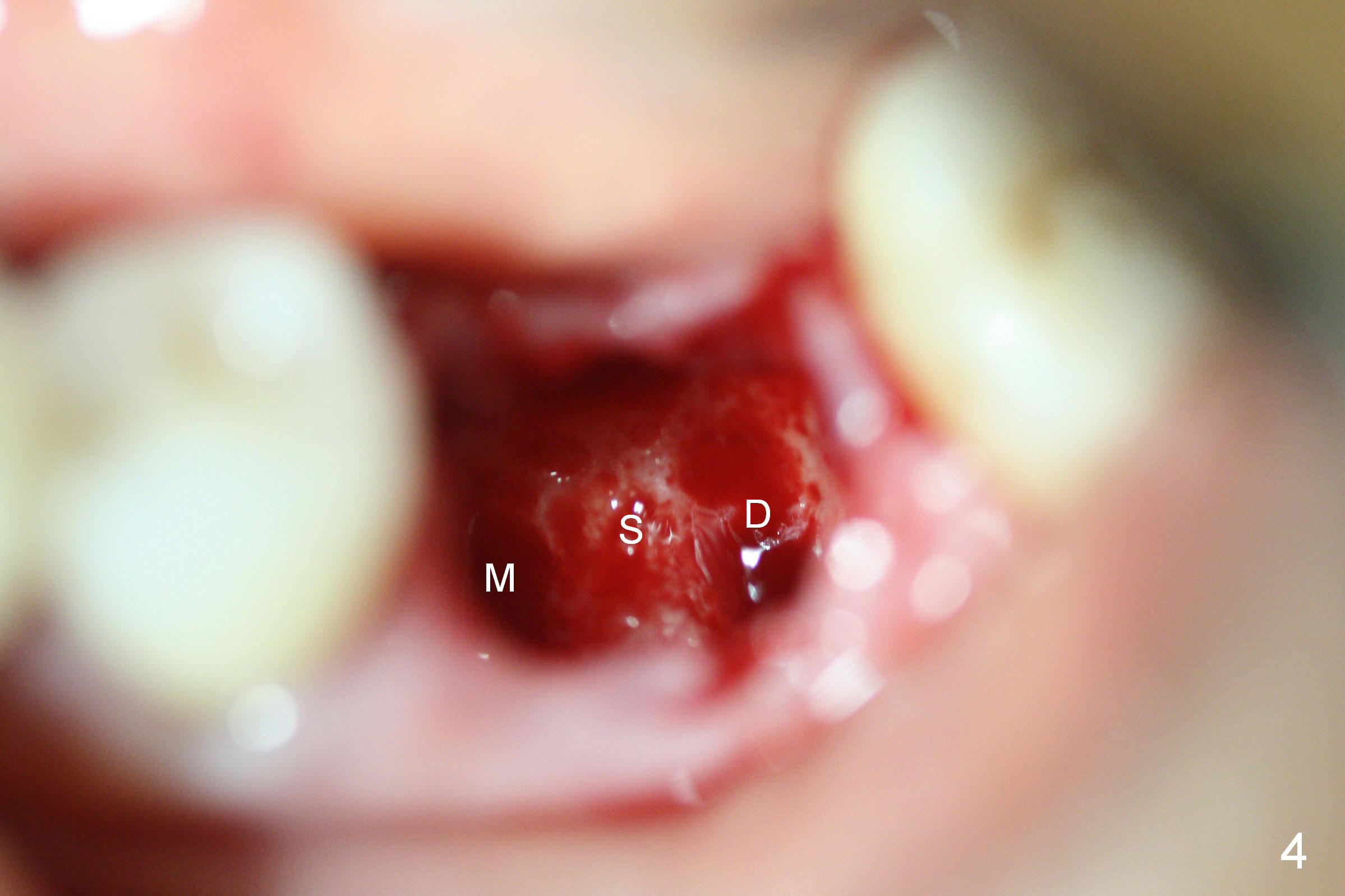
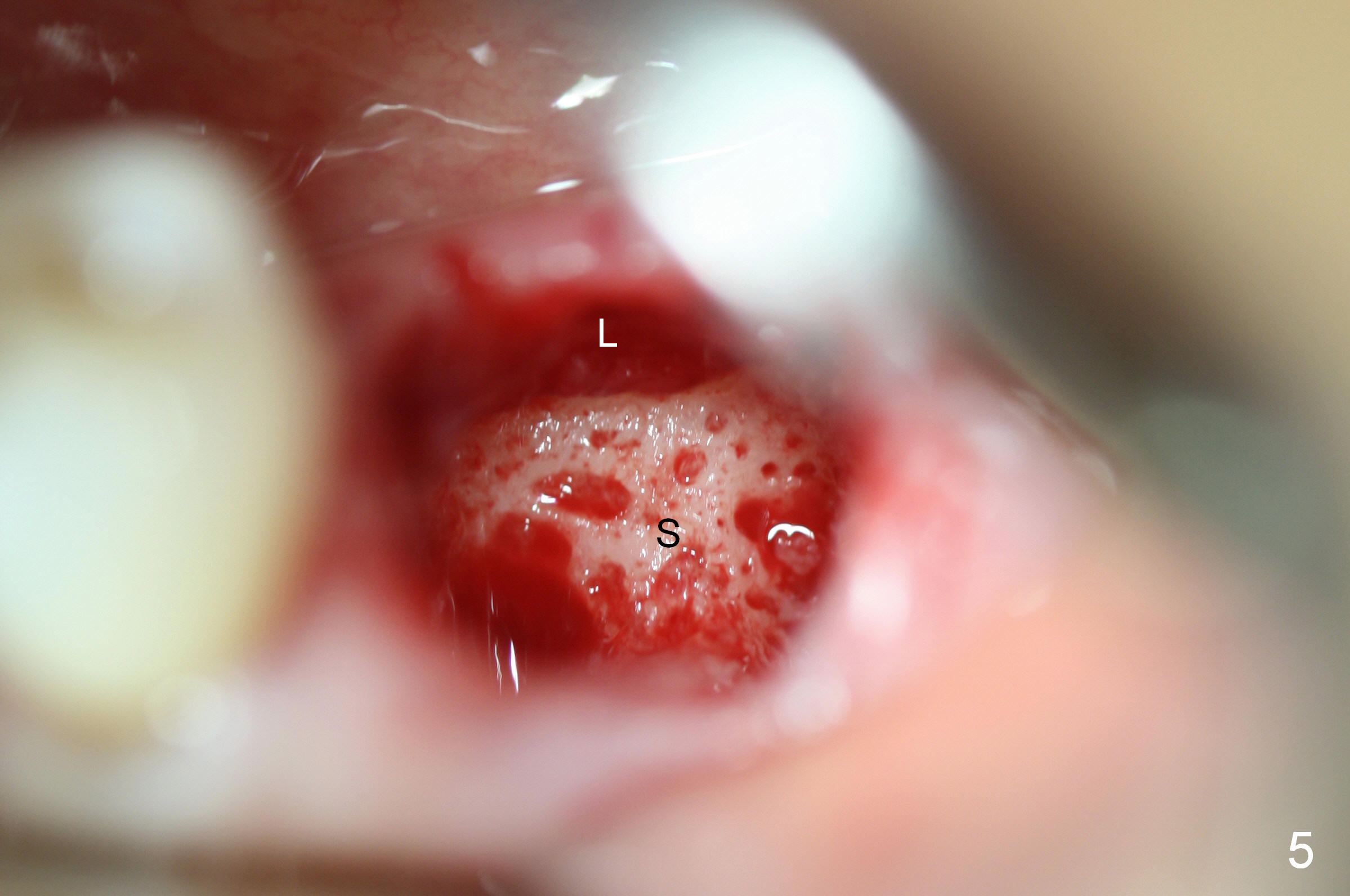
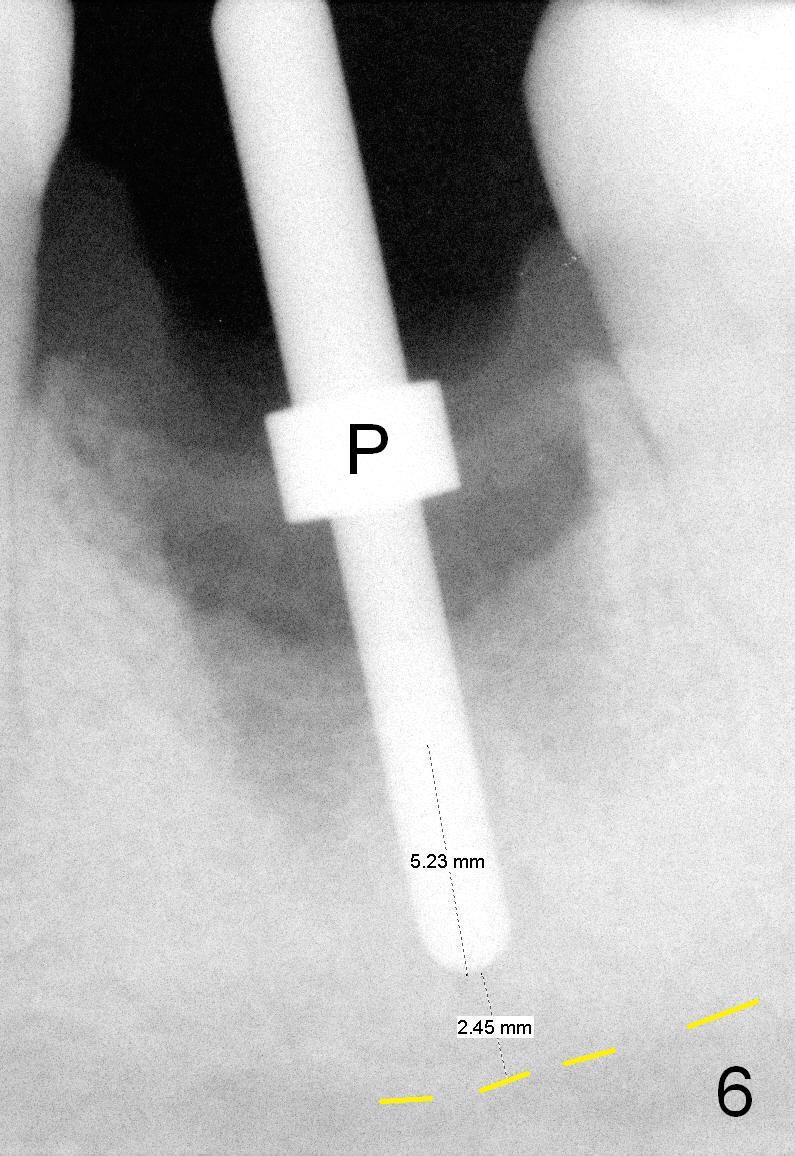
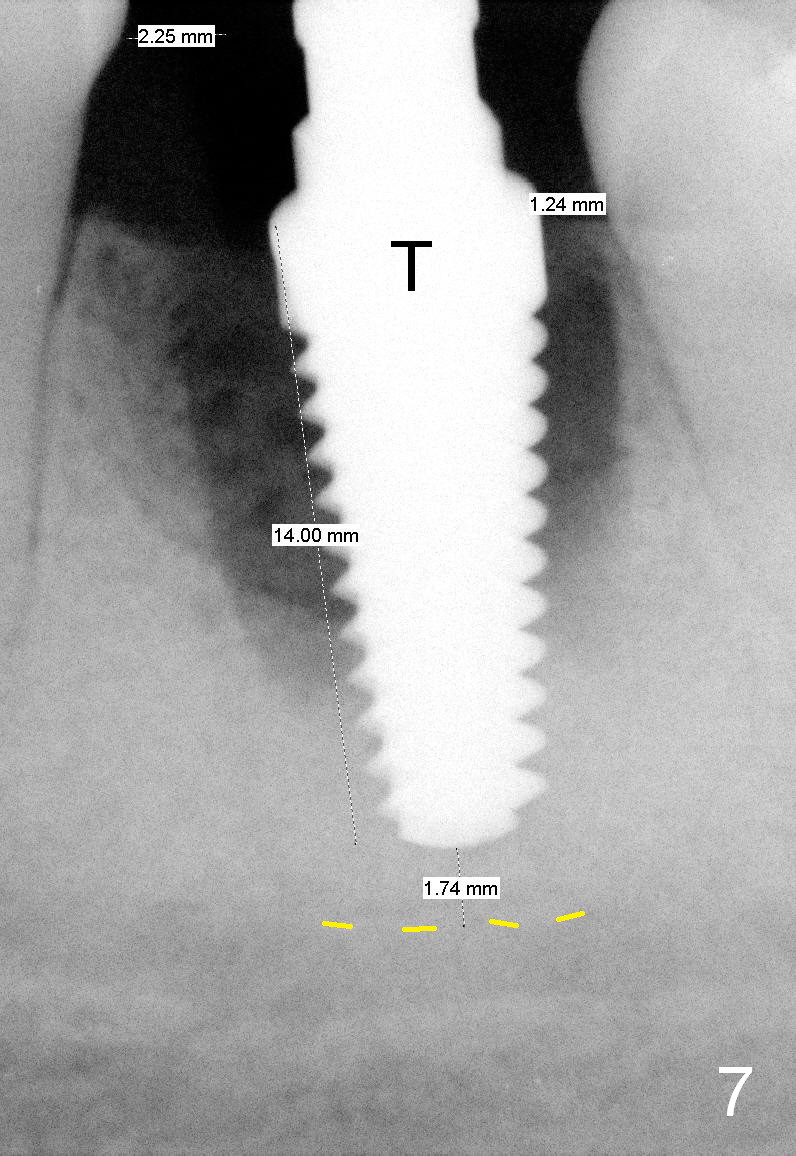
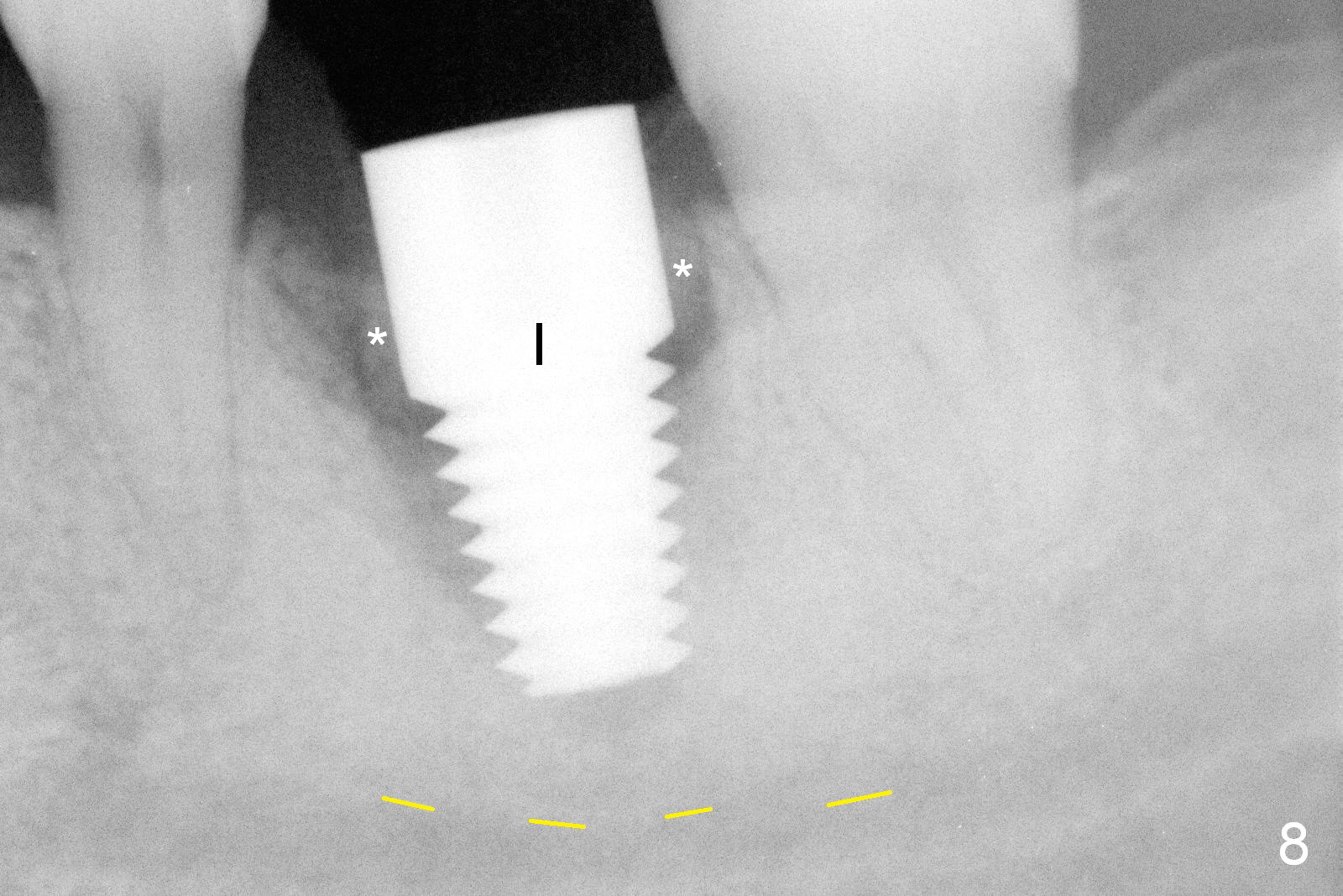
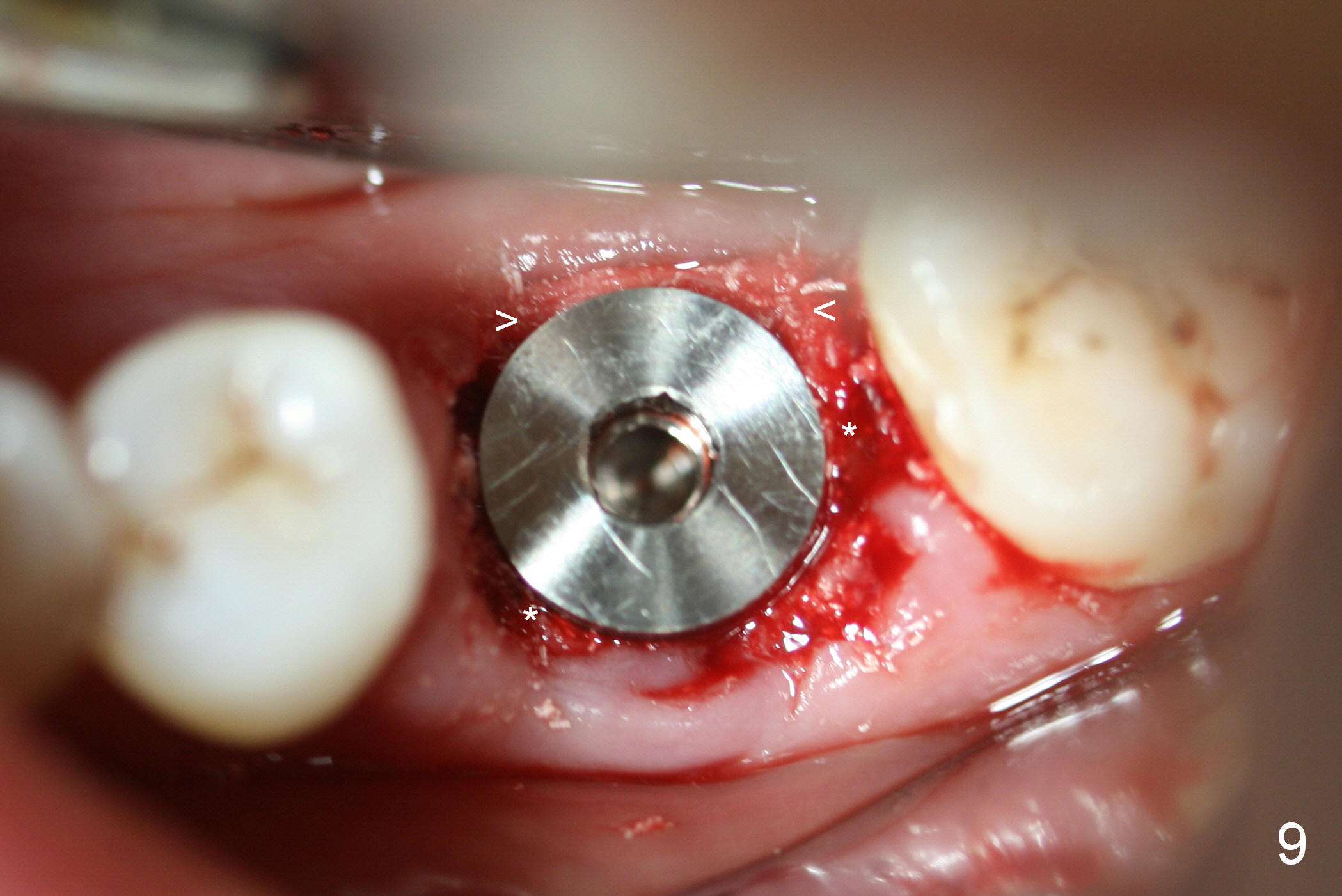
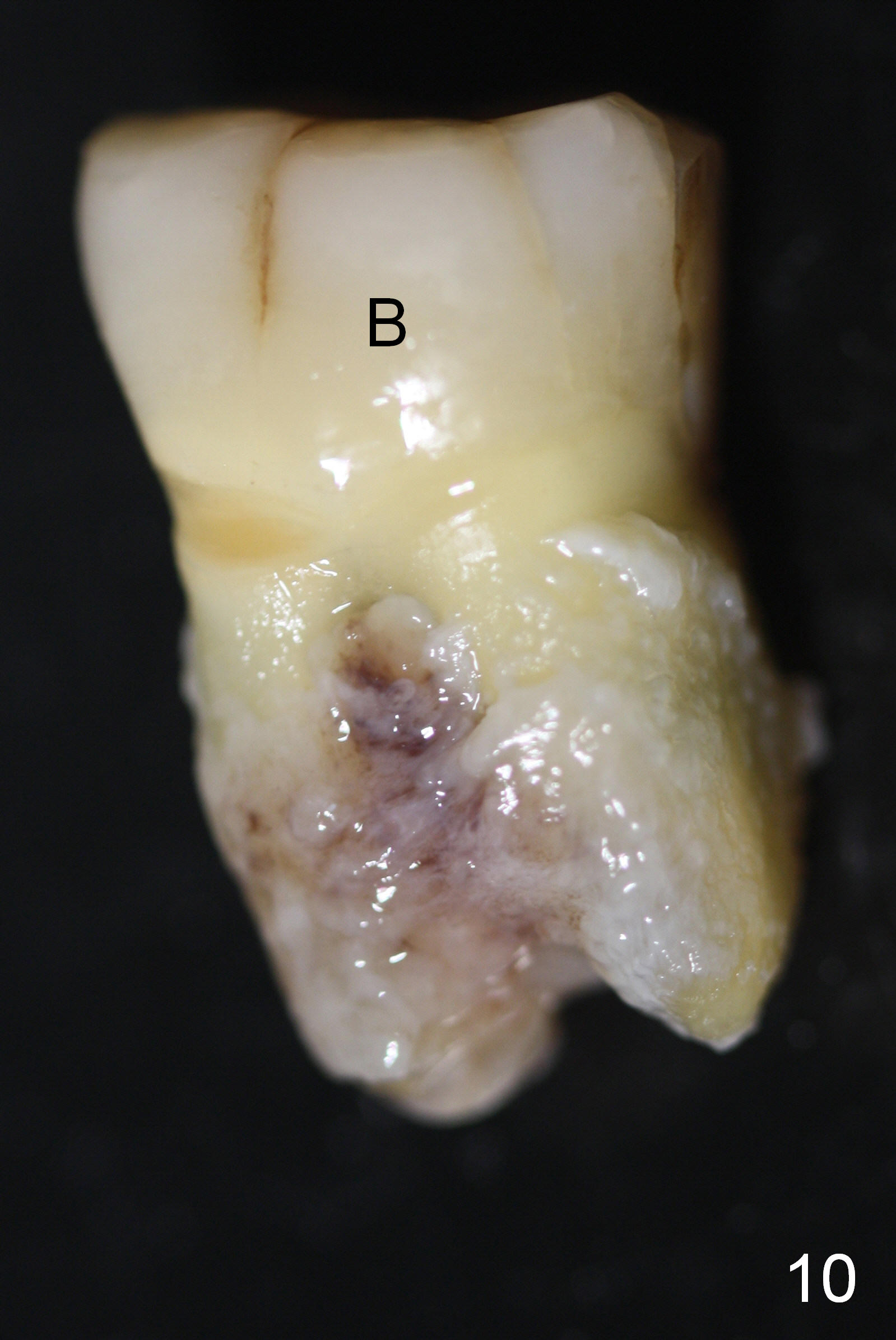
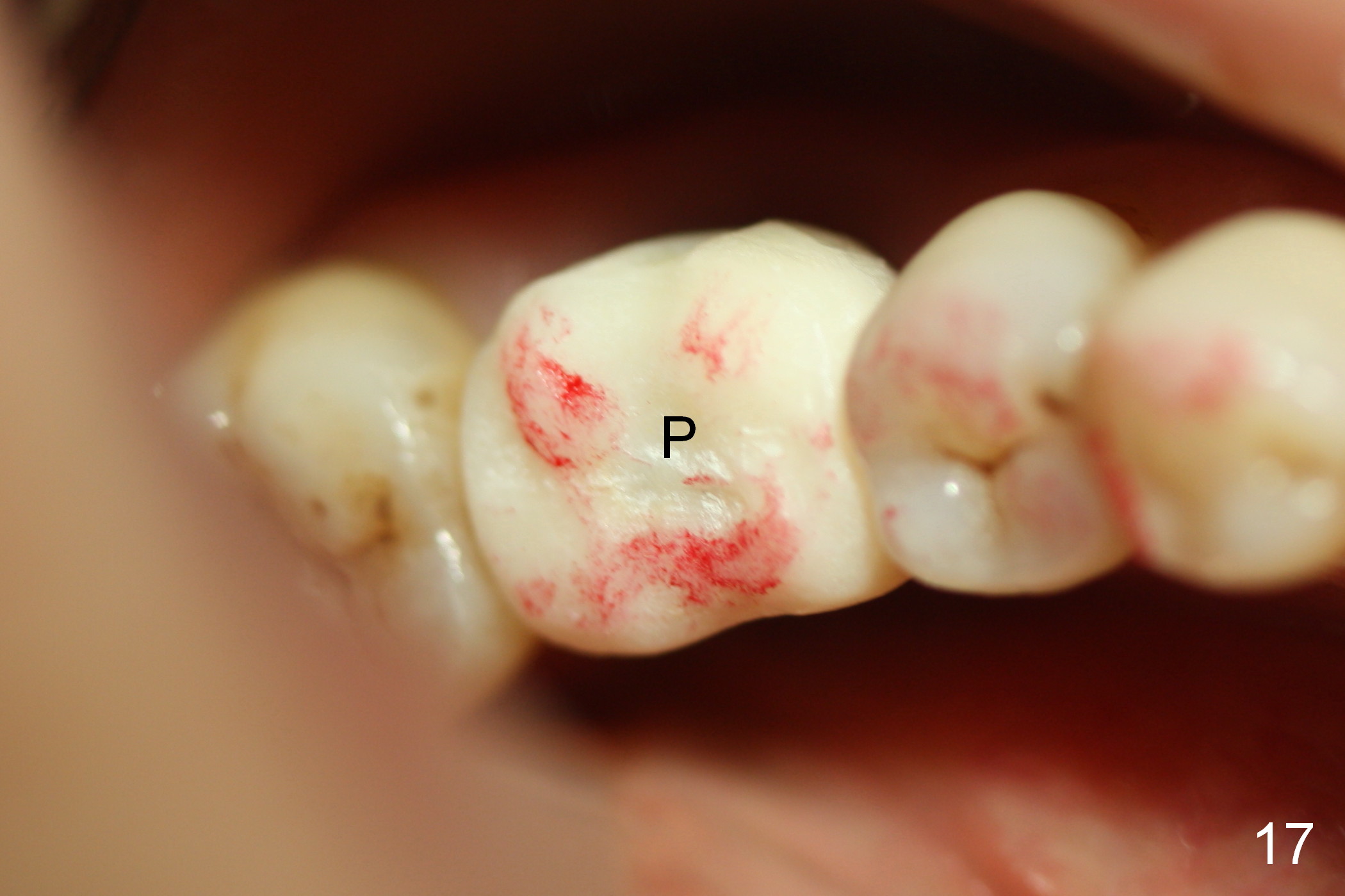
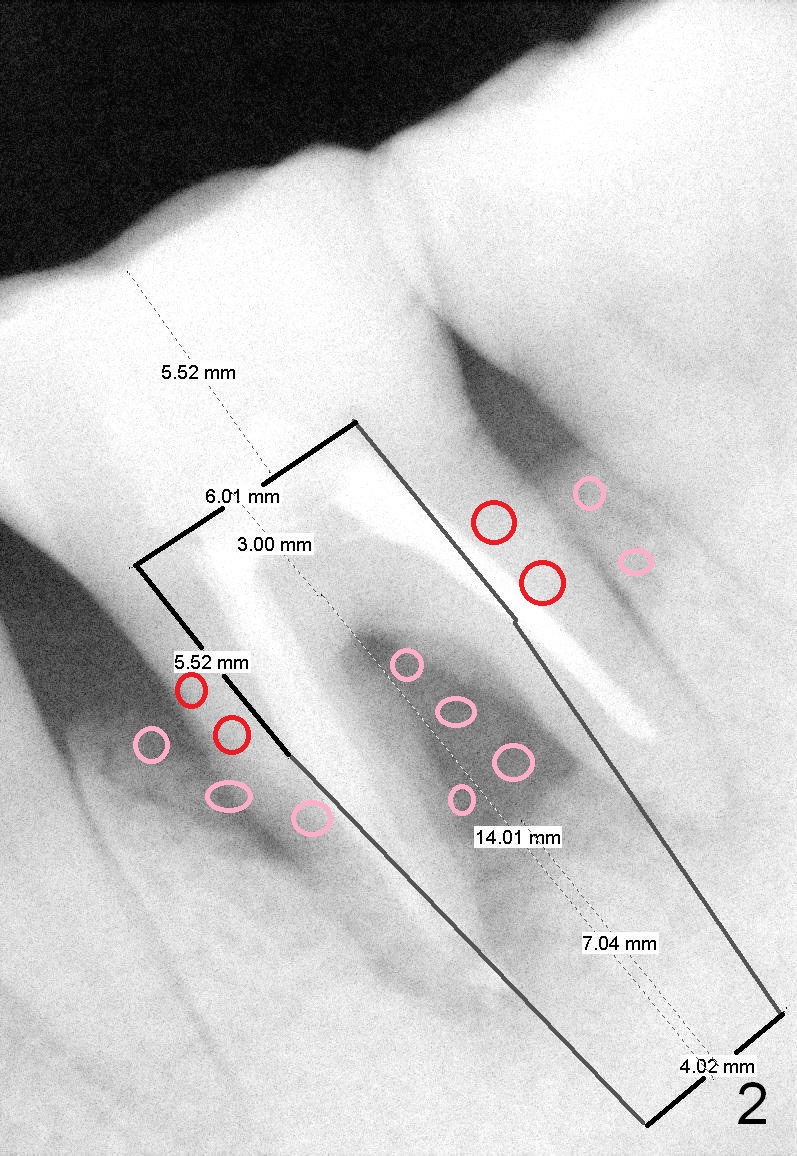
