

 |
 |
 |
 |
 |
 |
 |
 |
 |
|||
Bone Graft Post Guided Surgery
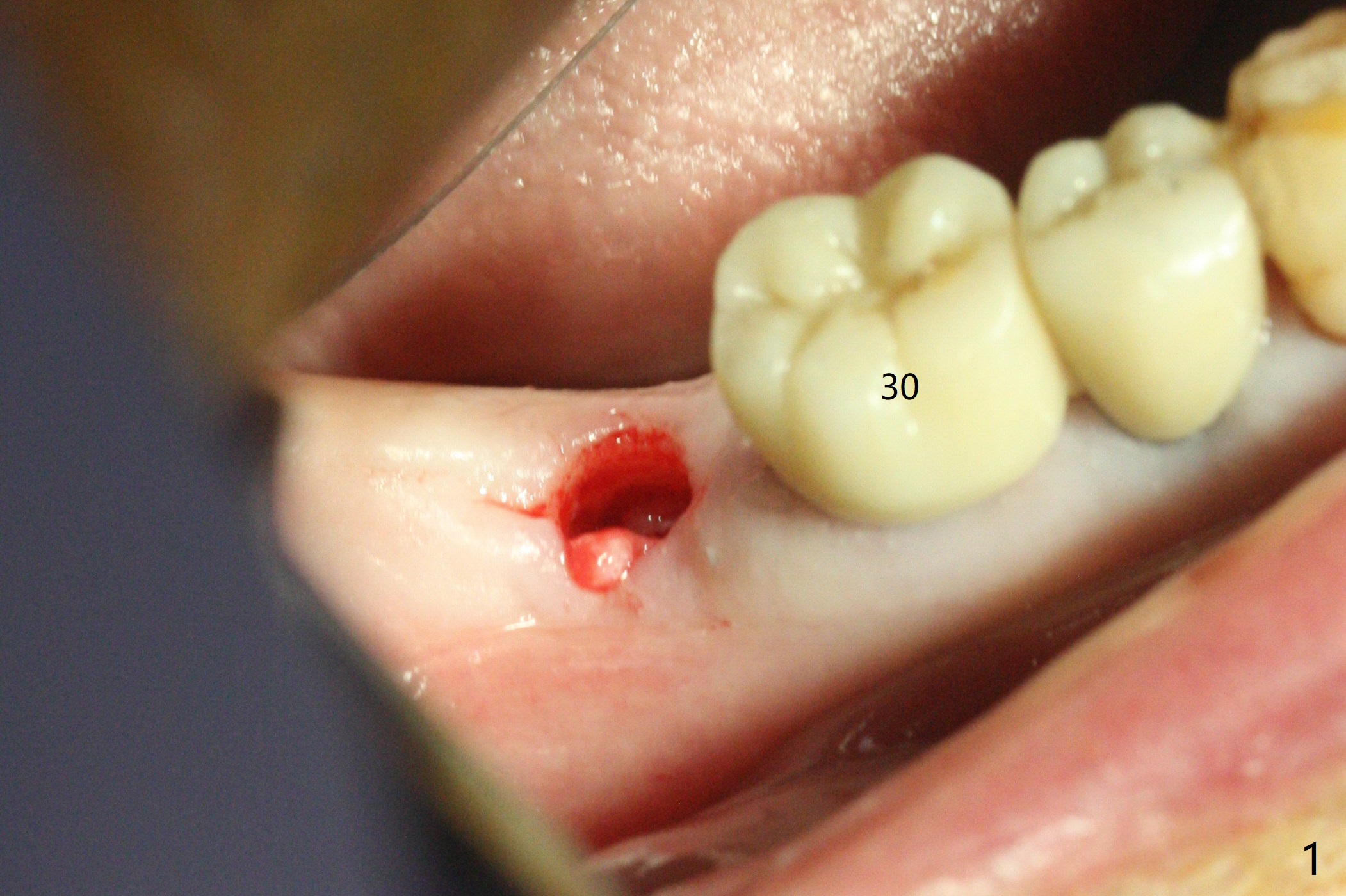
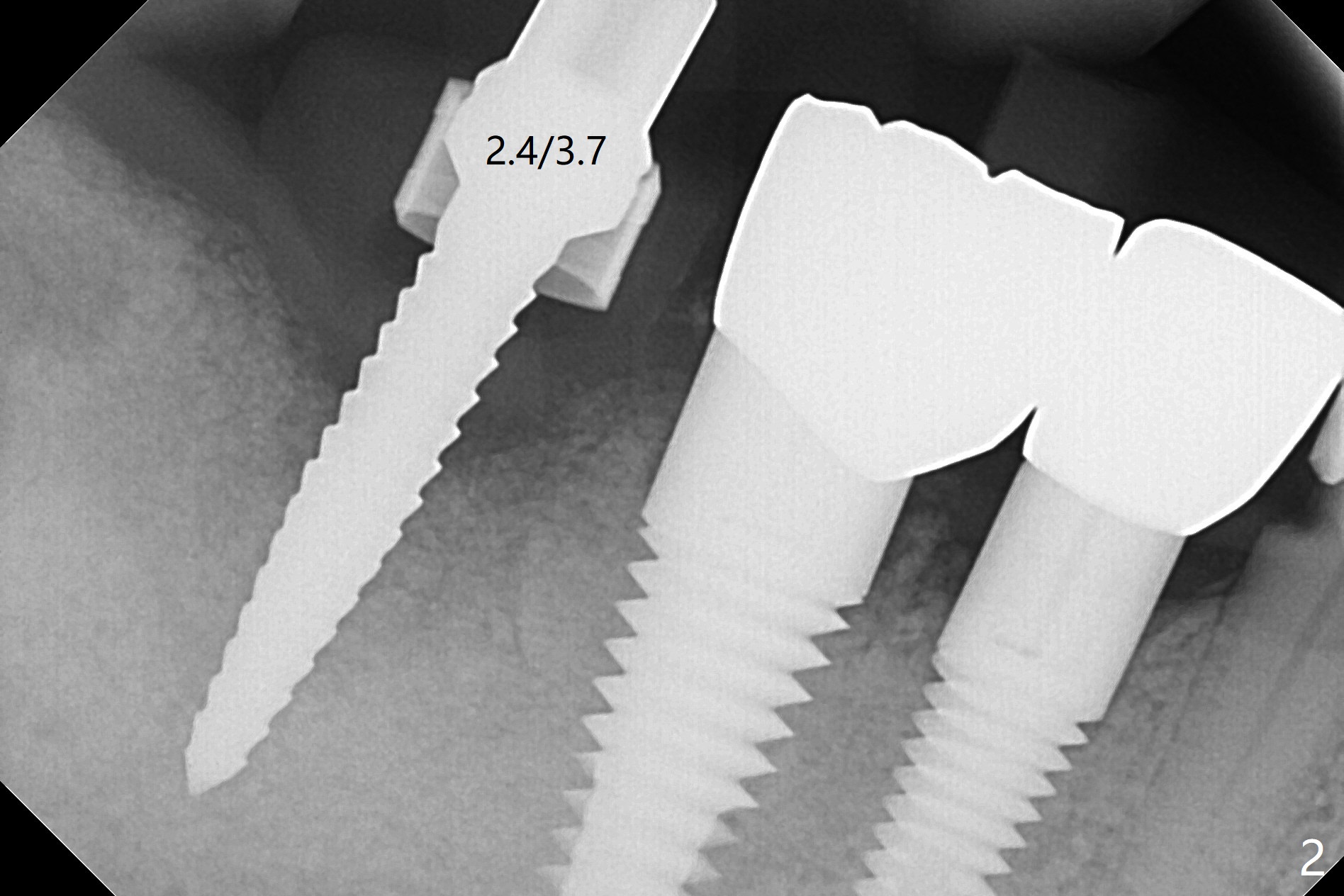
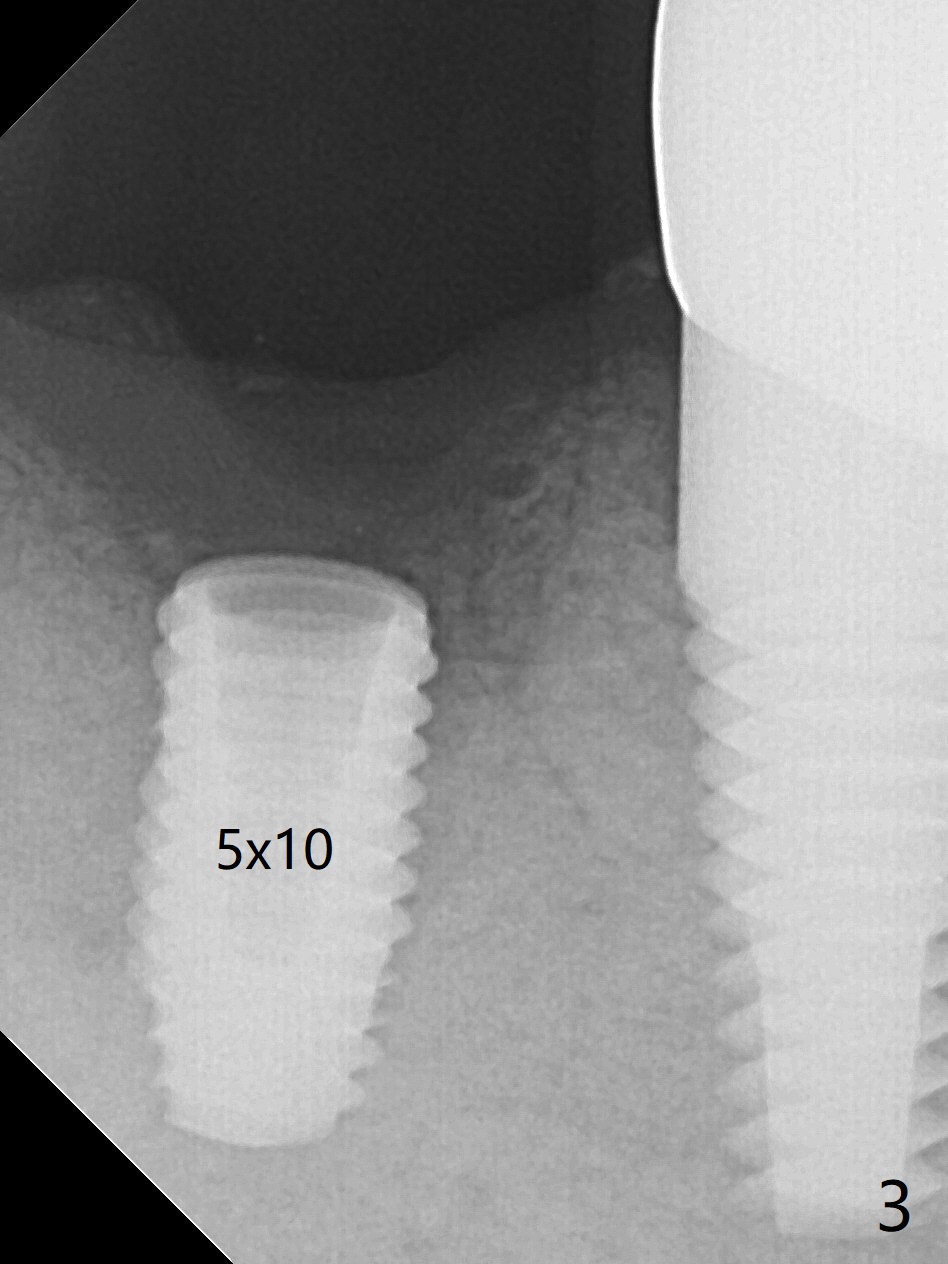
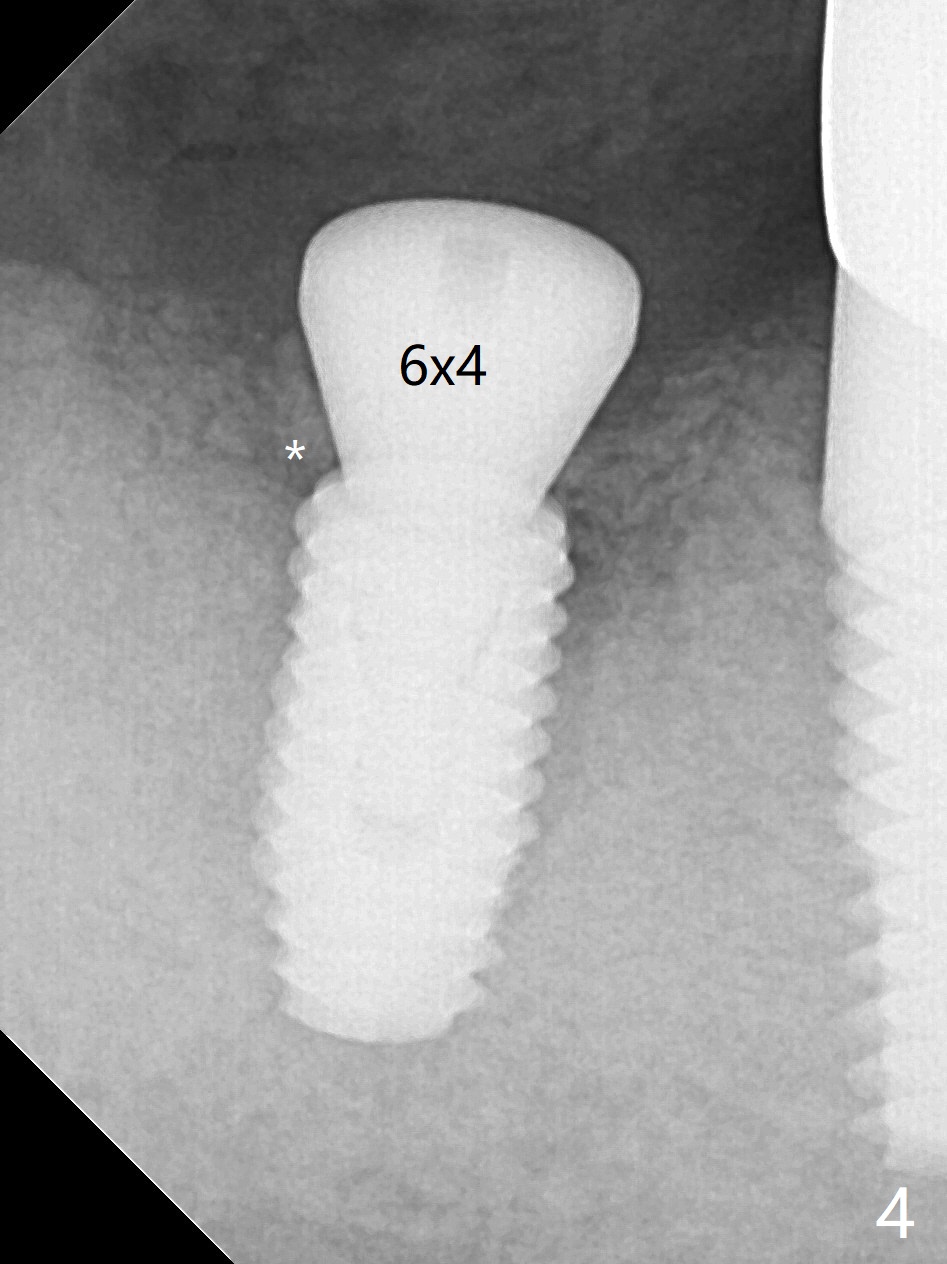
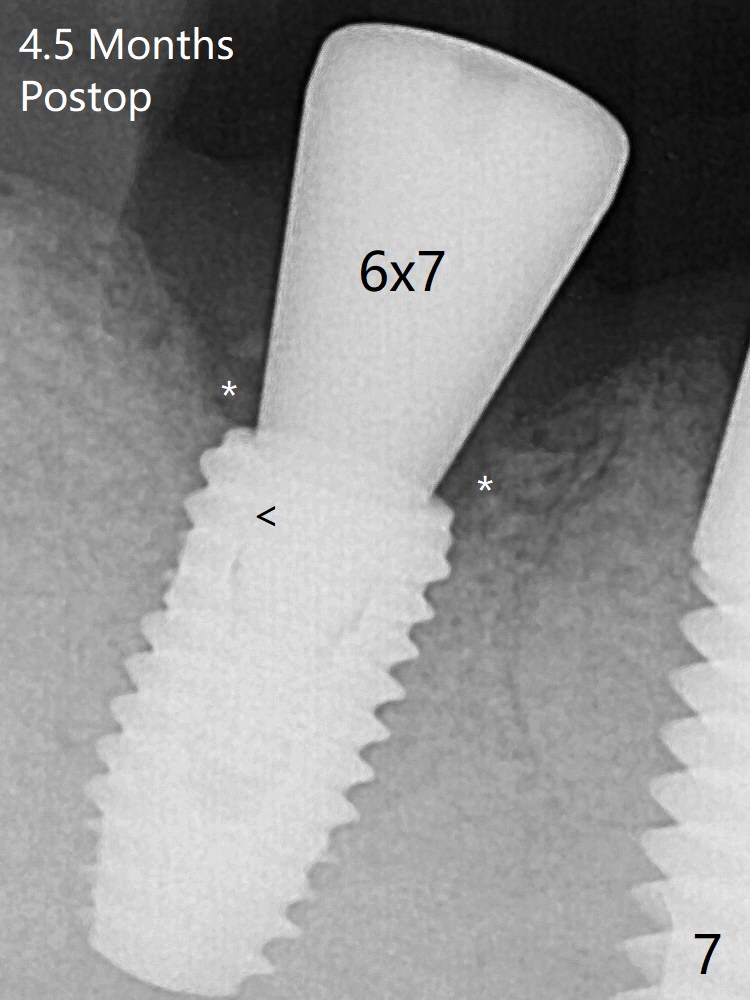
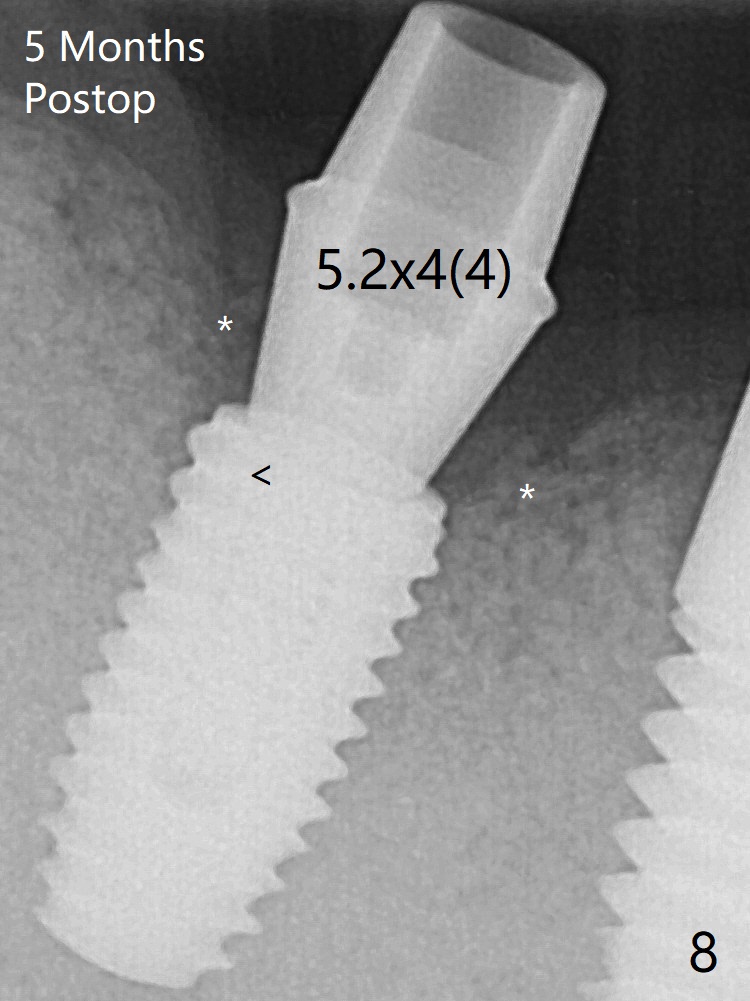
