

.jpg)

 |
 |
 |
|
 |
 |
 |
|
 |
 |
 |
.jpg) |
 |
 |
 |
|
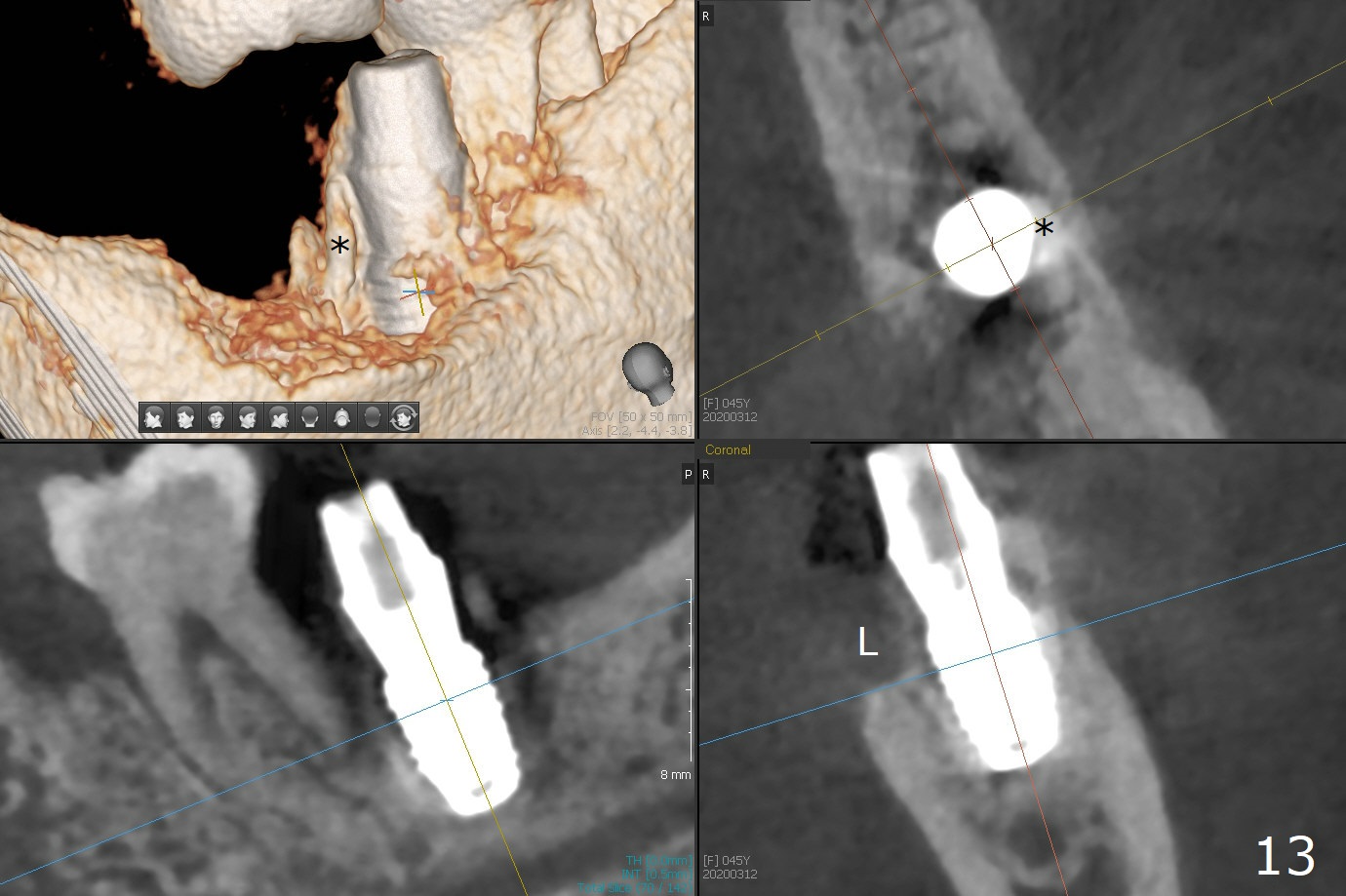
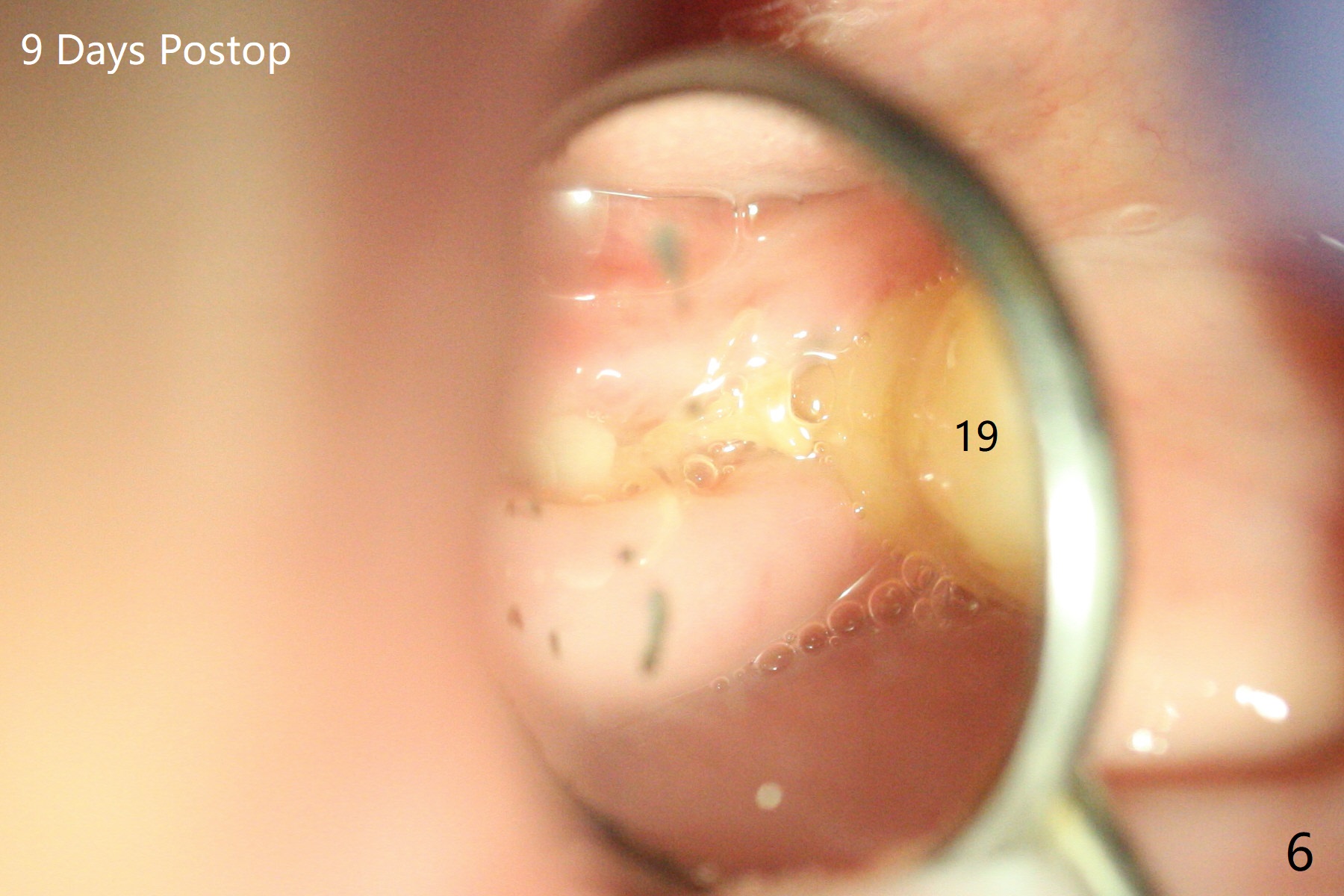
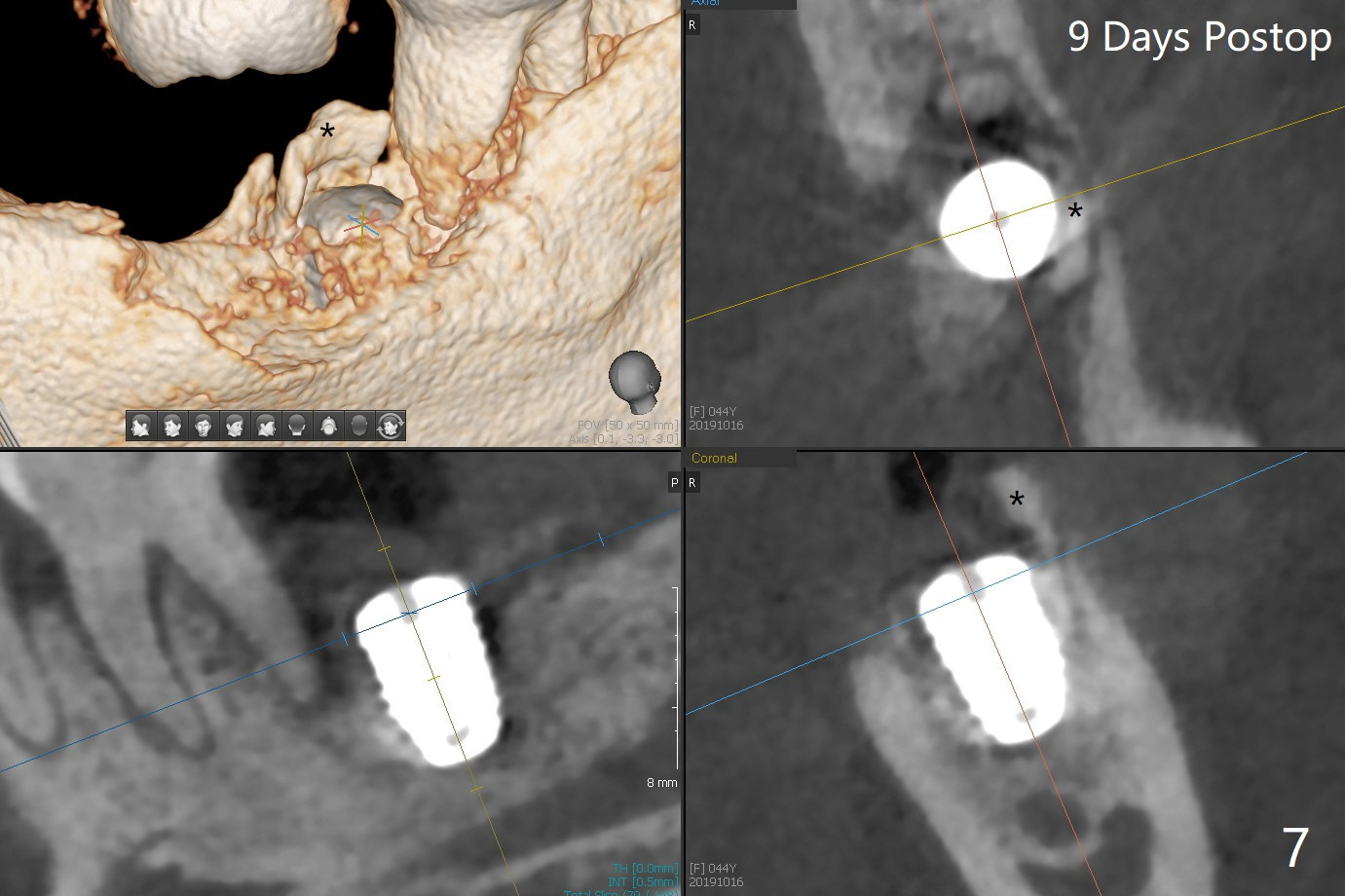
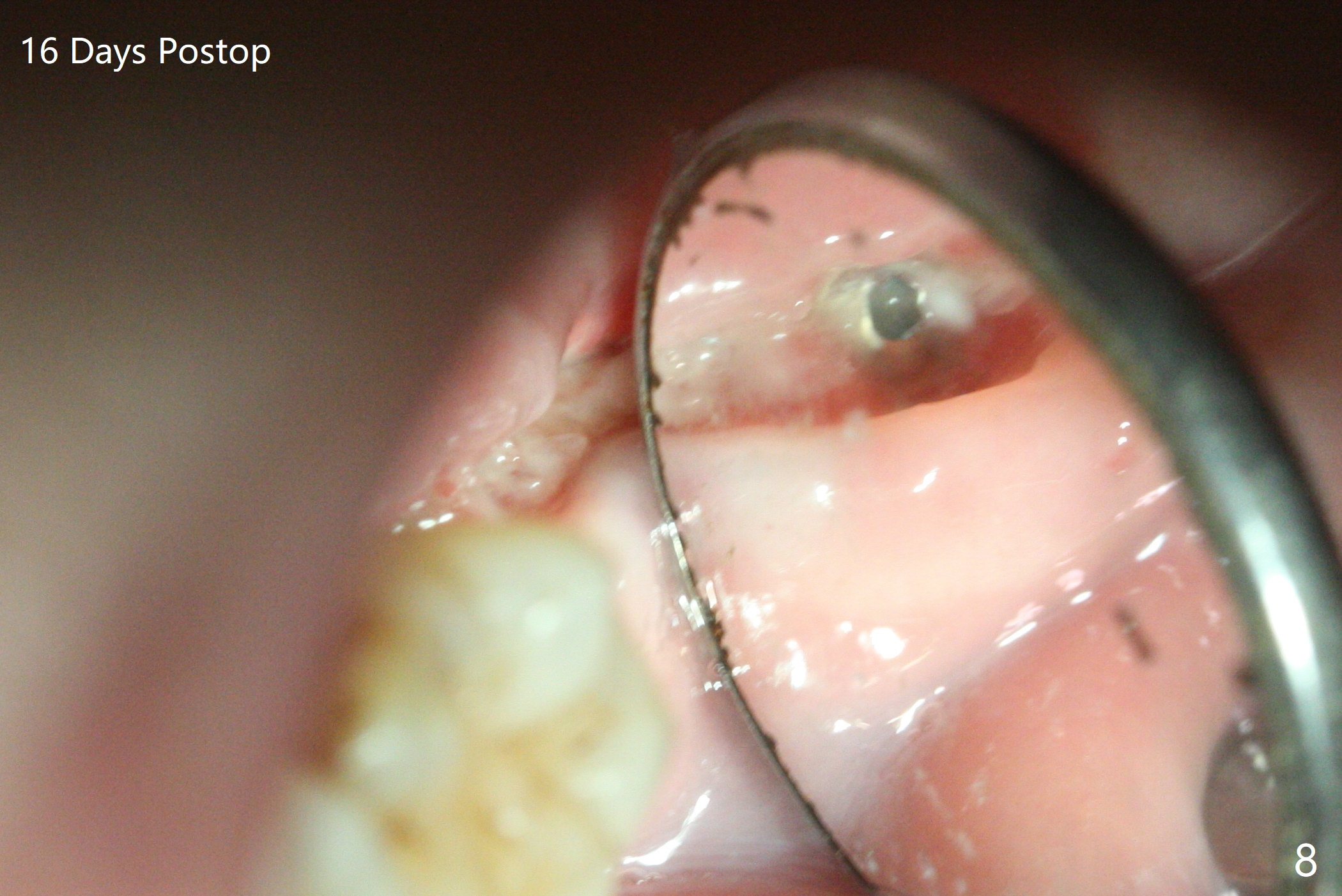
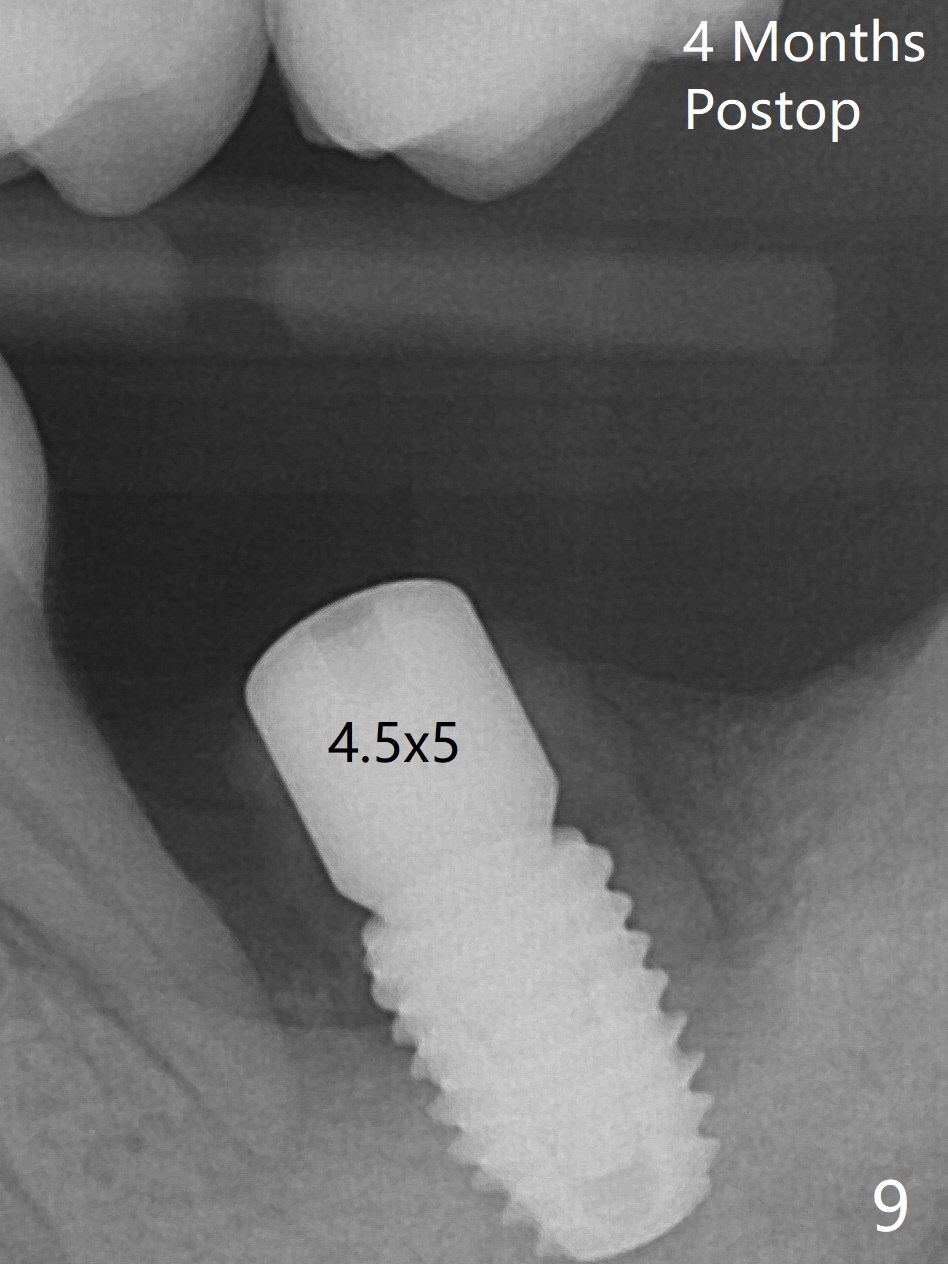
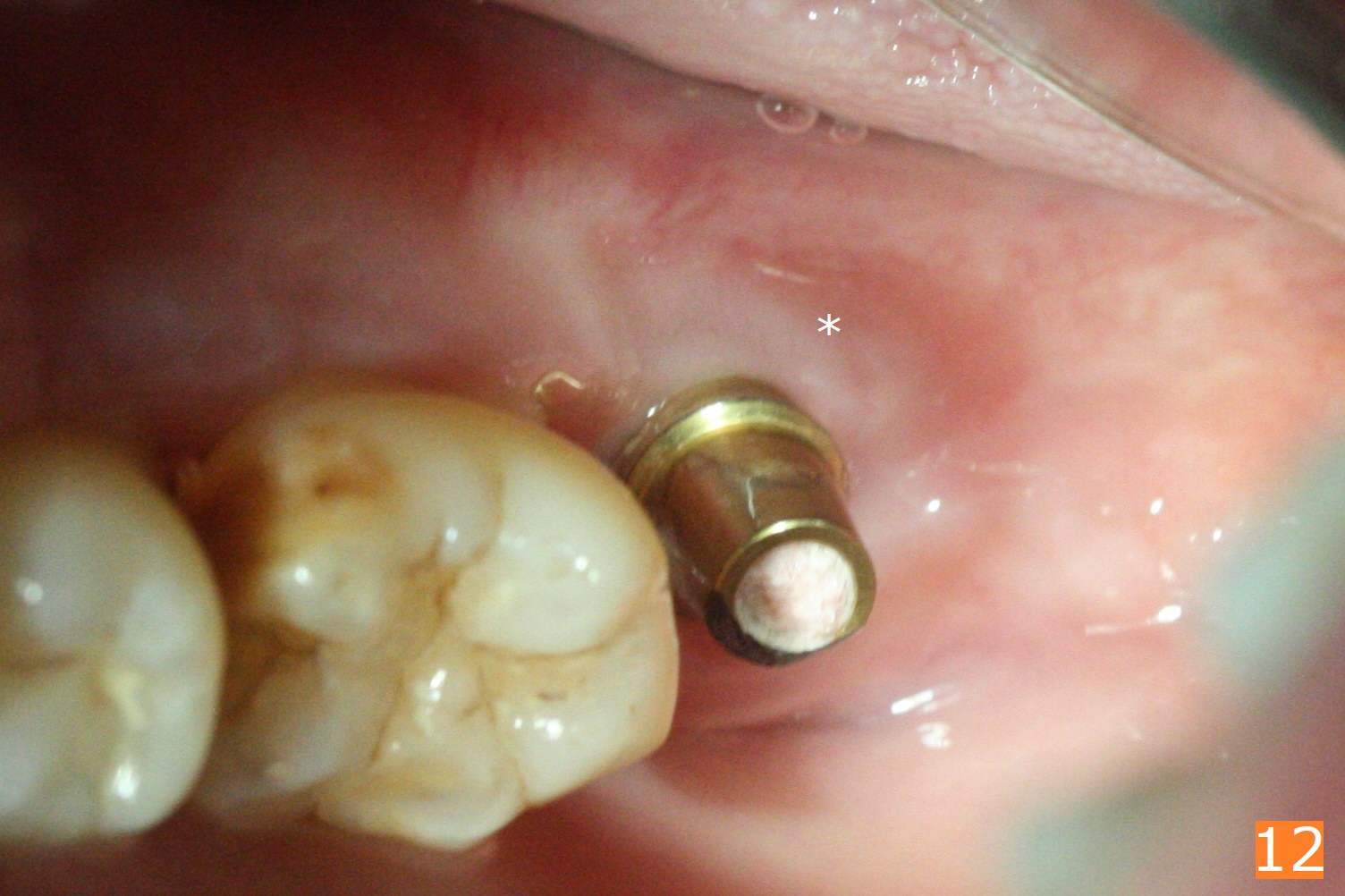
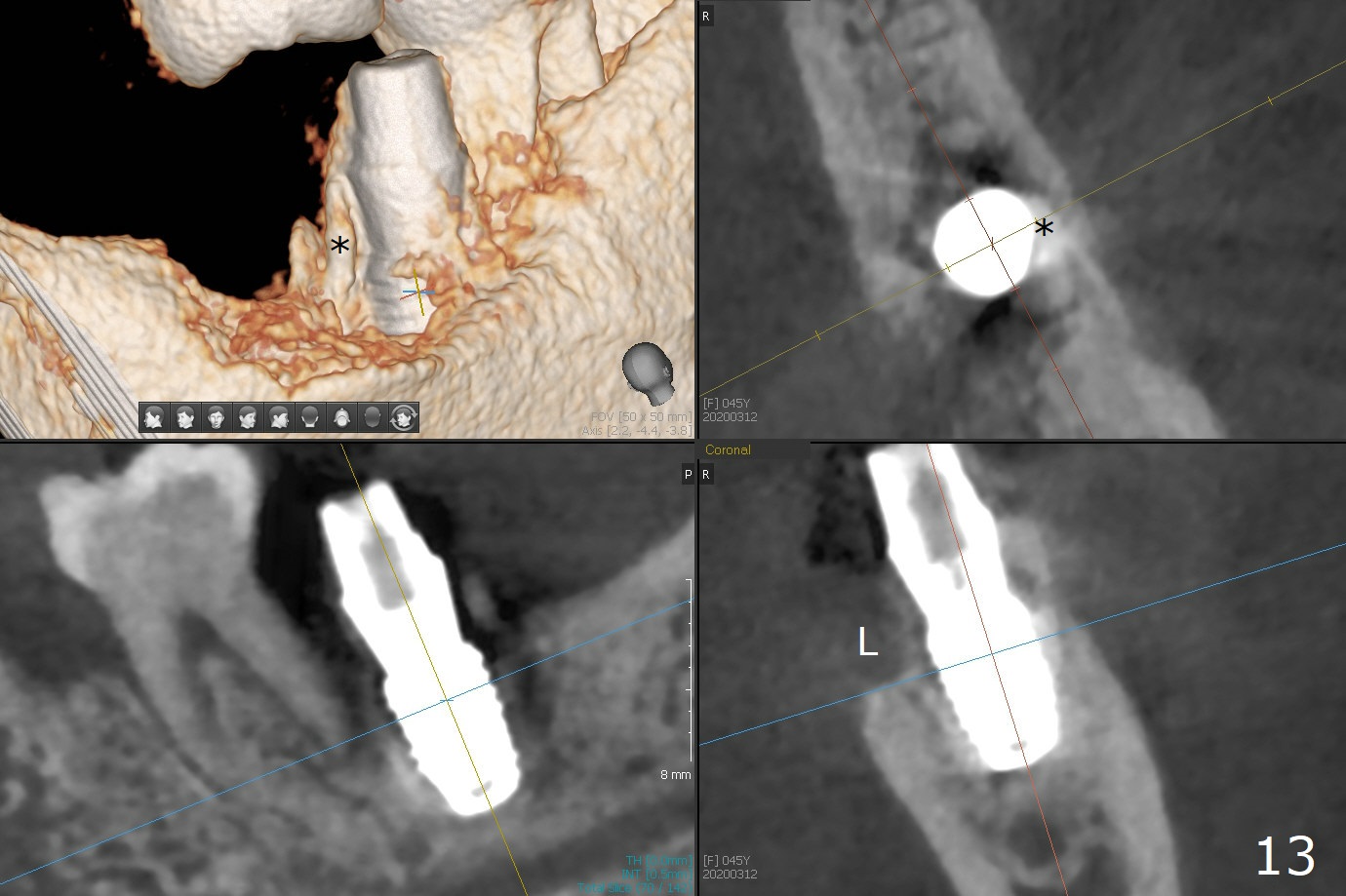
Molar Socket Shield I