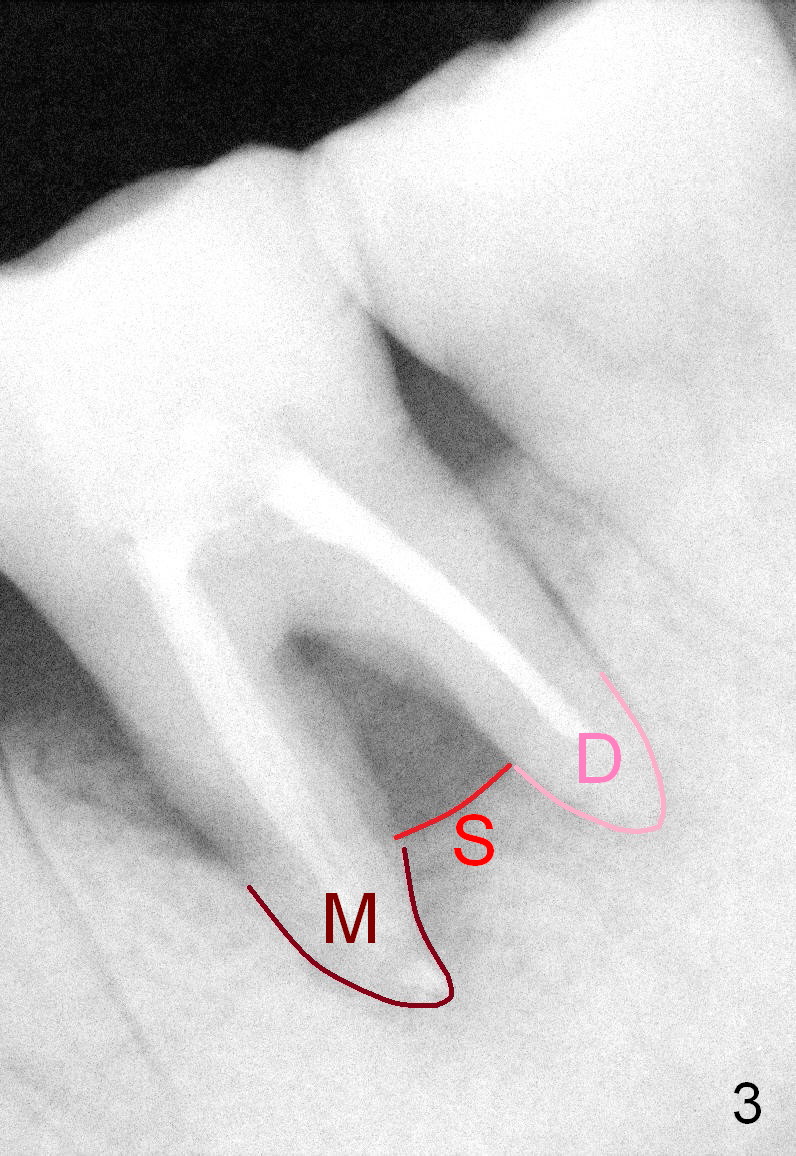
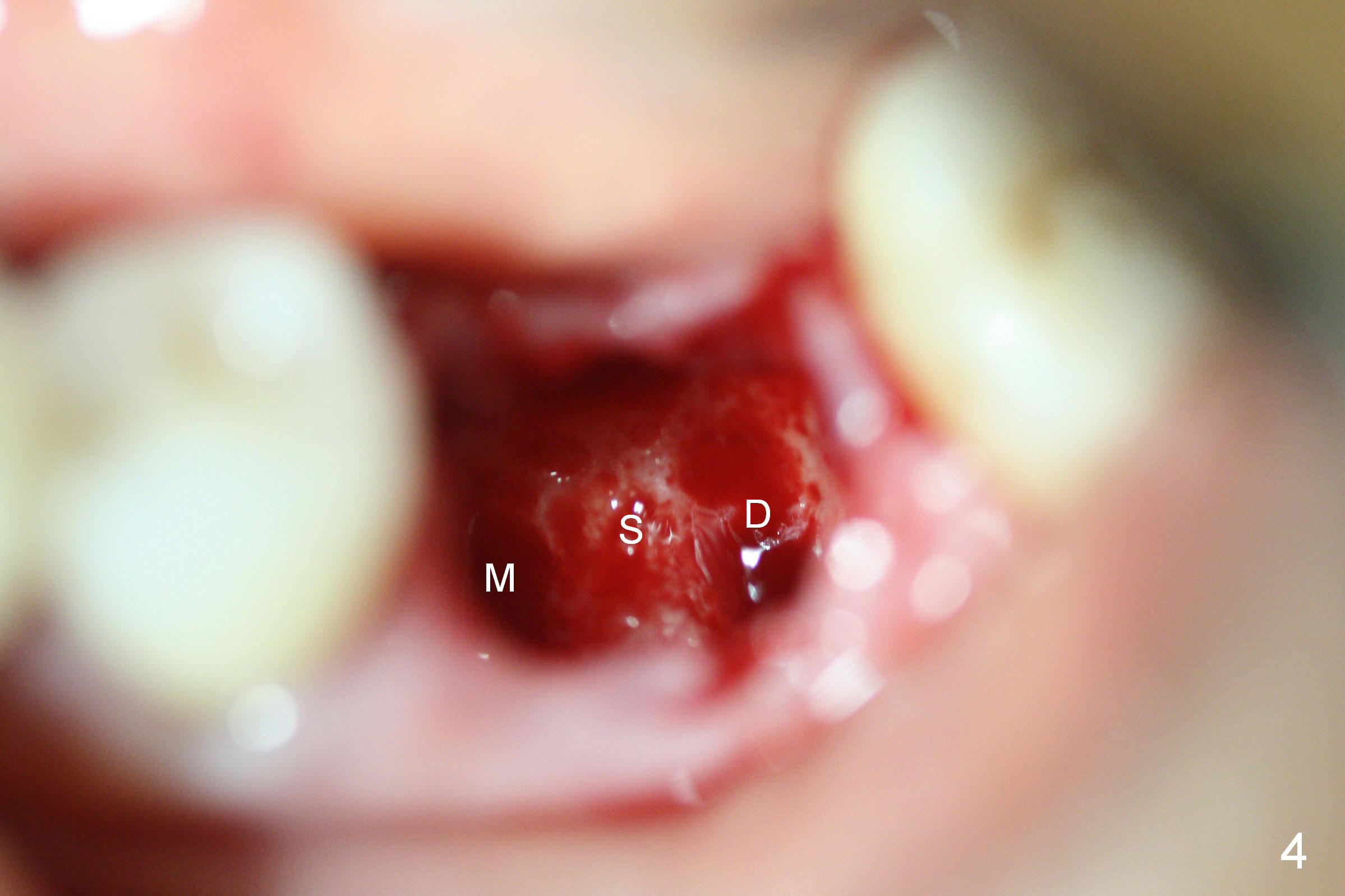
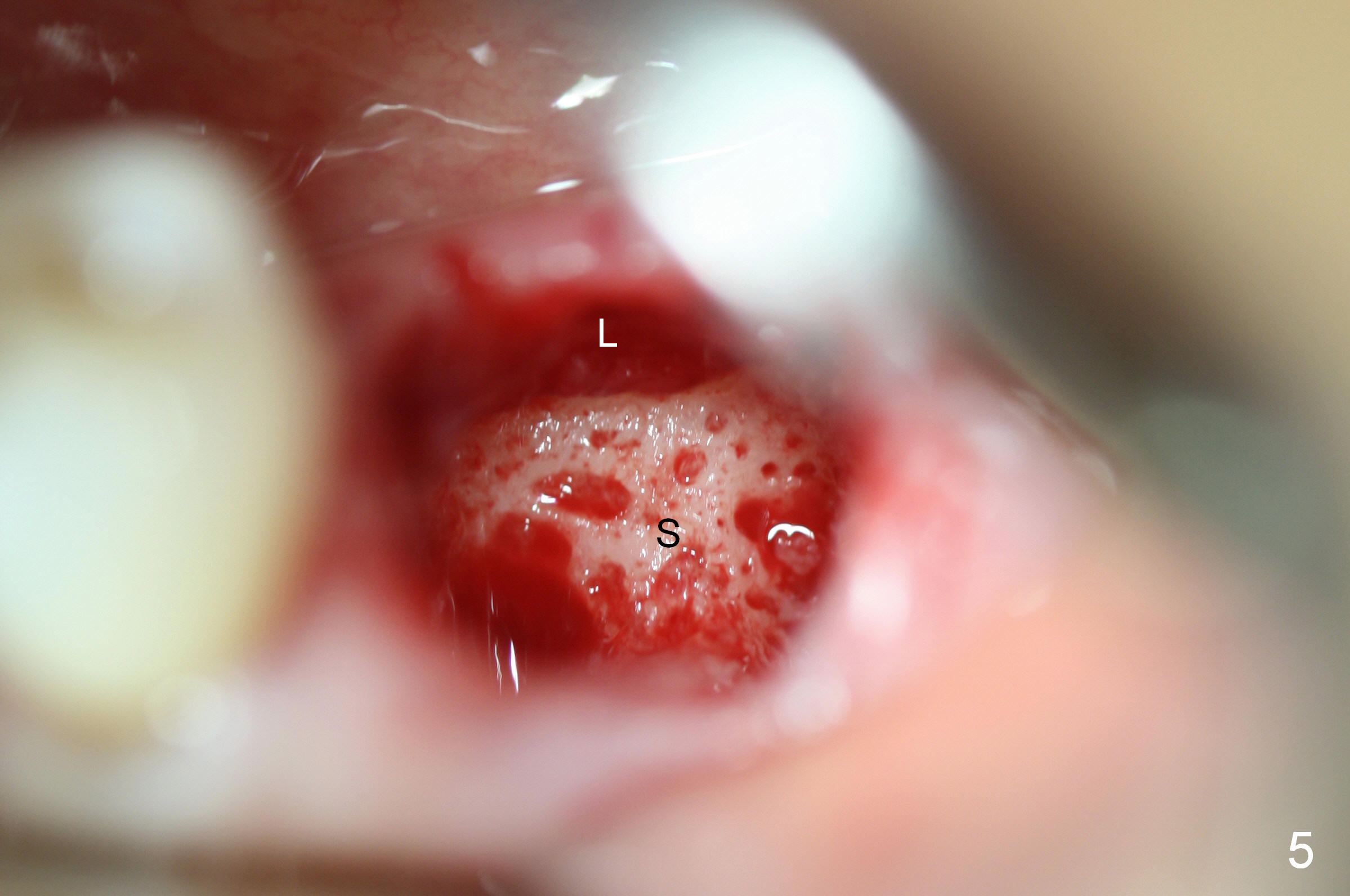
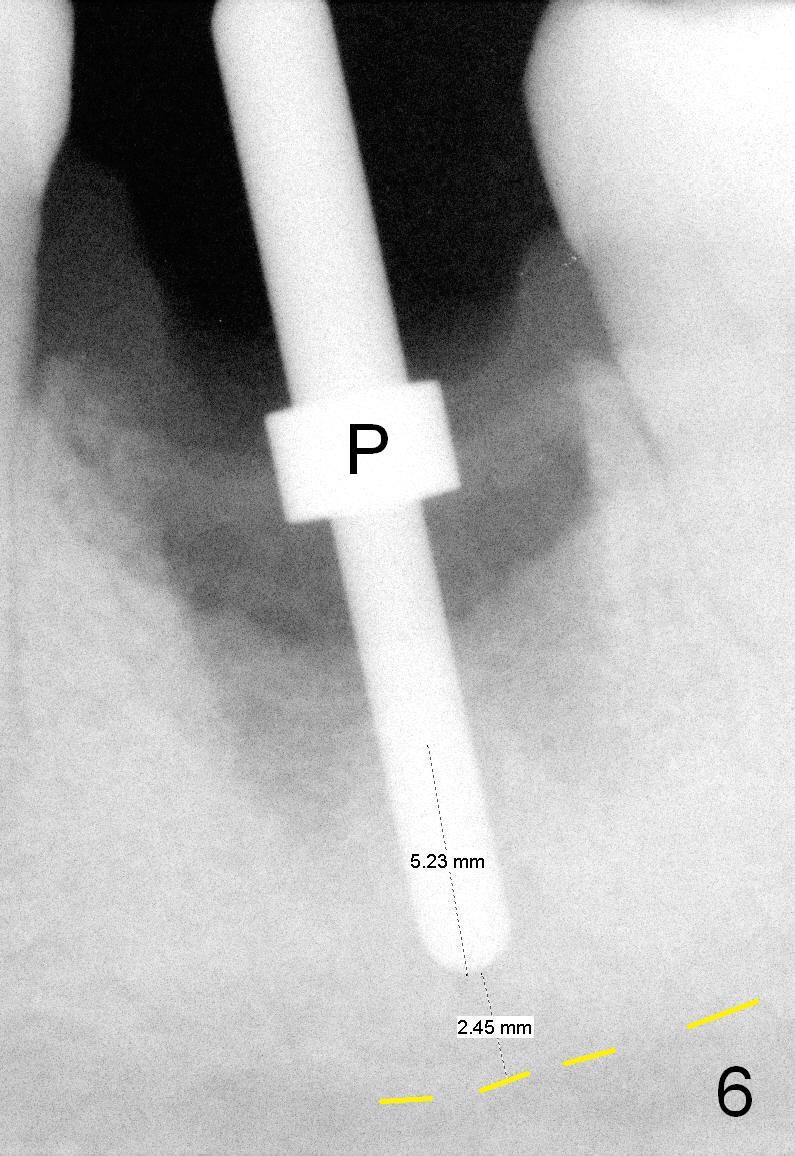
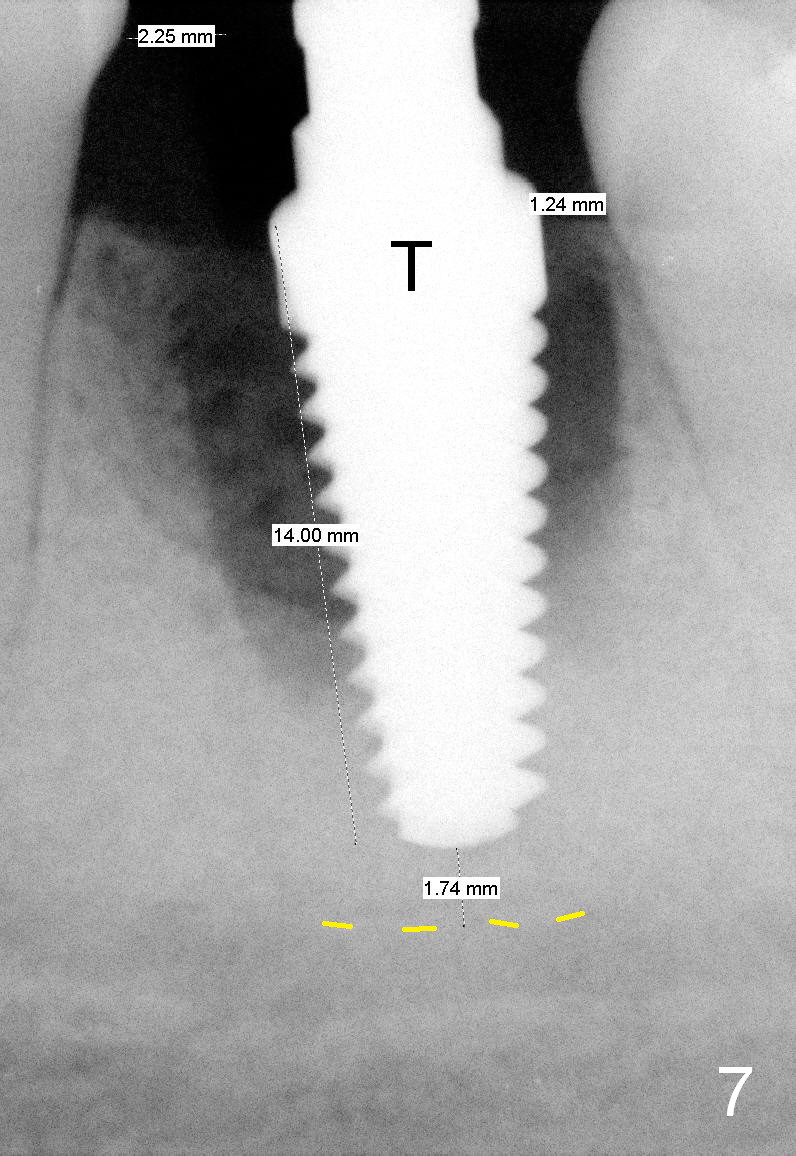
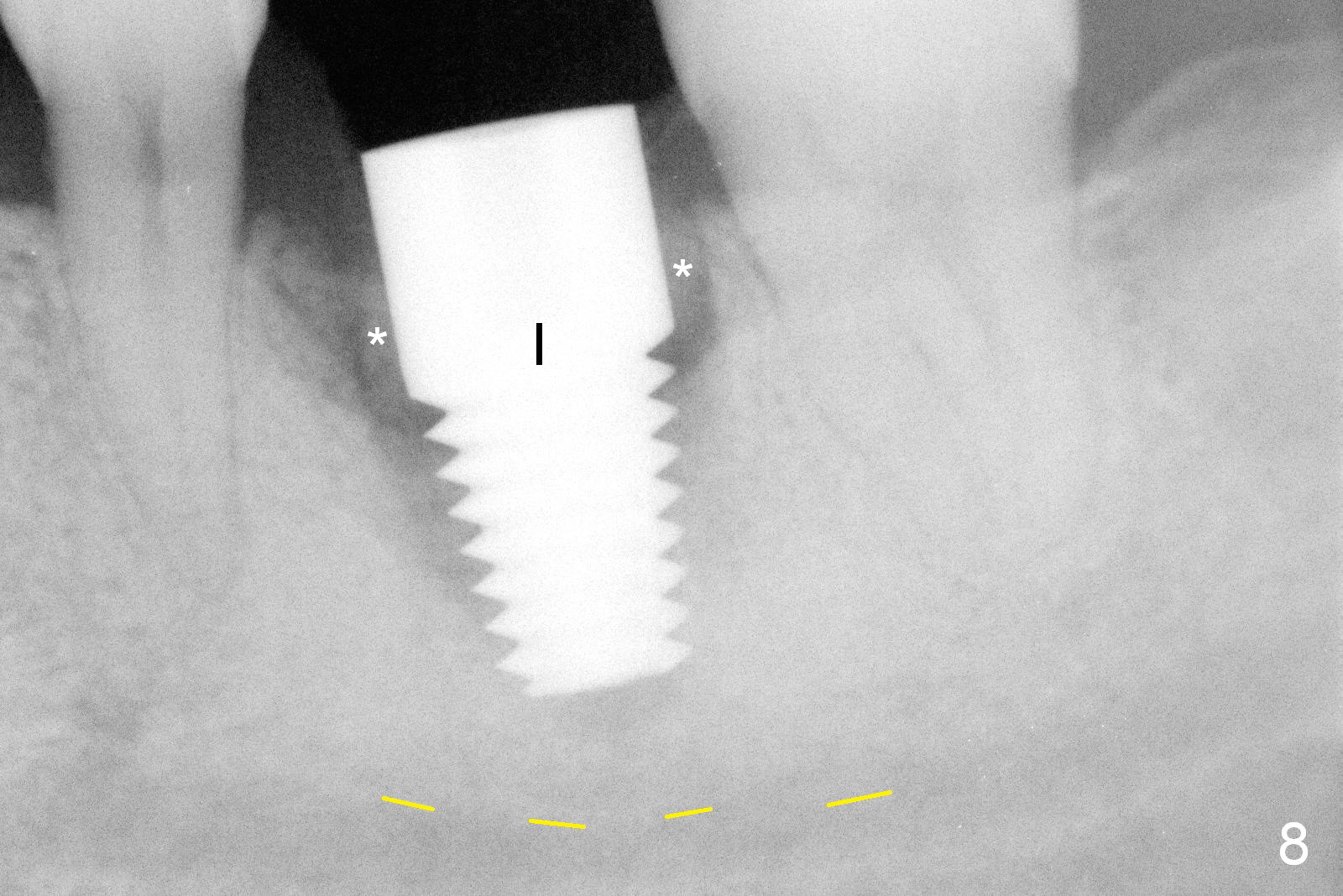
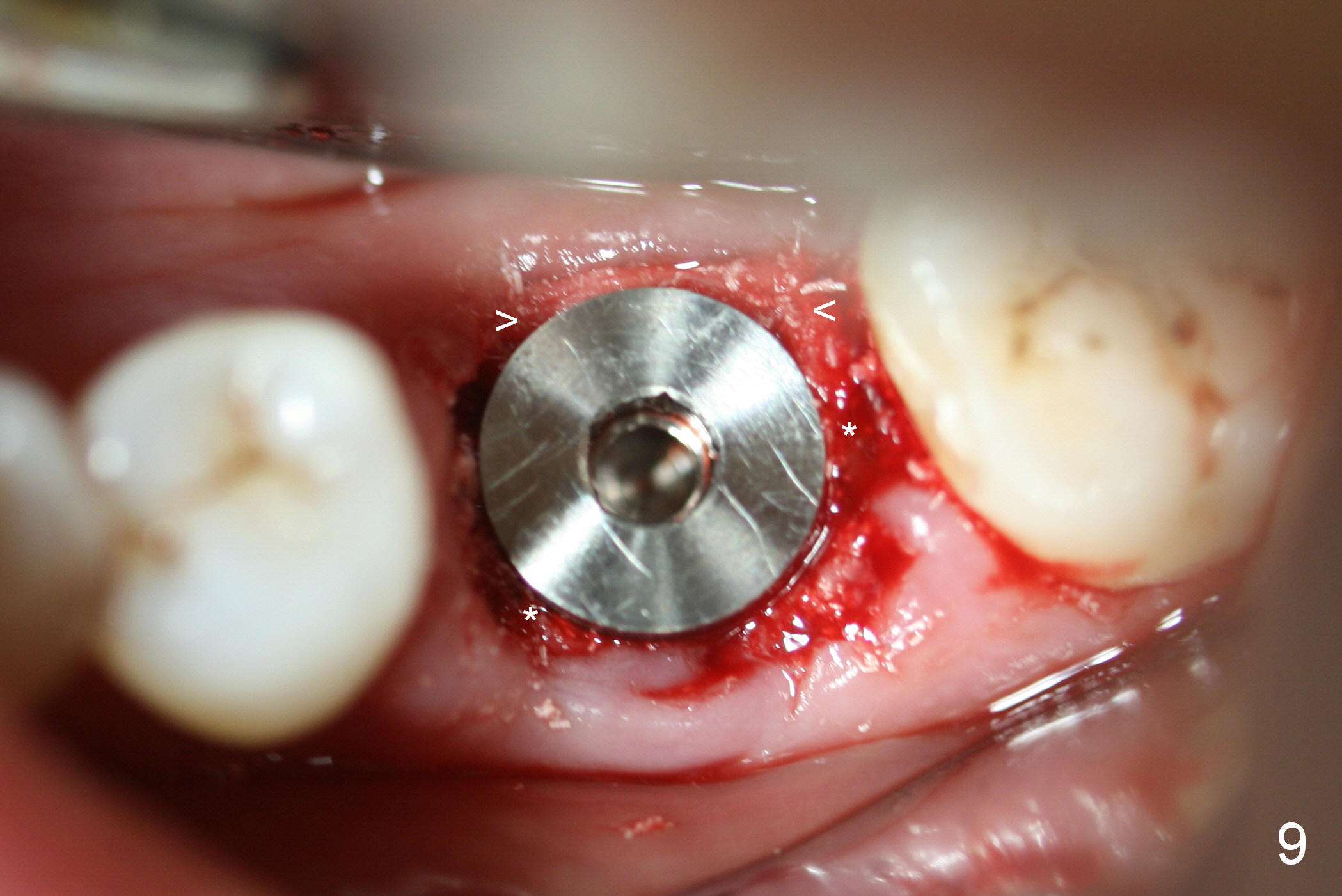
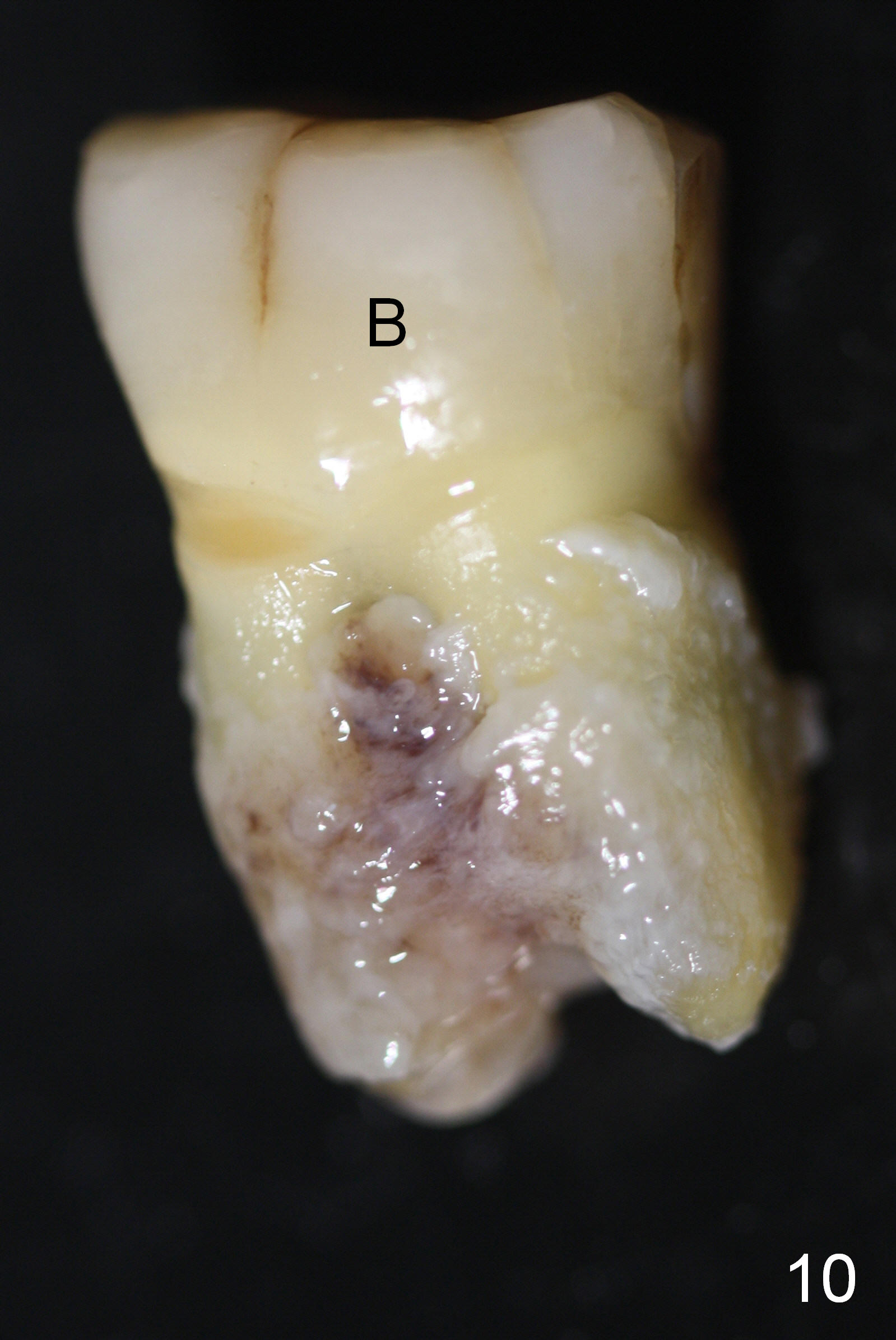
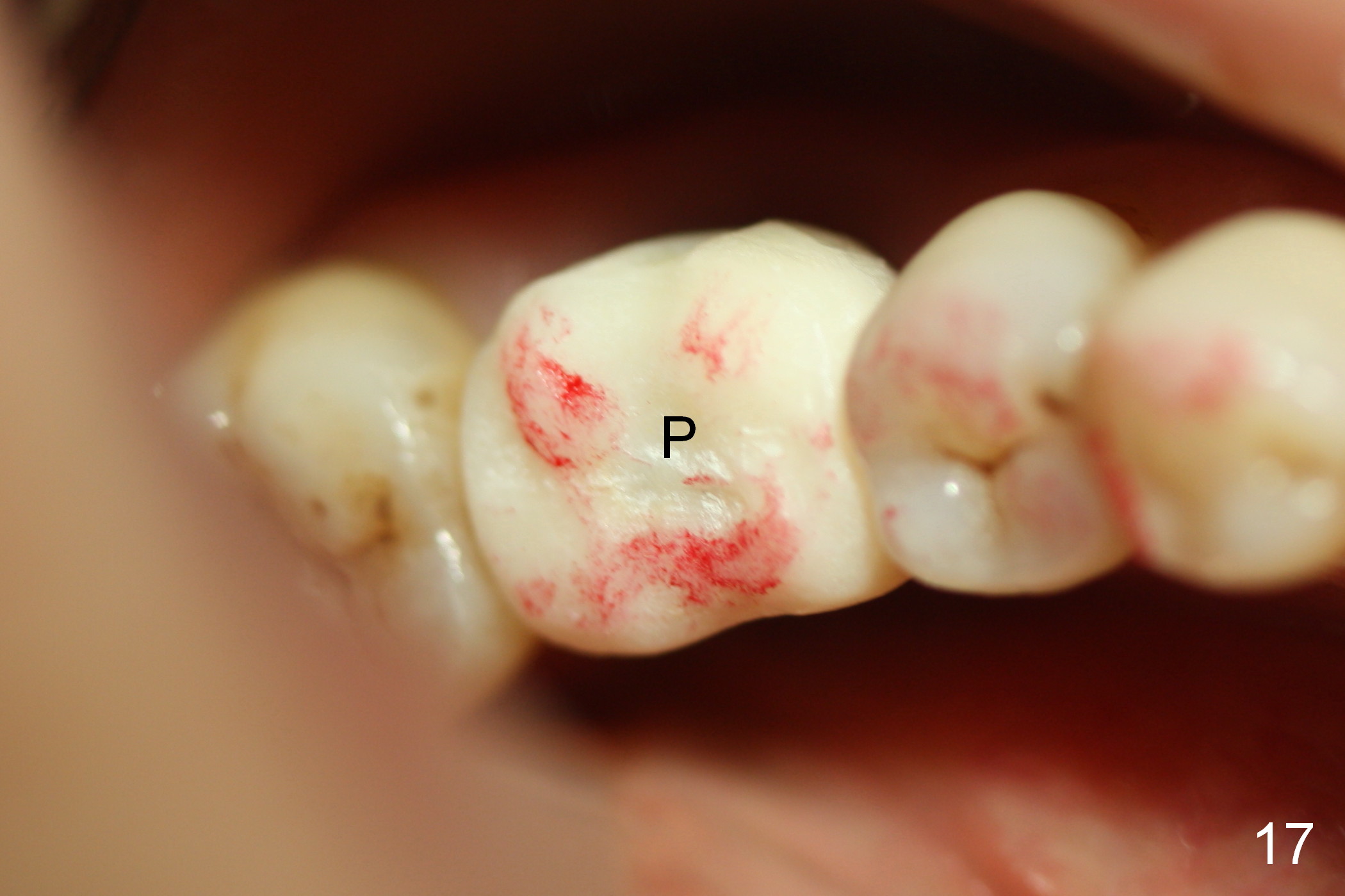
