














 |
 |
 |
 |
 |
 |
 |
 |
 |
 |
 |
|
 |
 |
 |
|||
 |
 |
 |
|||
 |
 |
 |
 |
||
 |
 |
 |
|||
 |
 |
 |
|||
Buccal Gap Closure
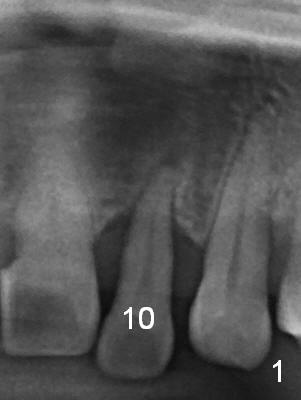
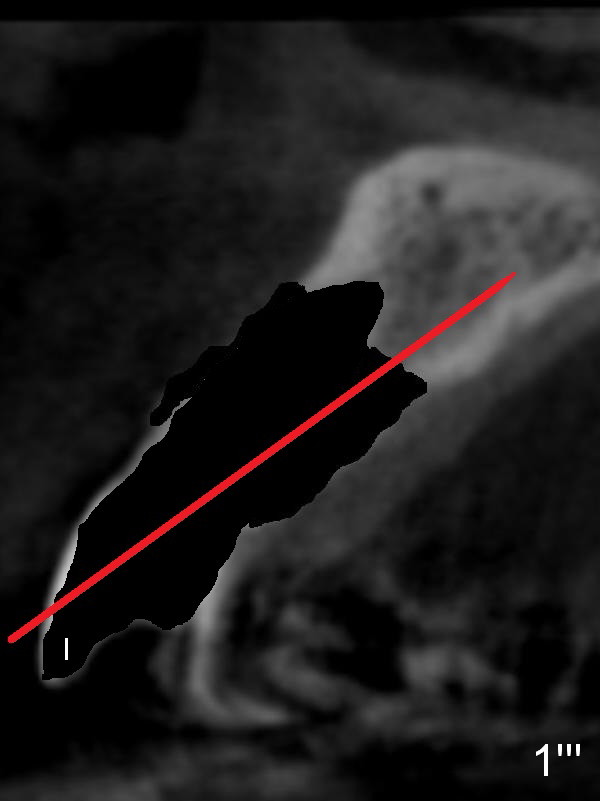
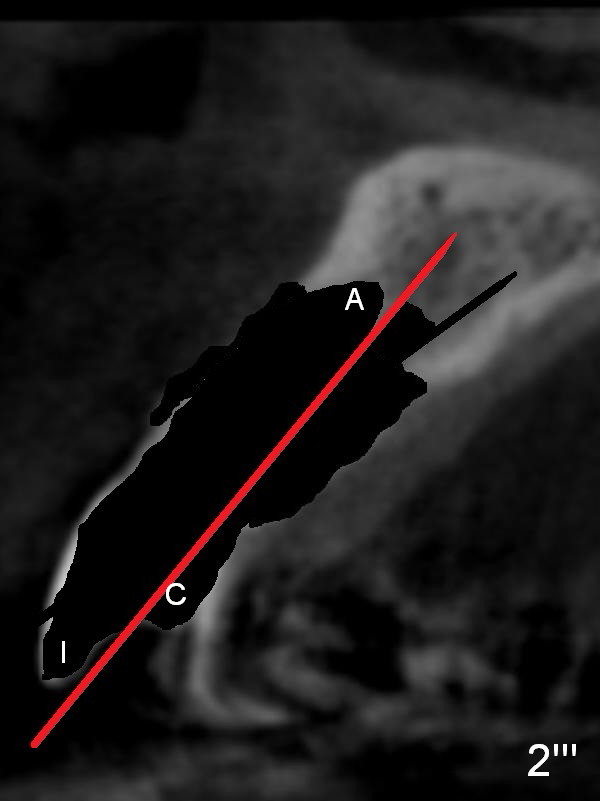
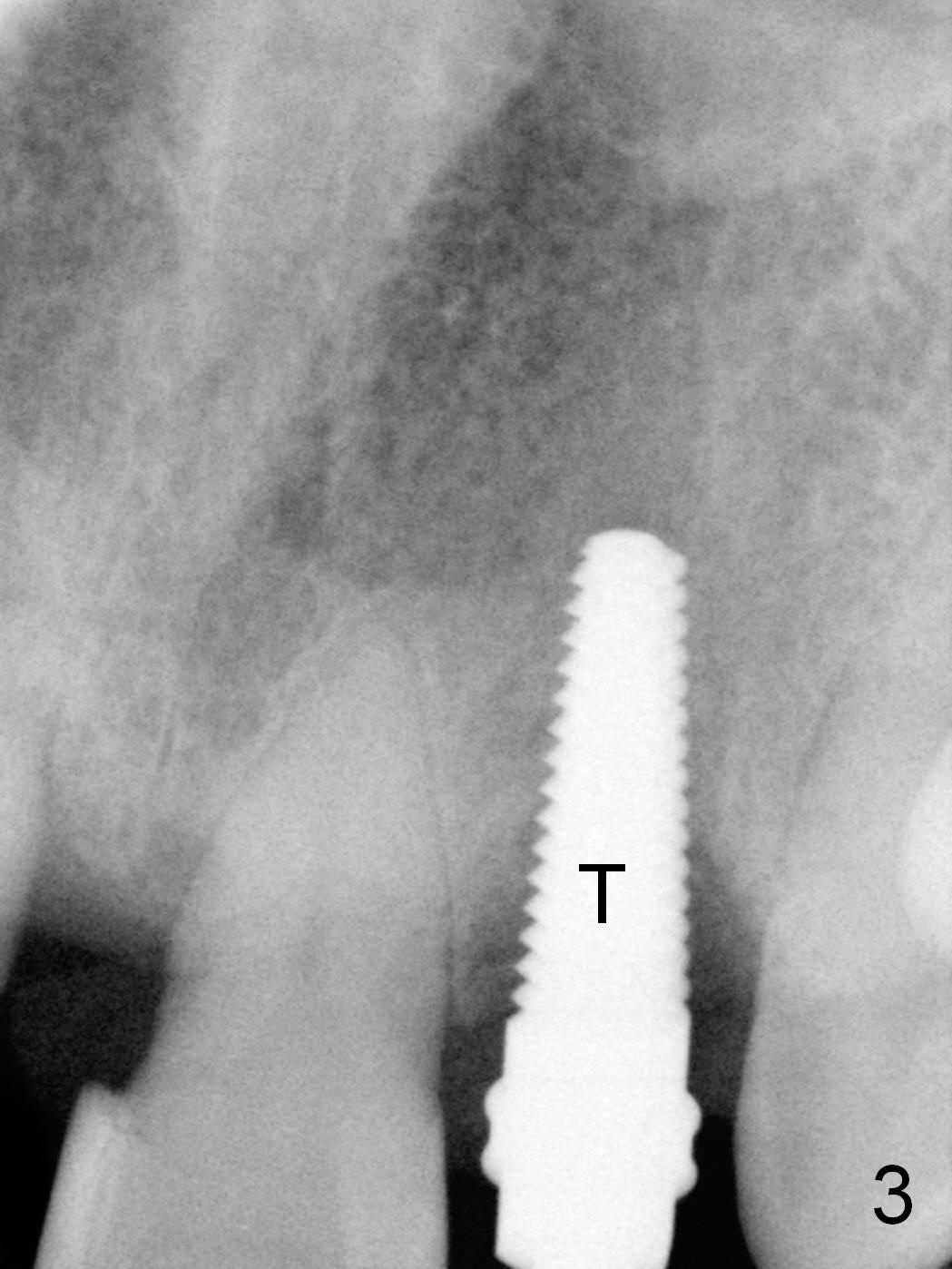
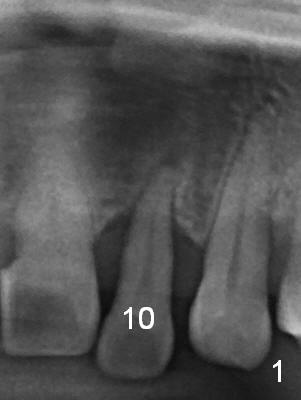
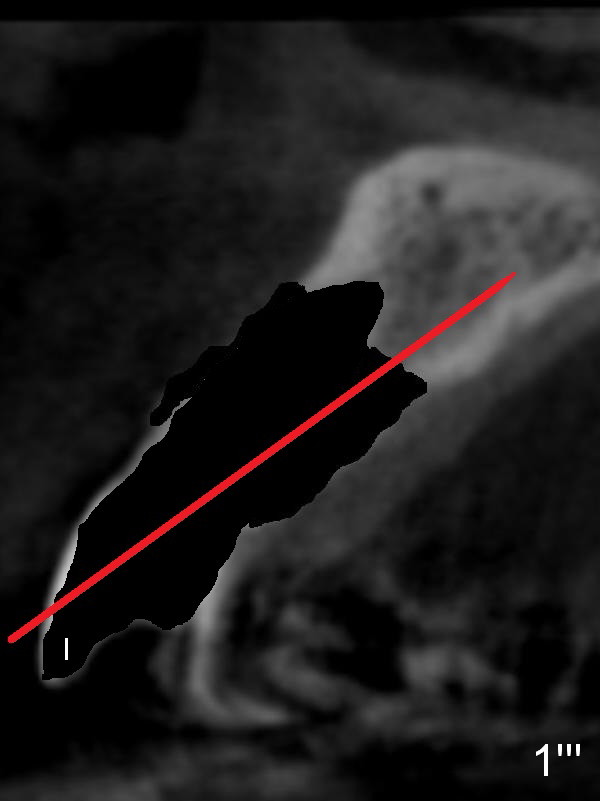
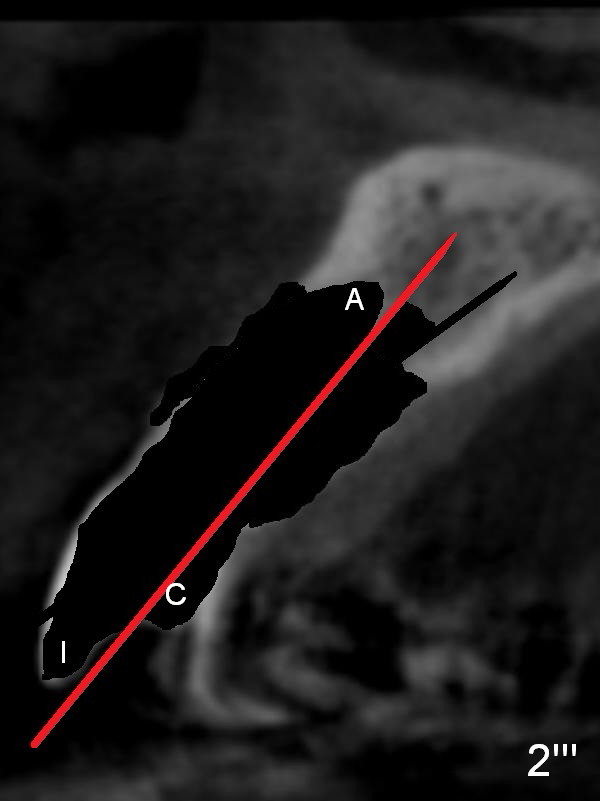
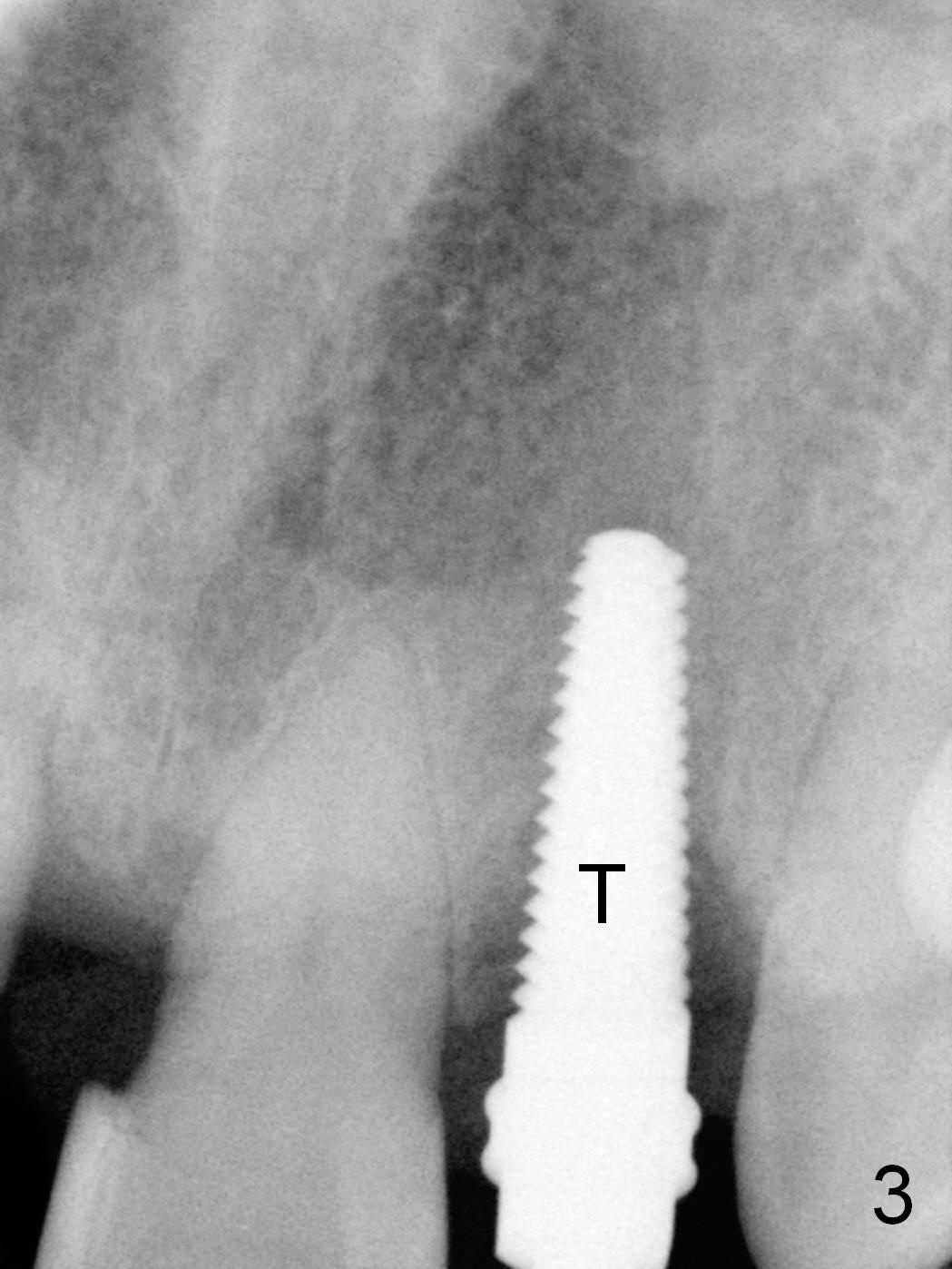
Prior to the surgery, the patient mentions that the future tooth at the site of #10 should not imitate the one in the drifted position (Fig.1). The buccal gingiva is found to be thick. Fig.1',1'' are CBCT cross section of the tooth #10 from another patient with illustrations to show that the palatal (P) bone is flat before (Fig.1') and after (Fig.1'') extraction. Initial osteotomy (Fig.1'' ^; Fig.1''' red line; Fig.2 (PA)) is palatal to the apical socket (A). It appears too palatal. After withdrawing the pilot drill (Fig.2'), a Lindamann bur is used to remove bone (Fig.2'' *) between the initial osteotomy and the apical socket. Ultimately the new osteotomy (Fig.2''' red line) is changed so that it is palatal to the apical socket and the incisal edge and past through the cingulum (C).