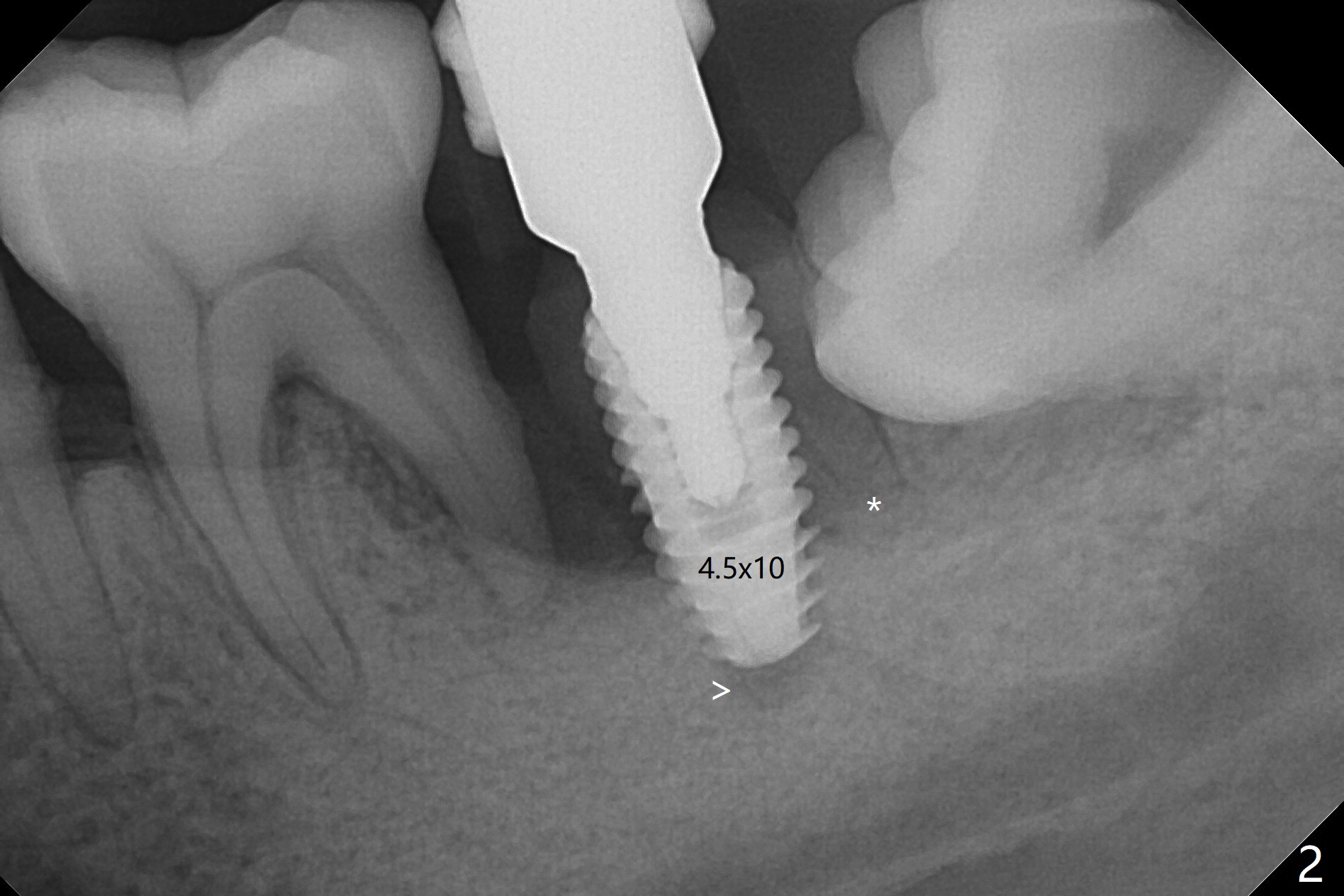
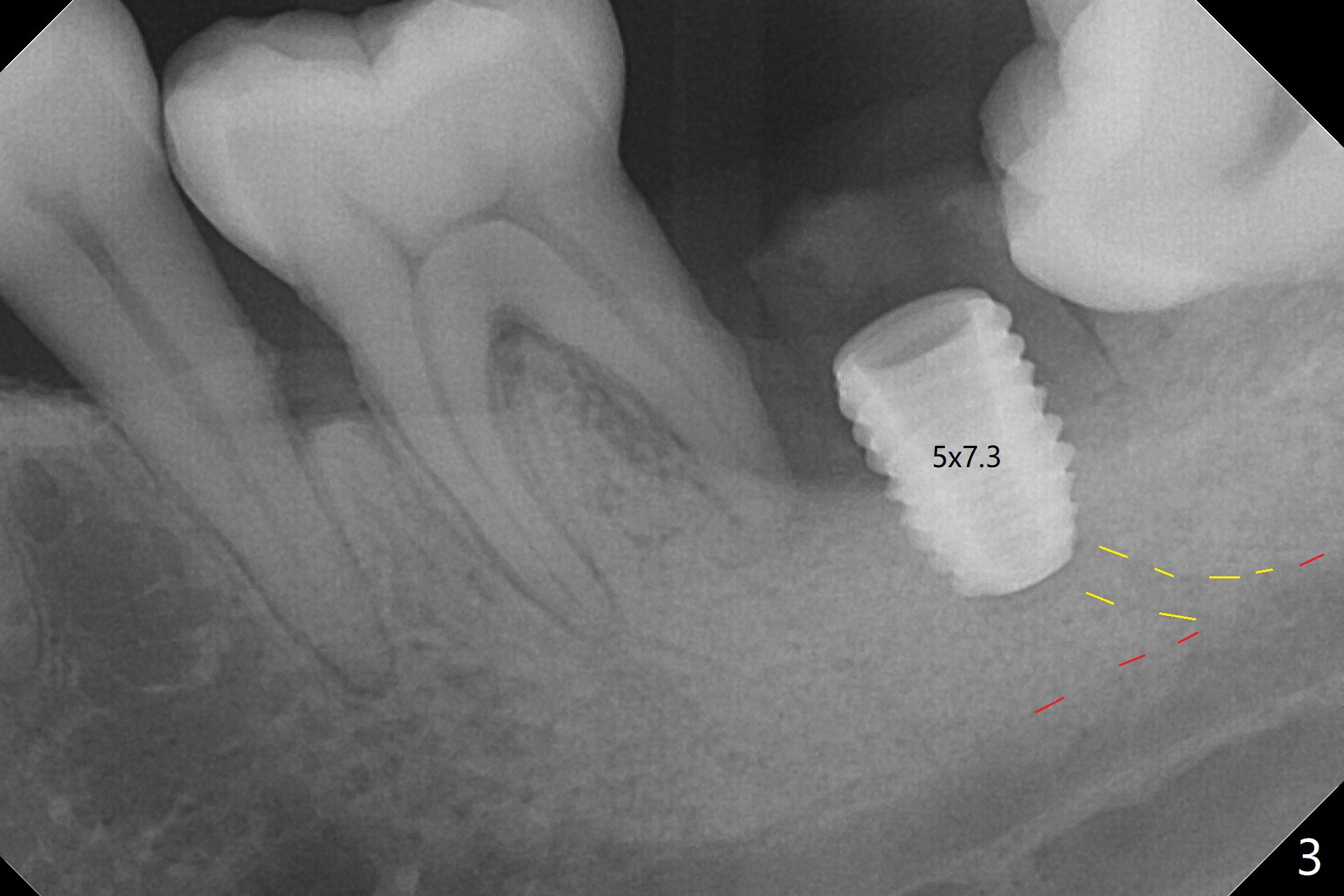
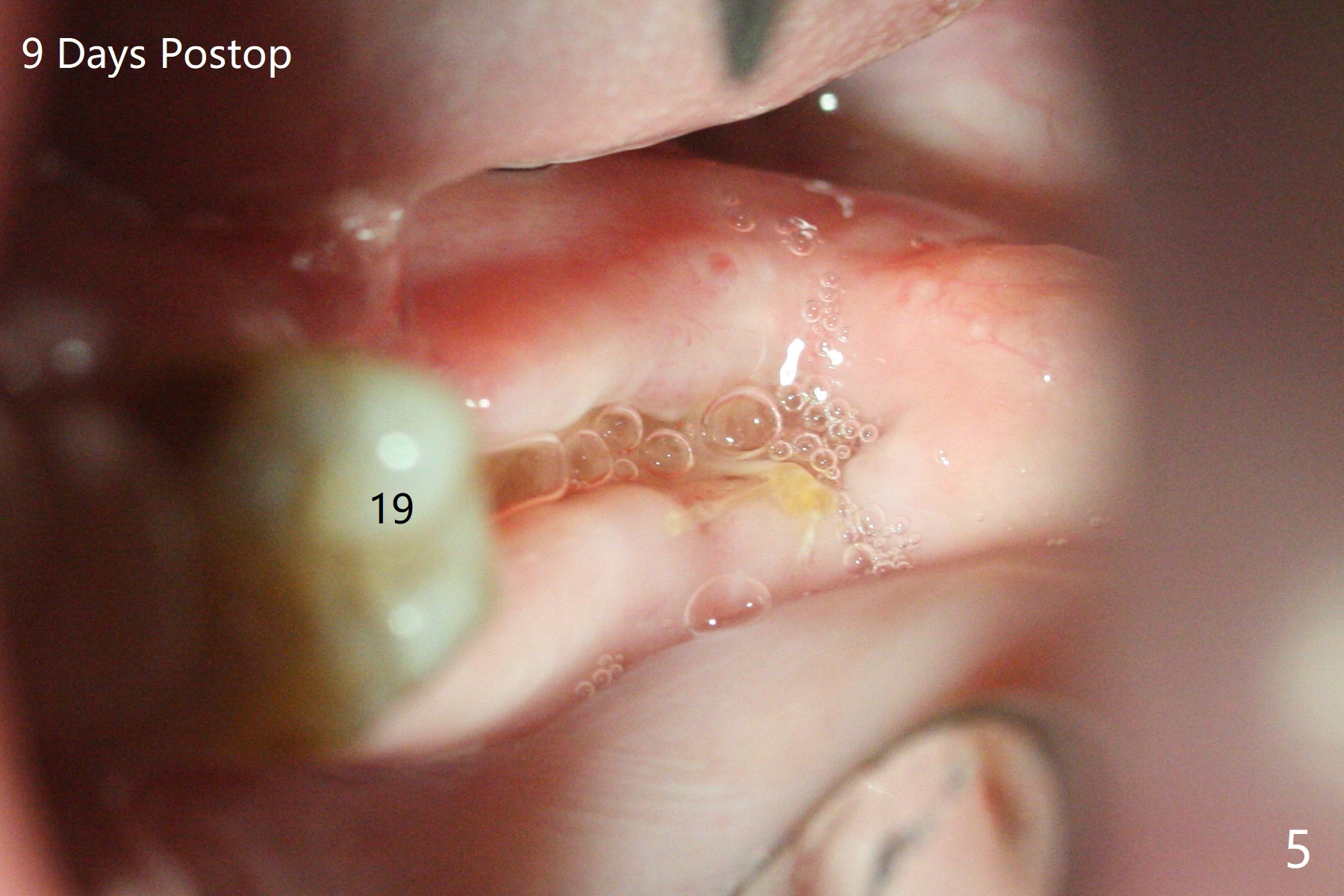
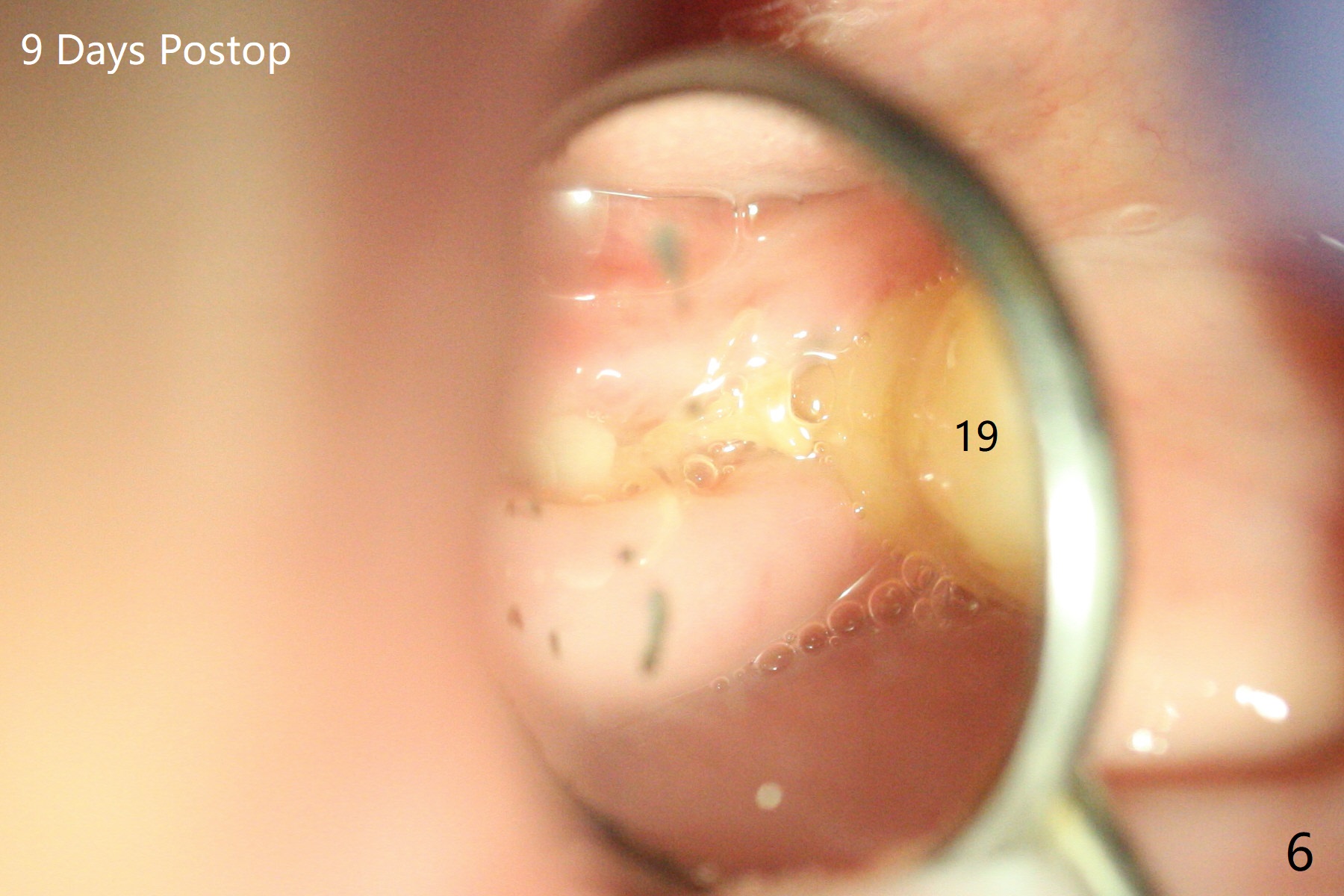
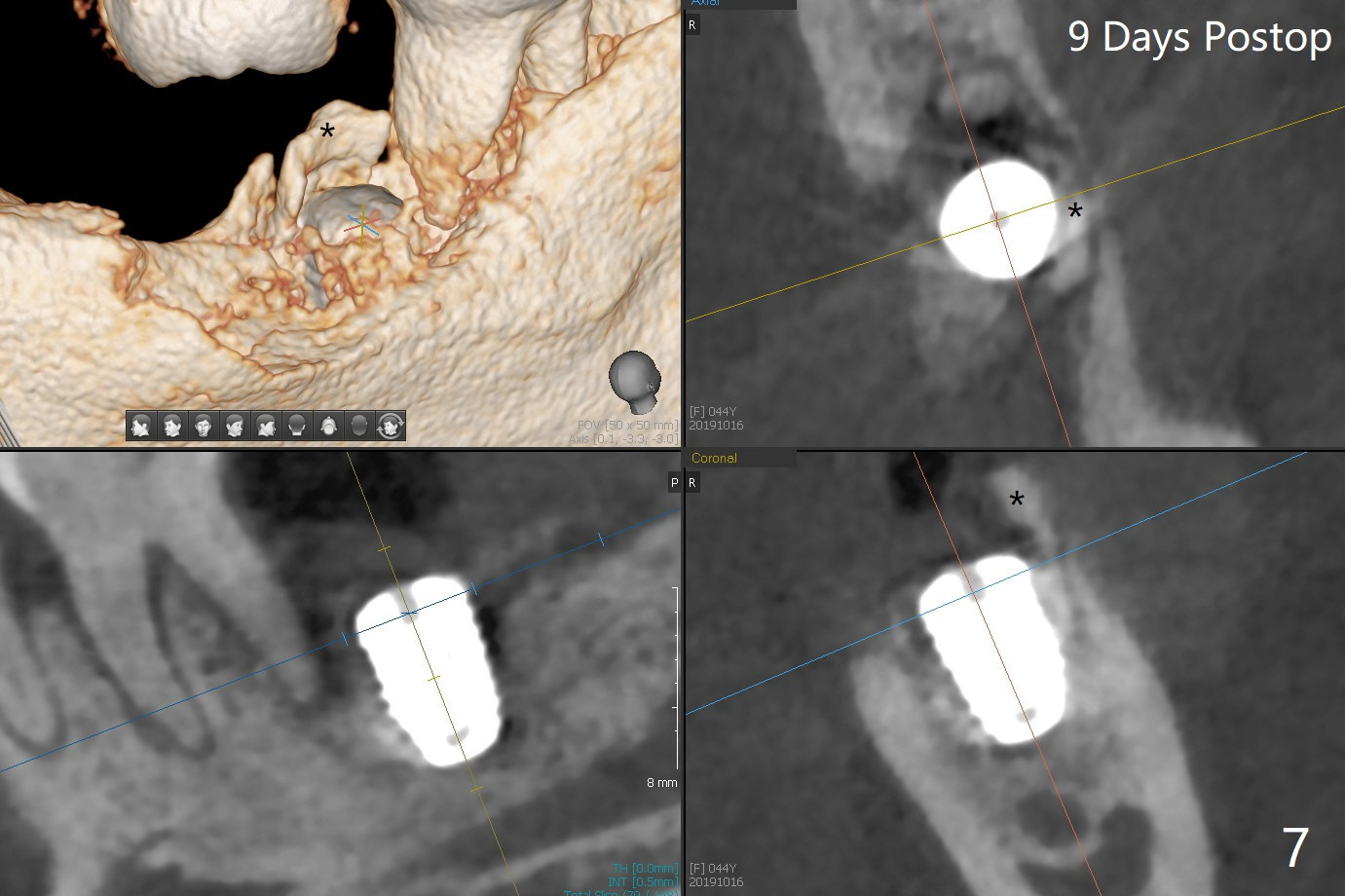
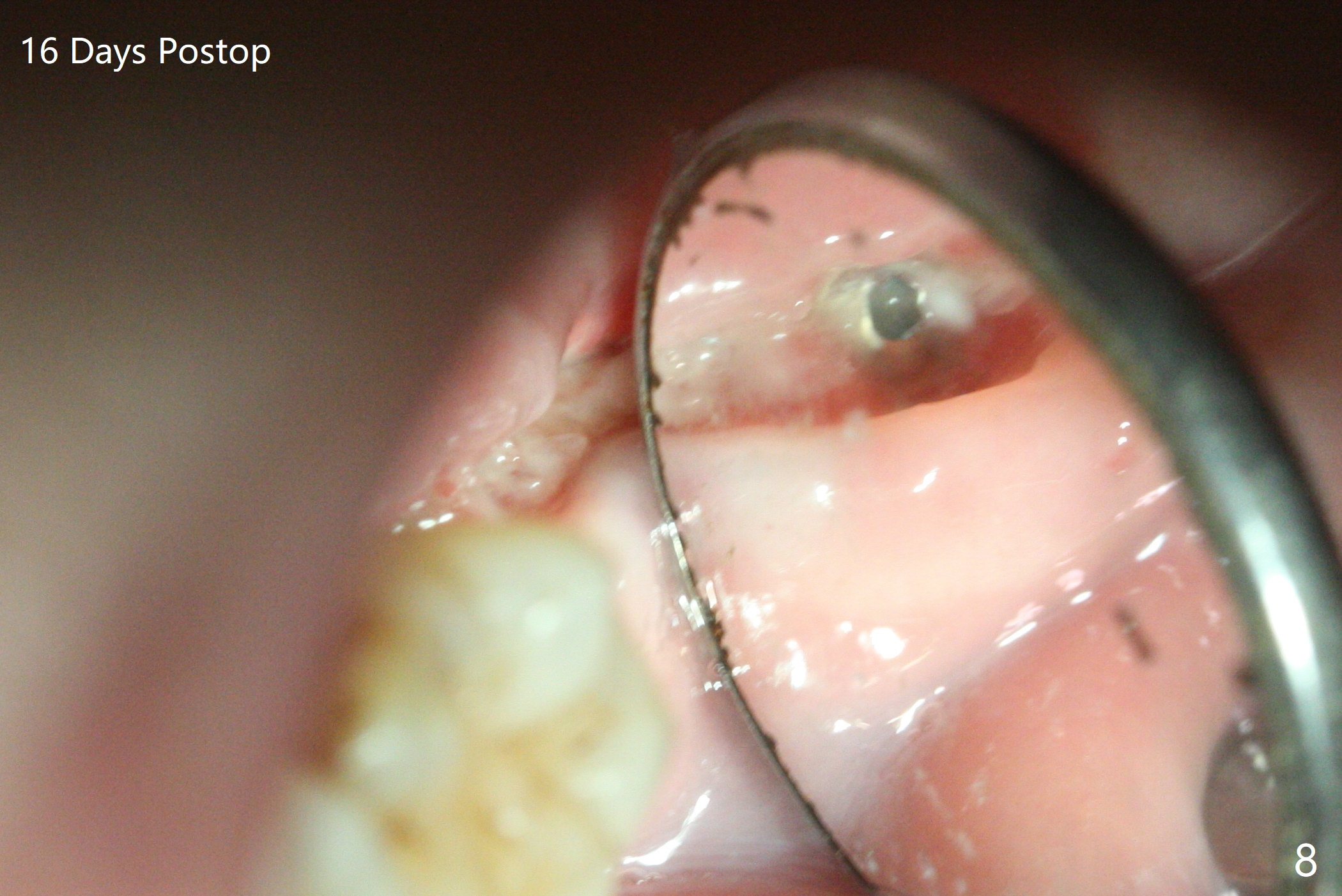
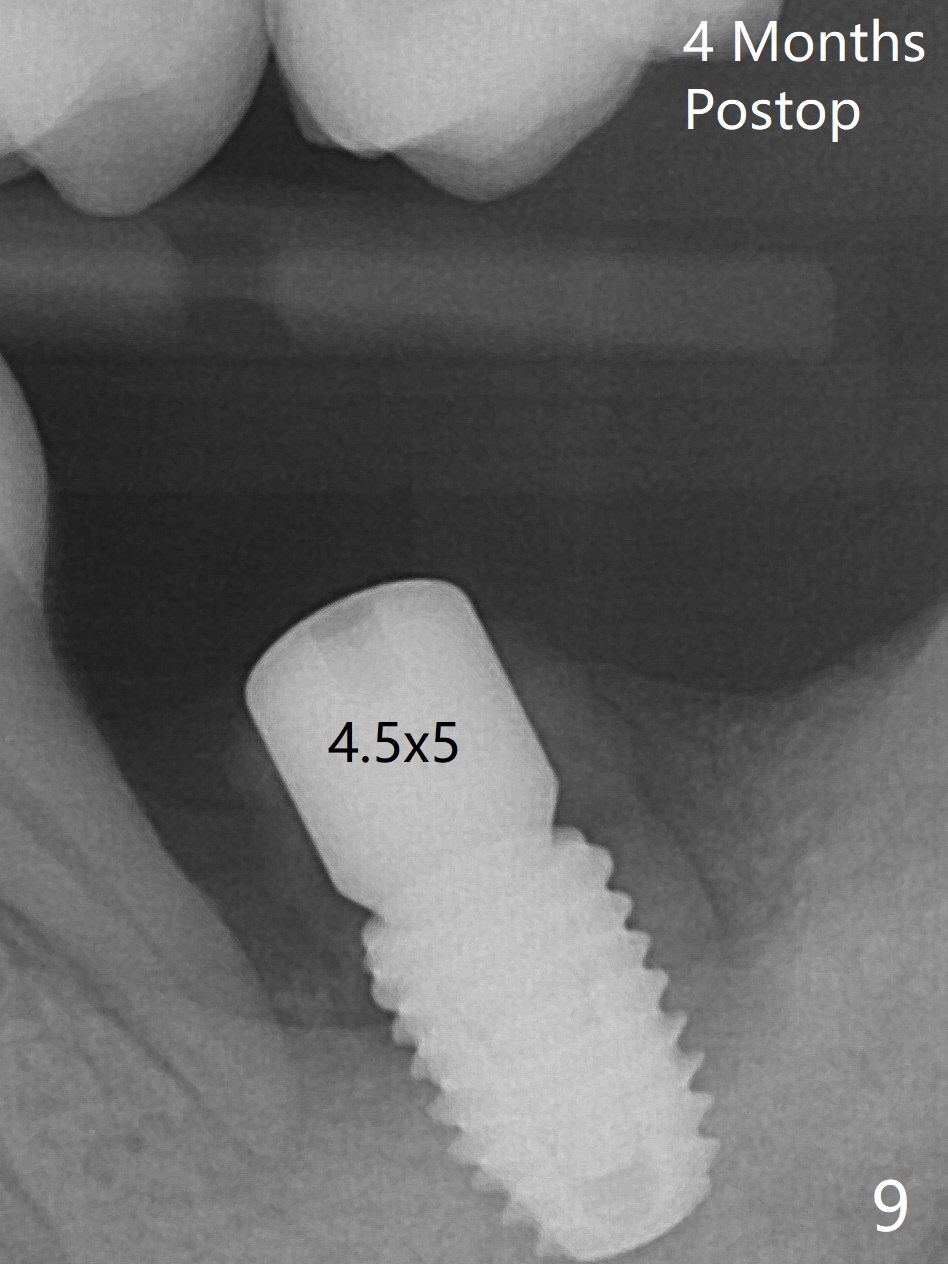
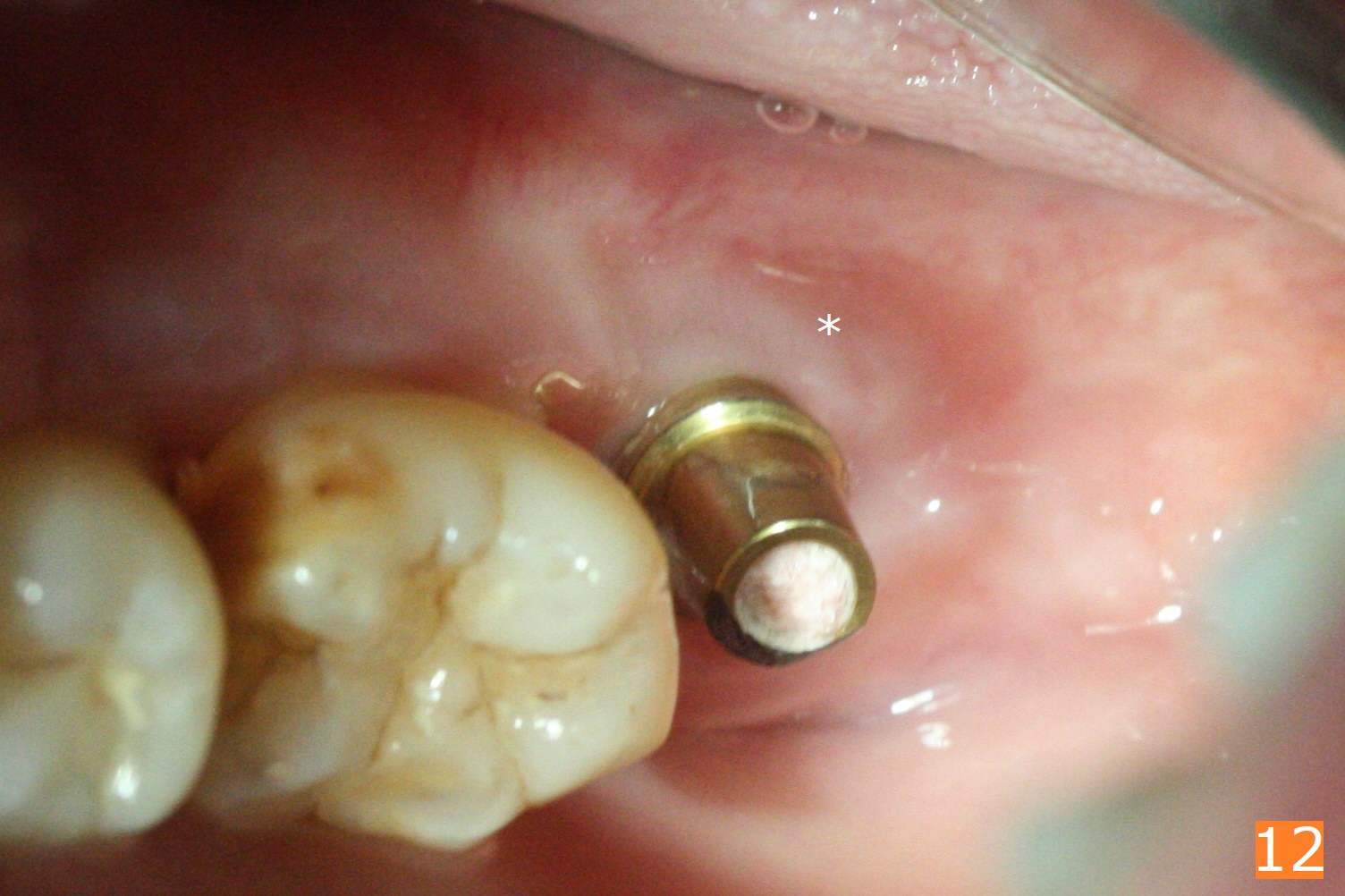
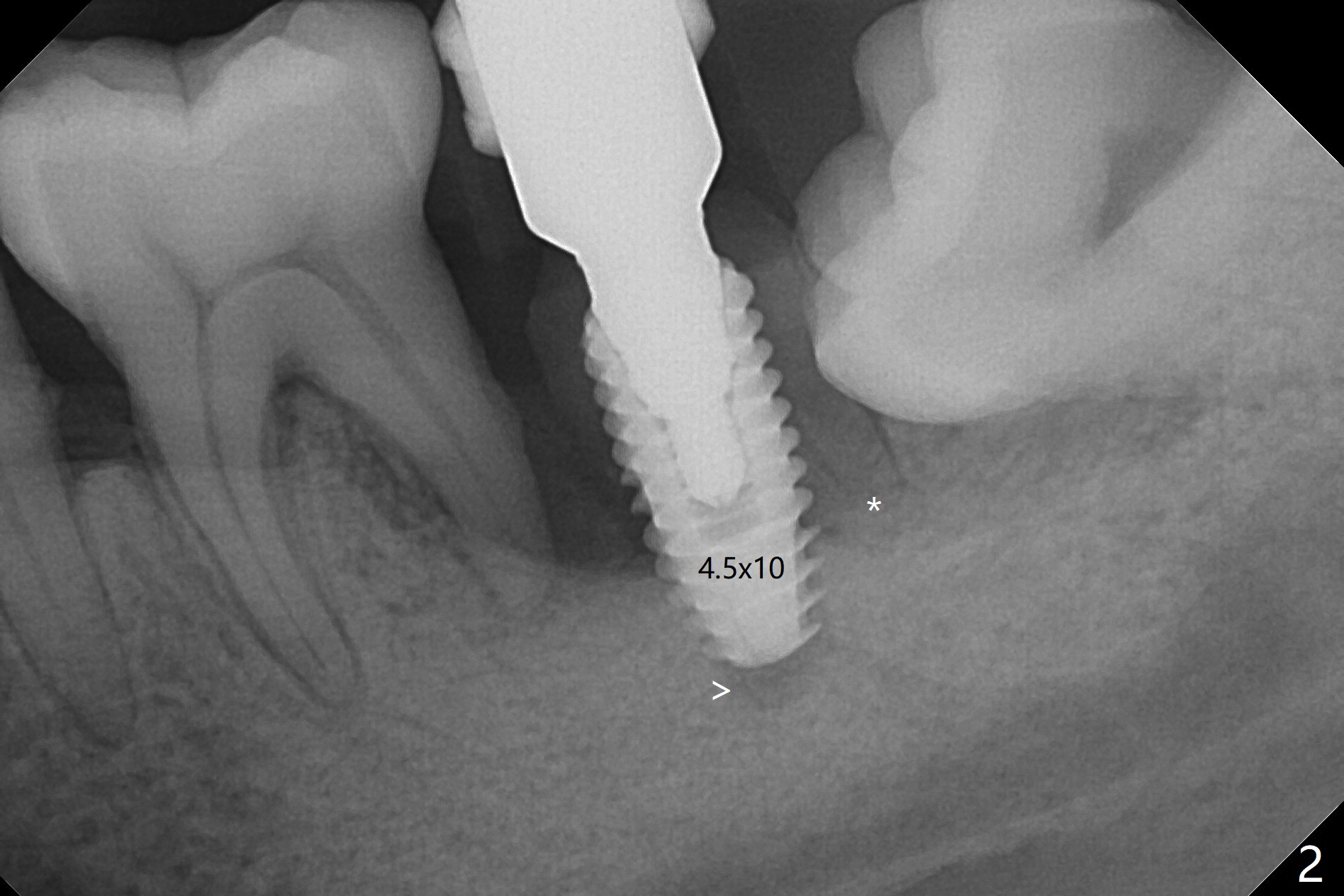
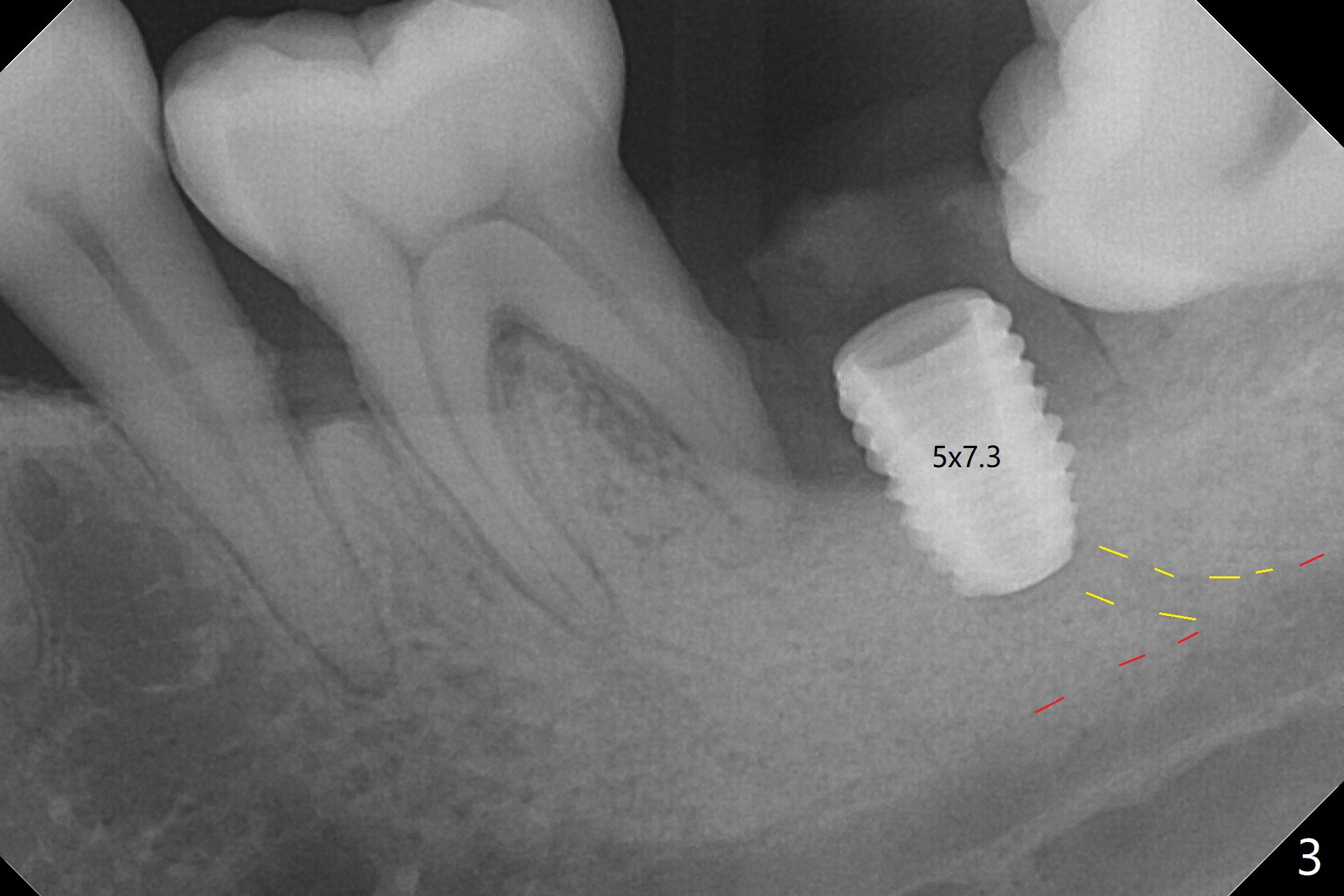
