_original%20design.jpg)

 |
_original%20design.jpg) |
 |
 |
 |
, |
Improvement of Immediate Implant with Periodontitis
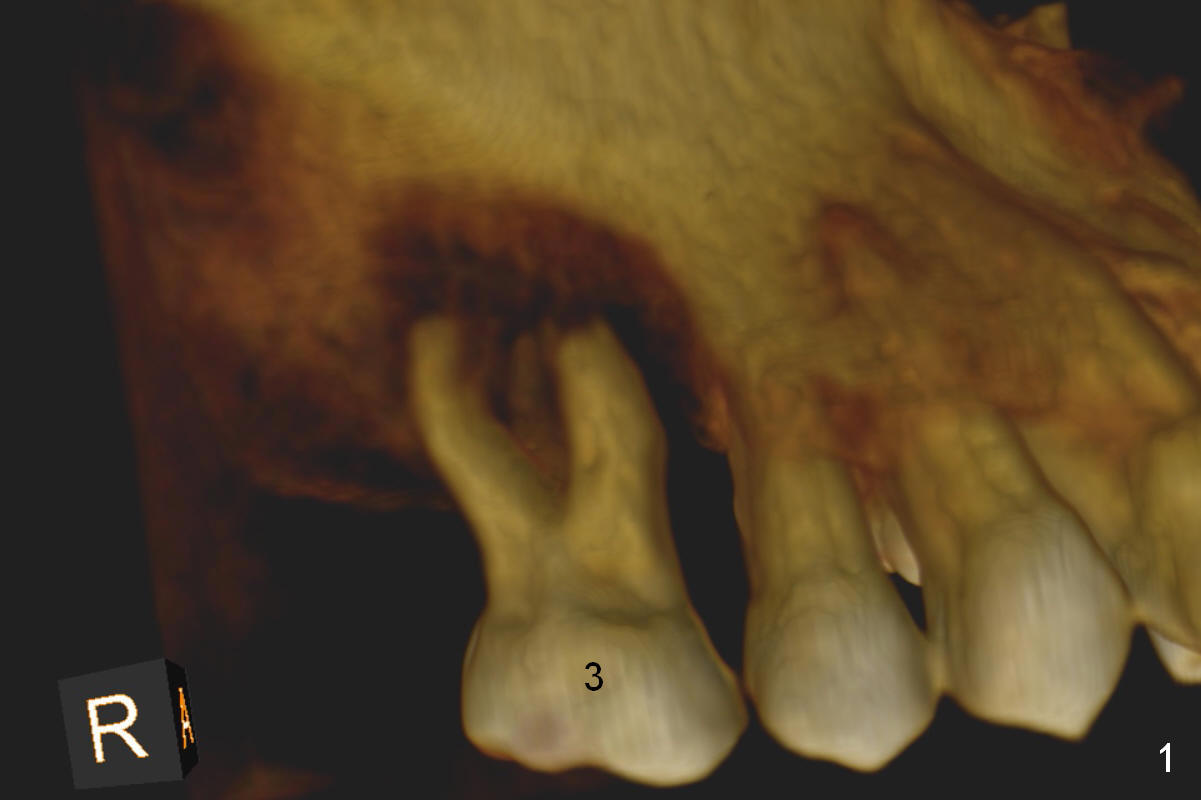
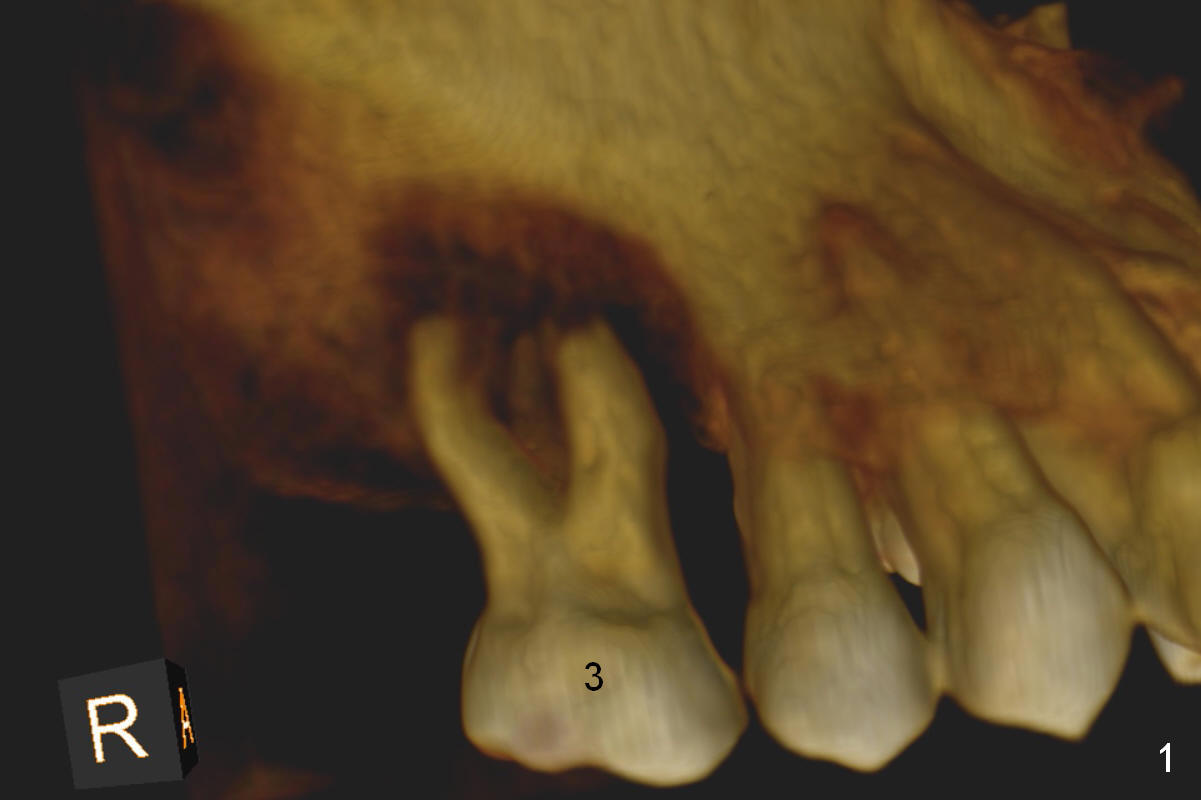
It may take 6 months for #19 implant re-placement after socket preservation. The tooth #3 is symptomatic (Fig.1). In spite of implant failure at #19, the best treatment for #3 of the same patient is still immediate implant. Previous practice is to place an implant as long as possible (Fig.2). The coronal threads are not covered by the native bone. Bone graft (red circles) cannot guarantee thread