When the patient returns for #19 immediate implant, the lingual furca pocket is deeper than the buccal with lingual purulent discharge. Immediate preop PA confirms large furca radiolucency (Fig.1 *). Tentative size of the implant is 6x14 mm with ~ 7 mm in new bone (septum; Fig.2). The septum is low, and flat (Fig.3 red line, S), while the mesial and distal sockets are shallow (brown (M) and pink (D) outlines). These X-ray findings are consistent with clinical ones when the tooth is extracted (Fig.4,5). In fact the lingual plate is absent. After removal of granulation tissue lingually, the osteotomy starts in the septum, more buccal, with a 2 mm pilot drill. PA is taken with a parallel pin (Fig.6 P). The osteotomy is sequentially enlarged with reamers, followed by insertion of taps (Fig.7: 6x17 mm (14 mm deep)). Prior to placement of a 7x14 mm implant (Fig.8 I: >60 Ncm), a piece of Osteotape (collagen membrane saturated with Osteogen, a type of Hydroxyapaptite) is placed against the lingual defect, followed by bone graft lingually. More bone graft is placed in the peri-implant gaps (Fig.8,9 *). The extracted tooth is examined postop (Fig.10 (buccal), 11 (lingual)). Considering the large lingual defect, perio dressing is placed after insertion of an abutment. In this case, it appears that the perio dressing offers better wound protection than an immediate provisional. Fig.12-14 show the perio dressing 1 week postop. It is dislodged 3 days later. Although there is more implant exposure lingually (Fig.15) than buccally (Fig.16), there is no sign of inflammation 4 weeks postop. To prevent the adjacent and opposing teeth from drifting during osteointegration, an early provisional is fabricated with minimal occlusal contact (Fig.17-19). The patient is advised not to chew on the affected side.