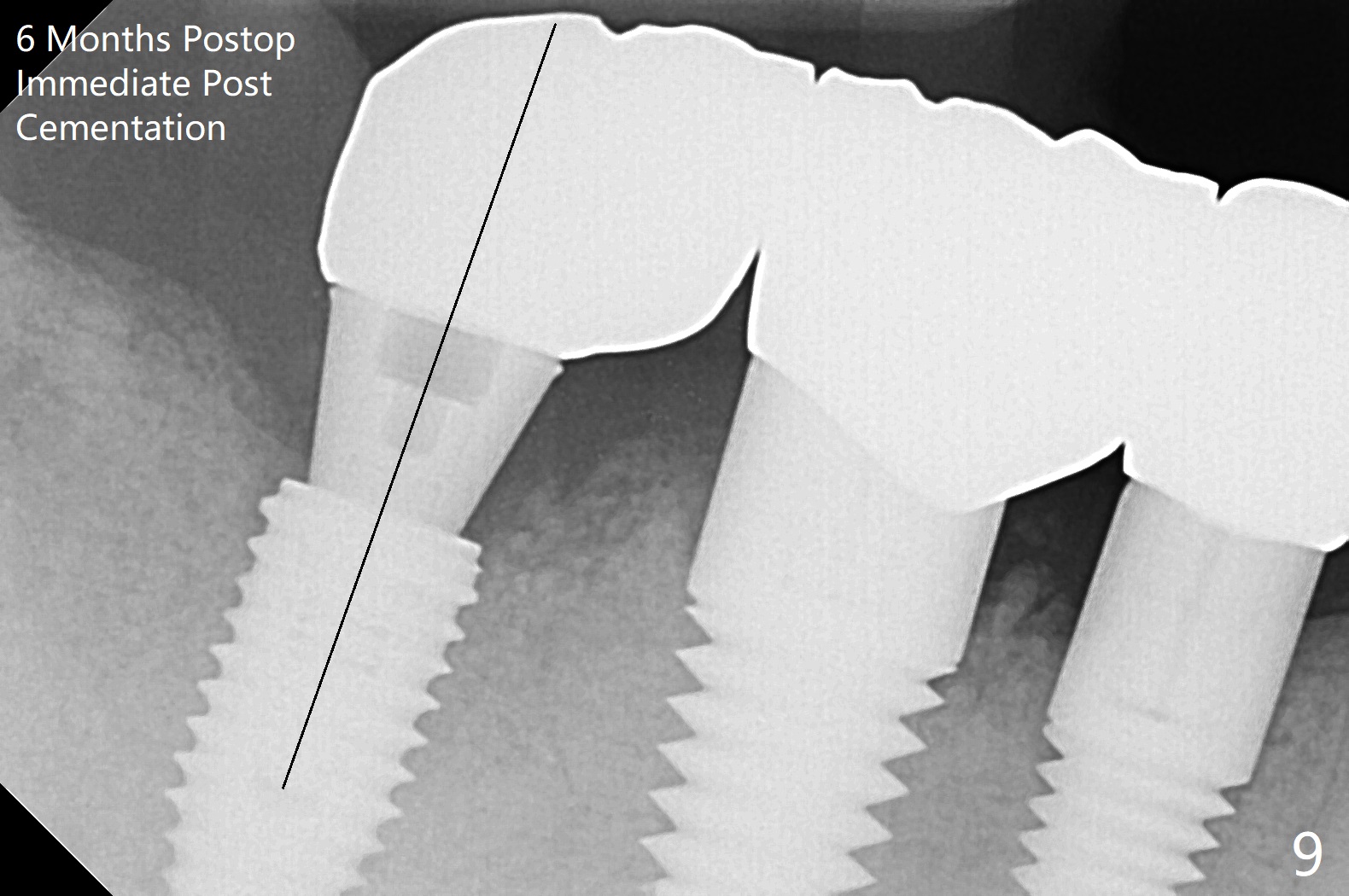
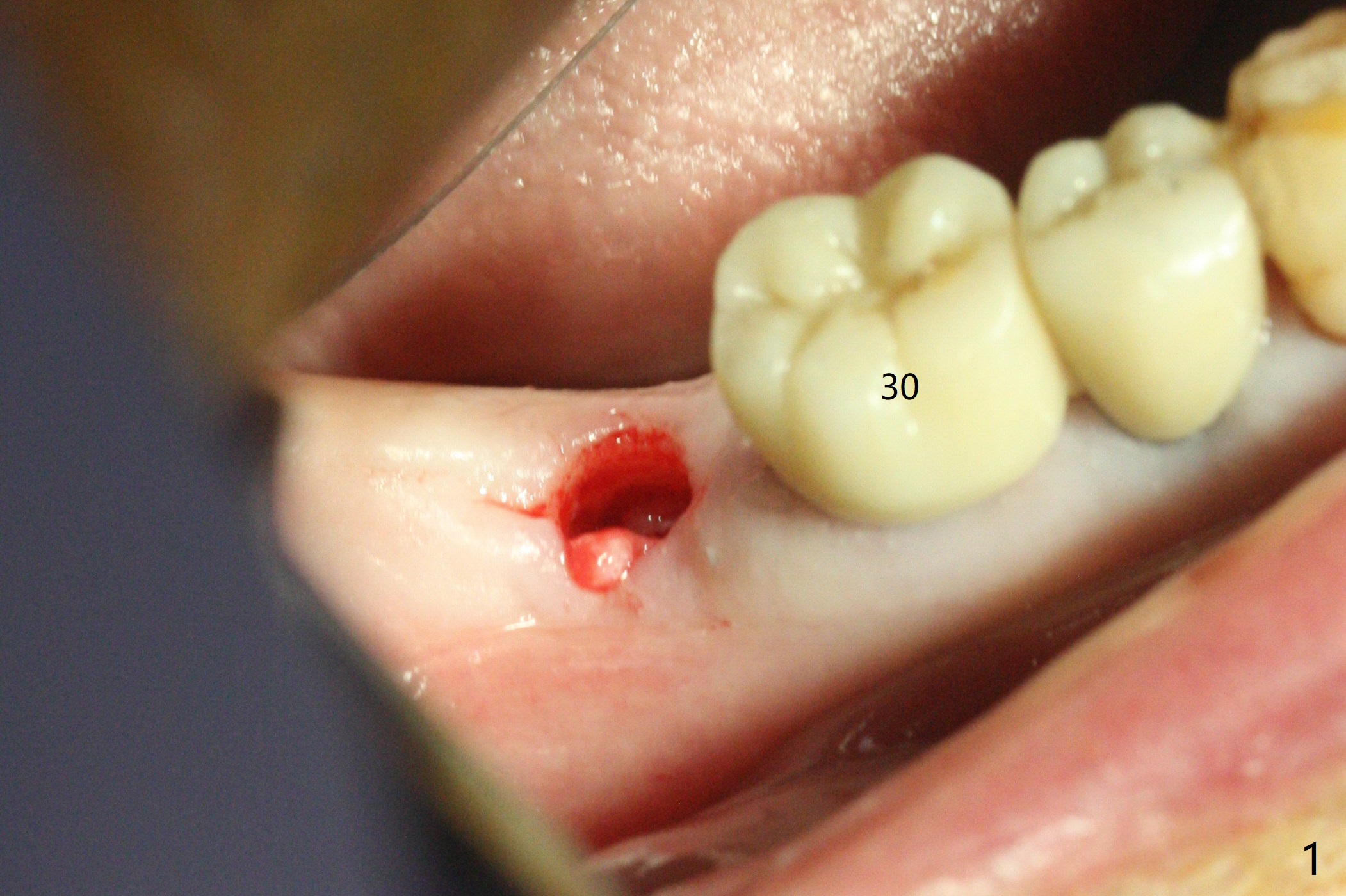
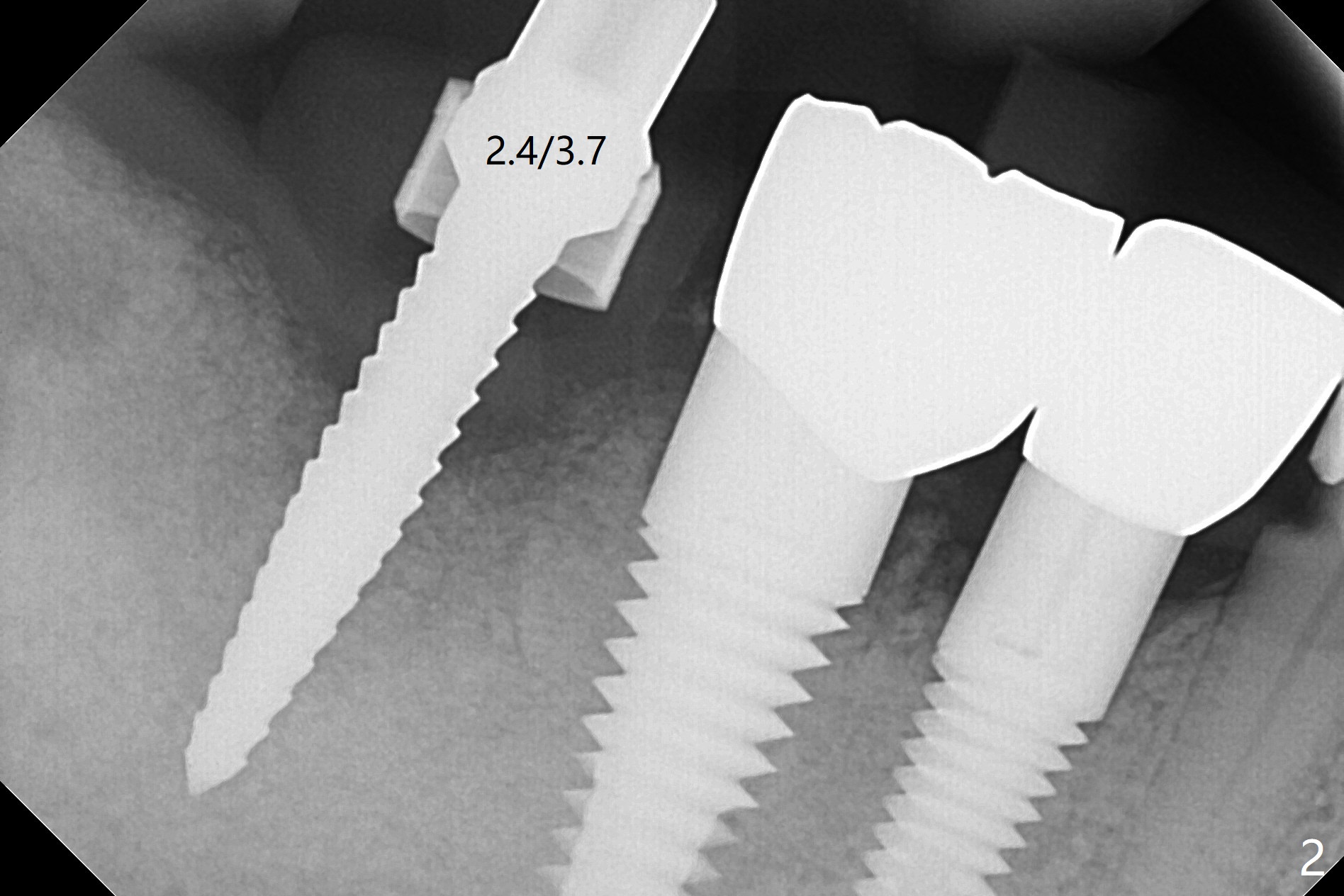
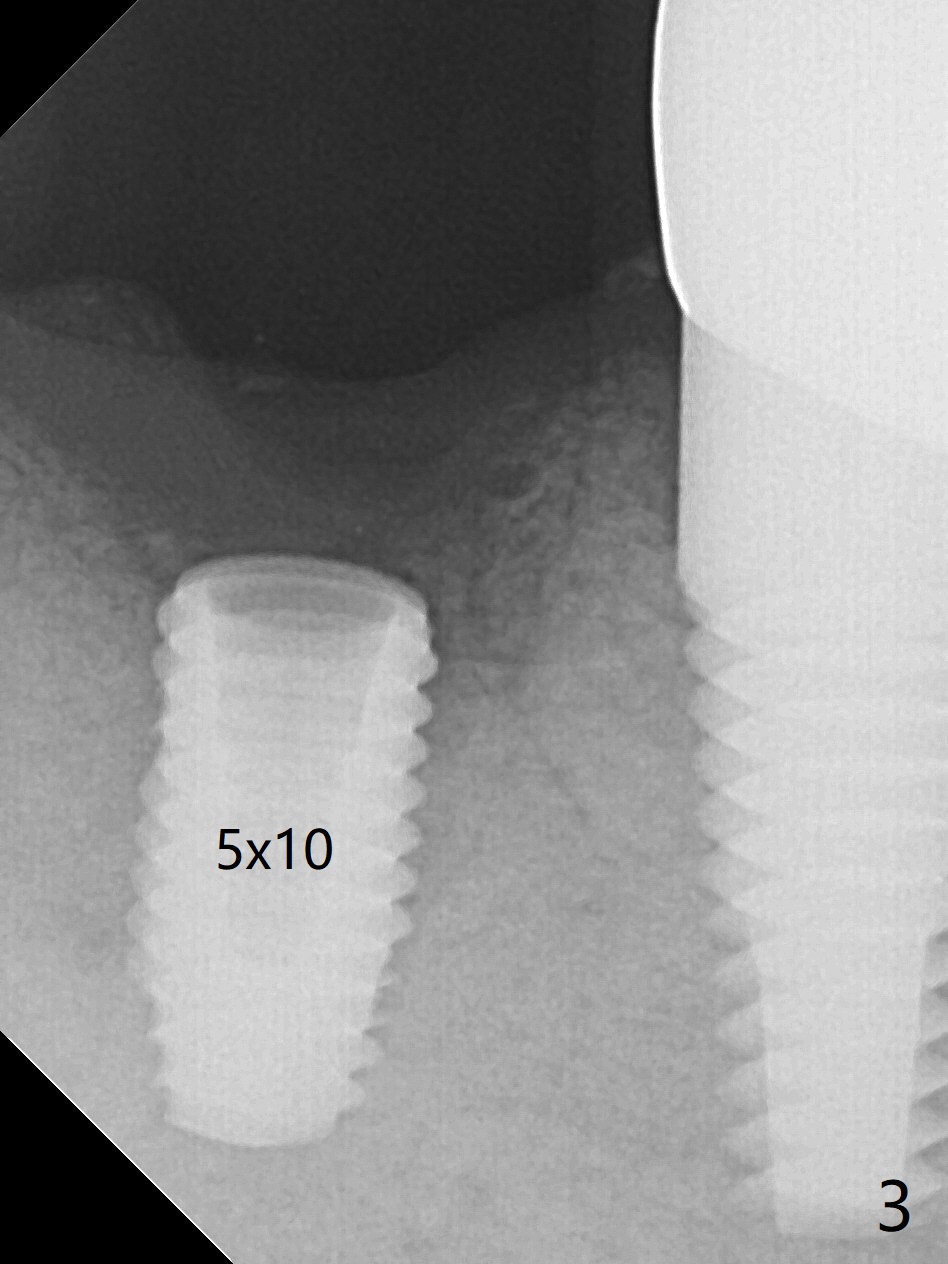
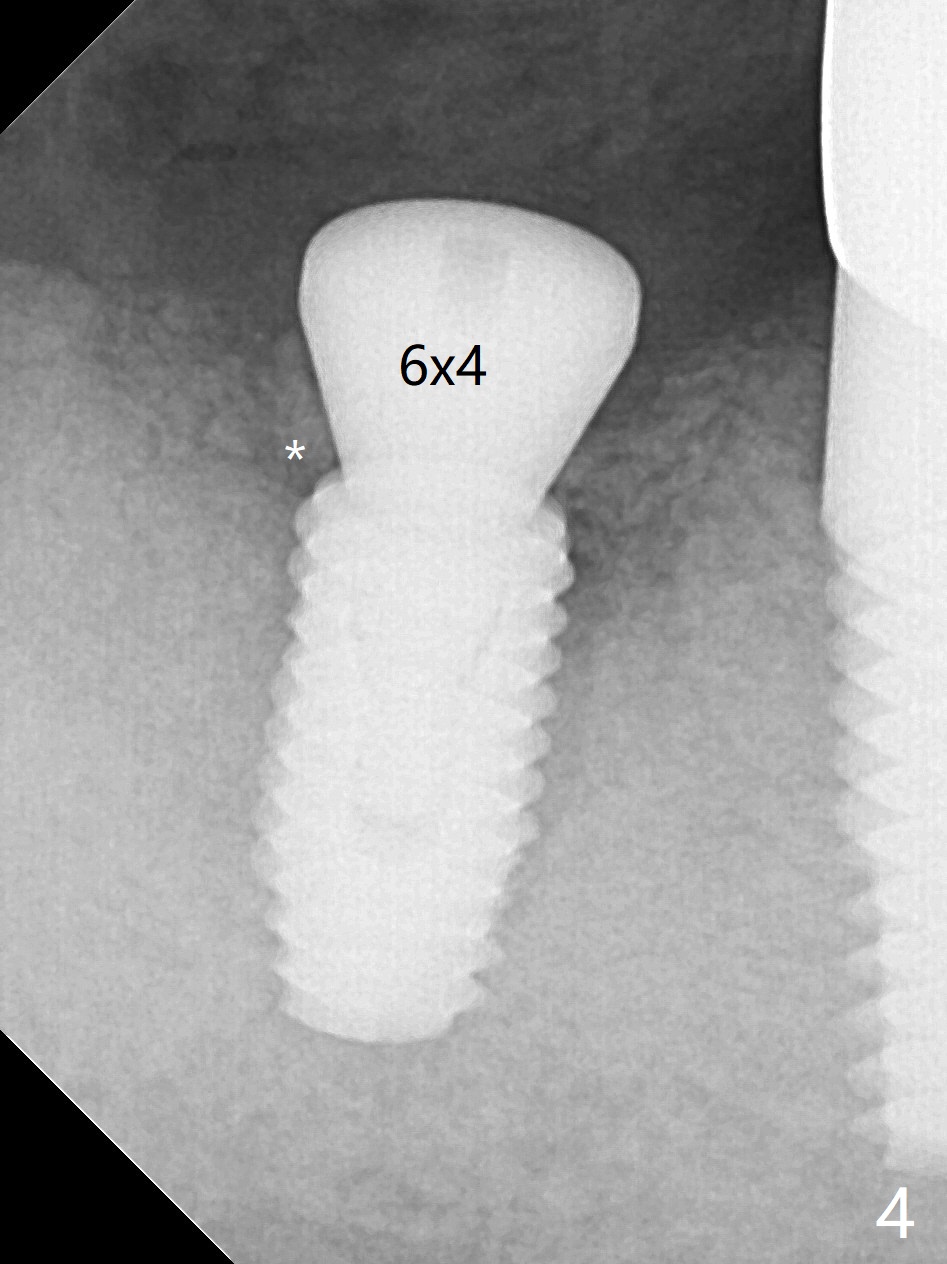
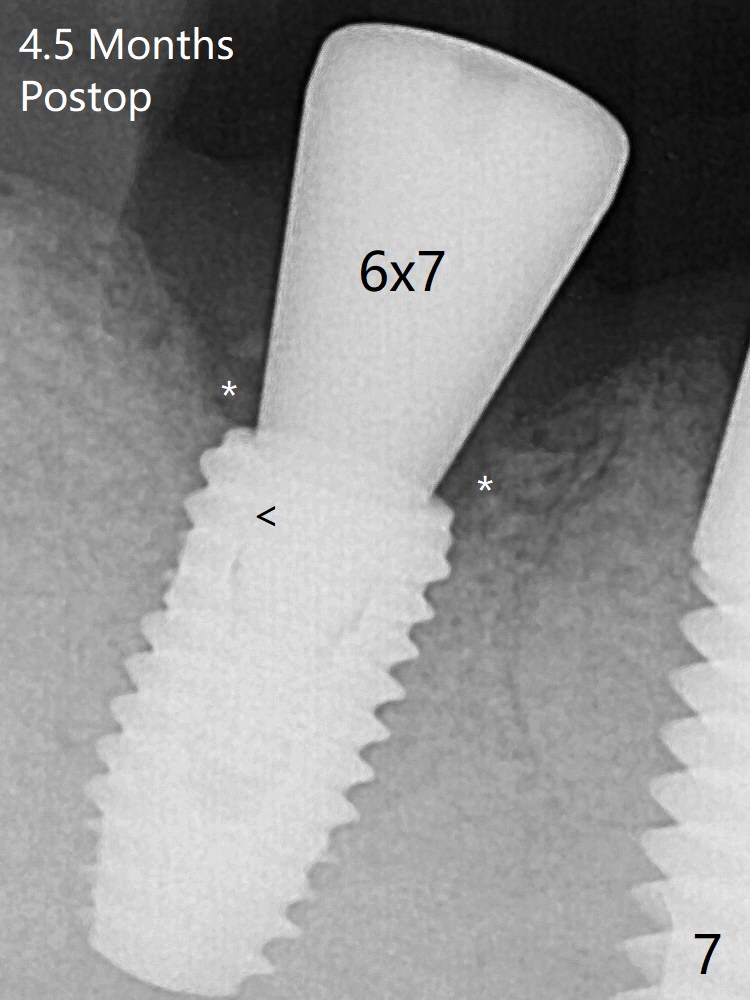
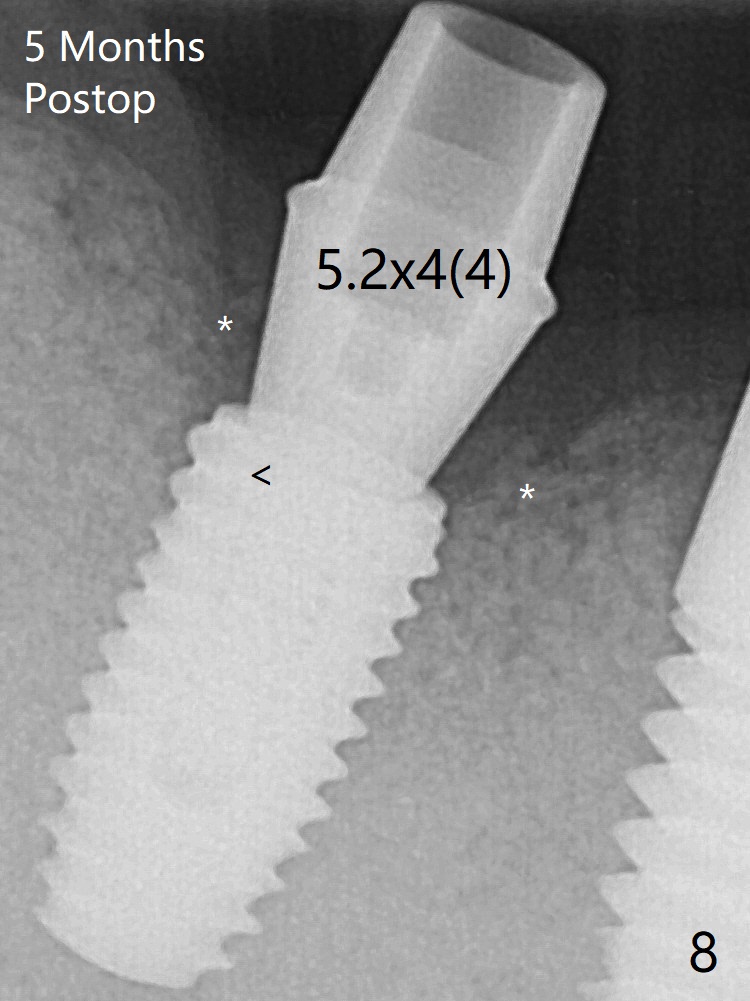