coverage. Periimplantitis may develop more likely in periodontitis patients if bone graft is not tightly packed.
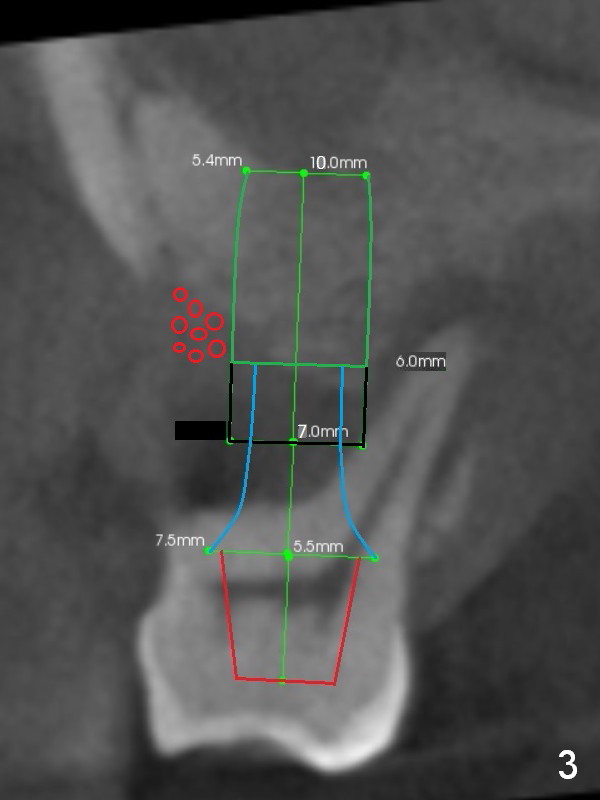
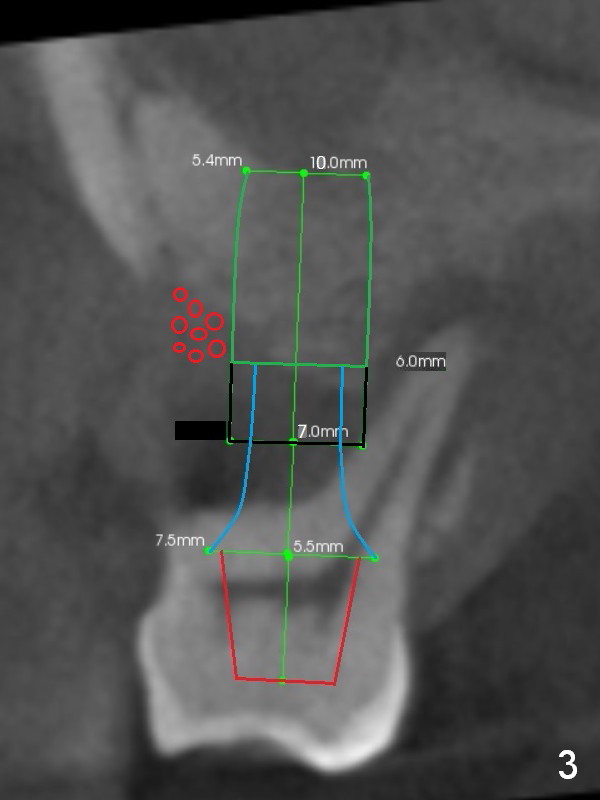
A safe method is to use a shorter implant and place it as deep as possible so that the majority of the threads are subcrestal (Fig.3 green). Pack bone graft tightly (smaller red circles) and also check whether there is a piece of gauze in the socket prior to grafting. The corresponding changes are to place a long abutment with long cuff (7.5x7(5) mm). Bone density is relatively low. Prepare bone expanders.