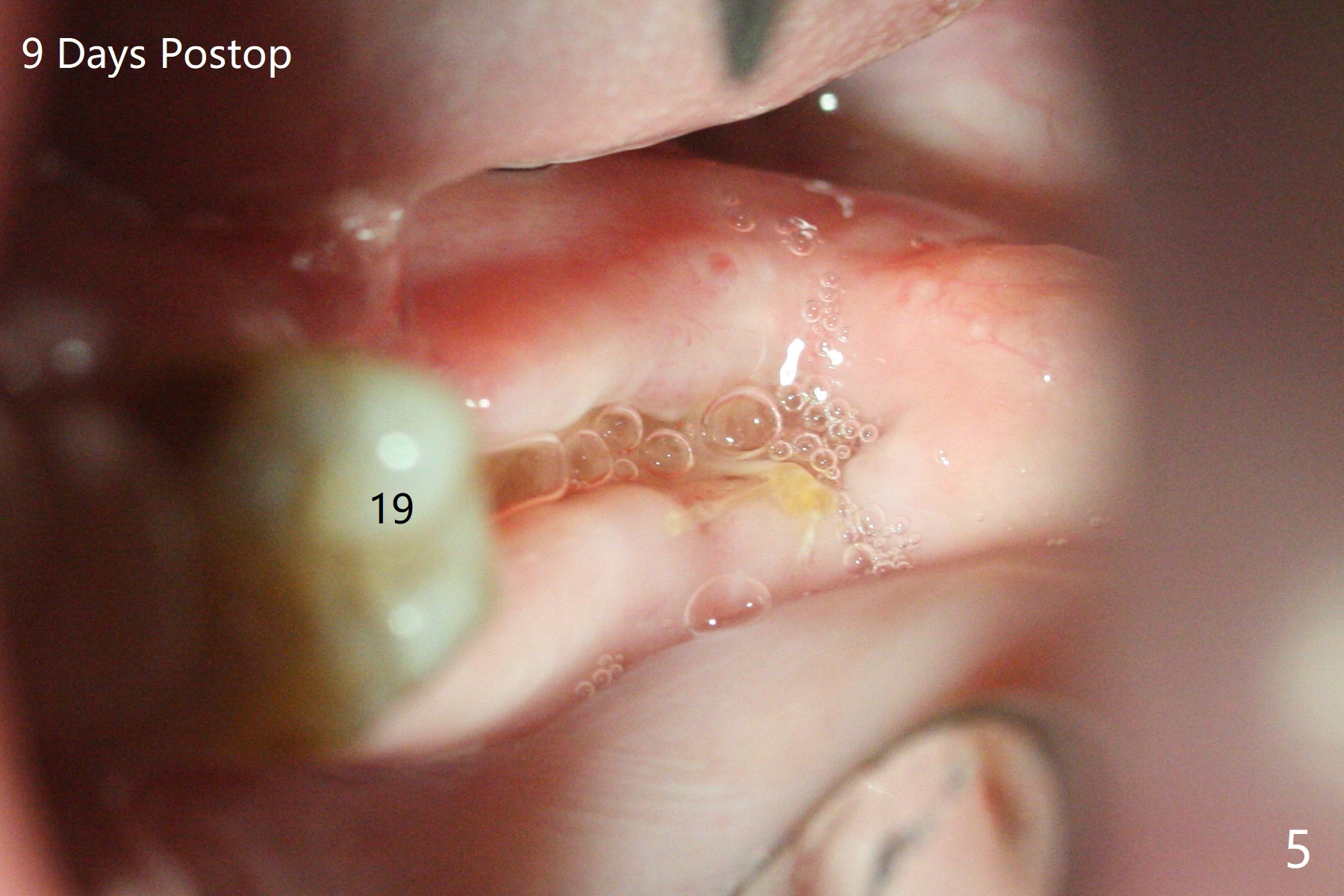
Socket shield (partial extraction therapies) is going to be conducted in this case to form a substitute buccal plate of the 2nd molar (Fig.1 *). The apex of the shield that contacts the 4.5x10 mm dummy implant cannot be removed because of poor access (Fig.2 * (12 mm offset)). Due to high bone density, a 4.5 mm drill