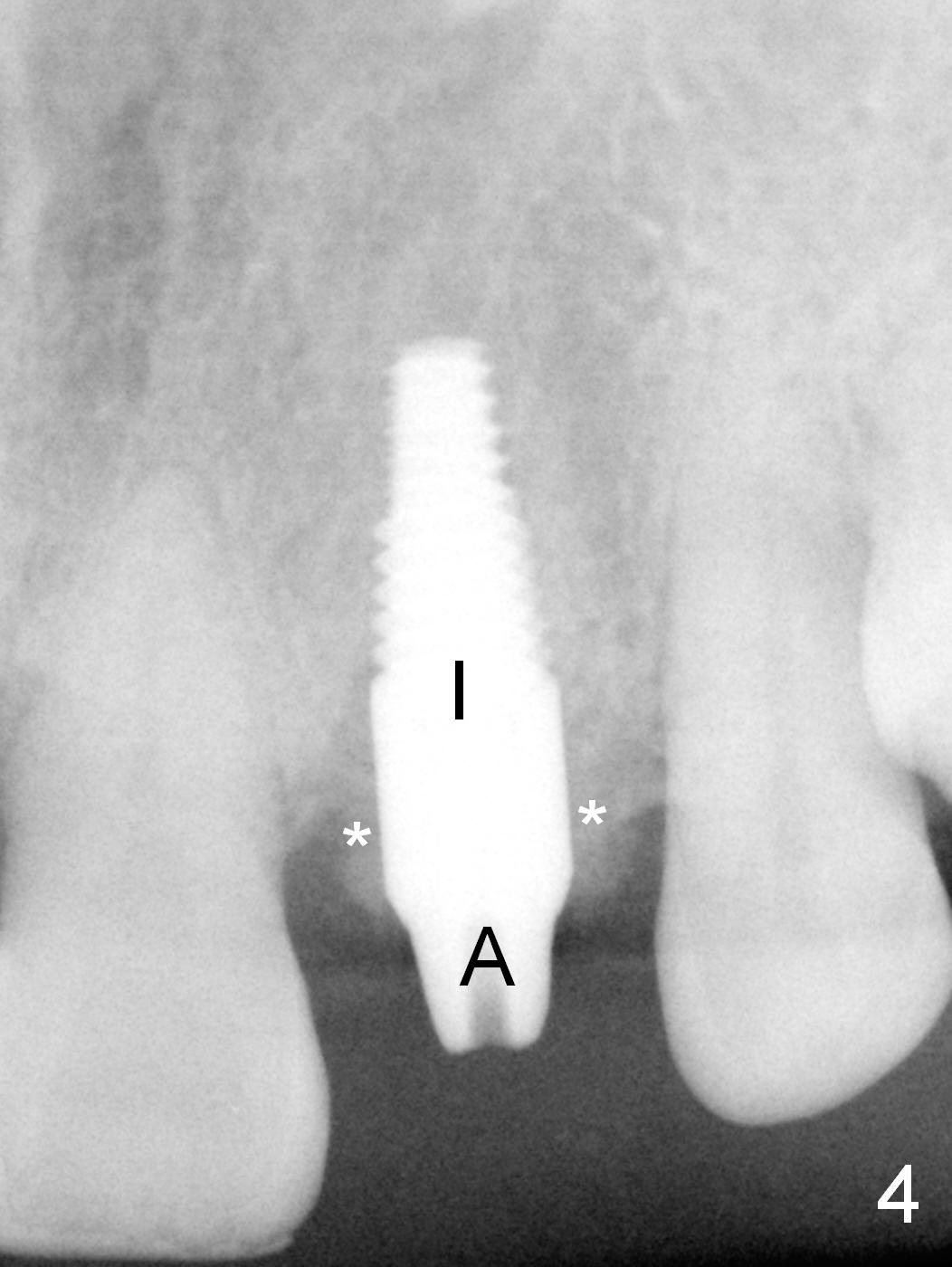
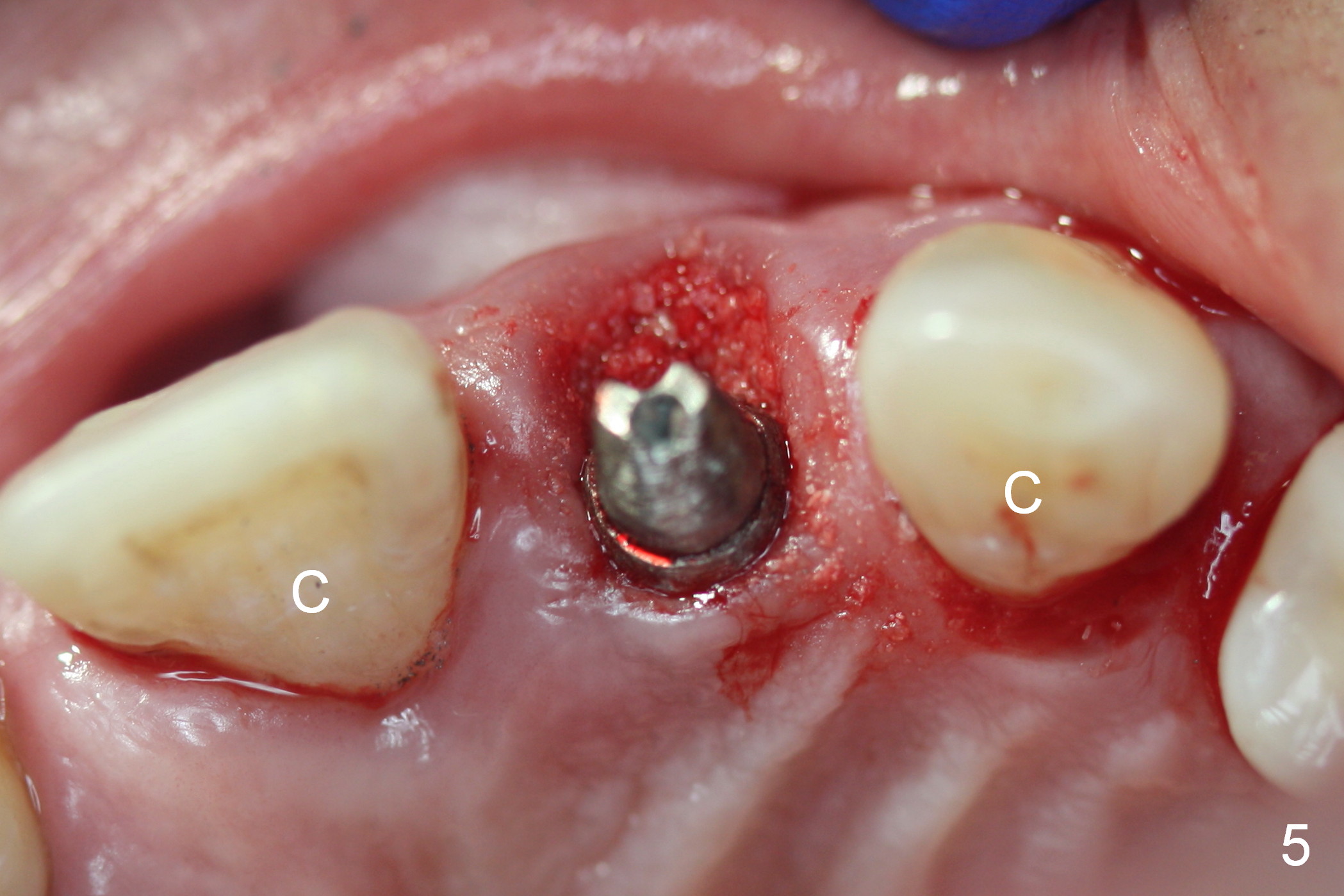
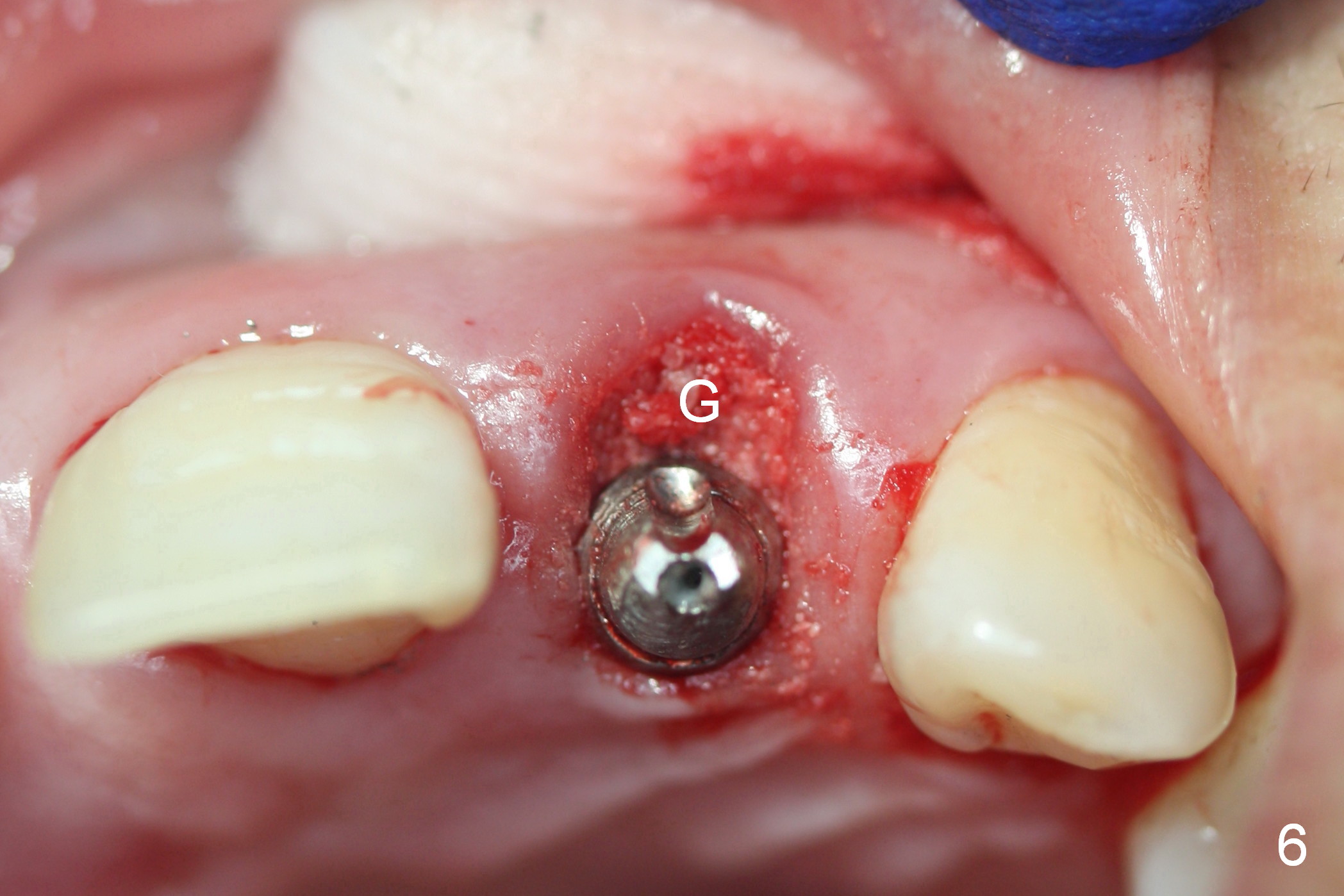
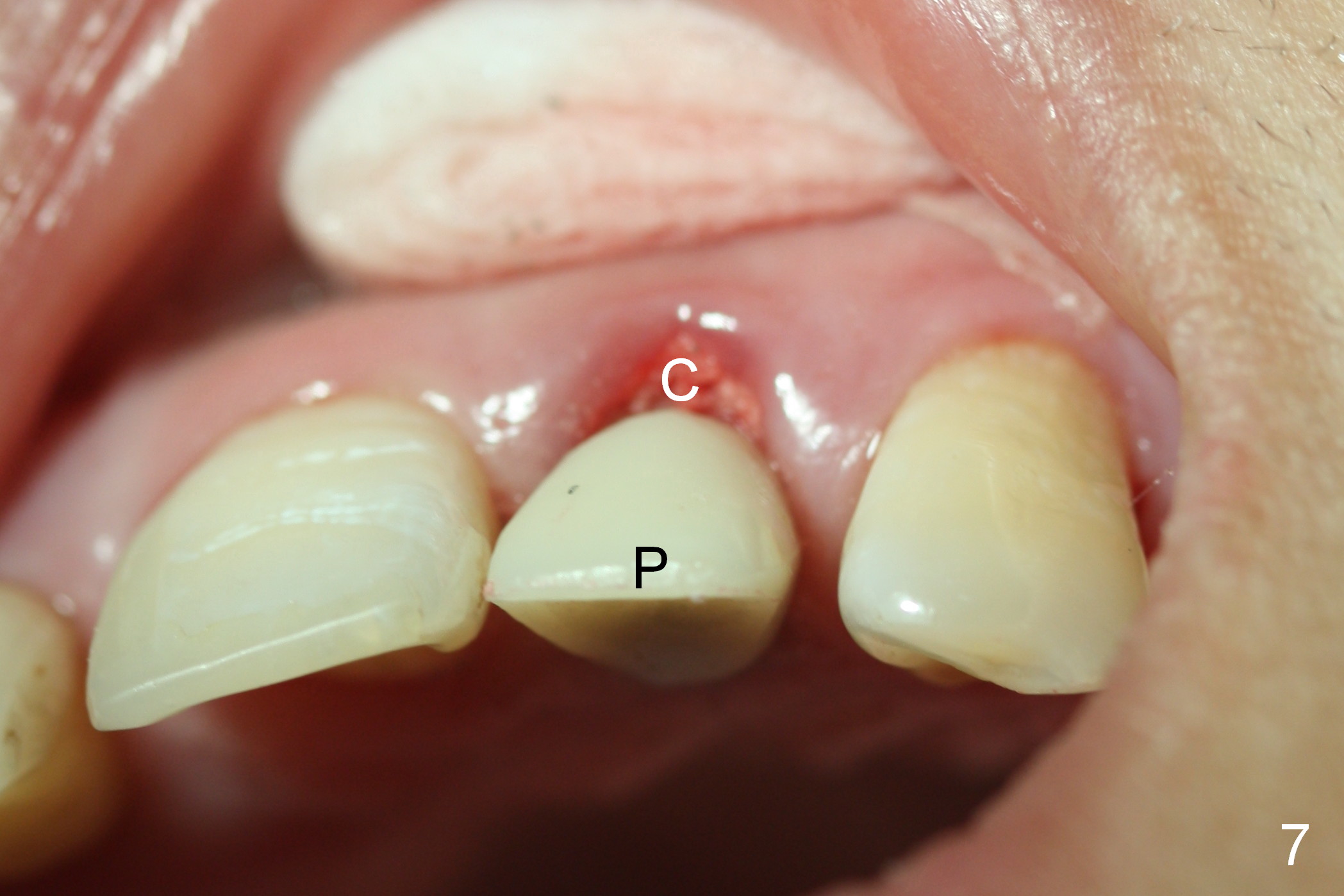
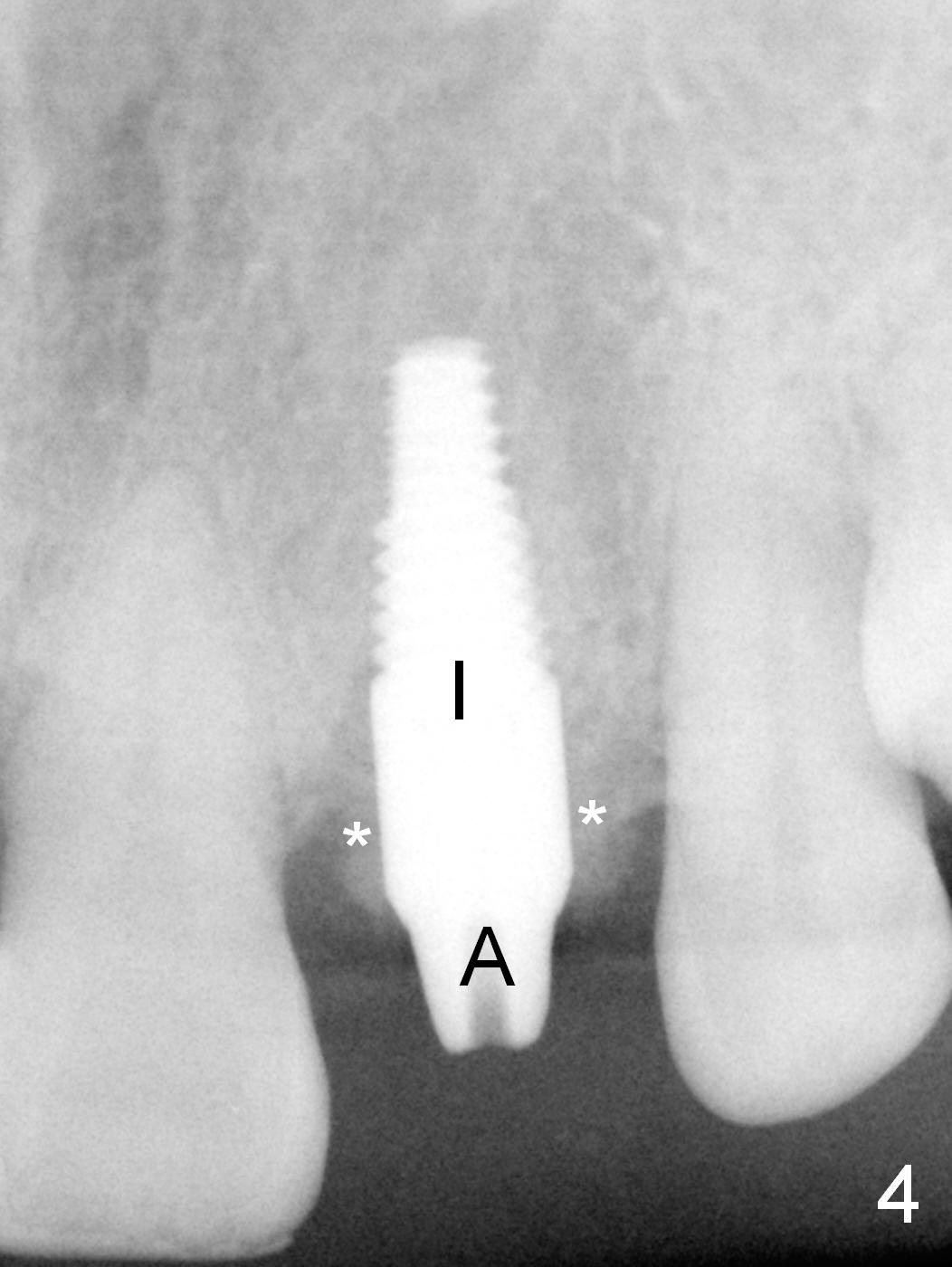
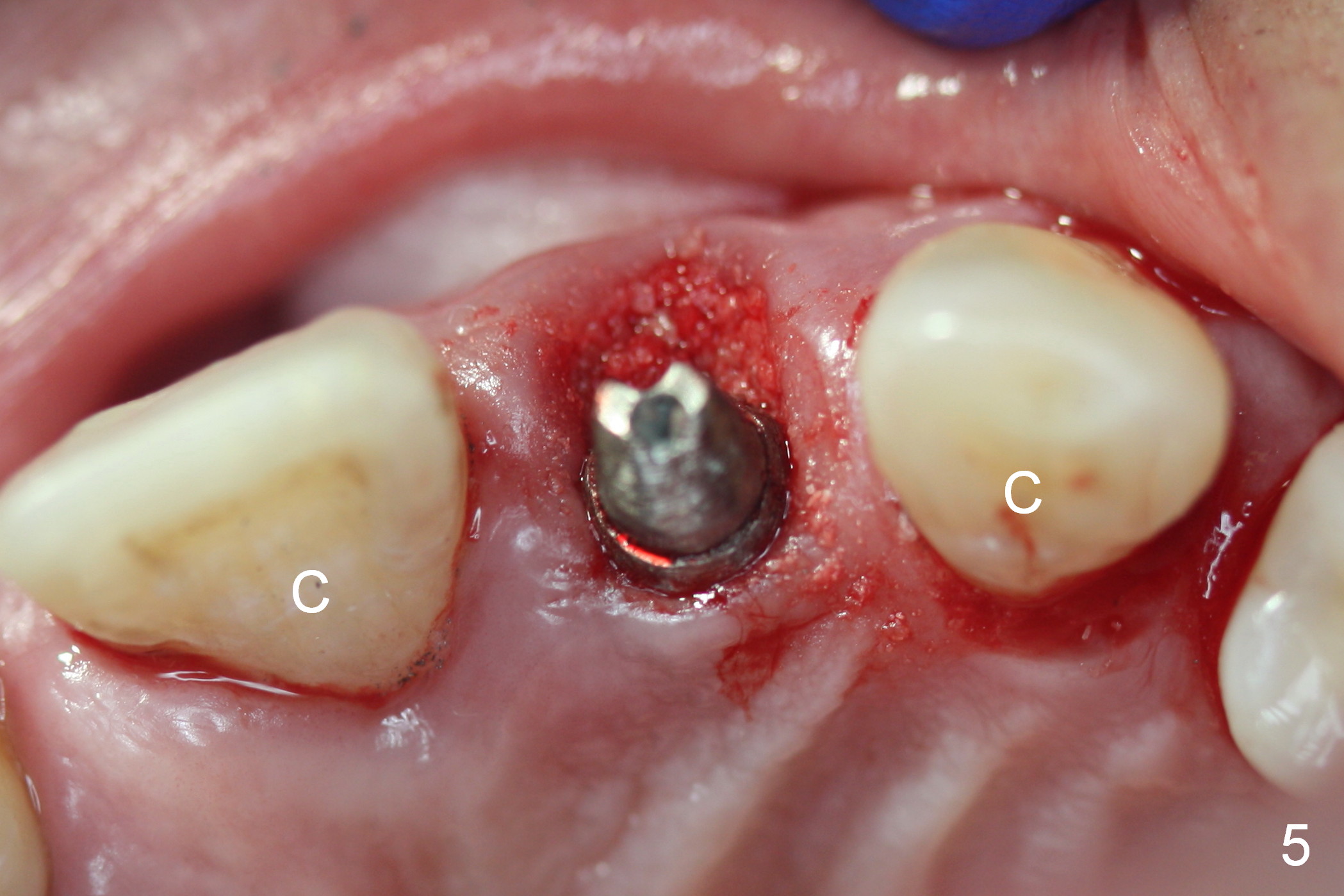
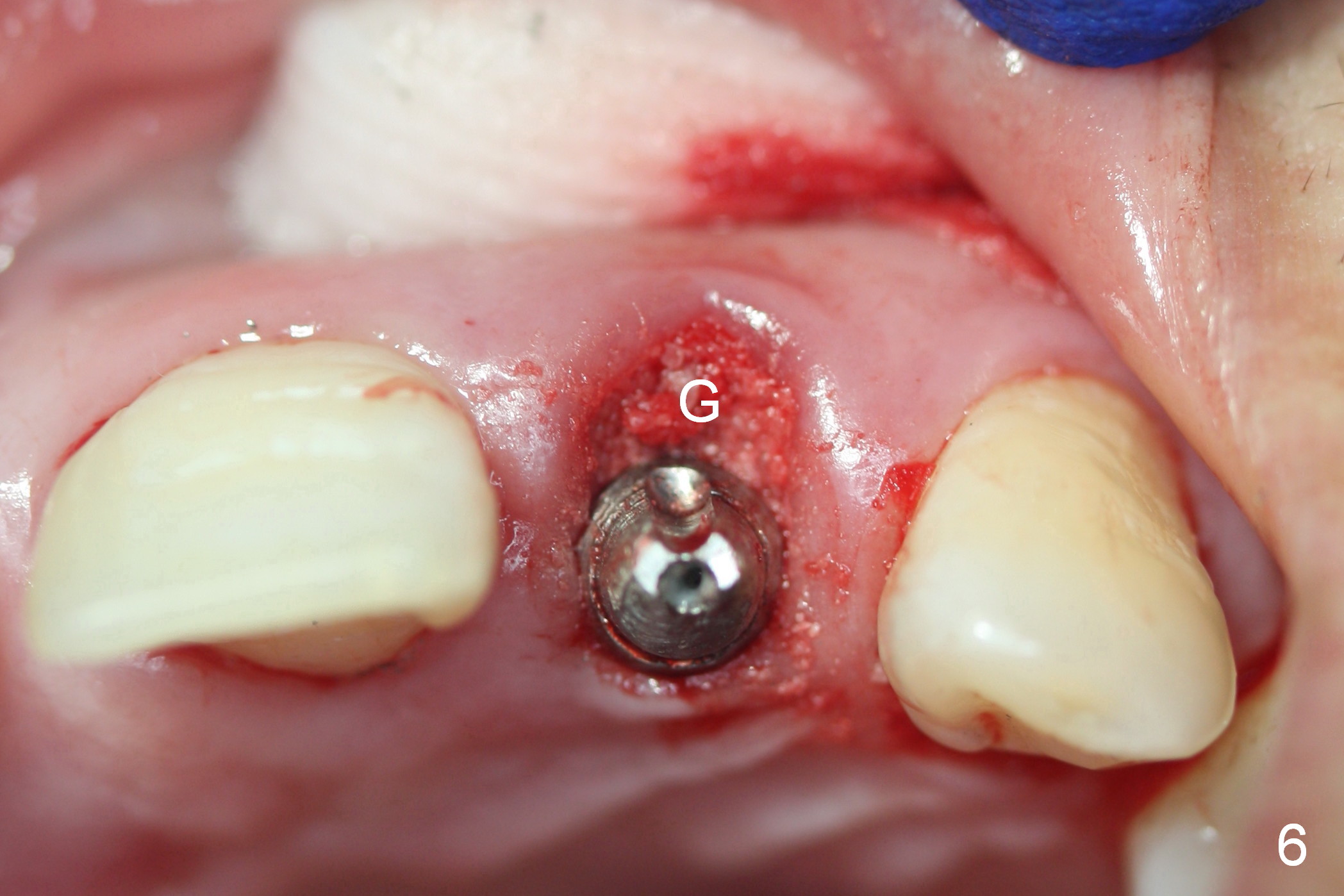