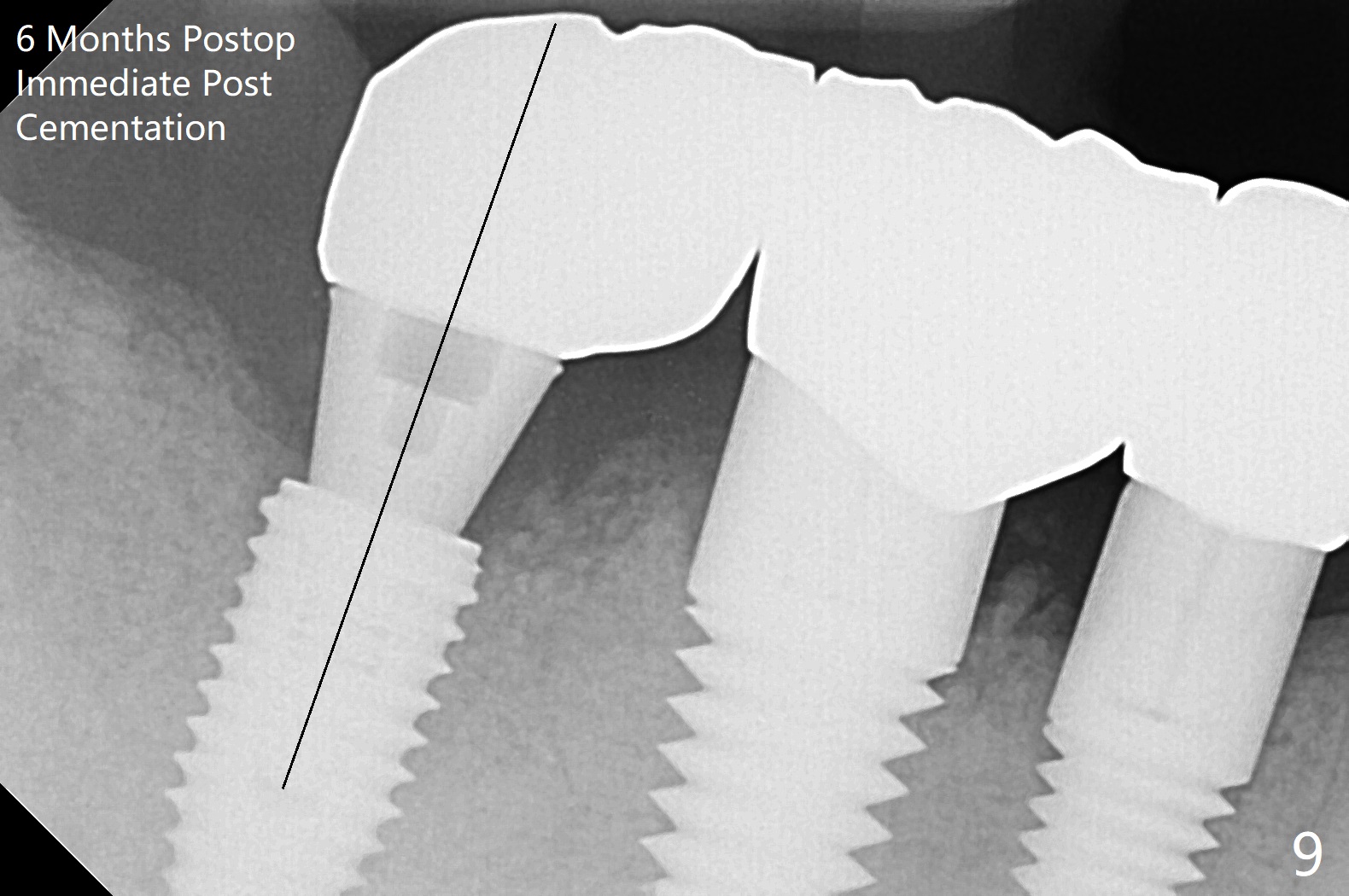
After 2.2x10 mm drill at #31 (Fig.1), bone expansion is conducted with 1.7/3.1 mm and 2.4/3.7 mm Expanders with guide (Fig.2) and 3.0/4.4 mm one without guide. Guided surgery resumes as planned to remove the lingual and apical bone. The buccal bone looks porous from the osteotomy