


Periimplantitis (Protocols, Table), Armaments, Clindamycin
Xin Wei, DDS, PhD, MS 1st edition 09/29/2017,
last revision 06/18/2018
 |
 |
 |
 |
 |
 |
 |
|
 |
 |
Return to
Lower
Molar Immediate Implant, Prevent
Molar Periimplantitis (Protocols, Table), Armaments, Clindamycin Xin Wei, DDS, PhD, MS 1st edition 09/29/2017, last revision 06/18/2018 |
|
Bone or Tissue-level Implant?
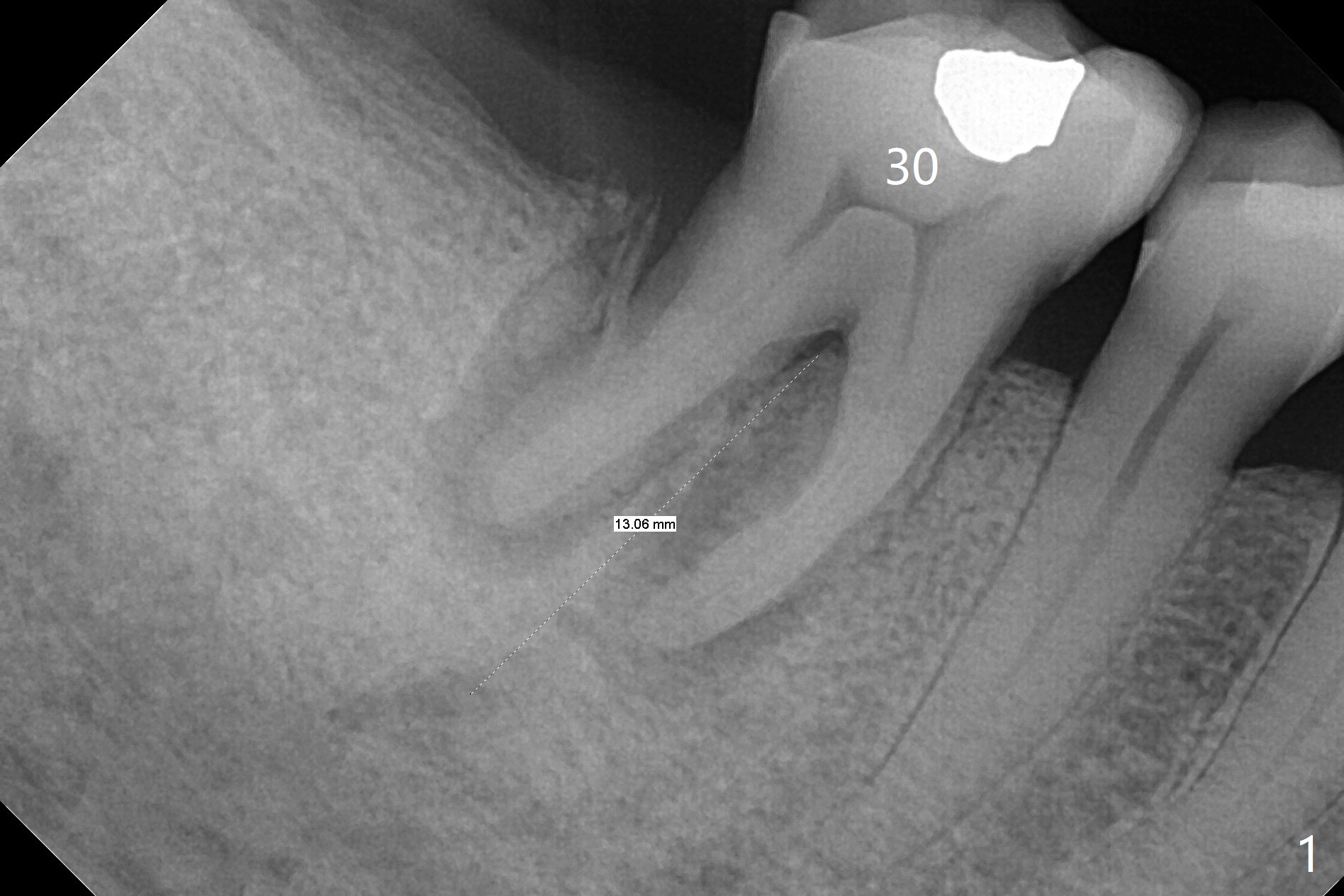
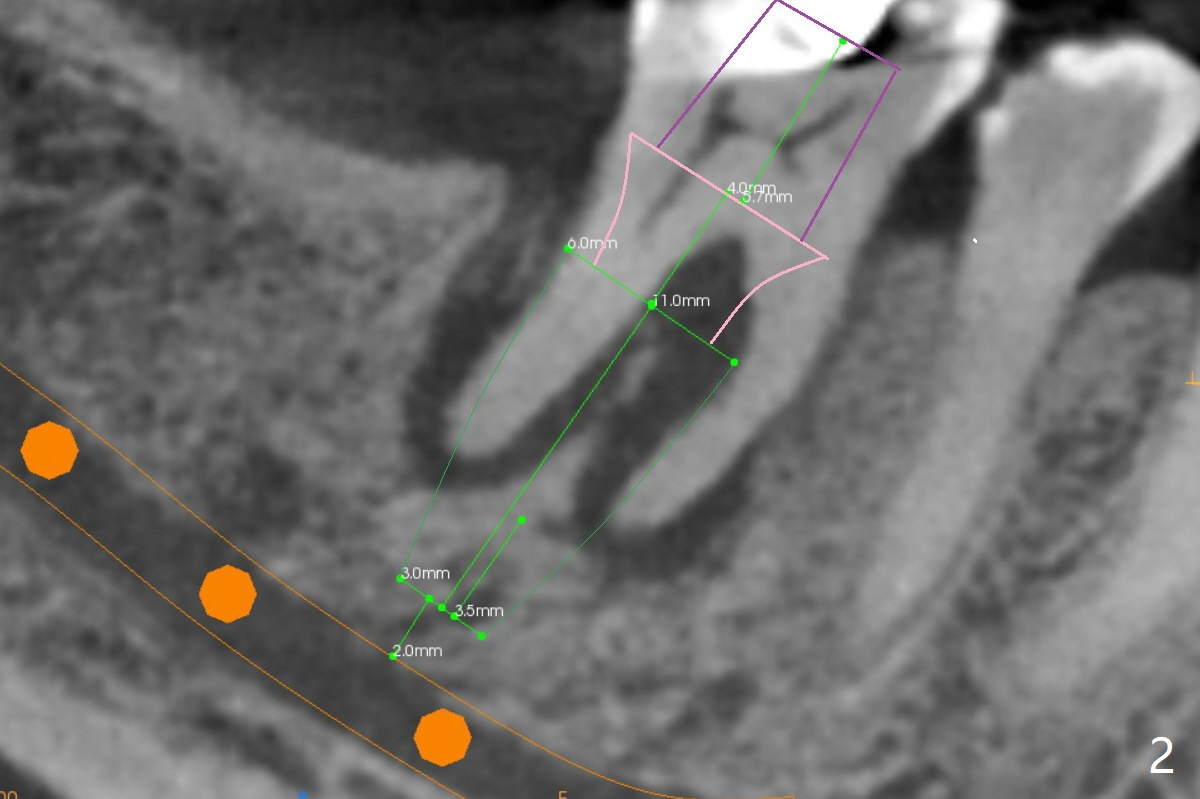
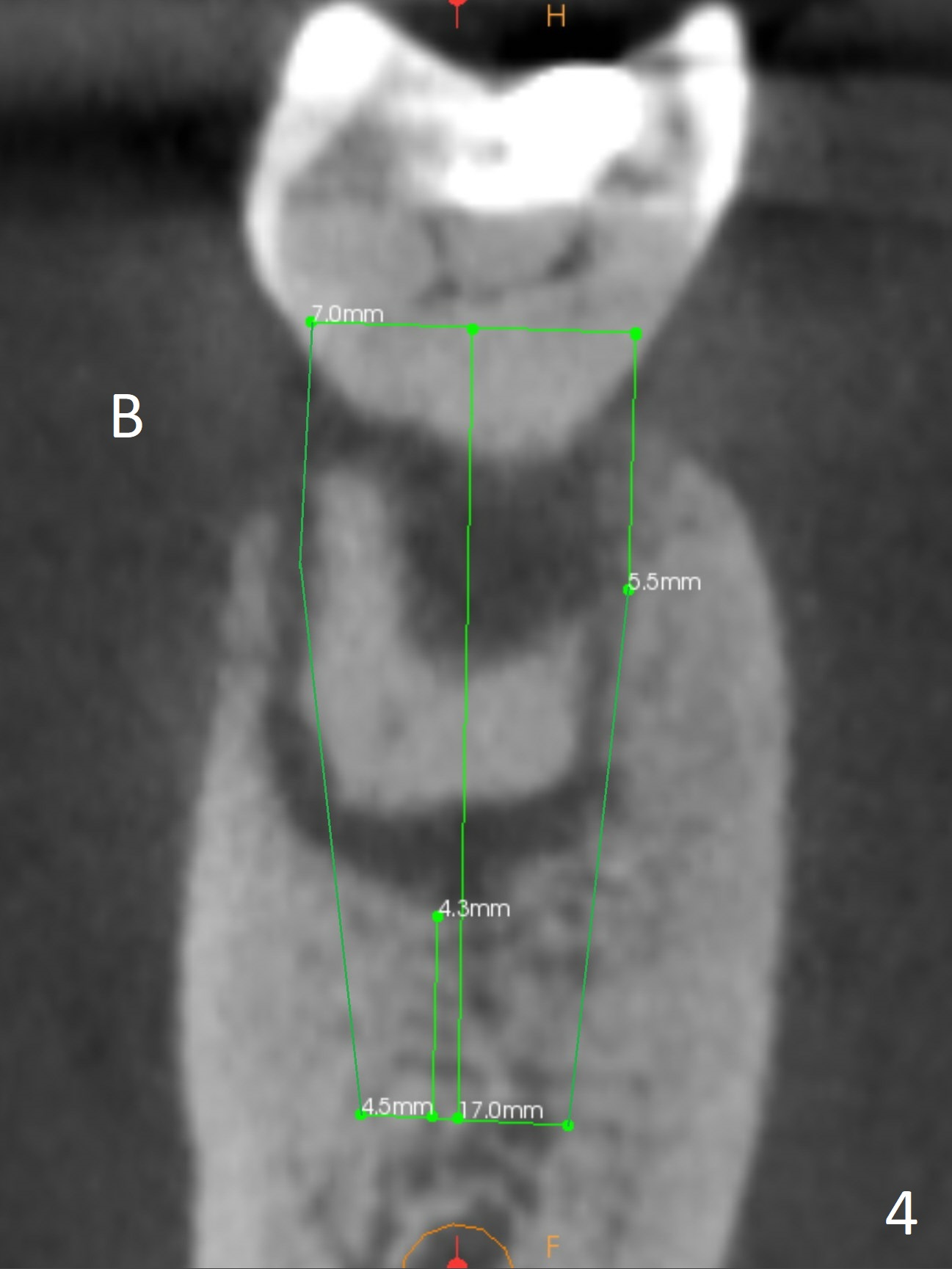
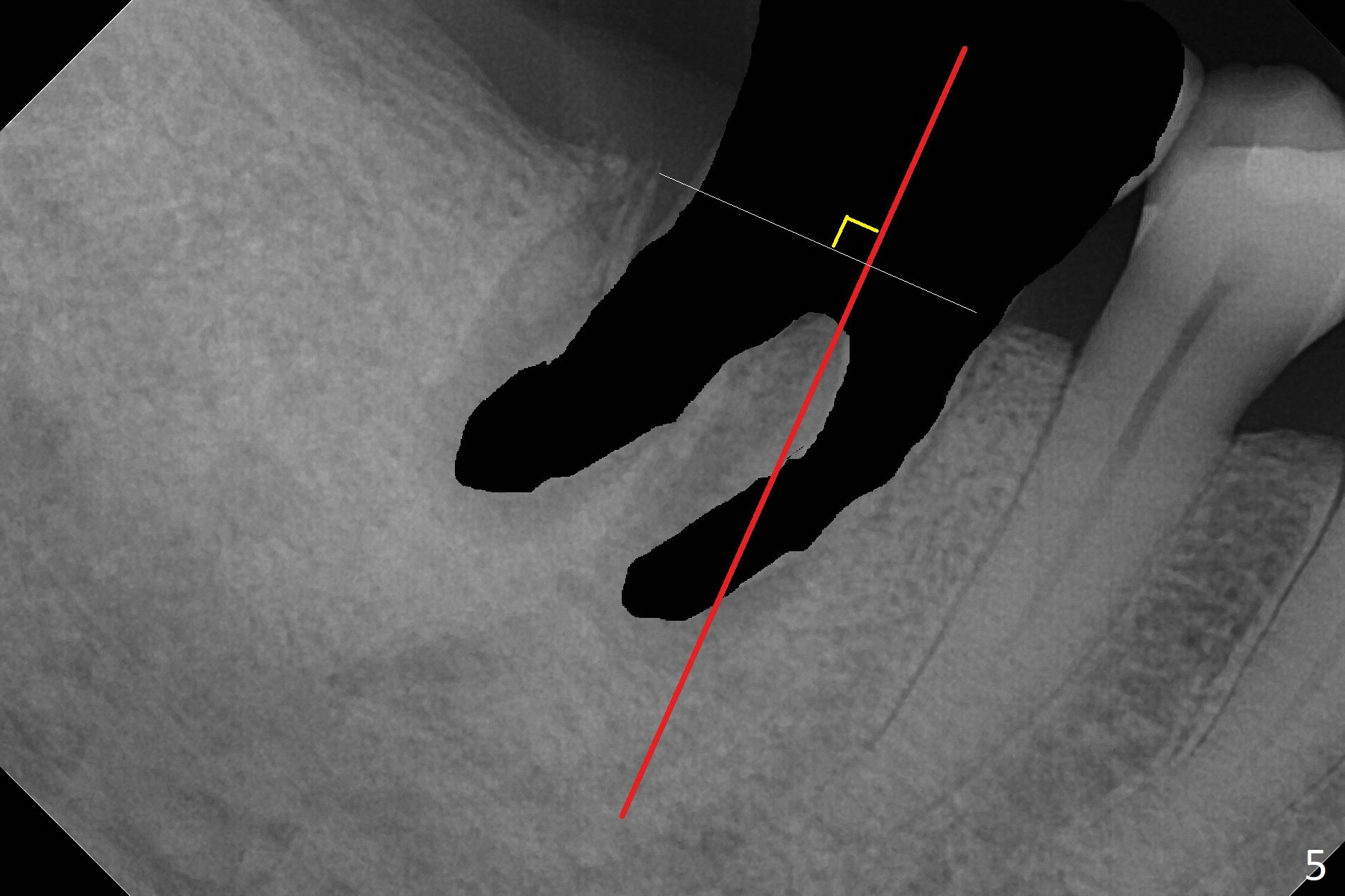
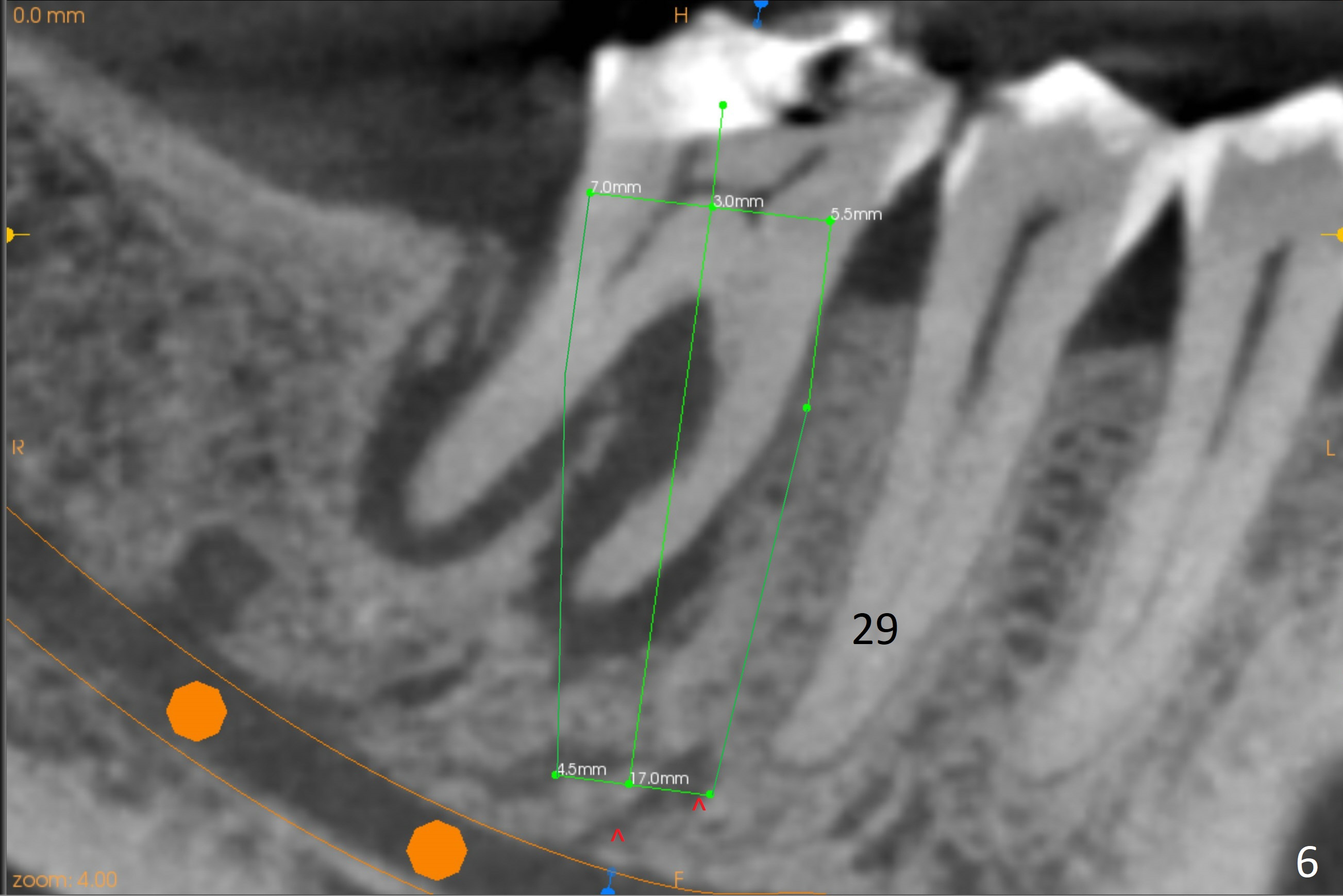
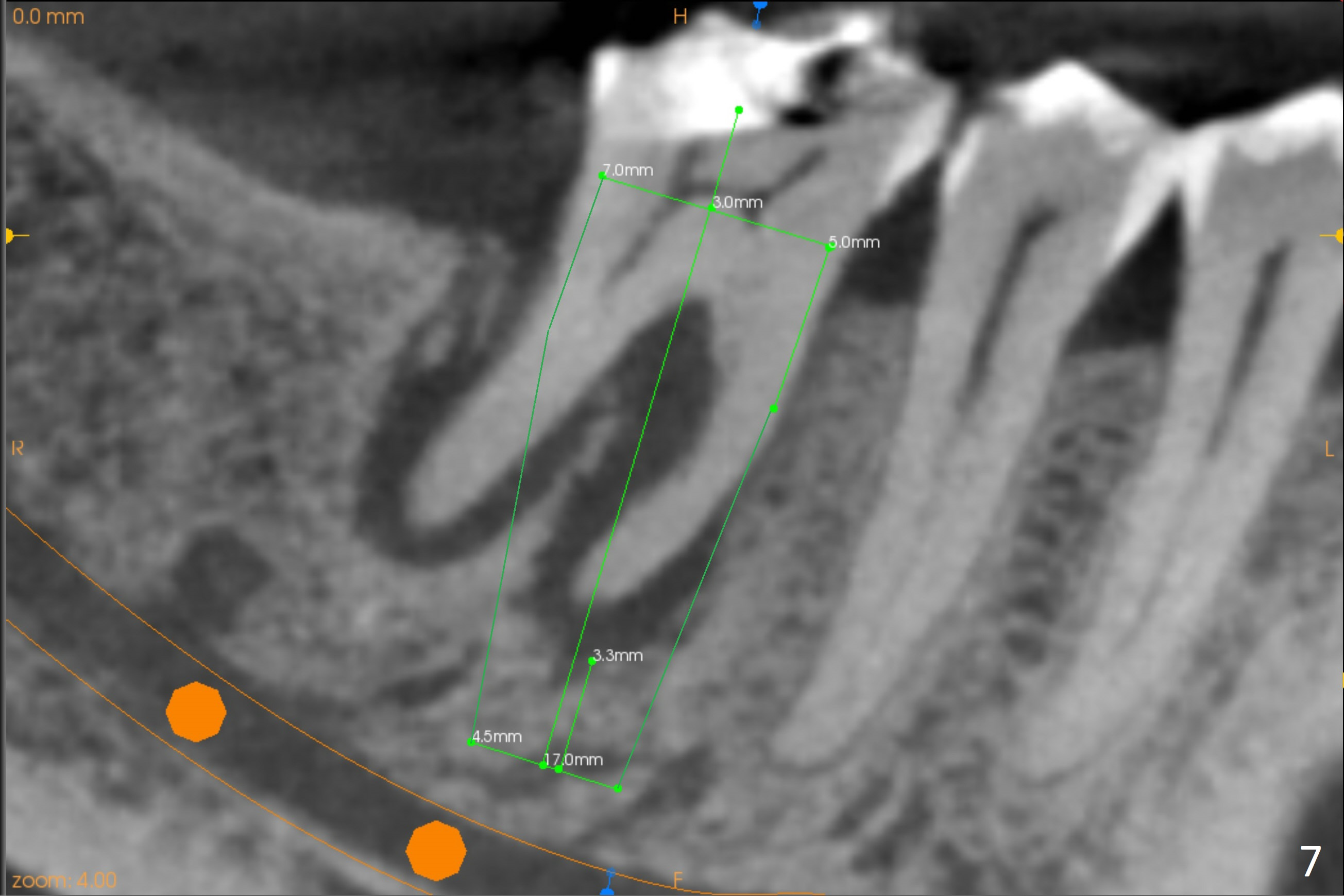