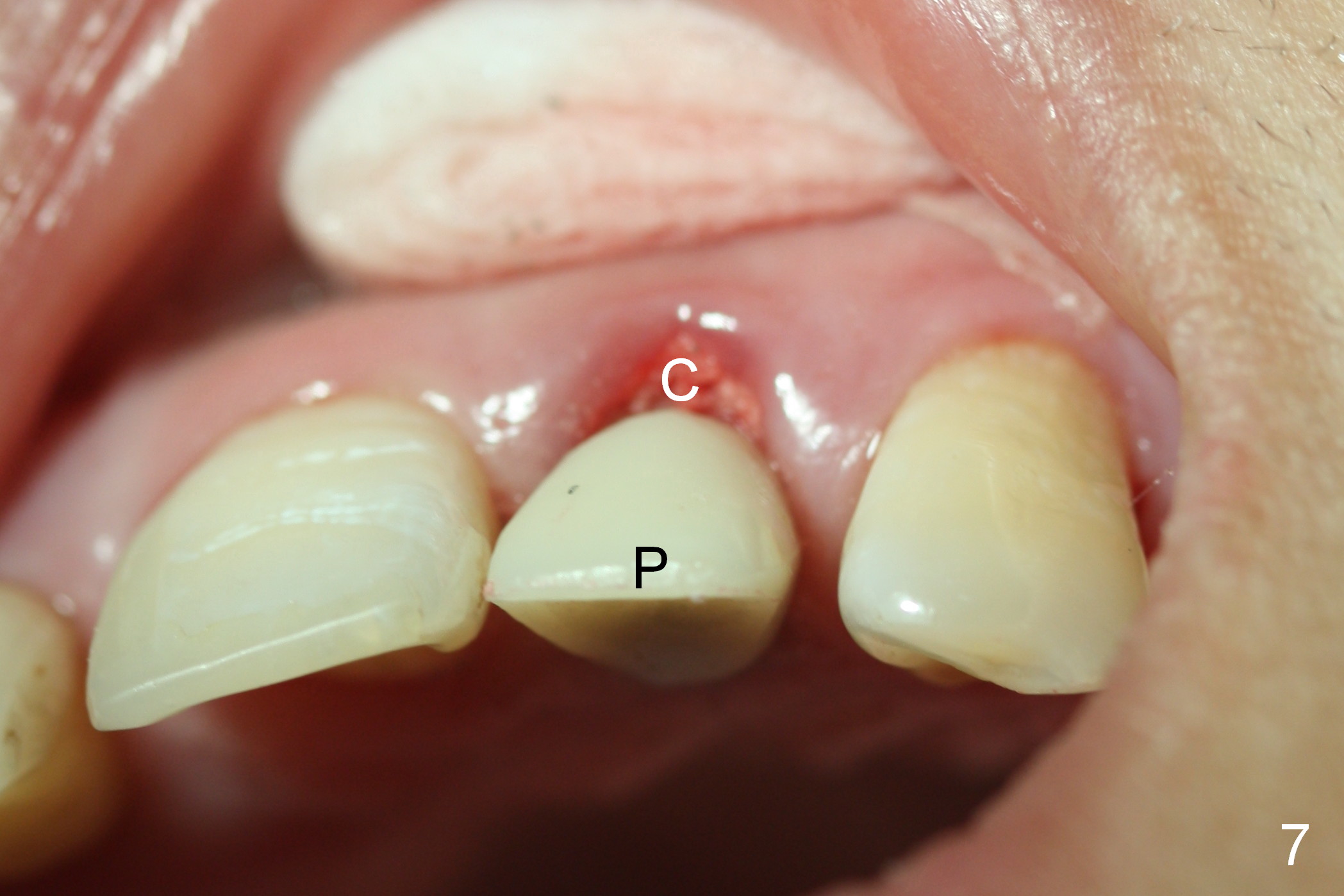
A 4.5 mm tap is stable (Fig.2 T). A 4.5x14 mm tissue-level implant (Fig.4 I) is placed with insertion torque > 60 Ncm. The implant is placed palatally, at the level of the cinguli of the neighboring teeth (Fig.5 C). The buccal gap is closed initially with bone graft (Fig.6 G), and secondarily with an immediate provisional (Fig.7 P), and collagen membrane (C). The latter is covered by perio dressing. The temporary restoration restores the normal position of the tooth (Fig.8). This case is much easier than the one done one day earlier.