opening. Mixture of autogenous and allograft is packed against the bone plate from the osteotomy before implant placement, but the 5x10 mm implant is unable to be seated completely. After removal of the bone graft from the osteotomy site and use of 4x11.5 mm drill for ~ 1 mm, the implant is seated with ~ 60 Ncm (Fig.3). With buccal incision, bone graft is placed over the distobuccal exposed implant thread (Fig.4 *) following placement of a 6x4 mm healing abutment. Oozing from the wound (thrombocytopenia) is controlled by Polysyn suture and perio glue (Fig.5). The mesial wound dehiscences 7 days postop when DO composite is placed at #28 (Fig.6). Two days later the patient returns because of hemorrhage in brushing. After placement of a taller healing abutment (6x7 mm) with triple antibiotic ointment (although the gingiva cuff is healthy), periodontal dressing is applied. Then the wound heals. The longer healing abutment remains seated (Fig.7 <) without interference from the crest (*) 4.5 months postop. A smaller cemented abutment (5.2x4(4) mm) is chosen with the same outcomes (well seated without gap (Fig.8 < between the implant and abutment), clearance from the crest (*)) 5 months postop. The final crown is cemented 6 months postop with distal access hole (Fig.9 black line), which may be related to design using normal 2nd molar tooth. In fact this patient has small teeth.
Return to Lower Molar Immediate Implant, Trajectory II
Xin Wei, DDS, PhD, MS 1st edition 08/01/2019, last revision 02/04/2020