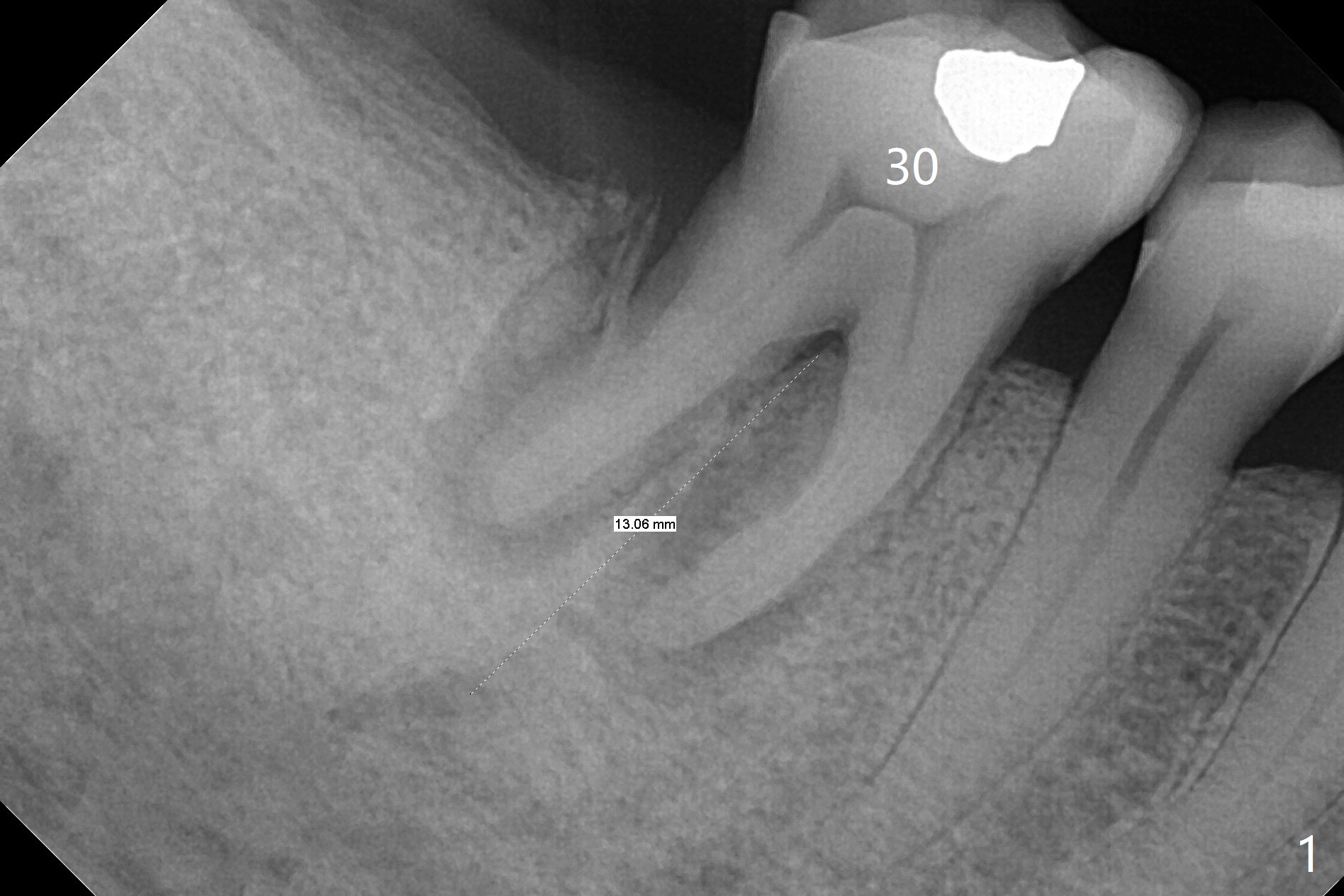
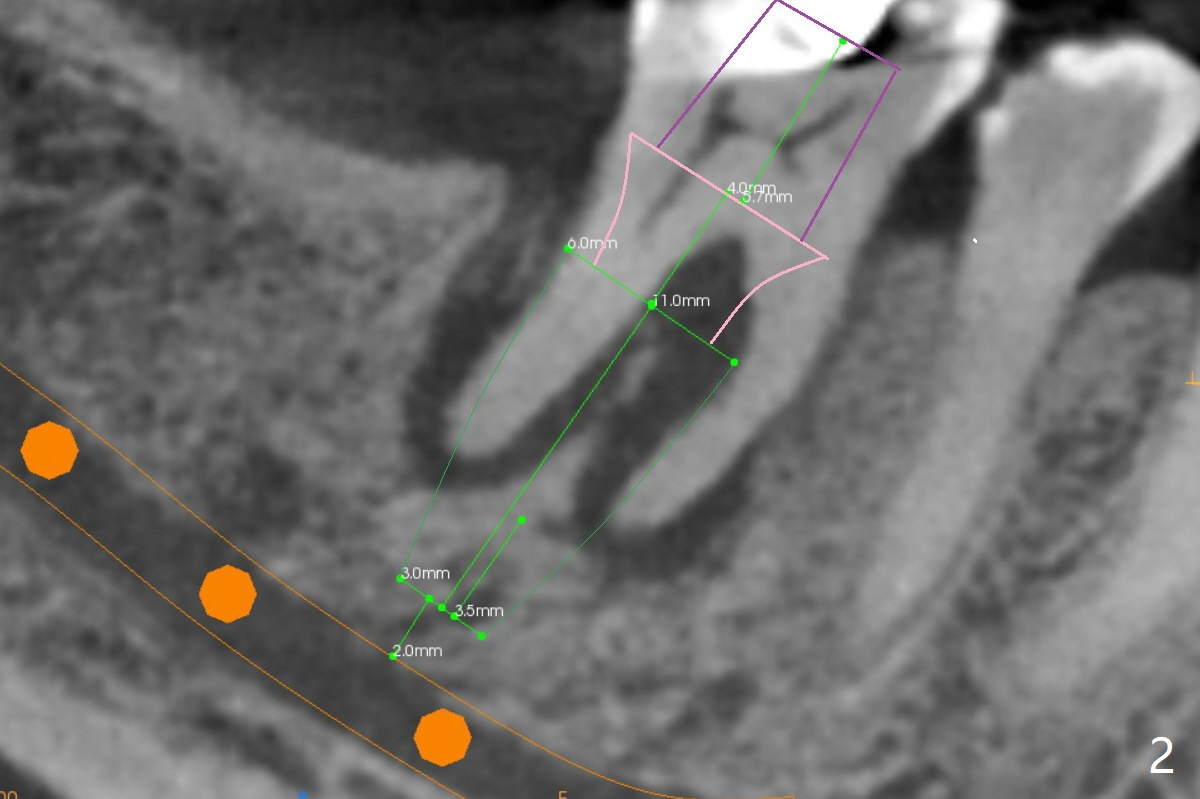
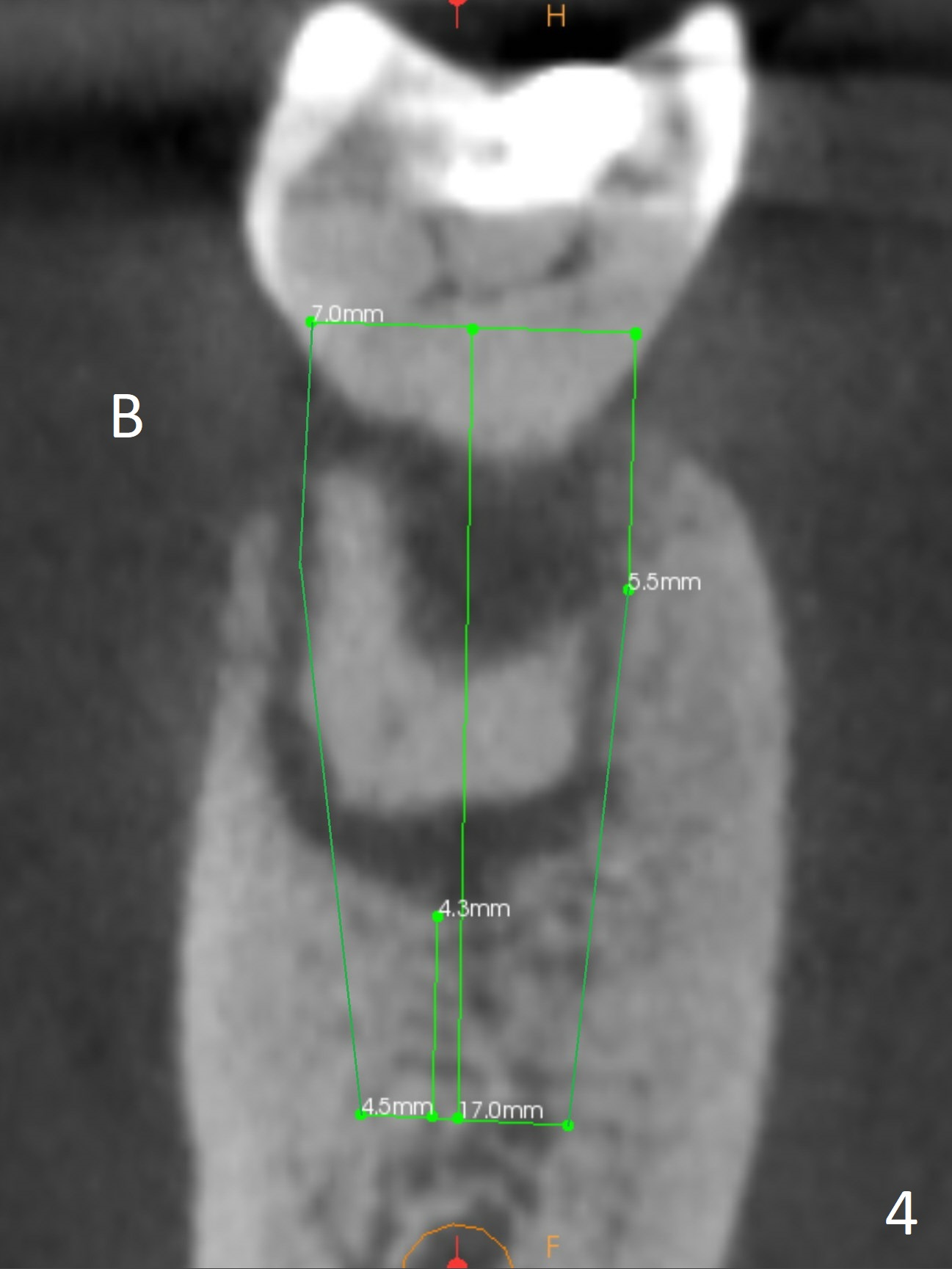
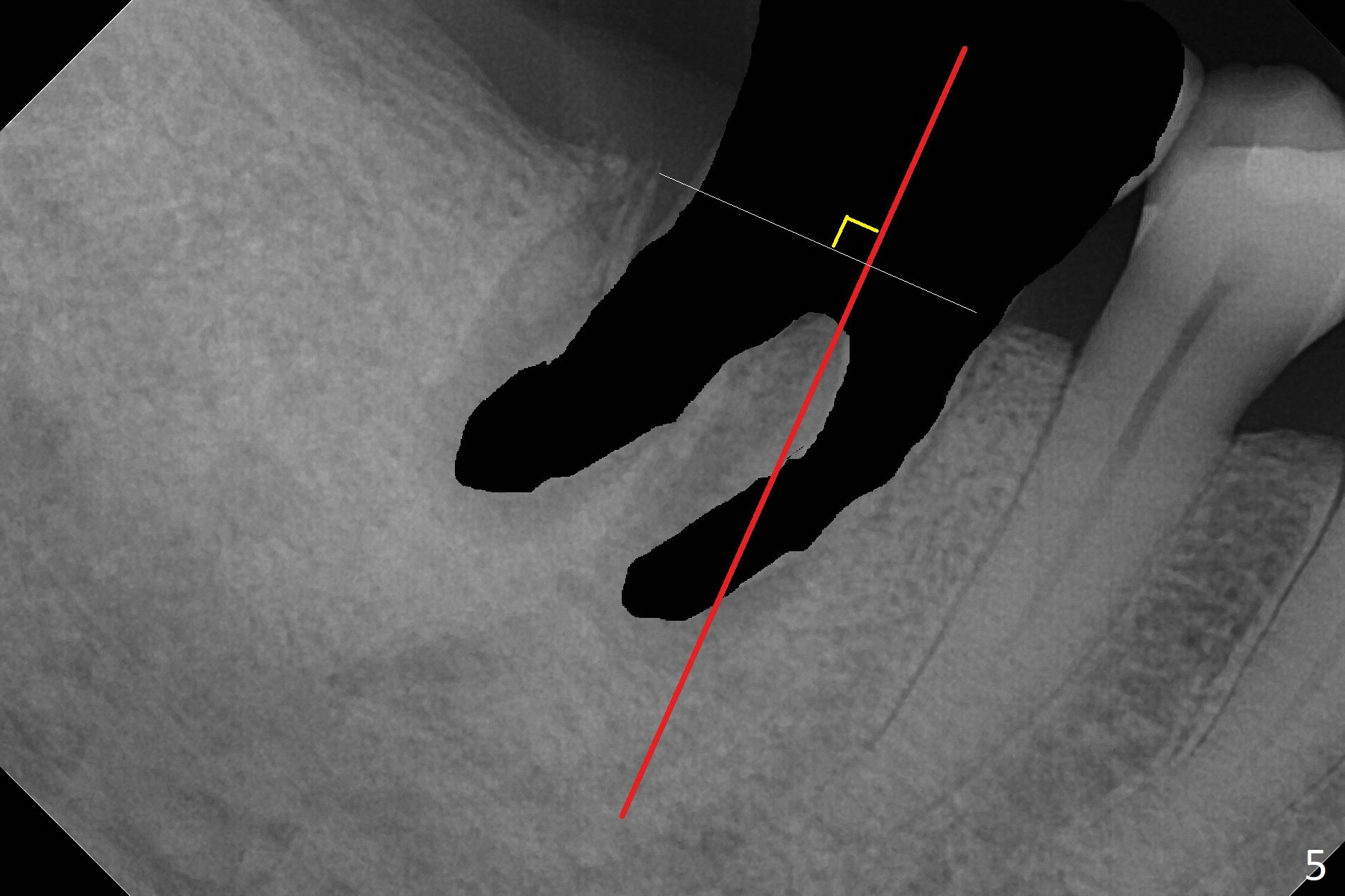
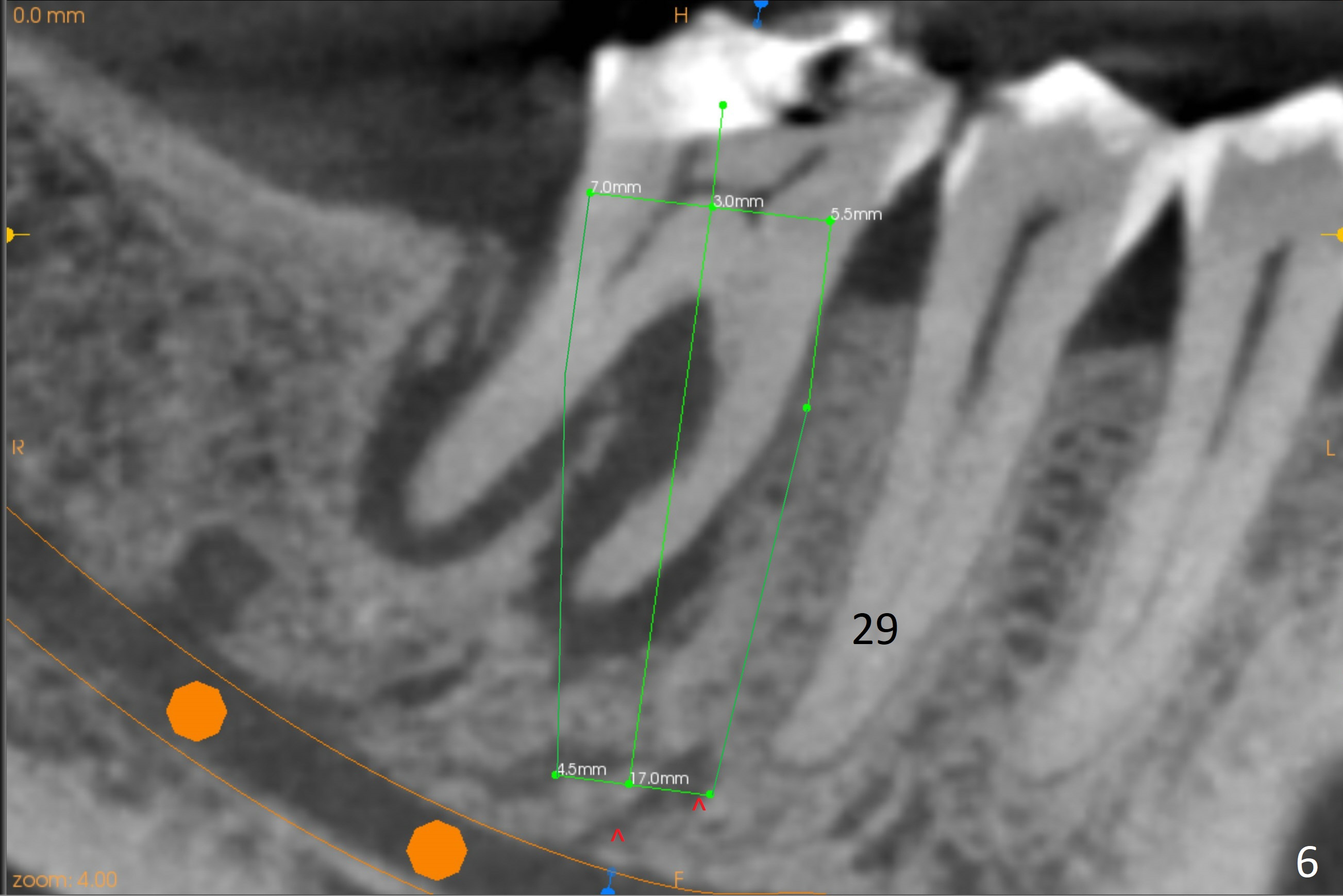
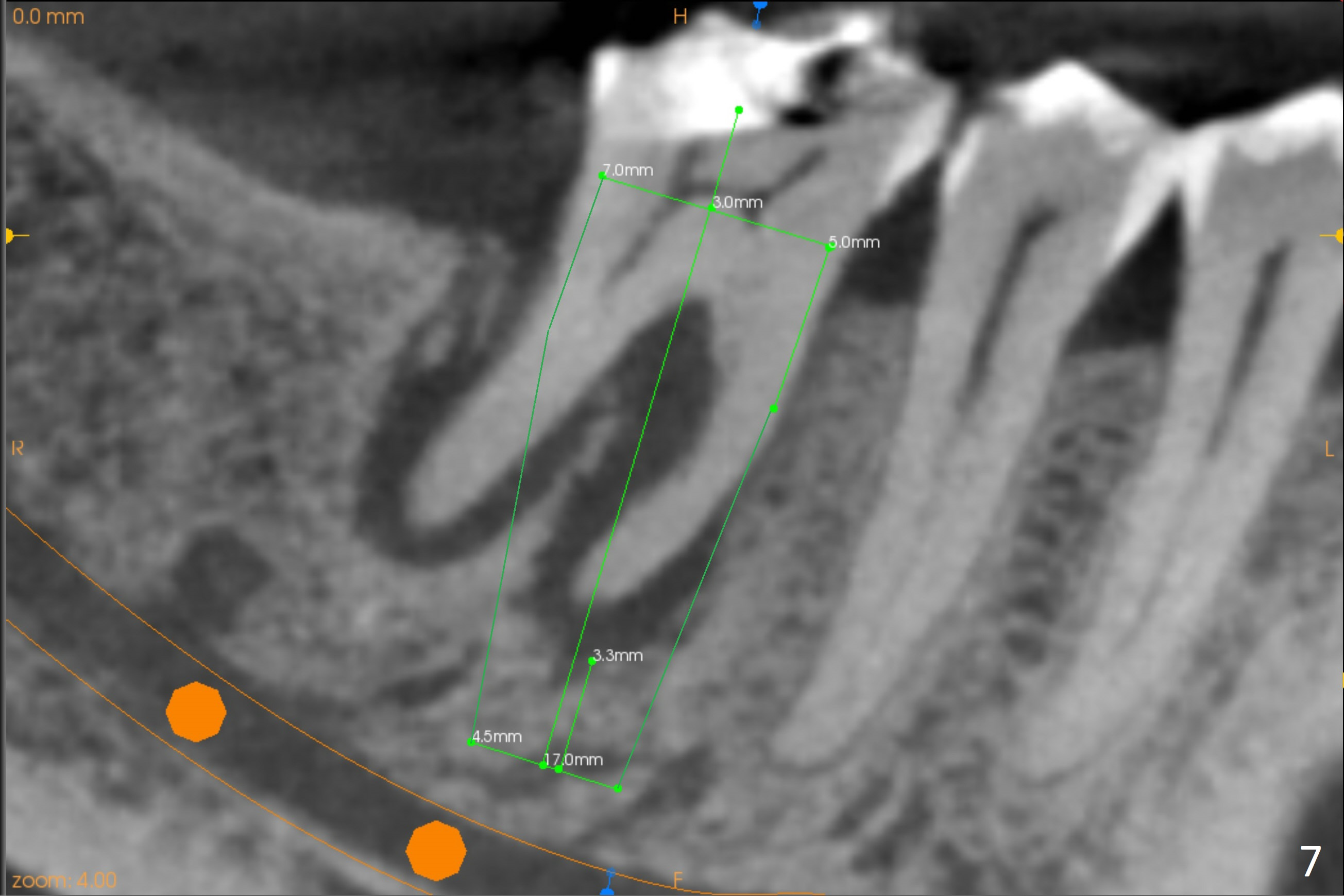
A 71-year-old woman (bruxer) wants to remove the tooth #30 (occlusal