The patient returns for follow up 2 weeks postop (Fig.9-12). The perio dressing has been dislodged. A flipper that restores the maxillary posterior teeth has been worn. The incisal edge of the provisional appears to have been labially displaced (Fig.9 I, compare to Fig.7). The collagen membrane is attached subgingival (Fig.9,10 *). Fig.11, 12 show the relationship between the provisional and the flipper (F) after adjustment.
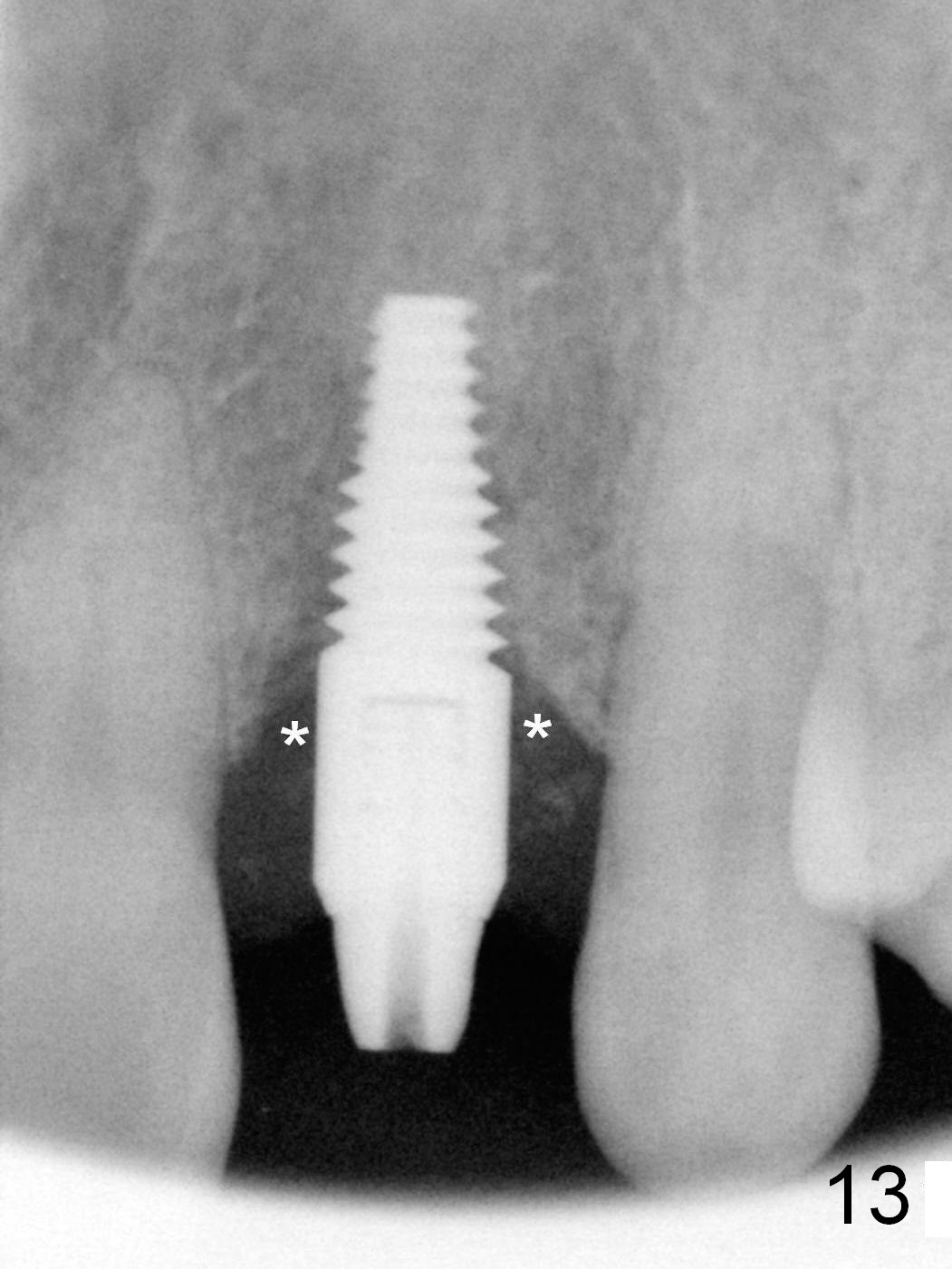
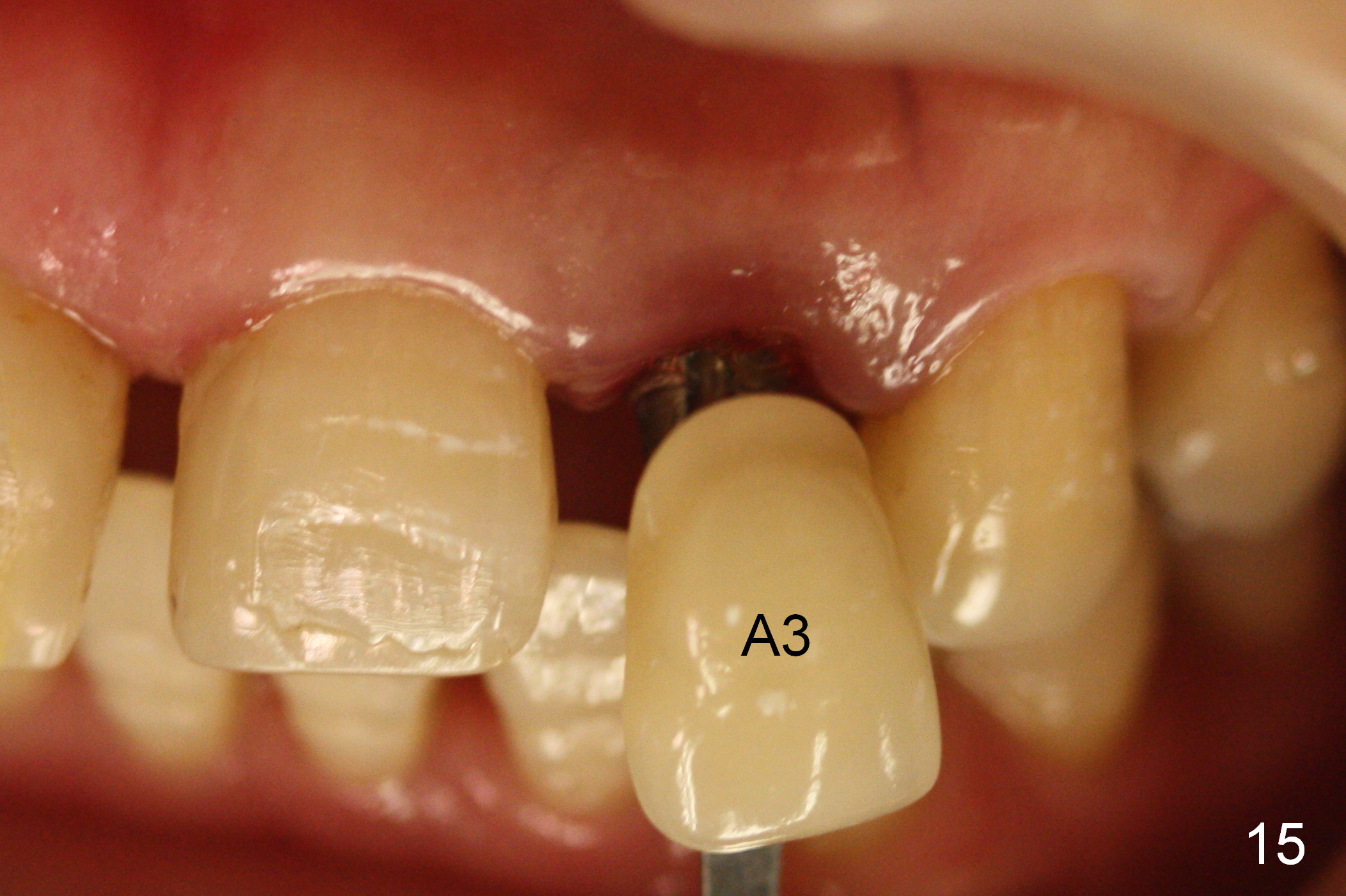
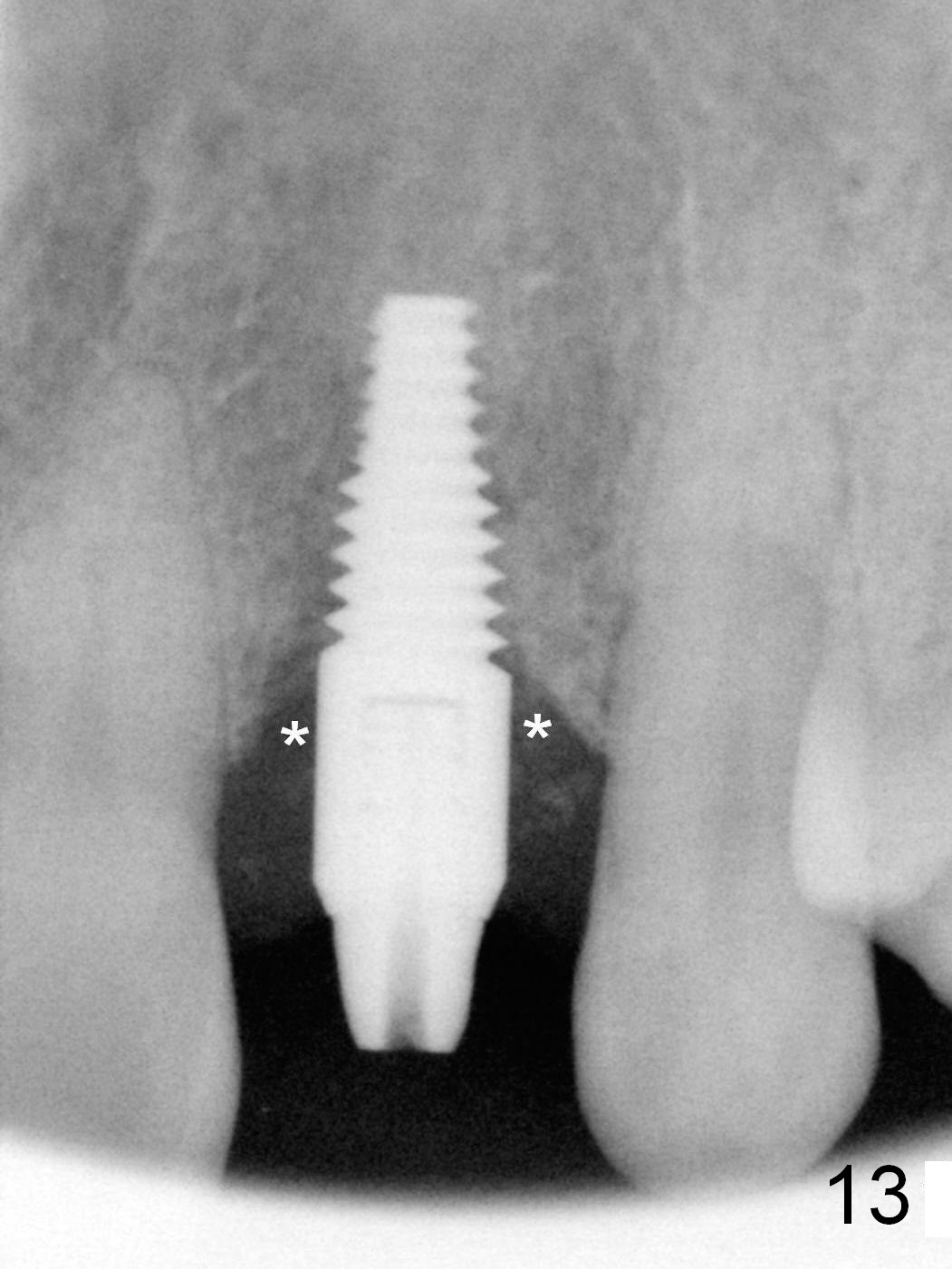
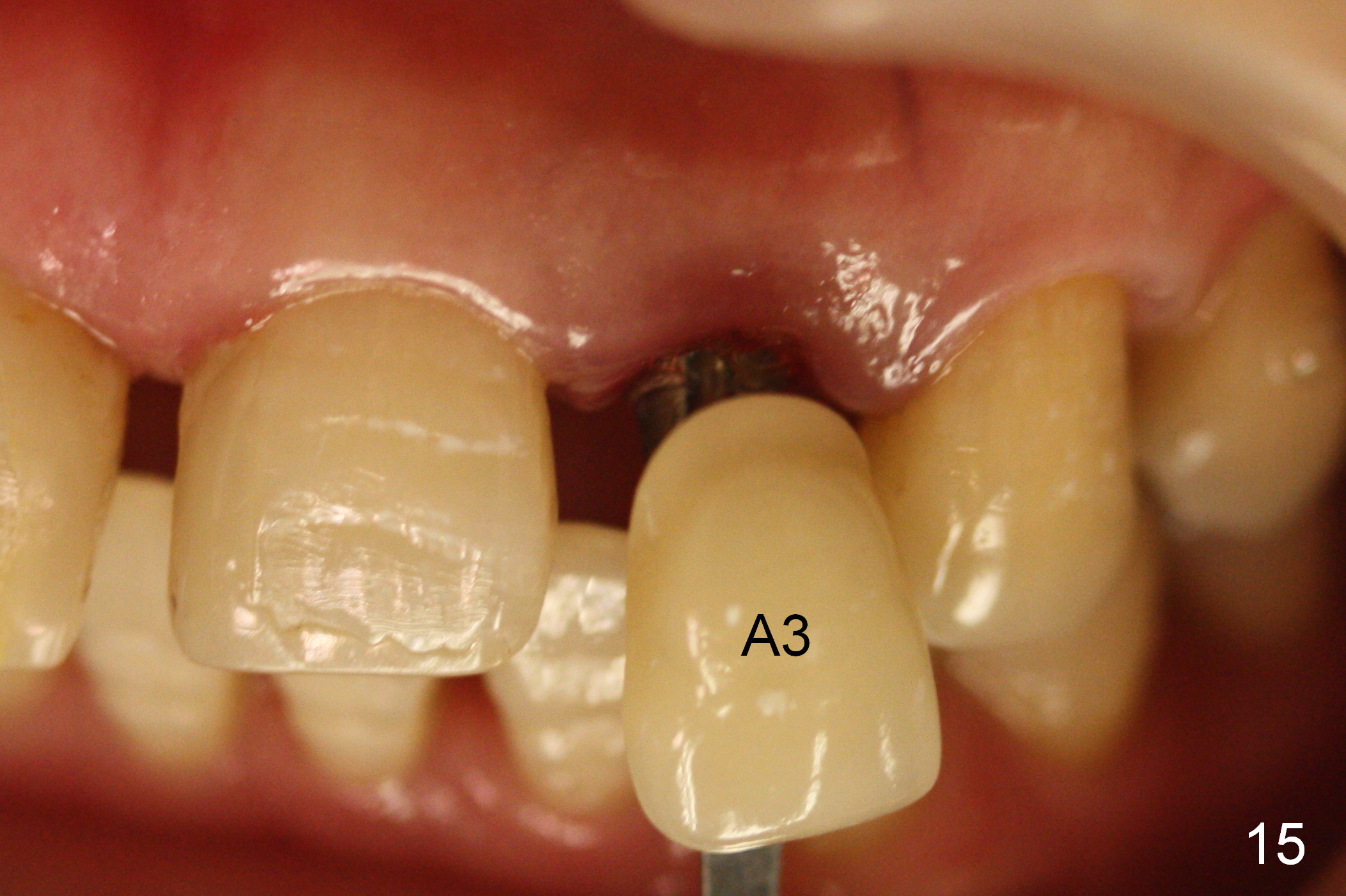
Three months postop, the implant (Fig.13) is processed for impression (stump shade (Fig.14), regular shade selection under room light (Fig.15,16) and dental headlight (Fig.17,18). The crown margin (Fig.20 ^, at the same level of the retention groove (apical end: *)) is subgingival.