has to be used in order to place a 5x7.3 mm definitive implant (Fig.3). In spite of the fact that the implant seems to be completely seated, the implant is ~ 1 mm supracrestal lingually. After implant removal, a 4.5x11.5 mm drill cannot reach the depth due to high bone density. 800 RPM instead of 50 RPM may help. When the implant is reseated, it appears to be .5 mm deeper than before clinically, although it looks incompletely seated in X-ray (Fig.4 <). The insertion torque is 60 Ncm. Allograft mixed with PRF is placed around the implant with cover screw, particularly mesiolinguodistal (Fig.4 *). The sockets of #17 and 18 are approximated with the help of 2 piece of PRF and collagen plug. The wound dehisces 9 days postop (Fig.5,6), although asymptomatic. Forced closure of the sockets with suture seems unnatural. An immediate provisional should have been fabricated. CT shows possible loss of part of bone graft (Fig.7). Regraft seems necessary in the appointment of uncover. Antibiotic is prescribed for another week. The gingiva seems healthy around the exposed healing screw 16 days postop (Fig.8). After debridement, the healing screw is then changed to a 4.5x5 mm healing abutment. The majority of the bone graft is lost without immediate provisional in 4 months (Fig.9 * (<: socket shield)). Then a 5.5x5 mm healing abutment is inserted for impression next appointment. A 5.2x4.5(4) mm cemented abutment is placed before impression (Fig.10). With socket shield (Fig.11 ^), the buccal gingiva looks more keratinized than the lingual one (Fig.12 *). Photos are taken immediately pre-cementation. Socket shield (*) covers the implant and abutment buccally (Fig.13 CT taken immediately pre-cementation).
Return to
Lower
Molar Immediate Implant,
Prevent Molar Periimplantitis (Protocols,
Table)
Trajectory II
Shield
Xin Wei, DDS, PhD, MS 1st edition
10/07/2019, last revision
03/15/2020