trauma, possible root fracture) for implant following the one at #14 (Fig.1). IBS abutment screw tends to loosen in functioning if the implant is placed too deep and/or off the longitudinal axis. If these two conditions are not controlled well, switch to a large tissue-level implant. A drawback of placing the implant in the septum is that the mesial margin of the abutment (Fig.2 pink) is subcrestal. If the implant is placed in the mesial socket (Fig.5 red line), the imagined abutment margin plane (white line) is parallel to the mesiodistal crests. Initial osteotomy entry point in the mesial socket and trajectory should be adjusted intraop (compare Fig.6 and 7) so that the apex of the implant will not be too close to the apex of the tooth #29 (to avoid truncating the neurovascular supply to the tooth (Fig.6 red arrowheads)) at the same time the abutment inclination is not too compromised (Fig.7). To prevent pressure upon the buccal (Fig.4 B) plate, osteotomy should be slightly lingual and/or the diameter of the implant is to be < 7 mm. Use a 3 mm unipost for provisional and probably 5 mm one for definitive restoration. Apply bonding to the post if the implant is 6 mm or less. The provisional margin should be wide and deep for deep margin and easy impression later. Use IS drills with 4 mm stopper for osteotomy if the septum is absent. Prepare Rongeur and surgical handpiece to remove the remaining septum if needed. Be wary of the distally curved root tip of #29. In fact there is a mesiodistal crack line (Fig.8 arrowheads) with buccal recession (Fig.9, 2 weeks preop).