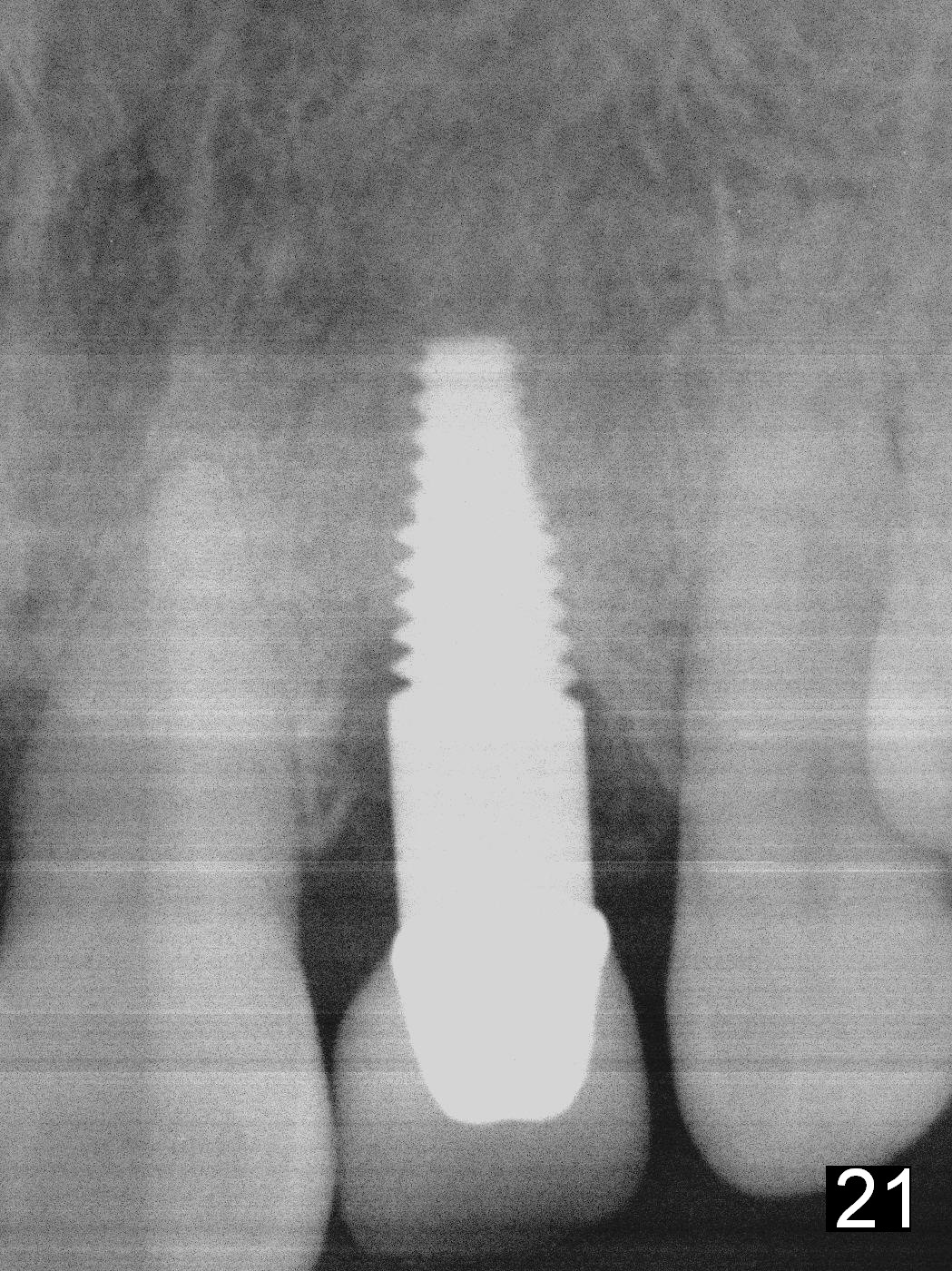
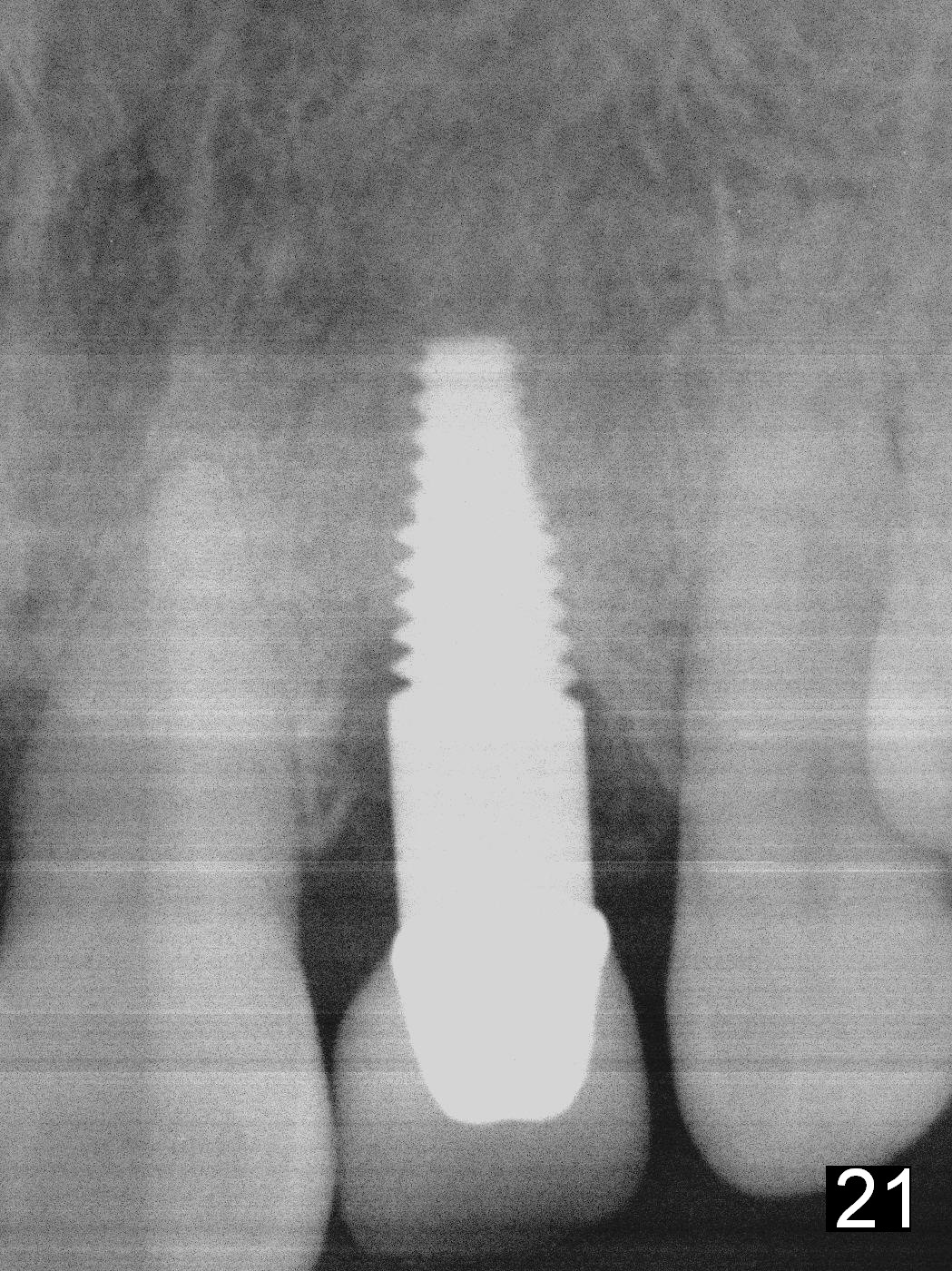
Five months post cementation, there is no sign of peri-implantitis or bone loss (Fig.21). The patient wants to take care of the displaced tooth #8.
Return to Upper Incisor Immediate Implant,
Technicians
Xin Wei, DDS, PhD, MS 1st edition 05/29/2015, last revision 01/19/2018