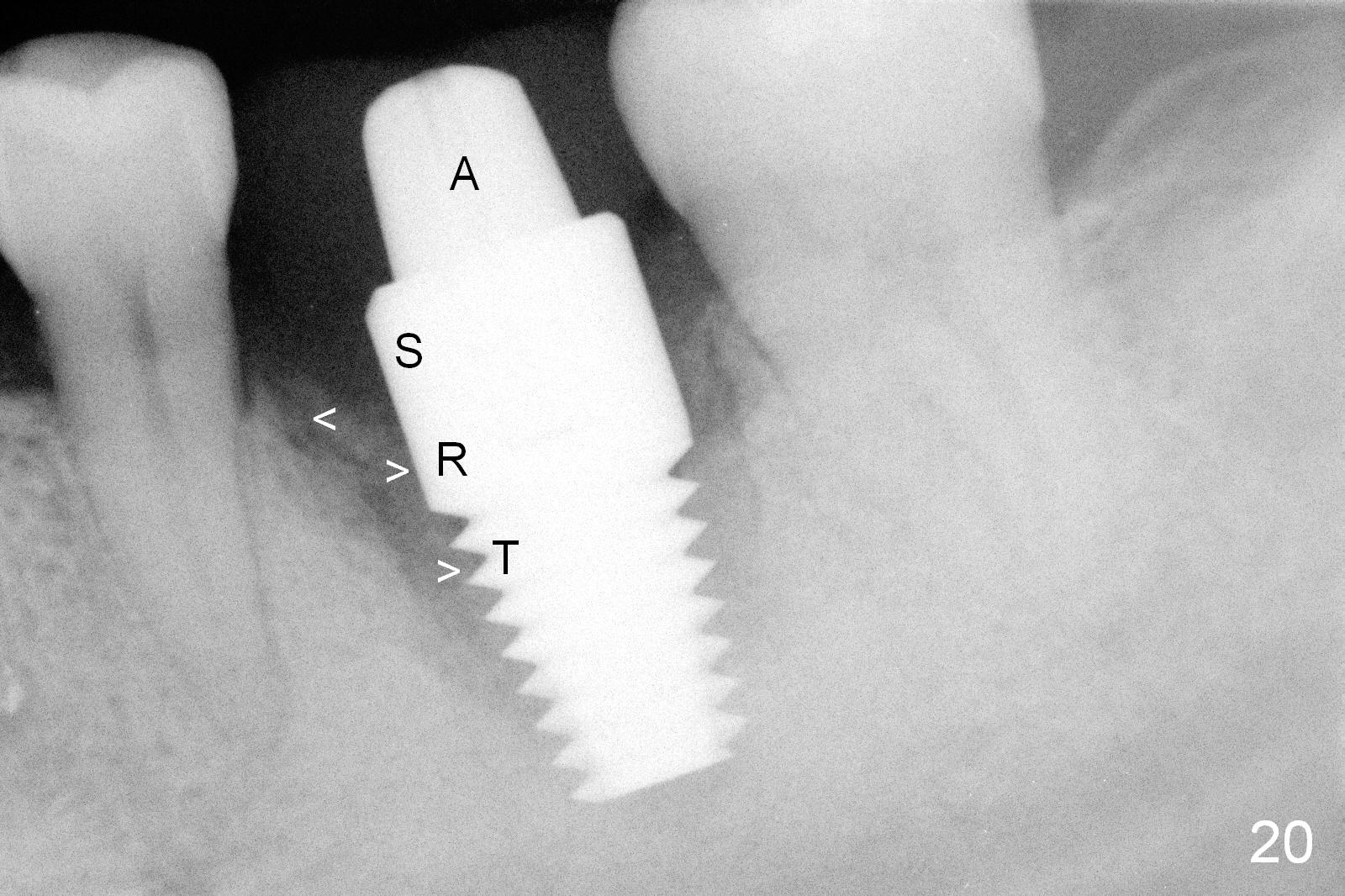
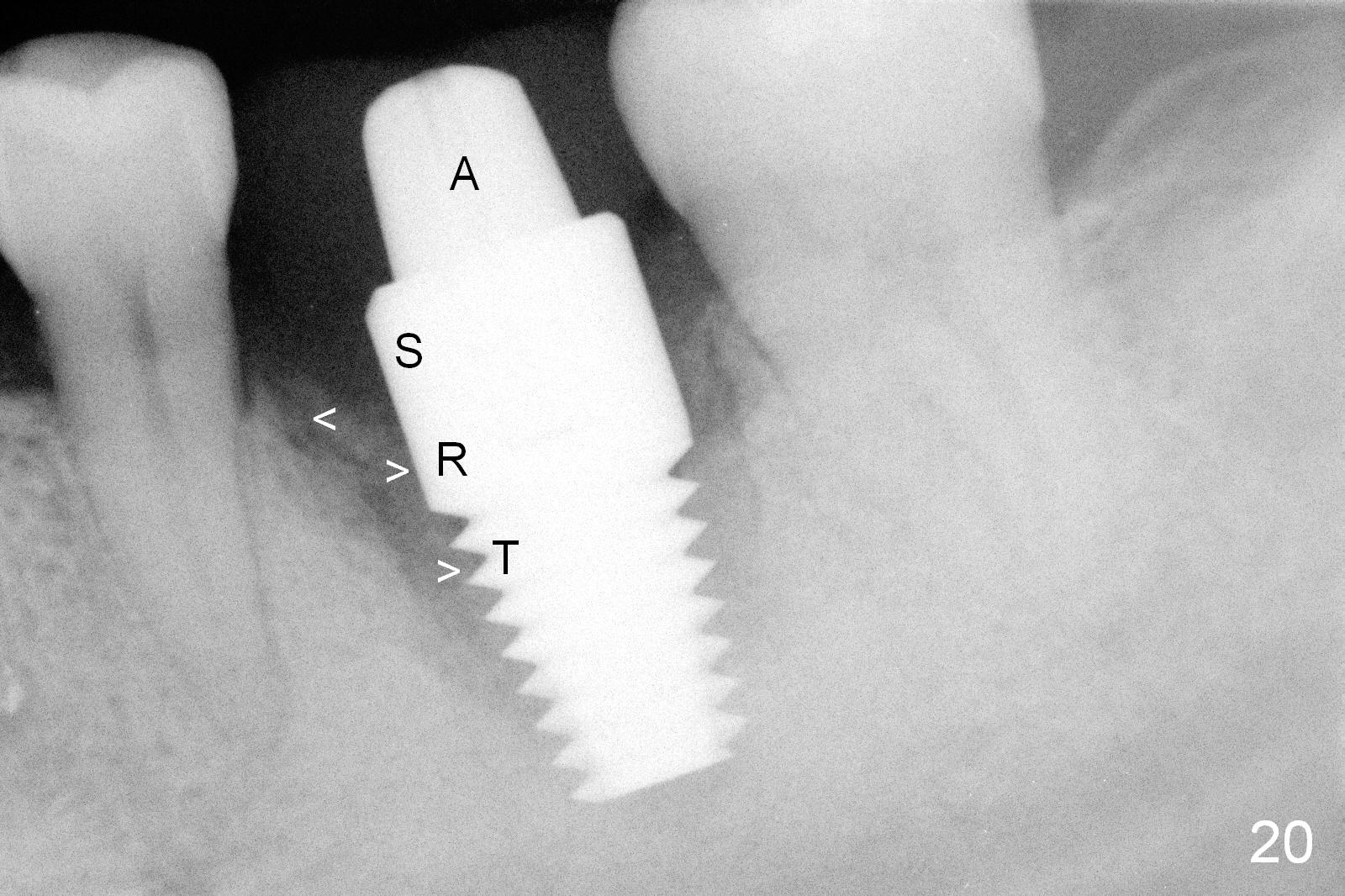
Four months postop, bone graft remains attached to (Fig.20 >) the rough (R) and thread (T) surfaces of the implant, while moving away from (<) the smooth (S) surface. This is what it should be. There is a small area of perforation of the provisional (Fig.21 linguoocclusal view). When the latter is removed for the final restoration, the lingual gingiva is healthy, suggesting no infection underneath and possible normal lingual plate regeneration (Fig.22 *).
It is also reasonable to fabricated an immediate provisional for next implant at a healed site.
Return to Lower Molar Immediate Implant,
Posterior Immediate Provisional
Xin Wei, DDS, PhD, MS 1st edition 02/19/2015, last revision 01/19/2018