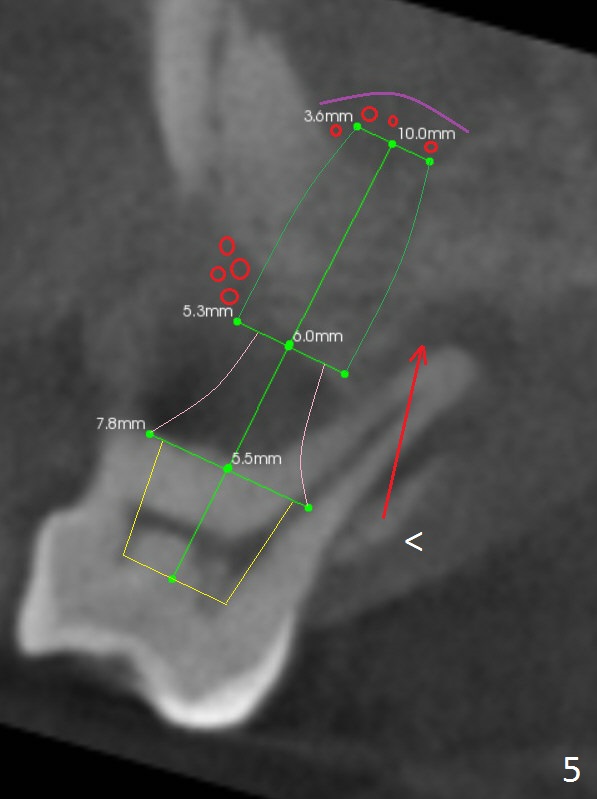
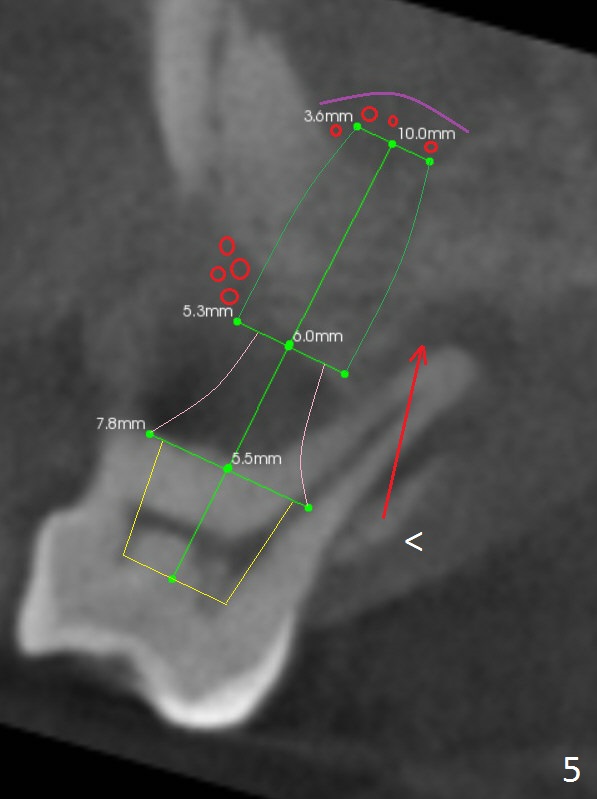
When the crown at #19 is cemented, the tooth #3 is found to have severe buccal recession (Fig.4). A 5.3x10 mm implant is not only placed deep, but also palatal (Fig.5, Clindamycin). An abutment will be selected with the longest cuff (6 mm (pink)). To make the palatal gingival margin recede, the coronal palatal bone (<) will be broken and pushed to the palatal socket.
Before implant placement, insert PRF plug or membrane (purple curved line) and allograft (red circles). The remaining PRF membranes will be used to cover buccal defect. Draw 4-5 tubes of blood.
Return to
Upper Arch,
Molar Immediate Implant,
Prevent Molar Periimplantitis (Protocols,
Table),
IBS,
19,
9,
23
Buccal Root Exposure
Xin Wei, DDS, PhD, MS 1st edition 06/09/2016, last revision 04/29/2018